Summary
Background
Preoperative knowledge of intrahepatic bile duct (IHD) anatomy is critical for planning liver resections, liver transplantations and complex biliary reconstructive surgery. The purpose of our study was to demonstrate the imaging features of various anatomical variants of IHD using magnetic resonance cholangio-pancreatography (MRCP) and their prevalence in our population.
Material/Methods
This observational clinical evaluation study included 224 patients who were referred for MRCP. MRCP was performed in a 1.5-Tesla magnet (Philips) with SSH MRCP 3DHR and SSHMRCP rad protocol. A senior radiologist assessed the biliary passage for anatomical variations.
Results
The branching pattern of the right hepatic duct (RHD) was typical in 55.3% of subjects. The most common variant was right posterior sectoral duct (RPSD) draining into the left hepatic duct (LHD) in 27.6% of subjects. Trifurcation pattern was noted in 9.3% of subjects. In 4% of subjects, RPSD was draining into the common hepatic duct (CHD) and in 0.8% of subjects into the cystic duct. Other variants were noted in 2.6% of subjects. In 4.9% of cases there was an accessory duct. The most common type of LHD branching pattern was a common trunk of segment 2 and 3 ducts joining the segment 4 duct in 67.8% of subjects. In 23.2% of subjects, segment 2 duct united with the common trunk of segment 3 and 4 and in 3.4% of subjects segment 2, 3, and 4 ducts united together to form LHD. Other uncommon branching patterns of LHD were seen in 4.9% of subjects.
Conclusions
Intrahepatic bile duct anatomy is complex with many common and uncommon variations. MRCP is a reliable non-invasive imaging method for demonstration of bile duct morphology, which is useful to plan complex surgeries and to prevent iatrogenic injuries.
MeSH Keywords: Anatomic Variation; Bile Ducts, Intrahepatic; Cholangiopancreatography, Magnetic Resonance
Background
The anatomy of the biliary tree is complex, with the existence of multiple intrahepatic and extrahepatic anatomical variants. Serious consideration of the surgical anatomy of the liver has begun with the advent of therapeutic interventions for the bile duct, liver resections and partial liver transplantations with increasing frequency and complexity. Accurate widespread knowledge of the biliary anatomy and its variations is needed to plan the surgeries and minimize post-operative complications [1,2]. MRCP is an accurate and non-invasive imaging technique for demonstration of bile duct anatomy. It is a safer modality, devoid of ionizing radiation, which can be performed in patients allergic to iodinated contrast agents [2–4].
The intrahepatic bile ducts typically follow the portal veins along their anterior aspect. The right hepatic duct is composed of an anterior segmental branch, which drains Couinaud’s segment 5 and 8 of the liver, and a posterior segmental branch, which drains segment 6 and 7. The right anterior sectoral duct (RASD) is vertically oriented whereas the right posterior sectoral duct (RPSD) is more horizontally oriented. Normally, RPSD passes posterior to RASD and joins it from the medial aspect. The left hepatic duct drains segments 2, 3 and 4 of the liver. The bile duct from the caudate lobe usually joins the origin of the left and right hepatic ducts. The right and left main hepatic ducts unite in the hilum to form the common hepatic duct (CHD) [1,5]. The typical branching pattern is seen in 50–60% of population with a significant number of subjects showing variation in the branching pattern.
The purpose of our study was to demonstrate the imaging features of various anatomical variants of IHD using magnetic resonance cholangio-pancreatography (MRCP) and to document the prevalence of each type in our population.
Material and Methods
The Institutional Medical Ethics Committee approved this study for a period of two years, i.e. from 2011 to 2013. In our present study, 255 MRCP cases were analysed who were referred to MRCP with different clinical diagnoses. As many as 31 of them were excluded due to poor images and obscuration of biliary anatomy by gross hepatic and biliary pathologies. Hence, our final study group included a total number of 224 cases (113 males and 111 females; age range 12–86 yrs).
A Philips 1.5-Tesla MRI unite with a torso phased-array coil was used. Thick Slab MRCP sequence (SSh MRCP Rad: TR-8000 ms; TE-800 ms; flip angle 90 degrees; FOV 300 mm; 40 mm thick oblique coronal slices at 0.4-mm interval on breath hold) was taken with the sections passing through the porta hepatis and rotating around a point anterior to the portal vein. Thin Slab sequence (MRCP HR SENSE: TR-1204 ms; TE-650 ms; flip angle – 90 degrees; FOV 260; 1 mm thick straight coronal sections at 0.8-mm interval) with maximum intensity projection (MIP) sets of MRCP HR SENSE sequence were obtained in the coronal plane.
Image analysis: A senior consultant radiologist assessed the images in PACS and presence of any common or uncommon variants was documented. The following intrahepatic anatomic variants were studied.
Huang et al. [6] classified the right intrahepatic bile ducts depending on the site of insertion of the right posterior sectoral bile duct (RPSD), into 5 types. Karakas HM et al. [7] revised the classification depending on the site of insertion of RPSD as well as its distance from the confluence of RASD and LHD (Table 1).
Table 1.
Classification of right hepatic duct variations according to Huang et al. and Karakas et al.
| Huang type | Description | Karakas type |
|---|---|---|
| A1 | Right posterior sectoral duct (RPSD) drains into the right anterior sectoral duct (RASD) | K1 – distance of RPSD and RASD junction >1 cm from the confluence of RHD and LHD |
| K2a – distance of RPSD and RASD junction ≤1 cm from the confluence of RHD and LHD | ||
| A2 | Trifurcation pattern of insertion of RPSD, RASD and left hepatic duct (LHD) | K2b |
| A3 | RPSD drains into LHD | K3a – junction of RPSD and LHD ≤1 cm from the confluence |
| K3b – junction of RPSD and LHD >1 cm from confluence | ||
| A4 | RPSD drains into the common hepatic duct (CHD) | K4 |
| A5 | RPSD drains into the cystic duct | K5 |
The left hepatic duct confluence was classified into three types according to Cho A et al. [8] (Table 2).
Table 2.
Classification of left hepatic duct variations according to Cho A et al.
| Classification | Description |
|---|---|
| Type 1 | Segment 2 and 3 ducts join to form a single lateral segmental duct with one or two segment 4 ducts opening into this and forming LHD |
| Type 2 | A common trunk of segment 3 and 4 ducts forms the common channel and segment 2 duct joins to form LHD |
| Type 3 | Segment 2, 3 and 4 ducts joins together to form LHD |
Further aberrant and accessory bile ducts and complex unclassified patterns of biliary tree variants are accordingly described.
Statistical Methods: Descriptive and inferential statistical analysis was carried out and results on continuous measurements were presented as Mean ±SD (Min-Max) and results on categorical measurements in Number (%).
Results
According to the Huang classification, type A1 branching pattern was noted in 124 (55.3%) cases, type A2 in 26 (9.3%) cases, type A3 in 62 (27.6%) cases, type A4 in 9 (4.0%) cases, and type A5 in 2 (0.8%) cases.
According to Karakas, type K1 was seen in 26.3%, K2a in 29%, K2b in 9.3%, K3a in 25.8%, K3b in 1.7%, K4 in 4.0%, and K5 in 0.8% of subjects.
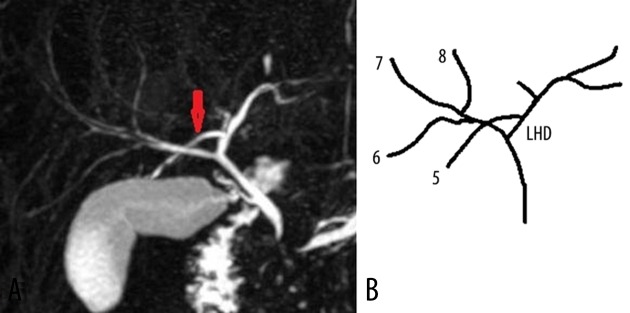
Normally, RPSD joins RASD from the medial aspect. In 5 out of 124 subjects, RPSD joined RASD from the lateral aspect (Figure 1).
Figure 1.
(A) Coronal 3D MR cholangiopancreatography, and (B) schematic diagram show RPSD (red arrow) joining the RASD (white arrow) from its lateral aspect. CD – Cystic duct, GB – gall bladder.
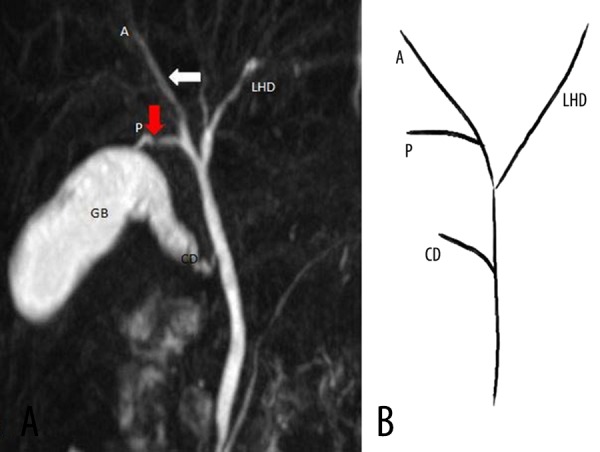
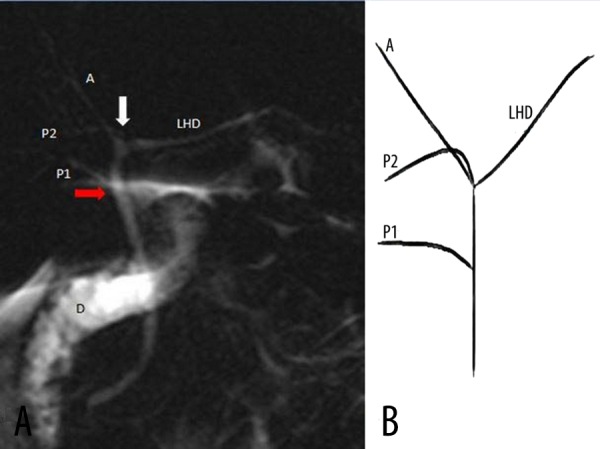
In 5 (2.2%) of our cases there was separate drainage of the superior and inferior RPSD. In 1 case, the superior RPSD joined RASD and the inferior RPSD joined CHD. In 1 case, the superior RPSD entered between the confluence of RASD and LHD and the inferior RPSD entered CHD (Figure 2). In 2 cases the superior RPSD joined LHD and the inferior RPSD joined CHD (Figure 3). In 1 case, the superior and inferior RPSD joined RASD separately.
Figure 2.
(A) Coronal 3D MR cholangiopancreatography and, (B) schematic diagram show the superior RPSD draining into the confluence supraportally (white arrow), forming trifurcation pattern and the inferior RPSD joining CHD infraportally (red arrow). A – RASD, P1 – inferior RPSD, P2 – superior RPSD, D – duodenum.
Figure 3.
(A) Coronal 3D MR cholangiopancreatography, (B) and schematic diagram show the superior RPSD from segment 7 (red arrow) draining into LHD and the inferior RPSD from segment 6 (blue arrow) joining CHD infraportally.
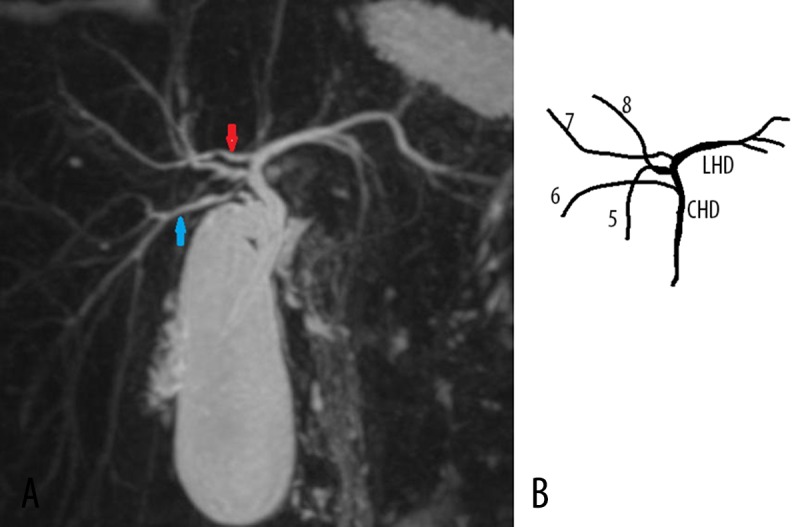
Aberrant segmental duct from the right lobe was seen in 10 (4.4%) cases. In one case, segment 6, 7, and 8 joined together to form RHD. Aberrant duct from segment 5 was seen joining LHD (Figure 4). In another case there was a common duct of segment 5 and 6 joining CHD (Figure 5).
Figure 4.
(A) Coronal 3D MR cholangiopancreatography, and (B) schematic diagram show ducts from segment 6, 7 and 8 joining together to form RHD, and an aberrant duct from segment 5 (red arrow) joining LHD.
Figure 5.
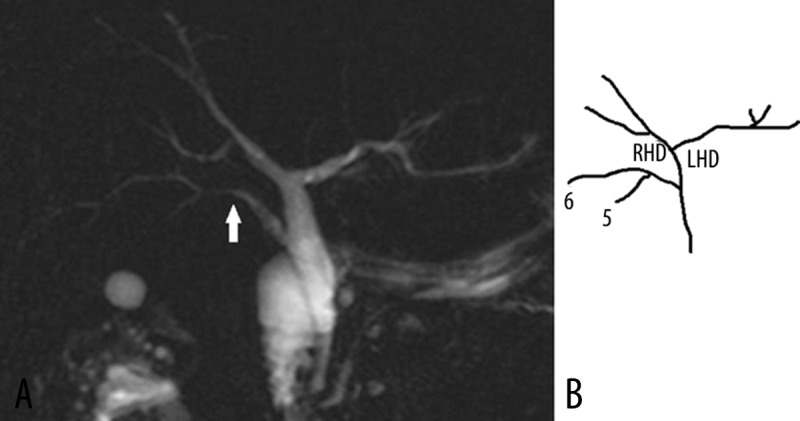
(A) Coronal 3D MR cholangiopancreatography, and (B) schematic diagram show aberrant drainage of segment 5 and 6 into CHD through a common duct (white arrow).
Type 1 LHD confluence was seen in 152 (67.8%) subjects, type 2 in 52 (23.2%) and type 3 in 9 (4.0%) (Figures 6–8). Other uncommon branching patterns of LHD were seen in 11 (4.9%) cases. Aberrant union of segment 2 duct to the right hepatic duct was seen in 2 (0.8%) cases, aberrant union of segment 2 duct at the confluence of RHD and LHD was seen in 1 (0.4%) case, aberrant union of segment 4 duct to the common hepatic duct was seen in 5 (2.2%) cases and aberrant union of segment 4 duct at the confluence of RHD and LHD was seen in 2 (0.8%) cases (Figures 9, 10).
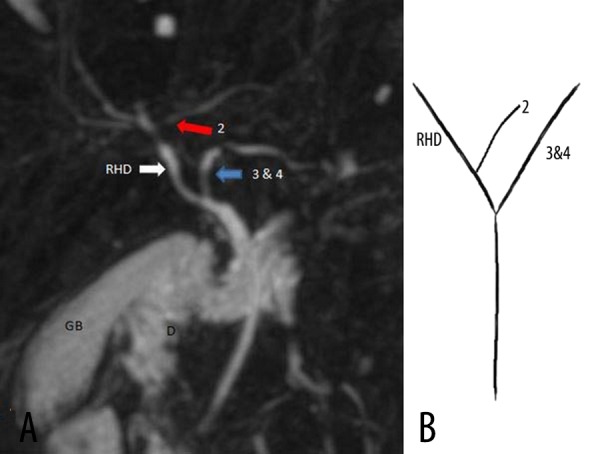
Figure 6.
(A) Coronal oblique 3D MR cholangiopancreatography and, (B) schematic diagram show type 1 LHD, in which segmental bile duct 2 and 3 form a common channel and segment 4 bile duct joins it to form LHD (white arrow). Also, note the aberrant insertion of RPSD (red arrow) into LHD with a distance of 11 mm before the confluence (Type k3a).
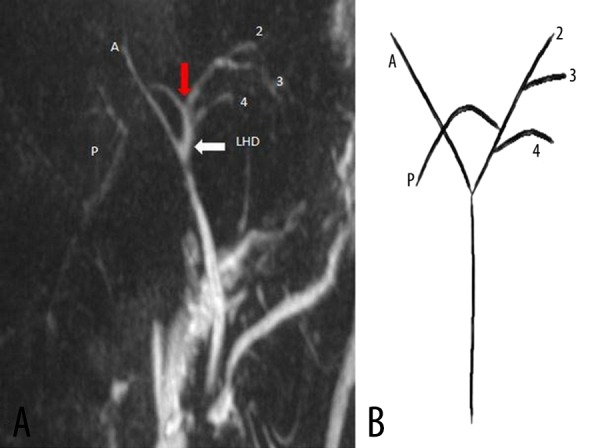
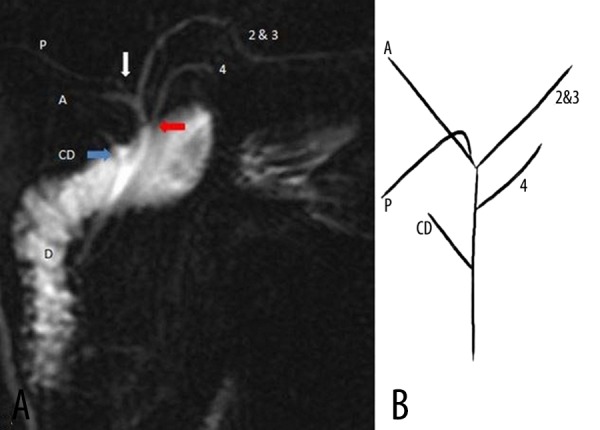
Figure 7.
(A) Coronal oblique 3D MR cholangiopancreatography, and (B) schematic diagram show type 2 LHD variant, in which segmental bile duct 3 and 4 form a common channel and segment 2 bile duct enters it to form LHD (yellow arrow). Moreover, note the aberrant insertion of RPSD (red arrow) into LHD (yellow arrow) with a distance of 8 mm from the confluence (Type K3b). There is also calculus in the gall bladder (black arrow) and CBD (black arrow head. GB – gall bladder, D – duodenum.
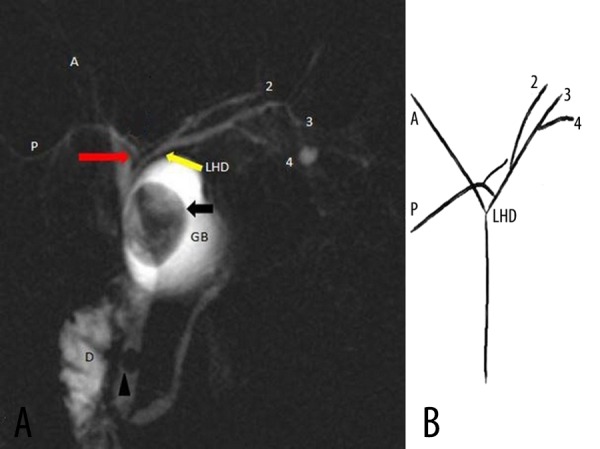
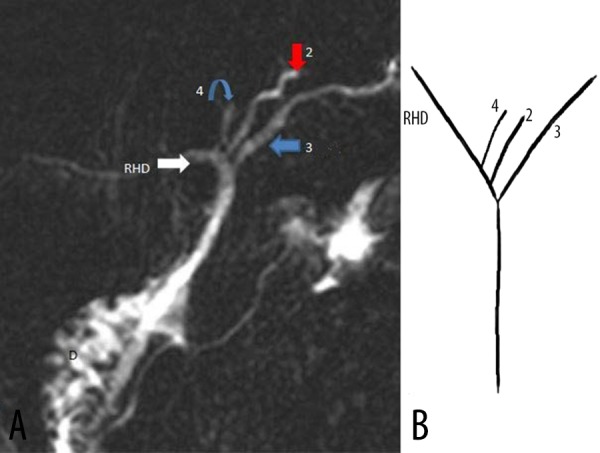
Figure 8.
(A) Coronal 3D MR cholangiopancreatography and (B) schematic diagram show type 3 LHD variant, in which segmental bile duct 2, 3 and 4 have the trifurcation pattern. Also, note the aberrant insertion of RPSD (red arrow) into LHD (white arrow). There is an accessory bile duct (blue arrow) inserting laterally at the confluence.
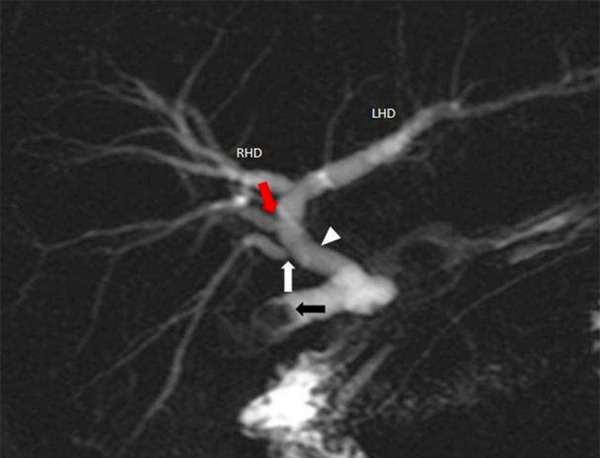
Figure 9.
(A) Coronal oblique 3D MR cholangiopancreatography and (B) schematic diagram show an aberrant union of segment 2 bile duct (red arrow) into RHD (white arrow). Segmental bile duct 3 and 4 form a common channel (blue arrow) and it drains to RHD (white arrow) to form CHD. GB – gall bladder, D – duodenum.
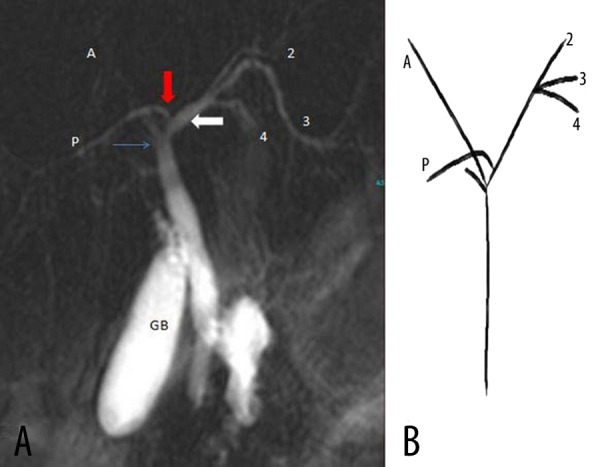
Figure 10.
(A) Coronal 3D MR cholangiopancreatography and (B) Schematic diagram reveal an aberrant union of segment 4 bile duct into CHD (red arrow). RPSD (white arrow) joins RASD to form RHD (type A1).
In 1 case there was drainage of segment 2, 3, and 4 ducts separately with RHD. No LHD was formed in that case (Figure 11).
Figure 11.
(A) Coronal oblique 3D MR cholangiopancreatography and (B) Schematic diagram show an individual union of segment 2 bile duct (red arrow), segment 3 bile duct (blue arrow) and segment 4 bile duct (curved blue arrow) into RHD (white arrow).
In 4 (1.7%) cases there was an accessory duct from the right lobe. In 2 cases it drained into CHD and in 2 cases at the lateral aspect of confluence of RHD and LHD (Figure 8). In 1 case there were aberrant and accessory segmental 5 ducts joining CHD separately (Figure 12). An accessory left hepatic duct was seen in 5 (2.2%) cases. In 4 cases it drained into RHD. In 1 case it drained into CHD.
Figure 12.
Coronal oblique 3D MR cholangiopancreatography shows an aberrant segment 5 duct (white arrow) and accessory segment 5 duct (red arrow) separately draining into CHD (white arrow head). Calculi noted within the gall bladder (black arrow).
In 1 case there was a complex branching pattern of the bile ducts (Figure 13).
Figure 13.
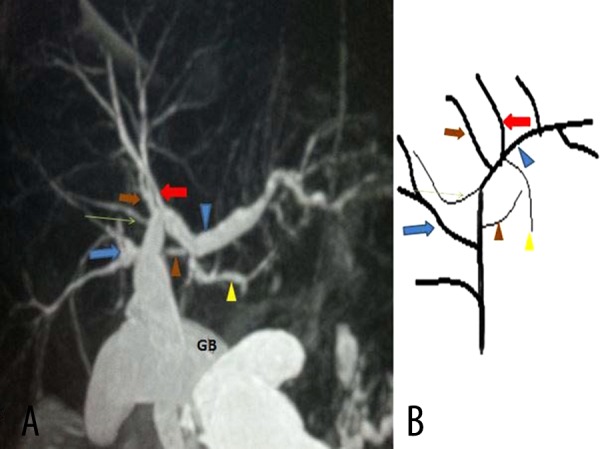
(A) Coronal oblique 3D MR cholangiopancreatography and (B) schematic diagram show a complex IHD variant. Two segment 8 ducts (brown and red arrows) and segment 7 duct (red arrow) separately join with LHD to form CHD, followed by an accessory segment 7 duct (green arrow) and common channel of segment 5 and 6 ducts (blue arrow) entering CHD. Accessory segment 4 duct (brown arrow head) enters CHD medially. Segment 4 duct (yellow arrow head) joining the common channel of segment 2 and 3 to form LHD.
Discussion
Typical branching patterns of intrahepatic biliary ducts are found in 53–63% of population [9–12]. In our present study this typical anatomy was seen in 55.3% of cases. Various anatomical variations in bile duct branching have been recognized and different classifications have been proposed [6–9,11]. However, none of them is complete and several uncommon rare variations have been identified in different studies [12]. Knowledge of the intrahepatic duct branching pattern and its variants is very important prior to right or left liver harvesting in living donor liver transplantation, segmental or lobar resection, or biliary intervention procedures. Presence of these variations makes the surgery technically more difficult and increases postoperative complication [1,13,14]. Drainage of the right posterior sectoral duct (RPSD) to the left hepatic duct was the most common variant in our study (27.6%) followed by trifurcation pattern (9.3%). This finding is common also to other previous studies [7,9,11,13–15]. Presence of this variation increases the chance of right sectoral bile duct injury during left hepatic resections. Drainage of RPSD to LHD with acute angulation increases the risk of bile stasis and repeated cholangitis [11,12]. Different studies have shown that incidence of bile duct variation varied among different population groups [7]. Karakas et al. studied the distance of RPSD insertion in the right or left hepatic duct from the confluence. They divided type A1 into K1 and K2a, and type A3 into K3a and K3b. In 29% of our patients with type A1 pattern of RHD branching, the distance of RPSD insertion was less that 1 cm from the confluence (Karakas type K2a). Similarly, in 1.7% of patients with type A3 pattern, the distance was less than 1 cm (Karakas type K3b). Preoperative knowledge regarding the distance of the branches from the confluence helps the surgeon to modify the surgical procedure with a requirement of a more demanding microsurgical technique in these groups of patients [7].
Separate superior and inferior RPSD drainage was noted in 2.2% of our cases. Ohkhubo et al. reported a similar pattern in 5% of their cases [11]. Aberrant posterior sectoral or segmental duct from the right lobe to the common hepatic duct was noted in 9% of our cases and to the cystic duct in 1.3%. During laparoscopic cholecystectomy, inadvertent resection or ligation of these ducts might lead to complications like biloma, bile leakage and atrophy of the draining segment [1,9,16,17].
The most prevalent left hepatic duct confluence in our study was of type 1 (67.8%), i.e. where the common channel of segment 2 and 3 joins with segment 4 duct to form LHD. This pattern was seen in 59–78% of patients in previous studies [8,10,11]. Aberrant segment 4 duct draining into the confluence of RHD and LHD was noted in 0.8% of our cases and into CHD in 2.2% of our cases. Ohkhubo et al. reported a 2% incidence of such an anomaly [11]. Good anatomical knowledge of these ducts is essential before segmentectomy for hilar malignancy or left lobe harvesting in living donor liver transplantation [10,11,18].
Another uncommon variation is an accessory duct, which was reported in 2–6% of cases as a solitary finding or as associated with other variants [1,9]. Accessory duct is an additional bile duct draining a particular segment in addition to a normal duct. Aberrant duct is the only duct draining a particular segment with anomalous drainage. Aberrant ducts are surgically more important. Ligation or injury of accessory ducts leads to biloma and bile leakage and ligation of aberrant duct causes recurrent cholangitis and atrophy of the draining segment or segments [1,14]. We have seen accessory ducts from the right lobe in 1.7% of our subjects and from the left lobe in 2.2% of cases.
Many unclassified complex anatomy cases have been reported in different studies. We saw three such cases. In one case there were two parallel aberrant and accessory ducts draining into CHD. In the second case, bile ducts from segment 2, 3, and 4 joined RHD separately, without formation of LHD. In the third case the anatomy was more complex, involving both right and left lobe ducts. These rare but complex anatomies should be recognized prior to any surgery or intervention procedure [12].
Limitation of our study was that we did not compare the result with any other modality like intrahepatic cholangiogram. Segmental and subsegmental branches in a non-dilated system are sometimes difficult to identify in unenhanced MRCP and identification of small aberrant and accessory ducts may not be possible.
Hepatocyte specific gadolinium-enhanced MRCP has been proven to be more accurate in delineating the anatomy of bile ducts [19]. However, limited availability, high cost, longer acquisition time and risk of contrast-induced adverse reactions are some of the limitations of this procedure [20].
Conclusions
Anatomical variations of biliary passage have been encountered on various levels with existence of multiple common and uncommon anomalies. MRCP is used as a modality for safer and non-invasive evaluation of biliary diseases and in preoperative imaging of complex hepatic surgical procedures, liver donors and biliary interventions. Knowledge of these variations is useful to prevent iatrogenic injuries which increase post-operative morbidity and mortality.
References
- 1.Mortelé KJ, Ros PR. Anatomic variants of the biliary tree: MR cholangiographic findings and clinical applications. Am J Roentgenol. 2001;177:389–94. doi: 10.2214/ajr.177.2.1770389. [DOI] [PubMed] [Google Scholar]
- 2.Hyodo T, Kumano S, Kushihata F, et al. CT and MR cholangiography: Advantages and pitfalls in perioperativeevaluation of biliary tree. Br J Radiol. 2012;85:887–96. doi: 10.1259/bjr/21209407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Catalano OA, Singh AH, Uppot RN, et al. Vascular and biliary variants in the liver: implications for liver surgery. Radiographics. 2008;28:359–78. doi: 10.1148/rg.282075099. [DOI] [PubMed] [Google Scholar]
- 4.Xu YB, Bai YL, Min ZG, Qin SY. Magnetic resonance cholangiography in assessing biliary anatomy in living donors: A meta-analysis. World J Gastroenterol. 2013;19:8427–34. doi: 10.3748/wjg.v19.i45.8427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gazelle GS, Lee MJ, Mueller PR. Cholangiographic segmental anatomy of the liver. Radiographics. 1994;14:1005–13. doi: 10.1148/radiographics.14.5.7991810. [DOI] [PubMed] [Google Scholar]
- 6.Huang TL, Cheng YF, Chen CL, Lee TY. Variants of the bile ducts: clinical application in the potential donor of living related hepatic transplantation. Transplant Proc. 1996;28(3):1669–70. [PubMed] [Google Scholar]
- 7.Karakas HM, Celik T, Alicioglu B. Bile duct anatomy of the Anatolian Caucasian Population. Surg Radiol Anat. 2008;30:539–45. doi: 10.1007/s00276-008-0365-y. [DOI] [PubMed] [Google Scholar]
- 8.Cho A, Okazumi S, Yoshinaga Y, et al. Relationship between left biliary duct system and left portal vein: evaluation with three-dimensional portocholangiography. Radiology. 2003;228:246–50. doi: 10.1148/radiol.2281020740. [DOI] [PubMed] [Google Scholar]
- 9.Choi JW, Kim TK, Kim KW, et al. Anatomic variation in intrahepatic bile ducts: an analysis of intraoperative cholangiograms in 300 consecutive donors for living donor liver transplantation. Korean J Radiol. 2003;4:85–90. doi: 10.3348/kjr.2003.4.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kitami M, Takase K, Murakami G, et al. Types and frequencies of biliary tract variations associated with a major portal venous anomaly: Analysis with multi-detector row CT cholangiography. Radiology. 2006;238:156–66. doi: 10.1148/radiol.2381041783. [DOI] [PubMed] [Google Scholar]
- 11.Ohkubo M, Nagino M, Kamiya J, et al. Surgical anatomy of the bile ducts at the hepatic hilum as applied to living donor liver transplantation. Ann Surg. 2004;239:82–86. doi: 10.1097/01.sla.0000102934.93029.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kostov DV, Kobakov GL. Six rare biliary tract anatomic variations: implications for liver surgery. Eurasian J Med. 2011;43:67–72. doi: 10.5152/eajm.2011.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma V, Saraswat VA, Baijal SS, Choudhuri G. Anatomic variations in intrahepatic bile ducts in a north Indian population. J Gastroenterol Hepatol. 2008;23:e58–62. doi: 10.1111/j.1440-1746.2008.05418.x. [DOI] [PubMed] [Google Scholar]
- 14.Barsoum NR, Samie AA, Adel A, Asaad RE. Role of MRCP in assessment of biliary variants in living donor liver transplantation. The Egyptian Journal of Radiology and Nuclear Medicine. 2013;44:131–36. [Google Scholar]
- 15.Lyu SY, Pan KT, Chu SY, et al. Common and rare variants of the biliary tree: Magnetic resonance cholangiographic findings and clinical implications. J Radiol Sci. 2012;37:59–67. [Google Scholar]
- 16.Babel N, Sakpal SV, Paragi P, et al. Iatrogenic bile duct injury associated with anomalies of the right hepatic sectoral ducts: A misunderstood and underappreciated problem. HPB Surg. 2009;2009:153269. doi: 10.1155/2009/153269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hirao K, Miyazaki A, Fujimoto T, et al. Evaluation of aberrant bile ducts before laparoscopic cholecystectomy: helical CT cholangiography versus MR cholangiography. Am J Roentgenol. 2000;175(3):713–20. doi: 10.2214/ajr.175.3.1750713. [DOI] [PubMed] [Google Scholar]
- 18.Kawarada Y, Das BC, Onishi H, et al. Surgical anatomy of the bile duct branches of the medial segment (B4) of the liver in relation to hilar carcinoma. J Hepatobiliary Pancreat Surg. 2000;7(5):480–85. doi: 10.1007/s005340070018. [DOI] [PubMed] [Google Scholar]
- 19.Chiang HJ, Hsu HW, Chen PC, et al. Magnetic resonance cholangiography in living donor liver transplantation: comparison of preenhanced and post-gadolinium-enhanced methods. Transplant Proc. 2012;44(2):324–27. doi: 10.1016/j.transproceed.2011.12.035. [DOI] [PubMed] [Google Scholar]
- 20.Yeh BM, Liu PS, Soto JA, et al. MR imaging and CT of the biliary tract. Radiographics. 2009;29(6):1669–88. doi: 10.1148/rg.296095514. [DOI] [PubMed] [Google Scholar]