Abstract
A post-traumatic partial tear of the flexor hallucis longus tendon at the master knot of Henry and the resultant fibrosis of the knot can result in pain at the medial foot arch or posteromedial ankle pain with trigger hallux. Open debridement of the master knot of Henry is indicated if the symptoms do not improve with nonoperative treatment. The open procedure requires extensive soft-tissue dissection because the master knot of Henry is a deep structure. Endoscopic release of the master knot of Henry is an alternative to the open procedure and has the advantage of less surgical trauma and potential for less chance of recurrence of fibrosis of the master knot of Henry.
A flexor hallucis longus (FHL) tendon tear or fibrosis of the master knot of Henry can occur after acute or chronic repetitive hyperextension of the hallux metatarsophalangeal joint.1, 2 It can present as local pain and tenderness at the medial foot arch or as trigger hallux and pain at the posteromedial ankle.1, 2 Open debridement of the master knot of Henry has been suggested if conservative treatment cannot relieve the symptoms.1 However, this requires extensive soft-tissue dissection because the master knot of Henry is a deep structure. Endoscopic debridement has been proposed with the potential advantage of less surgical trauma and potential for less chance of recurrence of fibrosis of the master knot of Henry.2 The details of the endoscopic technique are described in this report.
Technique
The patient is prone with a thigh tourniquet applied to provide a bloodless operative field. The FHL tendon can be divided into 3 zones: Zone 1 of the FHL tendon is posterior to the ankle; zone 2 of the FHL tendon is from the fibro-osseous orifice of the posterior talar tubercles, under the sustentaculum tali, to the master knot of Henry; and zone 3 of the FHL tendon is distal to the master knot of Henry to its phalangeal insertion.3, 4, 5 Zone 1 FHL tendoscopy is performed through the posteromedial and posterolateral portals.4, 6 The posterolateral portal is at the lateral border of the Achilles tendon, just above the posterosuperior calcaneal tubercle. The posteromedial portal is at the intersection point between the medial border of the Achilles tendon and the line joining the undersurface of the sustentaculum tali and first metatarsal (Table 1).4 A Wissinger rod is inserted into the fibro-osseous orifice of the zone 2 FHL tendon sheath through the posteromedial portal under arthroscopic guidance. The rod passes through the zone 2 tendon sheath under the sustentaculum tali and penetrates the plantar aponeurosis. To facilitate the subsequent release of the master knot of Henry, the aponeurosis should be penetrated at a point distal to the level of the navicular bone.2 The passage of the rod should be smooth and without any resistance until it reaches the plantar aponeurosis.
Table 1.
Pearls for Endoscopic Release of Master Knot of Henry
| The posteromedial portal should be in line with the plantar surfaces of the sustentaculum tali and the first metatarsal. |
| The plantar portal should be distal to the navicular bone. |
| The major risks of the described procedure are injury to the tibial nerve at the tarsal tunnel and injury to the medial plantar nerve at the sole. |
| The ankle should not be in a position of dorsiflexion during the procedure. |
| To minimize the risk of injury to the medial plantar nerve, the release of the master knot of Henry should be performed under clear arthroscopic visualization and the suction should be kept to a minimum. |
The plantar portal incision is made at the tip of the rod (Fig 1). The arthroscopic cannula is inserted along the rod. The rod is removed, and a 4.0-mm 30° arthroscope (Dyonics; Smith & Nephew, Andover, MA) is inserted through the cannula. An arthroscopic shaver (Smith & Nephew) or arthroscopic punch (Acufex; Smith & Nephew) is inserted to reach the master knot of Henry through the plantar portal under arthroscopic guidance. The shaver passes through the flexor digitorum brevis muscle and fascial layer deep to the muscle before the master knot of Henry is reached (Fig 2). The fibrous tissue at the master knot of Henry is resected (Fig 3) until there are no more adhesions between the FHL and flexor digitorum longus tendons and independent gliding of the FHL and flexor digitorum longus tendons can be shown by moving the great toe and little toe (Fig 4). To avoid damage to the medial plantar nerve, the resection should be performed under clear arthroscopic visualization and the suction should be kept to a minimum (Video 1).
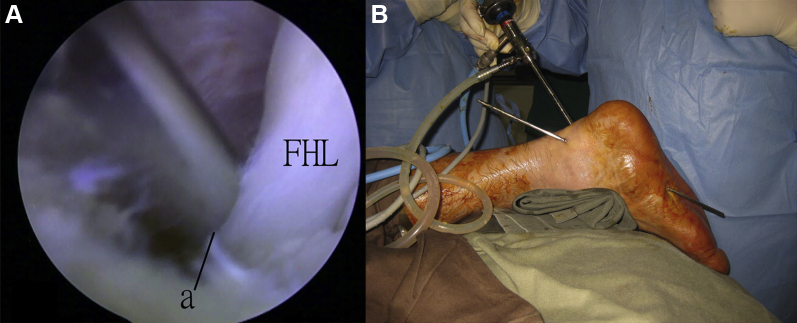
Fig 1.
Zone 1 flexor hallucis longus (FHL) tendoscopy of the right foot. The patient is in the prone position. (A) A Wissinger rod is inserted through the posteromedial portal into the orifice (a) of the zone 2 FHL tendon sheath under arthroscopic guidance. (B) The rod passes through the zone 2 FHL tendon sheath under the sustentaculum tali and penetrates the plantar aponeurosis distal to the navicular bone. The plantar portal incision is made at this point.
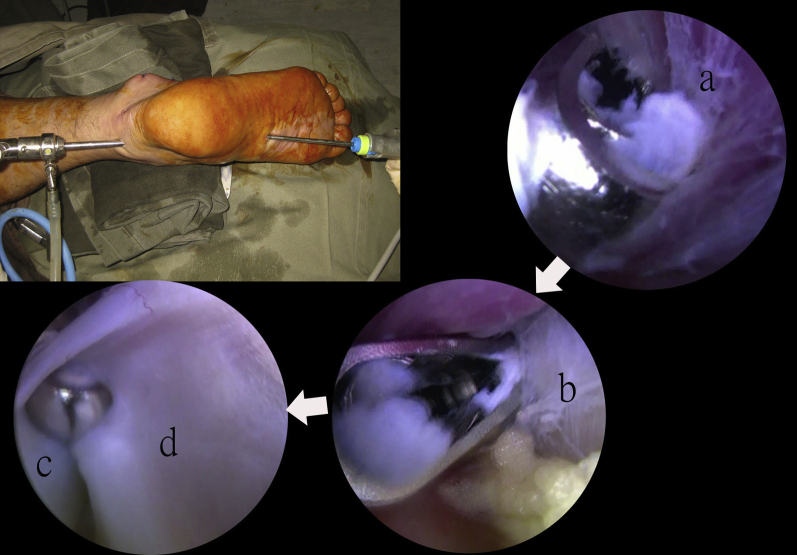
Fig 2.
Zone 2 flexor hallucis longus tendoscopy of the right foot. The patient is in the prone position. The arthroscopic shaver is inserted through the plantar portal and passes through the flexor digitorum brevis muscle (a) and the fascial layer deep to the muscle (b) before the master knot of Henry. Fibrosis between the flexor hallucis longus tendon (c) and the flexor digitorum longus tendon (d) is seen.
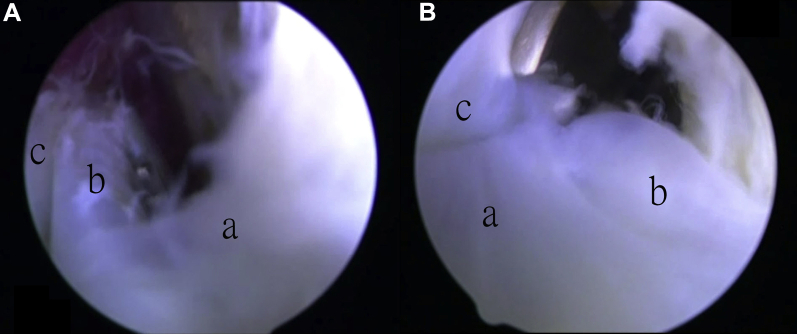
Fig 3.
Zone 2 flexor hallucis longus tendoscopy of the right foot. The patient is in the prone position. The posteromedial portal is the viewing portal. (A) The arthroscopic shaver or (B) the arthroscopic scissors is inserted through the plantar portal to resect the scar tissue (a) around the flexor hallucis longus tendon (b) and the flexor digitorum longus tendon (c) at the master knot of Henry.
Fig 4.
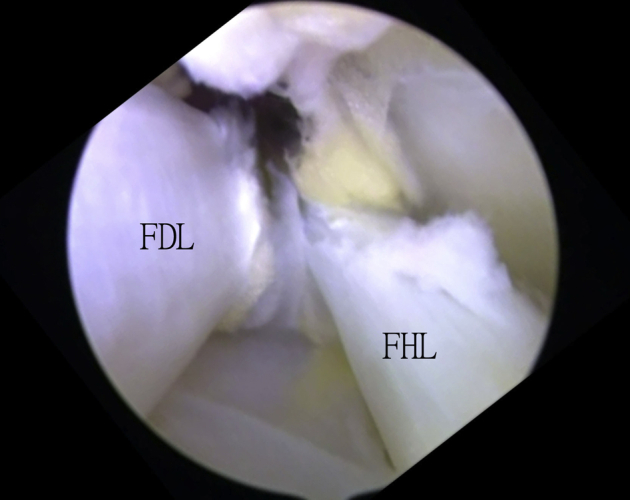
Zone 2 flexor hallucis longus (FHL) tendoscopy of the right foot. The patient is in the prone position. The posteromedial portal is the viewing portal. The FHL and flexor digitorum longus (FDL) tendons can be clearly seen after resection of the scar tissue at the master knot of Henry.
Discussion
“Intersection syndrome” of the foot implies extensive post-traumatic fibrosis of the master knot of Henry.2 It may be the healing phase of a partial tear of the FHL at the knot of Henry.2 Clinically, it can mimic trigger hallux with stenosing tenosynovitis behind the ankle.2, 7, 8, 9 There may be posteromedial ankle pain due to referral pain from irritation of the medial plantar nerve by the fibrotic master knot of Henry. Local pain and tenderness at the knot may or may not be present depending on whether synovitis is present at the knot.1, 2 Preoperative ultrasound and magnetic resonance imaging studies are not sensitive enough to detect this pathology.1, 2 FHL tendoscopy is a useful diagnostic and therapeutic tool. It has the advantages of less surgical trauma and the potential for less chance of recurrence. Stenosing tenosynovitis of the FHL tendon behind the ankle can be excluded by zone 1 FHL tendoscopy. The plantar portal in zone 2 FHL tendoscopy is usually located at the level of the talonavicular joint. The portal tract between the dorsomedial and plantar portals will then be proximal to the master knot of Henry. To approach the knot, the plantar portal should be made distal to the level of the navicular bone.
The described procedure is technically demanding and should be reserved for experienced foot and ankle arthroscopists. The major complications of this procedure are injury to the medial plantar nerve because it is close to the master knot of Henry and injury to the lateral plantar nerve because it can be compressed by the shaft of the arthroscope when it goes into the zone 2 FHL tendon sheath through the posteromedial portal.3, 5, 10 To avoid injury to the medial plantar nerve, the Wissinger rod should be inserted gently and resistance should not be encountered before the plantar aponeurosis is reached. Moreover, the debridement at the master knot of Henry should be performed under clear arthroscopic visualization and the suction should be kept to a minimum. Finally, the ankle should not be in a position of dorsiflexion during the procedure. Otherwise, the neurovascular bundle at the tarsal tunnel will tense up and compress on the shaft of the arthroscope.10
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Endoscopic release of master knot of Henry in right foot. The arthroscopic shaver or arthroscopic punch is introduced through the plantar portal under arthroscopic guidance. The instrument passes through the flexor digitorum brevis muscle and the fascial layer deep to the muscle before the master knot of Henry is reached. The fibrous adhesions between the flexor hallucis longus and flexor digitorum longus tendons are released until free independent motion of the tendons is observed. To minimize the risk of injury to the medial plantar nerve, the debridement should be performed under clear arthroscopic visualization and the suction should be kept to a minimum.
References
- 1.Boruta P.M., Beauperthuy G.D. Partial tear of the flexor hallucis longus at the knot of Henry: Presentation of three cases. Foot Ankle Int. 1997;18:243–246. doi: 10.1177/107110079701800411. [DOI] [PubMed] [Google Scholar]
- 2.Lui T.H., Chow F.Y. “Intersection syndrome” of the foot: Treated by endoscopic release of master knot of Henry. Knee Surg Sports Traumatol Arthrosc. 2011;19:850–852. doi: 10.1007/s00167-010-1394-8. [DOI] [PubMed] [Google Scholar]
- 3.Lui T.H., Chan K.B., Chan L.K. Zone 2 flexor hallucis longus tendoscopy: A cadaveric study. Foot Ankle Int. 2009;30:447–451. doi: 10.3113/FAI-2009-0447. [DOI] [PubMed] [Google Scholar]
- 4.Lui T.H. Flexor hallucis longus tendoscopy: A technical note. Knee Surg Sports Traumatol Arthrosc. 2009;17:107–110. doi: 10.1007/s00167-008-0623-x. [DOI] [PubMed] [Google Scholar]
- 5.Lui T.H., Chan K.B., Chan L.K. Cadaveric study of zone 2 flexor hallucis longus tendon sheath. Arthroscopy. 2010;26:808–812. doi: 10.1016/j.arthro.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 6.van Dijk C.N., Scholten P.E., Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871–876. doi: 10.1053/jars.2000.19430. [DOI] [PubMed] [Google Scholar]
- 7.Andersen L.I., Hvid I. Bilateral hallux saltans. Report of a case. Acta Orthop Scand. 1979;50:599–600. doi: 10.3109/17453677908989810. [DOI] [PubMed] [Google Scholar]
- 8.Lereim P. Trigger toe in classical-ballet dancers. Arch Orthop Trauma Surg. 1985;104:325–326. doi: 10.1007/BF00435951. [DOI] [PubMed] [Google Scholar]
- 9.Newman N.M., Fowles J.V. A case of “trigger toe.”. Can J Surg. 1984;27:378–379. [PubMed] [Google Scholar]
- 10.Lui T.H. Lateral plantar nerve neuropraxia after FHL tendoscopy: Case report and anatomic evaluation. Foot Ankle Int. 2010;31:828–831. doi: 10.3113/FAI.2010.0828. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic release of master knot of Henry in right foot. The arthroscopic shaver or arthroscopic punch is introduced through the plantar portal under arthroscopic guidance. The instrument passes through the flexor digitorum brevis muscle and the fascial layer deep to the muscle before the master knot of Henry is reached. The fibrous adhesions between the flexor hallucis longus and flexor digitorum longus tendons are released until free independent motion of the tendons is observed. To minimize the risk of injury to the medial plantar nerve, the debridement should be performed under clear arthroscopic visualization and the suction should be kept to a minimum.