Abstract
Arthroscopic reduction and internal fixation of glenoid fractures have been well described, especially for glenoid rim (Bankart) fractures, as well as for scapular body fractures with extensions into the articular surface. This approach has the advantage of decreasing comorbidities associated with a standard open approach, but it can be technically challenging and may not be amenable to all fracture patterns. Arthroscopic fixation of scapular fractures incorporating a transverse pattern along the inferior aspect of the glenoid is particularly challenging because of difficulty in accessing this space. We detail the use of a posteroinferior arthroscopic portal for fracture reduction and hardware placement in a scapular fracture with inferior glenoid involvement.
Scapular body fractures with extension into the glenoid articular surface are relatively uncommon injuries but can be challenging to treat. Typically, extra-articular scapular body fractures can be managed nonoperatively, but those patterns with extension into the glenoid articular surface often require operative intervention. Ideberg et al.1 provided a classification system for these intra-articular fracture patterns, with subsequent modification,2 that has been useful in determining treatment. In the past, these fracture patterns were treated exclusively through an open Judet approach.3 Although Cole and colleagues3, 4 have described modifications to the original Judet technique that have minimized soft-tissue trauma, the technique still requires significant soft-tissue dissection, risks injury to the neurovascular structures (particularly the suprascapular nerve), has the potential for postoperative weakness and stiffness, and does not allow full direct visualization of the articular surface of the glenoid.
Treatment of scapular fractures through arthroscopic techniques mitigates some of the risks seen with the open approach and may be more appropriate in elderly patients or in patients with multiple medical comorbidities. Arthroscopic treatment for glenoid fractures was first described for an Ideberg type I pattern, or a fracture of the anteroinferior glenoid.5 Subsequent reports have been published on arthroscopic treatment of Ideberg type III patterns, characterized by a transverse fracture line that separates the upper one-third to one-half of the glenoid fossa and the coracoid from the rest of the scapula, with superior-to-inferior screw fixation.6, 7 We describe arthroscopic surgical fixation of an Ideberg type V variant fracture pattern (Fig 1, Video 1). This pattern requires the use of a posteroinferior portal to properly reduce and fixate the inferior-based glenoid fracture component.
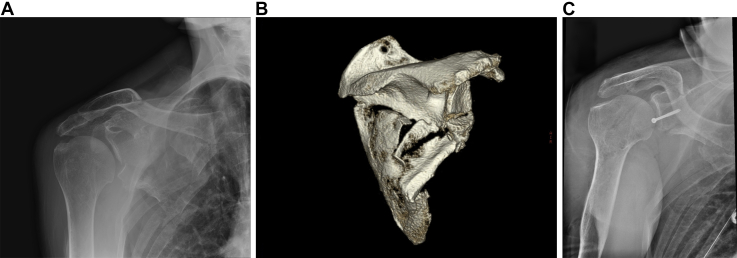
Fig 1.
Preoperative plain radiograph (A) and 3-dimensional reconstruction (B) of a right shoulder and scapula showing an Ideberg type V variant scapular fracture with intra-articular glenoid extension. (C) Postoperative radiograph showing screw placement and reduction of the articular surface.
Technique
Preoperative workup is imperative for patients with scapular fractures because these injuries are often associated with high-energy trauma and associated injuries. Plain radiographs serve as the initial imaging modality (Fig 1A), with computed tomography and 3-dimensional reconstructions serving to better define the fracture pattern (Fig 1B). Table 1 provides a stepwise sequential progression of our technique, and Table 2 lists potential pitfalls and keys to success.
Table 1.
Stepwise Technique Overview
| Preoperative |
| 3D CT reconstruction with humeral head subtraction |
| Medical stabilization/optimization |
| OR setup |
| Lateral decubitus position |
| Acquisition of fluoroscopic image before preparation and draping |
| Intraoperative assessment |
| Establishment of standard posterior viewing and anterior working portals |
| Diagnostic arthroscopy completion |
| Establishment of accessory posteroinferior (7-o'clock) portal and placement of cannula |
| Proper trajectory ensured using spinal needle |
| Fracture hematoma debridement and fracture mobilization |
| Provisional fracture reduction using probe |
| Guidewire placement through fragment into fracture site |
| Additional reduction using guidewire as joystick |
| Passage of guidewire into far cortex |
| Second guidewire placement outside of cannula for rotational stability |
| Cannulated screw placement |
| Assessment of fracture reduction |
| Postoperative management |
| Non–weight bearing |
| Sling use for comfort initially; progression to active ROM as tolerated |
| Resistance exercises at 6 wk postoperatively |
CT, computed tomography; OR, operating room; ROM, range of motion; 3D, 3-dimensional.
Table 2.
Potential Pitfalls and Keys to Success
| Access |
| Lateral decubitus positioning facilitates access to the posterior and inferior glenoid. |
| A long cannula is used in the posteroinferior portal to allow access for instrumentation and prevent soft-tissue interposition when one is placing fixation. |
| Misaligned trajectory of posteroinferior portal |
| A spinal needle is used to localize the posteroinferior portal to ensure the proper trajectory of the screw. |
| Inappropriate fracture mobilization |
| A Bankart elevator may be used; it will provide a broader surface than a probe and reduce the risk of fragment comminution. |
| The fracture fragment may be subducted beneath the superior intact glenoid. |
| Labral debridement may be needed to reduce “tethers” to mobilization. |
| Screw placement |
| Some cannulated screw systems may not have adequate length for complete screw insertion through the posteroinferior portal. |
| A long non-cannulated screwdriver should be available for use after initial placement of the screw with the cannulated screwdriver. |
A team most familiar with shoulder arthroscopy is beneficial in performing this type of procedure. We recommend the use of regional anesthesia, if available, in this case an indwelling interscalene catheter, to help minimize anesthetic use from general anesthesia during the case, as well as to provide postoperative pain control. The patient is placed in the lateral decubitus position using a beanbag (Universal Medical, Norwood, MD) with anterior and posterior positioners (Stulberg Hip Positioners; Innomed, Savannah, GA) as adjunctive stabilization. The operative extremity is held in position with the use of a standard traction device (Arthrex, Naples, FL) used for shoulder arthroscopy in the lateral position. The lateral position, in our experience, facilitates access to the inferior and posteroinferior aspects of the glenoid, which is required in the treatment of the Ideberg type V fracture pattern. Before preparation and draping, the C-arm should be placed superior to the head of the patient and placed in full “orbit” such that the receiver lies near the patient's face and the source is at the ventral aspect of the patient. This will allow the surgeon to bring the machine directly distal to obtain appropriate intraoperative fluoroscopic views.
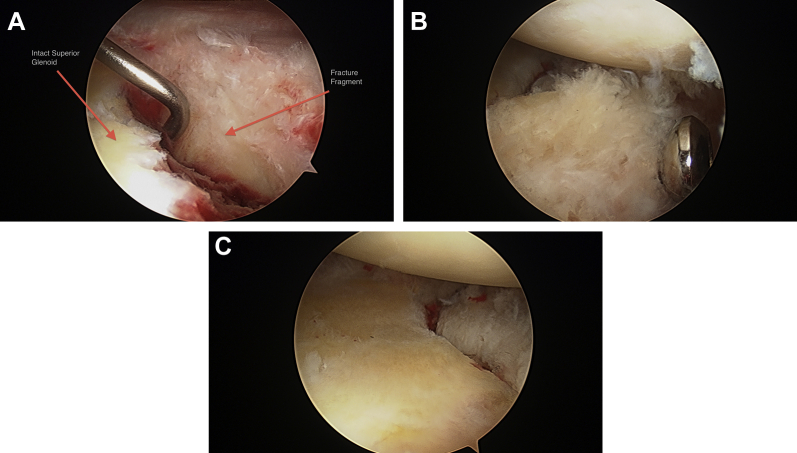
A standard posterior portal is made for introduction of the arthroscope into the joint. By use of an outside-in technique with a spinal needle, an anterior working portal is established within the rotator interval. In contrast to fixation of Ideberg type III fractures, it is not necessary to remove rotator interval tissue for adequate visualization. A diagnostic arthroscopy is carried out in standard fashion after fracture hematoma is removed from the intra-articular space. The primary goal of the procedure is to obtain anatomic reduction and secure fixation of the glenoid fracture fragment, but other interventions (labral or rotator cuff debridement) may be carried out at this time. An arthroscopic shaver (Stryker, Kalamazoo, MI) is used to remove hematoma from the fracture site so that the fracture pattern and orientation can be confirmed. These fracture patterns typically involve the inferior one-third to one-half of the glenoid, and most commonly, the fracture fragment is rotated such that the articular surface is facing superiorly (Fig 2A). Identification of the labrum at the periphery of the fragment helps to define the borders of the involved piece.
Fig 2.
Intraoperative images from the posterior portal of a right shoulder with the patient in the lateral decubitus position showing the large inferior glenoid fracture and articular step-off (A), the final location of the screw off of the articular service (B), and reduction of the fragment with restoration of the articular surface (C).
A probe is then used to assess fracture mobility. In delayed cases, use of a Bankart elevator provides a more broad and stout instrument with which to manipulate the fragment (Video 1). Often, the inferior fracture fragment is partially subducted underneath the intact superior glenoid and requires distal manipulation for full release. In addition, a portion of the intact labrum may need to be debrided to allow for complete visualization, mobilization, and reduction of the fracture fragment. A posteroinferior portal at the 7-o'clock position, approximately 2 to 3 cm inferior and distal to the standard posterior viewing portal,8 can be helpful for fracture release and manipulation and will be needed for hardware insertion later in the procedure. This posteroinferior portal is localized using a spinal needle to assess the position and trajectory in planning for screw fixation through this portal. Although percutaneous fixation is possible, we recommend placement of a cannula (8.25 mm × 9 cm; Arthrex) in this location to facilitate access and visualization to this area of the glenoid and reduce the chance of soft-tissue interposition between the screw and fracture fragment.
Once adequate mobilization of the fracture fragment is achieved, a probe is placed through the anterior portal into the fracture site, reducing the fragment into position. A non-threaded cannulated screw guidewire (4.0-mm partially threaded cannulated screw; Synthes, West Chester, PA) is then placed through the posteroinferior cannula and passed through this piece so that it just enters into the fracture site. It is important to place the guide pin away from the articular margin to prevent the screw head from abrading the humeral head articular cartilage. The arthroscopic probe is then placed beneath the tip of the wire, using the wire as a manual reduction tool to further manipulate the fracture fragment into position. The guidewire is advanced in a posteroinferior-to-anterosuperior direction into the superior glenoid cortex. The provisional reduction is then assessed, and if adequate, a second guidewire is placed outside, but just adjacent to, the cannula to prevent fracture displacement when placing the screw. The guidewire exiting the cannula is measured to determine the appropriate screw length before a 2.7-mm cannulated drill bit is used to drill the outer cortex of the fracture fragment only. The screw length is selected based on the measured guidewire length and is shortened by 2 mm to prevent screw penetration through the far cortex. During screw placement, compression of the inferior fracture fragment against the intact superior glenoid can be noted and maintenance of reduction can be visually confirmed (Fig 2C). Intraoperative fluoroscopy is used to assess screw placement and length, as well as fracture reduction. The guide pins are then removed. In most instances, the fracture fragment will not be large enough to accommodate more than 1 screw; however, in our experience fixation is secure, and success in the treatment of type III fractures with a single screw has been reported (Fig 2B). The incisions are closed in standard fashion, and a simple shoulder sling is placed for postoperative use.
Discussion
Fractures of the scapula that involve the glenoid can be treated both in an open manner and arthroscopically. Although it is now commonplace for Ideberg type I fractures (bony Bankart–type injuries) to be treated arthroscopically,5 minimally invasive treatment has only recently been described for Ideberg type III fracture patterns.6, 7 Yang et al.7 reported excellent outcomes at 2 years' follow-up in 18 patients with Ideberg type III fracture patterns treated by an arthroscopic technique.
Arthroscopic treatment of more involved fracture patterns, such as the Ideberg type V variant with an inferior glenoid fragment, as described in this report, has not previously been reported and requires a different surgical approach. One must realize that arthroscopic treatment of this type of scapular fracture addresses only the glenoid articular surface and not the scapular body, which may or may not have significant displacement. We believe, however, that restoration of the articular surface is the primary goal of this type of procedure because non-articular scapular body fractures are most commonly treated nonoperatively. Although this approach does not address concomitant scapular body fractures that may be present, it avoids a larger open incision and its comorbidities and gives direct visualization of the articular surface and reduction through the arthroscope.
Although not amenable to all fracture patterns, arthroscopic fixation of a large inferior glenoid fracture as shown in this case is safe and reproducible using the described technique, specifically with the use of a posteroinferior arthroscopic portal technique and inferior-to-superior screw trajectory. The posteroinferior portal for shoulder arthroscopy has been shown to be safe and effective for accessing the inferior aspect of the glenohumeral joint in cadaveric models, with mean distances of 39 ± 4 mm from the circumflex artery and 29 ± 3 mm from the axillary nerve and suprascapular nerve.8 The lateral decubitus position facilitates improved visualization and workflow through this portal. It is important to localize the posteroinferior portal with the use of a spinal needle, ensuring that the needle is oriented to allow for the proper screw trajectory. It is critical to obtain full fracture mobilization before attempted reduction, and the use of a Bankart elevator may be helpful in these instances. In cases in which the labrum is intact, labral debridement can also facilitate visualization and mobilization of the fragment.
We found the technique of advancing the guidewire such that it just enters the fracture site and then using a probe to lift up on the wire, essentially joy-sticking the fragment into the correct position, to be very effective. Using a second wire (outside of but parallel to the cannula) for rotational control prevented rotation of the fragment during screw insertion. Regarding instrumentation, it is necessary to use a long guidewire and cannulated screwdriver for screw insertion. This is particularly relevant when a long cannula (≥9 cm) is used in the posteroinferior portal in more muscular individuals. Some of the standard cannulated screw systems may not accommodate this length, and we experienced this with the Synthes 4.0-mm cannulated screw used for this case. If this occurs, the surgeon may use a cannulated screwdriver to partially insert the screw into the bone and then switch to a non-cannulated screwdriver after initial screw purchase in the superior intact glenoid. The choice of short versus long threaded screws will depend on the fragment size, but a transverse inferior-third fragment should allow for a long partially threaded screw to be used to optimize fixation strength.
Long-term outcome data on arthroscopic fixation of the Ideberg V variant scapular fracture described in this report are nonexistent. We believe that specific fracture patterns enable the use of a posteroinferior portal for arthroscopic fixation of glenoid fractures, decreasing many of the morbidities associated with a traditional open approach for these complex scapular fractures.
Footnotes
The authors report the following potential conflict of interest or source of funding: J.A.B. receives support from Synthes and Innomed. G.D.A. receives support from Cytonics.
Supplementary Data
Case presentation of arthroscopic fixation of an Ideberg type V variant fracture pattern using a posteroinferior portal. Viewing is performed through a standard posterior portal with the patient in the lateral decubitus position. A posteroinferior portal is created by an outside-in technique, and an 8.25-mm × 9-cm cannula is placed. Reduction is achieved with a probe and Bankart elevator, and fixation is achieved with a 4.0-mm partially threaded cannulated screw.
References
- 1.Ideberg R., Grevsten S., Larsson S. Epidemiology of scapular fractures. Incidence and classification of 338 fractures. Acta Orthop Scand. 1995;66:395–397. doi: 10.3109/17453679508995571. [DOI] [PubMed] [Google Scholar]
- 2.Mayo K.A., Benirschke S.K., Mast J.W. Displaced fractures of the glenoid fossa. Results of open reduction and internal fixation. Clin Orthop Relat Res. 1998:122–130. [PubMed] [Google Scholar]
- 3.Cole P.A., Dubin J.R., Freeman G. Operative techniques in the management of scapular fractures. Orthop Clin North Am. 2013;44:331–343. doi: 10.1016/j.ocl.2013.04.001. (viii) [DOI] [PubMed] [Google Scholar]
- 4.Anavian J., Gauger E.M., Schroder L.K., Wijdicks C.A., Cole P.A. Surgical and functional outcomes after operative management of complex and displaced intra-articular glenoid fractures. J Bone Joint Surg Am. 2012;94:645–653. doi: 10.2106/JBJS.J.00896. [DOI] [PubMed] [Google Scholar]
- 5.Cameron S.E. Arthroscopic reduction and internal fixation of an anterior glenoid fracture. Arthroscopy. 1998;14:743–746. doi: 10.1016/s0749-8063(98)70102-1. [DOI] [PubMed] [Google Scholar]
- 6.Tao M.A., Garrigues G.E. Arthroscopic-assisted fixation of Ideberg type III glenoid fractures. Arthrosc Tech. 2015;4:e119–e125. doi: 10.1016/j.eats.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang H.B., Wang D., He X.J. Arthroscopic-assisted reduction and percutaneous cannulated screw fixation for Ideberg type III glenoid fractures: A minimum 2-year follow-up of 18 cases. Am J Sports Med. 2011;39:1923–1928. doi: 10.1177/0363546511408873. [DOI] [PubMed] [Google Scholar]
- 8.Davidson P.A., Rivenburgh D.W. The 7-o’clock posteroinferior portal for shoulder arthroscopy. Am J Sports Med. 2002;30:693–696. doi: 10.1177/03635465020300051101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Case presentation of arthroscopic fixation of an Ideberg type V variant fracture pattern using a posteroinferior portal. Viewing is performed through a standard posterior portal with the patient in the lateral decubitus position. A posteroinferior portal is created by an outside-in technique, and an 8.25-mm × 9-cm cannula is placed. Reduction is achieved with a probe and Bankart elevator, and fixation is achieved with a 4.0-mm partially threaded cannulated screw.