ABSTRACT
Background
The incidence of patellar subluxation or dislocation has been documented up to 43/100,000 with females more prevalent then males. There are many contributing factors involving the hip, knee, and ankle that lead to patellar subluxation. A patellar position of lateral tilt with lateral glide may indicate weakness of the vastus medialis oblique (VMO) and adductors, increased tightness in the iliotibial band, and overpowering of the vastus lateralis. Patella alta can predispose an individual to lateral dislocation due to the patella placement outside of the femoral trochlear groove with a disadvantage of boney stability. Other factors that may cause the patella to laterally sublux or dislocate during a functional activity or sporting activity include a position of femoral external rotation, tibial internal rotation, and excessive contraction of the vastus lateralis. The medial patellofemoral ligament (MPFL) aids in the prevention of a lateral patellar subluxation or dislocation. In cases where there is recurrent subluxation/dislocation and Magnetic Resonance Imaging confirms a MPFL tear, a reconstruction may be the treatment of choice.
Purpose
The purpose of this case series is to describe the post-surgical physical therapy management of MPFL reconstructions, outcomes using the Modified Cincinnati Knee Outcome Measure (MCKOM) and to propose staged physical therapy interventions for this pathology in the form of a treatment progression.
Methods
Post-operative management data and outcomes were retrospectively collected using a detailed chart review methodology from seven subjects who underwent MPFL reconstruction.
Findings
The Modified Cincinnati Knee Outcome Measure (MCKOM) was analyzed for each participant in four sections that were most important to the return and maintenance of participation in sport. At follow-up the mean scores for the seven subjects in Section 3 (instability) was 19.3/20, Section 4 (overall activity level) was 17.3/20, Section 7 (running activity) was 4.5/5, and Section 8 (jumping and twisting) was 4.3/5. Overall all subjects scored over an 80 which indicated excellent results for return to activity/sport.
Conclusions
In this case series, seven subjects after MPFL reconstruction returned to sport or functional activity following a physical therapy treatment progression including proprioceptive-focused, and dynamic rehabilitation, along with a home exercise program. Based on these positive results and a review of relevant literature regarding MPFL rehabilitation, a rehabilitation progression was presented.
Level of Evidence
Level 4- Case Series
Keywords: Lateral patellar subluxation, medial patellofemoral ligament reconstruction, Modified Cincinnati Knee Outcome Measure
INTRODUCTION
Patellar subluxation or dislocation can lead to recurrent disability, time away from functional activity, and sports participation. The rate of patellar subluxation/dislocation has been documented up to 43/100,000 with reported rates greater in the female population.1,2,3 There are many contributing factors involving the hip, knee, and ankle that may lead to patellar subluxation. A patellar position of lateral tilt with lateral glide may indicate weakness of the vastus medialis oblique (VMO) and adductors, increased tightness in the iliotibial band, and an imbalance of the vastus lateralis over the medialis. Patella alta can predispose an individual to lateral dislocation due to the patella placement superior to the femoral trochlear groove with a subsequent loss of bony stability. Other factors that may cause the patella to laterally sublux or dislocate during a functional activity or sporting activity include a position of femoral external rotation, tibial internal rotation, and excessive contraction of the vastus lateralis.3
The bony contribution to stability comes from the patella being engaged in the track of the trochlea at the distal femur.4,5,6 The lateral trochlea of the femur is elevated with regard to the medial trochlea, in order to help resist lateral forces. Bony stability is most relevant between the ranges of 20 and 60 degrees of knee flexion.4,6,7 In the range of 0-20 degrees, in which the patella dislocates the most, the soft tissue restraints including the medial patellofemoral ligament (MPFL) are responsible for preventing lateral patellar subluxation or dislocation.4 During the 0-20 degree flexion range, the patella is in essence, floating, and not engaged in the bony groove. From 0-20 degrees, the MPFL is the primary ligament that provides 60% restraint to lateral patellar subluxation.4,8 The VMO dynamically aides the static stabilizer: the MPFL. The MPFL is in the second layer on the medial side of the knee, deep and distal to the insertion of the VMO. It originates superior posterior to medial femoral epicondyle, one centimeter distal to the adductor tubercle and close to the distal femoral growth plate. It also houses the adductor magnus, fibers of the medial collateral ligament (MCL), and the posteromedial capsule.8 The MPFL forms an arch with the superficial MCL and inserts laterally on the proximal two thirds of the medial patella. Some of the deep fibers also attach to the VMO.6,9,10
When repeated dislocations occur, the patient is typically sent for Magnetic Resonance Imaging (MRI) assessment. This assessment will determine if the medial patello femoral ligament is torn and if surgery is necessary. Panni et al suggest that MRI is the most accurate way to diagnose MPFL injury and found that a MPFL reconstruction would be more reliable than a repair.11 Smith et al published a meta-analysis regarding the differences in operative and nonoperative management after patellar dislocation. They found that there was a higher rate of recurrent patellar subluxation when dislocations were treated non-operatively.12
Several different surgical procedures have been discussed in the literature. Sampatacos and Getelman described the use of the semitendinosus allograft, the tensile strength of which is just over 200 N.13 The double bundle technique may aid in more completely correcting the original anatomy of the MPFL by decreasing patellar rotation and thereby improving its stability.14 Deie et al concluded that reconstruction of the MPFL using a semitendinosus graft was successful in three children (6-10 years of age) who had experienced repeated subluxation/dislocation. Galeazee and Baker also described good to excellent results in 81% of 53 knees with a recurrence rate of 5%.15 Aulia et al stated that other authors described 62%-82% excellent or good results in over 50 cases, with 8% reporting dislocation.16 They go on to suggest that the procedure can resolve dislocation and provide satisfactory patellofemoral congruence evidenced by a static Computerized Tomography (CT) scan.16
After surgery is performed, physical therapy is indicated. Mikashima et al discussed their post-operative course where patients were placed in a post-surgical knee immobilizer, began quadriceps isometric exercise initiated as tolerated, and passive range of motion (PROM) on day two. Immobilization in full extension continued for three weeks, full weight bearing was initiated at five weeks, jogging and mild sports activity at four months, and full return to sport at six months. The majority of their patients returned to previous sporting level based on their clinical findings.17
Menetrey, Putman, and Gard discussed criteria for return to sport after patellar dislocation or following surgery. Their definition of post operative patient success was when patients experienced no early re-injury, no residual pain, and demonstrated the ability to participate in sport after a five year period. Key factors in their rehabilitation program included clinical examination (assessment of the amount of laxity), strength development, especially the of the quadriceps and gluteus medius, development of neuromuscular control, performance of sport specific drills, and proper counseling between all members of the athlete's team. However, these authors noted that there is limited literature regarding the return to sport after such procedures.18 Therefore, this retrospective descriptive case series will investigate rehabilitation principles for post-surgical physical therapy treatment following MPFL reconstruction after multiple lateral patellar subluxations or dislocations.
The purpose of this case series is to describe the post-surgical physical therapy management of MPFL reconstructions, outcomes using the Modified Cincinnati Knee Outcome Measure (MCKOM), and to propose staged physical therapy interventions for this pathology in the form of a treatment progression. The authors’ hypothesis was that surgical reconstruction of the MPFL and post-operative physical therapy leads to excellent outcomes and safe return to sport or functional activity.
METHODS
Participants
This case series included two male and five female subjects, 14 to 35 years of age. All of the patients underwent MPFL reconstruction using autologous semitendinosus graft due to recurrent dislocation, had failed rehab prior to surgery, and had a confirmed tear of the MPFL on MRI. Subjects were excluded if they had undergone prior patellar surgery for MPFL reconstruction or other patellar realignment procedures.
Seven subjects consented to anonymous utilization of data gleaned from a detailed chart review of their physical therapy care. The subjects in this case series each underwent a MPFL reconstruction with a semitendinosus autograft from the ipsilateral side. IRB approval was granted and the rights of the subjects were protected. After consent to participate and following the completion of physical therapy, they were asked to fill out a Modified Cincinnati Knee Score any time from 28 to 200 weeks after discharge.
Procedure
Data were obtained through a detailed chart review of the subject's physical therapy treatment starting with the initial evaluation, progress notes, reevaluations, and discharges available via the Redoc 7.8 documentation note writing system. The clinical findings of importance were range of motion (ROM), strength, weight bearing status, bracing, and exercise progression which included proprioceptive activity. Other outcomes taken into consideration included timeframes and interventions related to dynamic proprioception, running, plyometrics, sport specific drills, and return to functional activity/sport participation. The physical therapy interventions for each of the subjects were performed by the physical therapy staff. The MCKOM score was used for the follow up outcome measure scores.
RESULTS
Table 1 displays demographics including; diagnosis, age, and gender of the included subjects, spanning 14 to 35 years of age.
Table 1.
Surgical Subjects Demographics
| Diagnosis | Surgical | Age (years) | Gender |
|---|---|---|---|
| MPFL Reconstruction | S1 | 17 | Female |
| MPFL Reconstruction | S2 | 35 | Female |
| MPFL Reconstruction | S3 | 30 | Female |
| MPFL Reconstruction | S4 | 18 | Female |
| MPFL Reconstruction | S5 | 19 | Male |
| MPFL Reconstruction | S6 | 14 | Female |
| MPFL Reconstruction | S7 | 17 | Male |
| Summary | N=7 | Range 14-35 | 5 female/2 male |
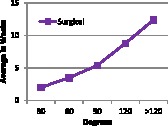
Range of motion achievements are reported in Table 2 and were taken according to methods described by Norkin and White using a Baseline goniometer.19 Mean range of motion achievements for all subjects are displayed in Chart 1.
Table 2.
Surgical Time Line for achievement of Range of Motion in Weeks.
| Surgical | Weeks to Obtain Full Extension |
Progression of Flexion ROM *Weeks from initial surgery date |
||||
|---|---|---|---|---|---|---|
| 30 ° | 60 ° | 90 ° | 120 ° | >120 ° | ||
| S1 | 4 | 4 | 6 | 11 | 13 | |
| S2 | 2 | 2 | 4 | 6 | 9 | 17 |
| S3 | 2 | 2 | 3 | 4 | 9 | 11 |
| S4 | 2 | 2 | 4 | 8 | 10 | 11 |
| S5 | 2 | 2 | 3 | 5 | 15 | |
| S6 | 2 | 2 | 3 | 7 | 9 | 10 |
| S7 | 4 | 3 | 4 | 9 | 10 | |
| Time range (weeks) | 2 | 3-4 | 3-8 | 5-11 | 10-17 | |
| Average (weeks) | 2 | 3.5 | 5.4 | 8.8 | 12.4 | |
Chart 1.
The immobilization and bracing progressions reported in Table 3 were dependent on the allowance of the referring physician.
Table 3.
Surgical Length of Time for Bledsoe to be Unlocked to 30 degrees Weeks from Initial Injury Date
| Surgical | Unlocked Bledsoe (Brace) Surgical |
|---|---|
| S1 | 6 |
| S2 | 3 |
| S3 | 4 |
| S4 | 3 |
| S5 | 3 |
| S6 | 4 |
| S7 | 4 |
| Time range (weeks) | 3-6 |
| Average (weeks) | 7.7 |
The progression of weight bearing status is presented in Table 4, which was based upon physician instruction and patient ability to fully weight bear on the involved extremity without loss of control of the knee during a normal gait pattern. The physicians for each of the surgical cases provided therapists with guidelines for their MPFL patients.20,21
Table 4.
Surgical Weight Bearing Status in Weeks from Surgery to Full Weight Bearing
| Surgical | FWB |
|---|---|
| S1 | 4 |
| S2 | 10 |
| S3 | 6 |
| S4 | 6 |
| S5 | 3 |
| S6 | 6 |
| S7 | 6 |
| Time range (weeks) | 4-10 |
| Average (weeks) | 5.9 |
FWB = full weight bearing
The descriptions regarding non-weight bearing exercises to advanced strengthening program are noted in Table 5 and means for all subjects are presented in Chart 2.
Table 5.
Length of Time for Transition from Table Exercises to Advanced Strengthening Exercises, in Weeks from Surgery
| Surgical | NWB Exercises | Adductor Strengthening | Advanced Strengthening Exercises |
|---|---|---|---|
| S1 | 4 | 4 | 5 |
| S2 | 2 | 3 | 5 |
| S3 | 2 | 5 | 4 |
| S4 | 2 | 7 | 3 |
| S5 | 2 | 3 | 4 |
| S6 | 2 | 4 | 5 |
| S7 | 2 | 4 | 5 |
| Time range (weeks) | 2-4 | 3-4 | 3-5 |
| Average (weeks) | 2.3 | 4.3 | 4.4 |
NWB = non weight bearing,
Table 5.
Exercise Details
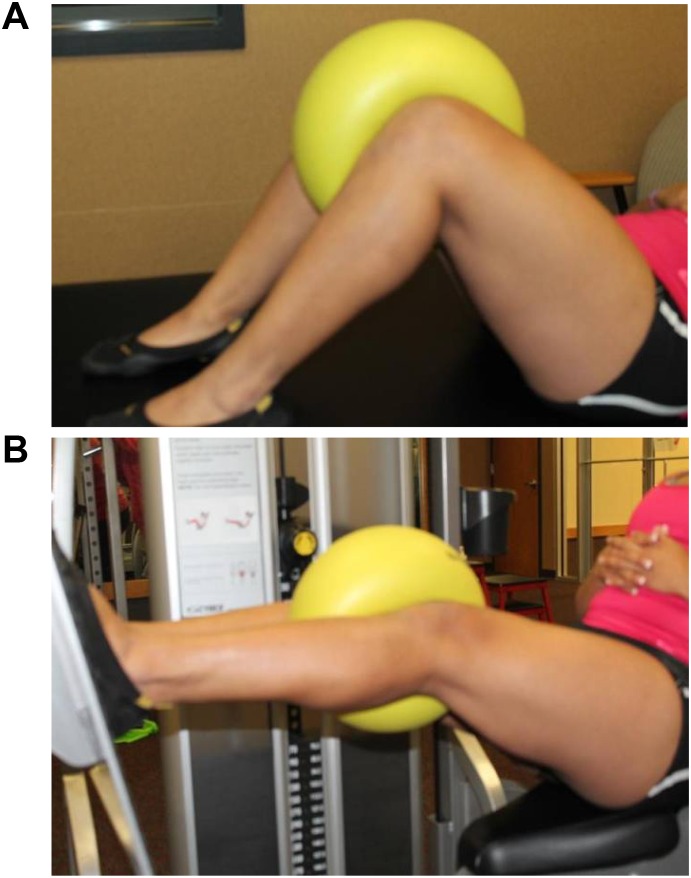
| Non Weight Bearing Exercises | Quad sets, SLR program, multiangle isometrics, modified range active knee extension (Figure 1) |
| Adductor Strengthening | Ball squeeze (Figure 2A), SLR adduction, bridging with ball squeeze |
| Advanced strengthening Exercises | Leg press, bilateral leg press, unilateral leg press, leg press with ball squeeze (Figure 2B), squats, squats with ball squeeze, lunges, step ups, shuttle (bilateral, unilateral, ball squeeze), progression to standing exercises, single leg strengthening progression: standing hip PREs all planes |
| Criteria for Progression | Progressing ROM, decreased edema, minimizing pain, without extensor lag, WBAT to FWB. Improved posture, increased endurance and power. |
Chart 2.
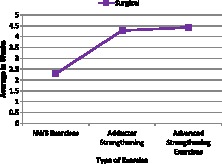
Figure 1.
Straight leg raise (NWB exercise).
Figure 2.
Adductor squeezes (Adductor Strengthening). A. Isometrically in hooklying. B. During leg press.
The timelines for return to sport or functional activity are outlined in Table 6, which lays out the progression from static to dynamic proprioceptive activity, running, plyometrics, sport specific drills, and return to a sport or functional activity.
Table 6.
Timeline for Return to Sport/Full Functional Activity Weeks from Surgery
| Subjects | Surgical | Stage I | Stage II | Stage III | Stage IV | Stage V | Stage VI Sport |
|---|---|---|---|---|---|---|---|
| 1 | S1 | 6 | 9 | 10 | 13 | 14 | 36 Track |
| 2 | S2 | 12 | 16 | 16 | 24 | - | 20 Domestic Engineer |
| 3 | S3 | 8 | 10 | 16 | 19 | 19 | 26 Gym Fitness |
| 4 | S4 | 6 | 6 | Left to Return to School | |||
| 5 | S5 | 6 | 10 | 15 | D/C due to Insurance Denial (Judo) | ||
| 6 | S6 | 10 | 20 | 21 | 19 | 19 | 19 Kickline |
| 7 | S7 | 7 | 16 | 20 | 23* | Cross Training | |
| Time frame (wks) | 6-12 | 6-20 | 10-21 | 13-23 | 14-19 | 19-36 | |
| Average (wks) | 7.85 | 12.4 | 16.3 | 19.6 | 17.3 | 27 | |
= subject dislocated opposite knee during post-rehab during work, therefore unable to progress to next stage until healed and returned from college (130 weeks)
Table 6.
Stage Definitions with Associated Exercises
| Stage I Proprioception | Static wobble board, dynadisc, single leg cone touch (Figure 3), bilateral to unilateral weight bearing (Figure 8) |
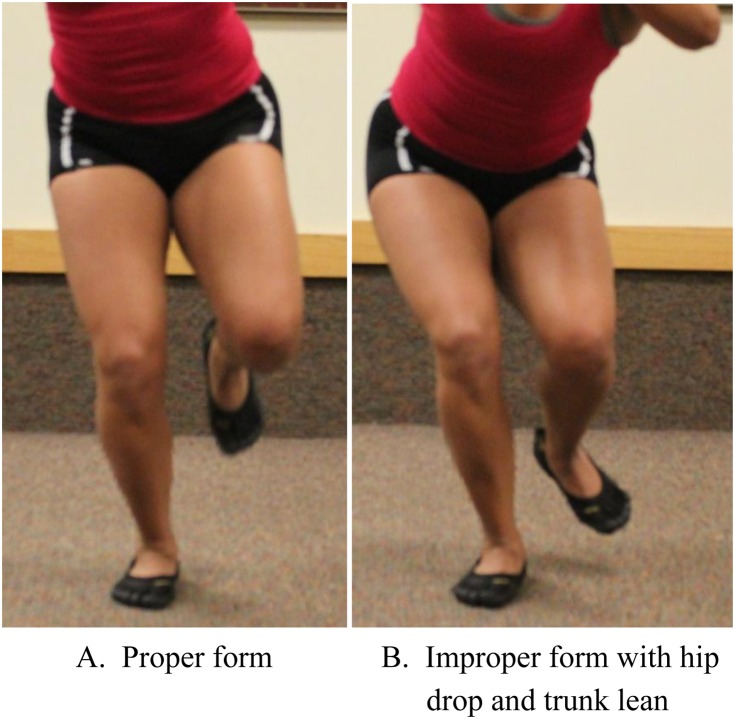
| Stage II Dynamic Proprioceptive: | Agility drills (shuffle, two step with circles), single limb squat, BOSU squats (Figure 4), single hopping in place (Figure 10) |
| Stage III Running | Progress speed as tolerated, cone drills |
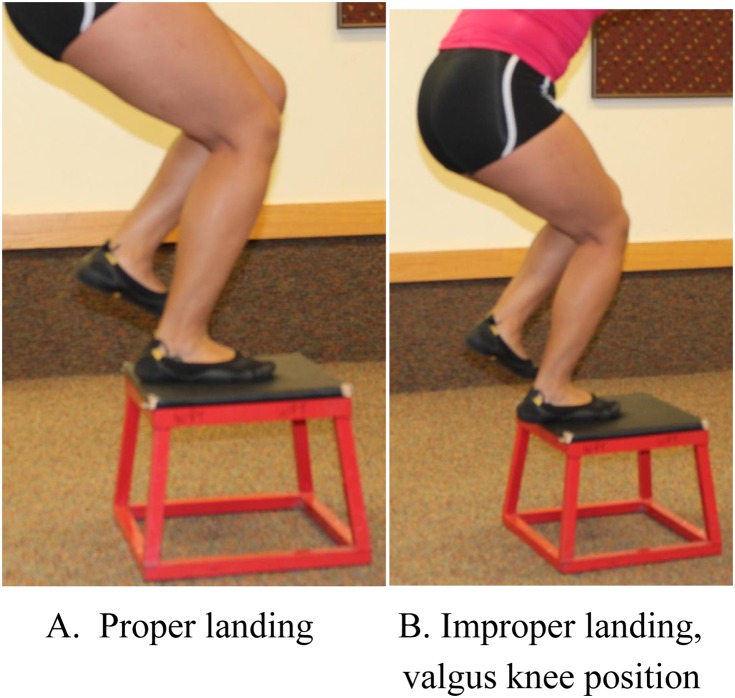
| Stage IV Plyometrics | Jumping boxes (Figure 6), jump and squat, hop and squat, lateral jump, single leg box jump (Figure 9) |
| Stage V Sport Specific Drills | Cutting (Figure 5), pivoting, activity based on sport (Figure 7) |
| Stage VI Return to Sport | Defined as the week that they returned to sport |
Figure 3.
Single Leg Stance with forward cone touch
Figure 4.

Dynamic Proprioception on BOSU™
Figure 5.

Running and cutting drills
Figure 6.
Plyometrics
Figure 7.
Sport Specific drills
Figure 8.
Single Limb Proprioception
Figure 9.
Single leg box jump
Figure 10.
Single leg hop land
The follow up MCKOM scores are displayed in Table 7. The physical therapists progressed each patient's program based on changes in ROM, contraction of the quadriceps muscle, assessment of gliding of the patella superiorly, and the ability to perform a straight leg raise without an extensor lag.22 Previous literature has suggested that the firing of the adductor muscle may aide in the recruitment of the VMO secondary to the MPFL being housed with the adductor muscle in the anatomical second layer of the knee. 23,24 Tables 8, 9, and 10 review the timeline for return running, jumping, and return to sport with the follow up data from the MCKOMS. Participants’ scores on the MCKOM reflect the outcome post rehabilitation in regards to return to function. Participants each returned to their prior sport or activity demands without instability or reoccurrence. Participant S1 returned to track, S2 was a domestic engineer, S3 and S7 returned to fitness that consisted of cross training, endurance training, and weight training, S5 returned to Judo, and S6 returned to kickline. Information for participant S4 was lost to follow up. The comparison between the point at which the participants reached Stage III (running) (Table 9) and his/her function at follow up exemplifies the success of the guideline in returning the participants to prior activity or level of function.
Table 7.
Knee Outcome Measure Scores (MCKOM) Follow up Date
| Subjects | Score Totals (MCKOM) | Follow up Timeline (weeks) |
|---|---|---|
| S1 | 100 | 200 |
| S2 | 90 | 30 |
| S3 | 100 | 28 |
| S4 | ||
| S5 | 100 | 104 |
| S6 | 82 | 70 |
| S7 | 83 | 78 |
Table 8.
Timeline for Return to Running
| Subject Number | Stage III | Follow Up (weeks) MCKOMS Section7 |
|---|---|---|
| S1 | 10 | 200 |
| S2 | 16 | 30 |
| S3 | 16 | 28 |
| S4 | Lost to follow up | Lost to follow up |
| S5 | 15 | 104 |
| S6 | 20 | 70 |
| S7 | 21 | 78 |
Stage III from Table 6
Section 7 on MCKOMS category on running
Table 9.
Timeline for Return to Jumping
| Subject Number | Stage IV | Follow Up (weeks) MCKOMS Section 8 |
|---|---|---|
| S1 | 13 | 200 |
| S2 | 24 | 30 |
| S3 | 19 | 28 |
| S4 | Lost to follow up | Lost to follow up |
| S5 | Not Documented | 104 |
| S6 | 19 | 70 |
| S7 | 23 | 78 |
Stage IV from Table 6
Section 8 on MCKOMS category on jumping and twisting
Table 10.
Timeline Return to Sport
| Subject Number | Stage VI | Follow Up (weeks) MCKOMS Section 4 |
|---|---|---|
| S1 | 36 | 200 |
| S2 | Discharged prior | 30 |
| S3 | 26 | 28 |
| S4 | Lost to follow up | Lost to follow up |
| S5 | Not Documented | 104 |
| S6 | 19 | 70 |
| S7 | Not Documented | 78 |
Stage VI from Table 6
Section 4 on MCKOMS category on return to sport
Modified Cincinatti Knee Outcome Score Definitions
| <30 Poor |
| 30-54 Fair |
| 55-79 Good |
| >80 Excellent |
When assessing the effectiveness of the rehabilitation guideline and return to activity, in Table 11, Sections 3,4,7, and 8 of the MCKOM were analyzed for all participants because each section examines a different facet of activity at follow up. Section 3 considered the participants regarding instability. Eighty-three point three percent of participants that responded answered in the top category (20 points) indicating excellent outcome and the other 16.6% in the very good outcome (16 points) regarding the affected knee giving way at follow up.
Table 11.
Surgical Knee Outcome Measure Scores Breakdown (MCKOM)
| Surgical Knee Outcome Measure Scores | |||||
|---|---|---|---|---|---|
| Section Score Totals | Total Score | ||||
| Sport | 3 | 4 | 7 | 8 | |
| Track | 20 | 20 | 5 | 5 | 100 |
| Domestic Engineer | 20 | 16 | 4 | 4 | 82 |
| Fitness activities: gym | 20 | 20 | 5 | 5 | 100 |
| Lost to Follow Up | |||||
| Judo | 20 | 20 | 5 | 5 | 100 |
| Kickline | 16 | 16 | 4 | 4 | 82 |
| Cross Training | 20 | 12 | 4 | 3 | 83 |
Section 3 = Giving Way
Section 4=Overall Activity Level
Section 7=Running Activity
Section 8=Jumping or Twisting
Section 4 of the MCKOM, considered overall activity level, which is important to compare to the time at which the participants returned to sport/functional activity (Stage VI, seen in Table 6). Participant S1 reached stage VI at week 36 and maintained ability at follow up 200 weeks later. Participant S2 did not reach full function during physical therapy but at week 30 performed her usual functional activity. Participant S3 reached Stage III-return to running, at week 16 and maintained until week 28. Participant S5 reached Stage VI at week 26 and maintained function at week 104 follow up. Participant S6 reached Stage VI at week 19 and continued thru week 70. Participant S7 reported back to training at at week 78 (Table 10). For Section 4 regarding overall activity level, 50% answered in the top category indicating and excellent score (20 points) and 33.3% responded with a very good outcome answer (16 points) (Table 11). Sections 7 (running activity) and 8 (jumping or twisting) were also considered for each participant individually due to the importance of both in consideration of ability for return to full functional activity.
Table 8 coincides with Stage III. running. Refer to Table 8 for time in weeks participants returned to Stage III and continued with follow up. For Section 7 of MCKOMS, 50% of participants answered in the top category indicating an excellent outcome (5 points) and the other 50% responded with a very good outcome (4 points). (Table 11).
Table 9 coincides with Stage IV-return to jumping jumping twisting activity. Refer to Table 9 for time in weeks participants returned to Stage IV. For Section 8 of the MCKOMS, return to jumping/ twisting activity, 50% of participants answered in the top category indicating an excellent score (5 points), 33.3% of participants answered with a very good outcome (4 points) and 17% responded with a fair outcome (3 points). (Table 11).
Of note, participants S2, S4, S5, and S7 did not reach Stage VI during their course of physical therapy.
Appendix 1 provides the authors' suggestions on a detailed rehabilitation program and timeline to return to sport or functional activity based on this case series.
DISCUSSION
The purpose of this case series is to describe the post-surgical physical therapy management of MPFL reconstructions, outcomes using the Modified Cincinnati Knee Outcome Measure (MCKOM) and to propose staged physical therapy interventions for this pathology in the form of a treatment progression. The authors’ hypothesis was that surgical reconstruction of the MPFL and post-operative physical therapy leads to excellent outcomes and safe return to sport or functional activity.
Seven subjects who had sustained repeated lateral patellar subluxations, failed previous conservative physical therapy, and underwent the MPFL reconstruction were considered for this study. All subjects were treated using a semitendinosus autograft. Ladenhauf, Berker, and stated that the “graft length is estimated by measuring the distance of the medial border of the reduced patella to the femoral insertion site, adding a total of 25 to 30 mm of length to allow the graft to be fixed within the bony sockets at each end.”10 This is very important during rehabilitation because the femoral insertion site is near the adductor tubercle and is tensioned at 30 degrees of knee flexion. For patients with an open growth plate, a guide wire was placed distal to the femoral growth plate.16 The range between 20 and 30 degrees of knee flexion is where the graft receives its tension so that the patella engages correctly in the trochlear sulcus. 15,24,27 A double limb graft is used9 and two tenodesis screws fixate it to the patella with the knee in 30 degrees of flexion, attempting to decrease risk of disturbance to the growth plate. 5,10,16 Due to the complexity of the surgery and the fixation, the surgeons supplied the therapist with guidelines for physical therapy. 20,21 Individualized alterations in progression of physical therapy care occurred based on the patient's response to surgery and the judgment of the physical therapist.
The progression of flexion ROM from 30 to 60 degrees took three to four weeks. For greater than 120 degrees of flexion to be achieved, 10 to 17 weeks was required. Difficulty in obtaining flexion appeared related to pain secondary to the surgery. The pain was reported in the posterior medial aspect of the knee, occurring especially during flexion. This finding was noted by Shah and Howard et al who discussed that the drilling of the adductor tubercle and harvesting the medial hamstring graft could lead to pain during knee flexion. They showed that 13.4 % of their patients had this potential complication after MPFL surgery. All of the patients in their study had full knee extension.6 Six subjects in this case series demonstrated full extension on their first visit and by the second visit the last subject gained full extension (Table 2). Due to the ability of subjects to obtain full extension and the surgical procedure to stabilize the instability of the patella, the treating therapists did not elect to perform any passive patellar mobilization. The isometric quadriceps set was chosen to provide a superior glide of the patella, in order to promote engagement in the trochlear groove and assist in controlling the knee during gait to prevent buckling.22 To this end, quadriceps strengthening began on the first visit with quadriceps isometrics and a progression of straight leg raises. The authors felt that the firing of the adductor muscle would aide in the recruitment of the VMO.10,25 Overall control of the lower extremity was considered in closed chain exercise positions for static and dynamic propioception with a progression to running, plyometrics, and sport specific drills.18
The Bledsoe hinged knee brace was used on all patients post-operatively, initially locked in full extension, and unlocked between three weeks and six weeks post-operatively. Clinically, patients may complain of pain along the medial aspect of the knee due to the graft harvest and the surgical procedure. Therefore, caution should be used with the tightness of the medial strap of the hinged brace. The surgical procedure caused post op edema, which likely contributed to muscular inhibition of the quadriceps. With an inhibited quadriceps muscle group, the bracing was initially required to allow the patient to ambulate. The physical therapists progressed ambulation based upon physicians recommendations, ensuring appropriate changes in ROM, decreased edema, contraction of the quadriceps muscle, improved active superior gliding of the patella, and the ability to perform a straight leg raise without an extensor lag were achieved.22 Weight bearing as tolerated occurred from two to eight weeks with the use of an assistive device. Full weight bearing occurred between four to ten weeks without a brace or assistive device.
The non-weight bearing strengthening program, which began on their first visit, consisted of a quadriceps strengthening and straight leg raise progression. The literature has not shown the utility of specific VMO strengthening, and Smith et al stated that specific VMO strengthening was not widely used in the studies included in their systematic review of treatment after lateral patellar dislocation. However, they also suggested that the vastus lateralis may overpower the VMO contributing to a lateral glide of the patella.1 The hypothesis for use of the adductors is their contribution to overall stability and the potential for improved anatomic position of the patella.23 Anatomically, the MPFL is connected to the VMO and adductors, specifically.6,9,10 This anatomic finding led the authors to implement strengthening of the adductors in order to impact recruitment of the VMO for improved dynamic medial stability of the patella. Although adductor strengthening began in the three to seven week timeframe, it should be noted that this muscle group may take longer than other groups to become pain free during isometric exercise due to the drilling of the adductor tubercle for the placement of the graft.6
Advanced strengthening exercises were initiated between three and five weeks post-operatively, with the majority (4/7) of the subjects taking up to five weeks to perform upright, weight bearing activity due to the weakness of the knee knee extensors. This advancement in the exercise program correlated with reports of decreased pain, edema, improved ROM, their weight bearing status, and the ability to stand without buckling of the knee. Other considerations for delaying exercise progression include poor recruitment of the lower extremity muscular system.
Proprioceptive and neuromuscular control exercise progression is crucial after this procedure. In order to perform proprioceptive exercises adequate ROM, strength, low pain with activity, appropriate weight bearing status, and acceptable postural ability is required. Subjects in this case series completed non-weight bearing exercises, adductor strengthening exercises, and advanced strengthening exercises prior to beginning weight bearing proprioceptive exercise. Each of the previously mentioned factors must be present in order for a full retraining progression to affect the proprioceptive neurological system.18 Static demand proprioception was initiated between six and 12 weeks. The progression to dynamic proprioception occurred between seven and 20 weeks. Progression of the treatment program including modified running occurred between 10 to 21 weeks.
The higher-level plyometric drill phase occurred from 13 to 23 weeks. The progression of the proprioceptive activities was adjusted to each subject's presentation, ability, and functional goals. The subjects were instructed regarding proper landing form during plyometric activities. The importance of this phase is for the subject to demonstrate the ability to control the landing without trunk lean, hip drop, or genu valgus. Subjects were also informed to land on their midfoot in order to absorb the ground reaction forces efficiently through the entire kinetic chain.28
Sport specific drills began within the 14th to 19th week and return to sport ranged from 19 to 36 weeks. Of the seven subjects, four completed the return to sport phase during their course of physical therapy treatment. The return to sport program was modified based upon the activity each subject was returning to. Sport specific drills consisted of cutting, pivoting, and implementation of sport specific activities. Menetrey et al discussed the importance of completing a detailed return to sport progression after a five-year follow up of patients who had sustained patella subluxations. Key factors for return in patients with and without surgery after lateral patellar dislocation included clinical exam, strength of the quadriceps and gluteus medius, the amount of laxity, neuromuscular control, sport specific drills, and proper counseling by all members of the athletes rehabilitation team.18
The MCKOMS is a functional questionnaire that offers patient-reported subjective information to the therapist regarding how knee pain is affecting daily life based on intensity of activity and frequency of pain. It consists of eight sections. After review of other outcome measures the authors felt the MCKOMS would be the best choice for comparison between time of discharge and follow up. For a patient with a chronic patellar subluxation the goals of reduction of giving way or instability, increasing overall activity level including tolerance of running, and jumping or twisting were important for the return of function for this population. All of the results were in the excellent range, according to the scoring of the MCKOM, with the lowest numerical value of 82 and three subjects with 100, indicating that they all returned to sport or functional activity. The average score of the six subjects that responded was 92.8 %, demonstrating excellent results.14,27
LIMITATIONS
This retrospective case series describes how patients progressed to return to sport after undergoing a MPFL reconstruction; however there are a few limitations. This research study is limited in regards to its design in that the collection of data was done after the completion of treatments. It has a small sample size and a limited age range (14-35 years old) decreasing the generalizability to ages outside of this range. This study also lacks random selection secondary to the use of volunteers that attended a specific outpatient clinic. From the seven surgical patients, physical therapy was discontinued early for two of the patients. One patient returned to school after seven weeks but reached Stage II and the other patient, who reached stage III, had an insurance denial after 15 weeks. Subject 7 reached stage IV at 23 weeks, but then had a complication of a lateral patellar dislocation on the opposite knee. This patient's care had to be altered, as he also left for school and was seen for a follow up at 130 weeks with the ability to perform stage V and VI at that time. Future studies should attempt to conduct a randomized control trial comparing MPFL reconstruction surgeries to conservative physical therapy approach.
CONCLUSION
The results of this case series suggest that in seven subjects who that subluxed or dislocated multiple times, and underwent MPFL reconstruction and progressive rehabilitation return to sport or functional activity with less instability was achieved as reported via the MCKOMS. The hypothesis, that surgical reconstruction of the MPFL would lead to good to excellent outcomes and safe return to sport or activity after physical therapy was confirmed. The subjects responses to return to sport or activity after physical therapy treatment was assessed using several scales within the MCKOMS and these scales might be helpful in evaluation of subjects after MPFL reconstruction.
The provided rehabilitation progression may be helpful to clinicians when designing a physical therapy progression for like patients. However, additional research should be performed on this progression and regarding the ability of patients to return to their specific desired activity.
APPENDIX 1: PROPOSED TREATMENT PROGRESSION FOR REHABILITATION AFTER MEDIAL PATELLO FEMORAL LIGAMENT RECONSTRUCTION
Weeks 1-4
Non weight bearing exercises: quad sets, SLR program, modified active knee extension, multiangle isometrics (2-4 weeks)
Weeks 3-6
Unlocked Bledsoe Brace (3-6 weeks)
Adductor strengthening: hook lying ball squeezes, SLR adduction, bridging with ball squeeze.
Advanced strengthening exercises: weight bearing exercises for hip, squats with ball squeezes, lunges, step ups, leg press with ball squeeze, single leg strengthening
Proprioception: static wobble board, dyna disc, BOSU activities
Weeks 4-10
Full Weight Bearing Dynamic Proprioceptive: cone touches (6-12 weeks), agility drills, single squat, hopping, walking lunges forward and backward (6-20 weeks)
Weeks 10-21
Running: (10-21 weeks): Interval training, alterations in stride length and cadence, progression based on endurance. Plyometrics: box jumps, jump and squat, hop and squat, diagonal hop, over hurdles (13-23 weeks)
Weeks 14-19
Sport Specific Drills: cutting, pivoting, activity based on sport (14-19 weeks)
Weeks 19-36
Return to sports/functional activity: (19-36 weeks)
Additional information for Appendix 1
| Criteria for Progression | In each stage protect surgical pathology while: progressing ROM, improved quadriceps contraction, decreasing edema, minimizing pain, improving flexibility, and without extensor lag. We observe the improved dynamic functional stabilization of the soft tissue structures, test for adequate strength, without substitution of other muscles. Progression of WBAT to FWB, decreased gait deviations. Key Factors: Endurance: This is the ability to maintain performance, for the entire duration of activity. Power This is the explosive, quick movement necessary to complete an action. An example is the swing of a bat, or golf club. |
| Red flags: | Pain, edema, altered postures to complete an exercise, fatigue on one side compared to another, or substitution from other muscles. |
REFERENCES
- 1.Smith TO Davies L Chester R Clark A Donell ST. Clinical outcomes or rehabilitation for patients following lateral patellar dislocation: A systematic review. Physiotherapy. 2010; 96:269-281. [DOI] [PubMed] [Google Scholar]
- 2.Tsai et al. Primary traumatic patellar dislocation. J Orthop Surg Res. 2012; 7(21) 1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buckens CF Saris DBF. Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability. Am J Sports Med. 2010;38 (1):181-188. [DOI] [PubMed] [Google Scholar]
- 4.Endo Y Shubin Stein BE Potter HG. Radiologic assessment of patellofemoral pain in the athlete. Sports Health. 2011; 3(2):195-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Biocos J Fulkeron JP Amis A. Current Concepts Review The medial patello femoral ligament. Am J Sports Med. 2007; 35 (3): 484-492. [DOI] [PubMed] [Google Scholar]
- 6.Shah JN Howard JS Flanigan DC Brophy RH Carey JL Lattermann C. A systematic review of complication and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012; 40(8):1916-1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bentley G Biant LC Carrington RW Akmal M Goldberg A Williams AM Skinner JA Pringle J. A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. JBJS (Br). 2003; 85(2):223-30. [DOI] [PubMed] [Google Scholar]
- 8.Duchman KR DeVries NA McCarthy MA Kuiper JJ Gorsland NM Bollier MJ. Biomechanical evaluation of medial patellofemoral ligament reconstruction. The Iowa Orthopedic Journal. 2013;33:64-69. [PMC free article] [PubMed] [Google Scholar]
- 9.Amis AA Firer P Mountney J Senavongse W Thomas N. P., Anatomy and biomechanics of the medial patellofemoral ligament. The Knee. 2003;10:215-220. [DOI] [PubMed] [Google Scholar]
- 10.Ladenhauf HN Berkes MB Green DW. Medial patellofemoral ligament reconstruction using hamstring autograft in children and adolescents. ArthrosTechn. 2013;2(2):151-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panni AS Vass M Cerciello S. Acute patellar dislocation. What to do? Knee Surg Sport Traum Arthrosc. 2013; 21:275-278. [DOI] [PubMed] [Google Scholar]
- 12.Smith TO Song F Donell ST Hing CB. Operative versus nonoperative management of patellar dislocation. A meta-analysis. Knee Surg Sports Traum Arthrosc. 2011;19:988-998. [DOI] [PubMed] [Google Scholar]
- 13.Sampataco NE Getelman MH. Medial patellofemoral ligament reconstruction using a modified reverse-loop technique. Arthr Techniq. 2013;2(2);175-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Irrgang JJ Anderson AF Boland AL Harner CD Kurosaka M Neyret P Richmond JC Shelbourne KD. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600-610. [DOI] [PubMed] [Google Scholar]
- 15.Deie M Ochi M Sumen Y Yasumoto M Kobayashi K Kimura H. Reconstruction of the medial patellofemoral ligament for the treatment of habitual or recurrent dislocation of the patella in children. J Bone Joint Surg. 2003:85-B: 887-890. [PubMed] [Google Scholar]
- 16.Aulia AG Falciglia F Giordano M Savignoni P Guzzanti V. Galeazzi's modified technique for recurrent patella dislocation in skeletally immature patients. J Orthop Sci. 2012;17:148-155. [DOI] [PubMed] [Google Scholar]
- 17.Mikashima Y Kimura M Kobayashi Y Miyawaki M Tomatsu T. Clinical results of isolated reconstruction of the medial patellofemoral ligament for recurrent dislocation and subluxation of the patella. ActaOrthop Belg. 2006;72 (1):65-71 [PubMed] [Google Scholar]
- 18.Menetrey J Putman S Gard S. Return to sport after patellar dislocation or following surgery for patellofemoral instability. Knee Surg Sports Traumat Arthrosc. 2014; 22(10):2320-2326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norkin CC White DJ. Measurement of Joint Motion A Guide to Goniometry, 3rd ed. Philadelphia, PA: F.A. Davis Company; 2003. [Google Scholar]
- 20.Fowler B. Medial Patellofemoral Ligament Reconstruction / Repair Rehabilitation Program. 2003; November. Retrieved from http://www.gundersenhealth.org/sports-medicine/physical-therapy/rehabilitation
- 21.Shubin Stein B. Rehabilitation following MPFL Reconstruction. Sports Rehabilitation and Performance Center. Accessed through Hospital for Special Surgery. New York, NY. 2010
- 22.Kendall FP McCreary EK Povance PG Rodgers MM Romani WA. Muscles Testing and Function with Posture and Pain. 5th ed. Baltimore, MD: Lippincott, Williams, and Wilkins; 2005 [Google Scholar]
- 23.Hodges PW Richardson CA. The influence of isometric hip adduction on quadriceps femoris activity. Scand J Rehab Med. 1993; 25:57-62. [PubMed] [Google Scholar]
- 24.Peng HT Kernozek TW Song CY. Muscle activation of the vastus medialisobliquus and vastus lateralis during a dynamic leg press exercise with and without isometric hip adduction. Phys Ther Sport. 2013: 44-49. [DOI] [PubMed] [Google Scholar]
- 25.Matsushita T Kuroda R Araki D Kubo S Matsumoto T Kurosaka M. Medial patellofemoral ligament reconstruction with lateral soft tissue release in adult patients with habitual patellar dislocation. Knee Surg Sports Traumatol Arthros. 2012. Published online springer-Verlag. link.springer.com/article/10.1007/s00167-014-2930-8/fulltext.html [DOI] [PubMed] [Google Scholar]
- 26.Sandmeier RH Burks RT Bachus KN Billings A. The effect of reconstruction of the medial patellofemoral ligament on patellar tracking. Am J Sports Med. 2000; 28(3):345-349. [DOI] [PubMed] [Google Scholar]
- 27.Noyes FR Barber SD Mooar LA. A rationale for assessing sports activity levels and limitations in knee disorders. Clin Orthop Relat Res. 1989;(246):238-249. [PubMed] [Google Scholar]
- 28.Errigo-Vitale T Rubino A. Injuries in Irish Step Dancing: Descriptive Case Series Review. Ortho PT Practice. 2014;26(4):238-247. [Google Scholar]