ABSTRACT
Rotator cuff pathology can contribute to shoulder pain and may affect the performance of sport activities, work, and activities of daily living. The partial articular supraspinatus tendon avulsion (PASTA) lesion represents a very common type of rotator cuff pathology seen in rehabilitation. When conservative treatment fails, surgery is generally required. Success of recovery depends on several factors, including: repair techniques, healing process related to timing, rehabilitation programs, and patient compliance with home exercises. To date, most treatment modalities and rehabilitation programs are based on clinical experience rather than scientific evidence. Therefore, the purpose of this clinical commentary is to provide an overview on the PASTA lesion, discuss the common treatment approaches adopted to date and to propose a rehabilitation program based on the available scientific evidence.
Level of Evidence
5
Keywords: Rehabilitation, rotator cuff, shoulder
INTRODUCTION AND BACKGROUND
Partial-thickness rotator cuff tears (PTRCTs) are a common cause of shoulder pain, limitations in activities of daily living (ADL), and time off from work.1,2 It has been reported that the incidence of PTRCTs is between 17% and 37% in the population3,4 and up to 80% in patients in their eighth decade of life.1,5 PTRCTs were difficult to diagnose before magnetic resonance imaging (MRI) and shoulder arthroscopy, therefore most scientific research has focused on full-thickness rotator cuff tears (FTRCTs). PTRCTs are generally classified according to their location and arthroscopic appearance. The partial articular supraspinatus tendon avulsion (PASTA) lesion is a type of PTRCT and is far more common than bursal-sided or intratendinous partial tears.7-11 According to Gratsman and Milne13 PASTA lesions comprise 91% of all PTRCTs. PASTA lesions are commonly found in overhead athletes, younger people12,13 and patients who smoke.14 Although the natural history of PASTA lesions remains unclear, this variety of tendon disruption is generally associated with pain and disability and it has been shown that 53% of PASTA lesions tend to enlarge.15 Both surgical techniques and postoperative rehabilitation are essential to optimize recovery. However, significant variations exist between surgical options and rehabilitation protocols. Therefore, the purpose of this clinical commentary is to provide an overview on the PASTA lesion, discuss the common treatment approaches adopted to date and to propose a rehabilitation program based on the available scientific evidence.
ANATOMY
The glenohumeral is a delicate ball-and-socket joint. Movement of the shoulder complex can be grossly divided into scapulothoracic and glenohumeral motion. The scapula provides a bony base for muscle attachments and load transfer. Abnormal scapulothoracic motion may be a factor that increases the risk of impingement syndrome and PTRCTs.16,17 Stability of the glenohumeral joint is provided by the joint capsule, ligaments, bony anatomy, and the negative pressure within the joint space. The rotator cuff provides compression of the humeral head on the scapula, increasing the stability of the joint.18 The muscles that form the rotator cuff are: supraspinatus, subscapularis, teres minor and infraspinatus. The supraspinatus muscle originates on the posterior aspect of the scapula, superior to the spine and inserts directly on the greater tuberosity of the humerus close to the articular surface. The lateral insertion of the supraspinatus is overlapped by the tendon of the infraspinatus, fusing the two into one structure.19,20 The subscapularis is the largest muscle-tendon unit. It originates on the anterior aspect of the scapula and inserts on the medial aspect of the biceps groove. The teres minor originates on the posterior surface of the axillary border of the scapula and inserts on the inferior-posterior aspect of the greater tuberosity of the humerus. The infraspinatus lies on the posterior aspect of the scapula. It originates inferior to the spine of the scapula and inserts on the greater tuberosity of the humerus, wrapping around the posterior aspect of the supraspinatus tendon. The subscapularis provides anterior stability and internal rotation motion to the humerus21 while the supraspinatus, teres minor and infraspinatus make up the posterior aspect of the rotator cuff which is responsible for abduction and external rotation of the shoulder.1,17,21,22
PATHOPHYSIOLOGY
Mechanisms leading to rotator cuff injury are still under debate. Generally, PTRCTs occur at the junction of the inferior part of the supraspinatus and the superior part of the infraspinatus, leading to the PASTA lesion.23 Most clinicians think that intrinsic, extrinsic and traumatic factors are all possible causes of PASTA tears. Among the intrinsic factors, changes in rotator cuff vascularity and metabolic changes associated with aging seem to play an important role. Some authors have shown that the size of the vessels are larger and more prevalent on the bursal side of the rotator cuff while the articular surface of the rotator cuff is relatively hypovascular.24 Results of histological studies have also shown that collagen is thinner and not as well organized on the articular surface of the rotator cuff when compared to the bursal surface of the rotator cuff,24 leading some authors to believe that the articular cuff is only one half as strong as the bursal counterpart.25 Alternatively, some authors that believe extrinsic and traumatic factors are primary contributors to in the development of PASTA lesions. Shear stresses that affect the supraspinatus tendon due to narrowing of the coracoacromial arch (extrinsic impingement) have been identified as a plausible cause of rotator cuff injury as they may generate a laminated disrepair of the surfaces of the cuff.13 Repetitive microtrauma may also cause articular surface tears especially when associated with overhead activities.6 Internal impingement as termed by Walch and colleagues26 has been demonstrated as another possible reason for the PASTA lesion in overhead athletes. It occurs due to the repetitive contact of the articular surface of the supraspinatus and infraspinatus tendons with the posterosuperior part of the glenoid during arm abduction and lateral rotation.23,27,28 Many authors believe that anterior shoulder micro-instability is contributory to internal impingement and to PASTA lesions although rotator cuff injuries have been demonstrated in otherwise stable shoulders.26,27
CLINICAL DIAGNOSIS
Clinical diagnosis of PASTA lesion can be difficult as not all PASTA lesions are symptomatic.29 Pain is generally present in the arc of motion between 60 ° and 120 °.6 Some authors have reported that PTRCTs can be more painful than FTRCTs.30,31 It has also been reported that pain may be correlated with increased levels of Substance P in the subacromial bursa rather than the extent or the depth of the tear of the tendon.32 Pain is generally provoked by resisted abduction with the shoulder positioned at 90 ° of abduction, in the plane of the scapula and in either internal or external rotation as in the empty/full can test. However, when considering pain as a symptom for detection of supraspinatus tendon tear Itoi et al suggest the utilization of the full can test.33 A positive lag test should make the clinician think of a FTRCT rather than PASTA lesion.34 Impingement tests such as those proposed by Neer and Hawkins may be positive.13 If impingement tests are positive, the internal rotation resistance strength test may be utilized to help distinguish between outlet (Neer) and non-outlet (internal) impingement. With the shoulder positioned at 90 ° of abduction, at approximately 80 ° of external rotation and with the elbow bent at 90 °, external and internal rotator muscles are tested with a resisted isometric contraction. A sign of apparent weakness of internal versus external rotation of the shoulder is considered positive for non-outlet (internal) impingement.35 For the overhead athlete, the clinician should also look for subtle signs of shoulder instability. Apprehension and relocation tests may be used during the examination although the presence of pain without apprehension is an unreliable finding for shoulder instability, as it is quite common in many other shoulder disorders.36-38 Physical examination findings for PASTA lesion can be non-specific and difficult to distinguish from other shoulder conditions. It has been reported that 30% of PASTA lesions occur concomitantly to other shoulder disorders.26,39 As a result, imaging modalities are essential for definitive diagnosis of the PASTA lesion.
IMAGING
A combination of imaging modalities is generally used for the assessment of PASTA lesion as no single imaging study has been shown to be particularly accurate. Radiographs, including an anteroposterior view of the shoulder, an axillary lateral view and a supraspinatus outlet view are sometimes used. However, they are more appropriate for assessing acromionclavicular lesions or glenohumeral disorders than PASTA lesions.40
Ultrasound imaging is an appropriate technique for assessment of rotator cuff tears and has been proved to be valuable for diagnosis of both FTRCTs and PTRCTs.41,42 It should be considered the best option considering safety, cost, and accuracy for FTRCTs.43 However, sensitivity of ultrasound imaging for PTRCTs is lower than magnetic resonance imaging (MRI).44
Although MRI techniques have recently improved the ability to detect subtle rotator cuff tendon abnormalities, findings of the MRI should be interpreted cautiously as false-negative results when compared to arthroscopy have been reported in a previous study.13 MRI has demonstrated high sensitivity and specificity (0.90) for FTRCTs,43 but poorer sensitivity for detection of partial rotator cuff tears.44 The clinical relevance of MRI is further limited as many individuals older than 40 years of age who demonstrate abnormal rotator cuff findings on MRI are symptom-free at the clinical evaluation.29 Thus, signs of partial rotator cuff tear on MRI could be an incidental finding in symptomatic as well as in asymptomatic patients.
CLASSIFICATION
PTRCTs are defined as definite disruption of fibers of the tendon and not simply fraying, roughening, or softening of the tendon surface. Tears can be classified with regards to the involved tendon, the location (articular, bursal or intratendinous) and the size, represented as the percentage of the tendon thickness torn or the vertical component relative to the tendon thickness. Although there is not a classification system specifically designed for PASTA lesions, two main rotator cuff tear classification systems are generally utilized. Ellman45 described the lesions of the rotator cuff tendon according to the location of the tear (articular surface, bursal surface and intratendinous) and the extension of the tear. Grade 1 tears are smaller than 3 mm, Grade 2 tears are between 3 and 6 mm, while Grade 3 tears involve more than one half of the cuff tendon thickness (generally more than 6 mm).
Snyder and colleagues39,40 have adopted a similar classification system based on the location of the tear (A = articular surface, B = bursal surface, C = complete) and on the arthroscopic appearance (grades from 0 to 4). Grade 0 represents a normal cuff. In Grade 1 there is minimal superficial fraying in an area smaller than 1 cm. Grade 2 signifies fraying and failure of the rotator cuff tendon in an area smaller than 2 cm. In Grade 3 there is fraying and fragmentation of the entire surface of the tendon. Grade 4 tears are characterized by a stable flap tear that often encompasses more than a single rotator cuff tendon that is larger than 3 cm.
The management of PASTA tears remains controversial. Most surgeons agree with the concept that treatment of PASTA lesions varies according to the stage and the pathology and should begin with conservative treatment. However, when more than one half of the thickness of the supraspinatus tendon is involved (Ellman or Snyder Grade 3) surgical repair in symptomatic patients is indicated.11,46
The final choice informing treatment for PASTA lesions should consider clinical evaluation, imaging findings, and classification of the tear. Treatment options are either conservative or surgical.
CONSERVATIVE TREATMENT
Treatment should start with physical therapy. Rest or activity modification with the avoidance of the movements that elicit pain should be included from the early stage of the management. Oral non-steroidal anti-inflammatory drugs may be beneficial for reduction of pain and inflammation47 although they are less effective than corticosteroids in terms of pain reduction.48 However, it is important to note that both non-steroidal anti-inflammatory and corticosteroid drugs may have deleterious effects on long-term tendon healing.49,50
Although commonly utilized to manage rotator cuff tears, many physical modalities and manual therapy techniques lack validated research that justifies their use. Laser therapy has been widely studied on several tendinopathies with mixed results. It has been suggested to be beneficial for shoulder tendinopathy51 and superior to therapeutic ultrasound in terms of pain reduction.52,53 Therapeutic ultrasound seems to help reverse the tendinosis54 and appears beneficial for calcific tendonitis of the supraspinatus.55 However, it has been shown to be no more effective than placebo for soft tissue disorders of the shoulder.56 Transcutaneous electrical nerve stimulation (TENS) for shoulder disorders has not been studied as much as laser and therapeutic ultrasound. It has been shown to be effective for post-surgical pain,57 but there is paucity of evidence regarding its effectiveness for PASTA lesions.
The use of joint mobilization techniques such as accessory movements and joint glides can be applied to assist in decreasing pain, muscle guarding, and restoring range of motion (ROM) deficits.58 Although joint mobilizations and mobilizations with movement have been found to not be superior to supervised exercise and to physician advice,59 manual therapy techniques to the glenohumeral joint seem to have positive effects across all painful shoulder conditions.60 A recent review investigating adults suffering of non-specific shoulder pain demonstrated that spinal manipulations and spinal mobilizations also help improve self perceived recovery when compared to usual care.61 Myofascial massage of trigger points located in the shoulder girdle soft tissues seems to be more effective than placebo in terms of pain and shoulder function in patients suffering from shoulder disorders.62-64
Once pain is manageable, physical therapy should proceed to restoring ROM deficits and strengthening of relevant muscle groups with particular focus on the scapular stabilizers and rotator cuff muscles,65,66 initially avoiding those exercises that maximally activate the supraspinatus muscle-tendon unit. Stretching techniques should be performed in those patients with total arc of motion limitations, particularly in the overhead athletes with glenohumeral internal rotation deficits due to posterior capsule tightness.67,68
Restoration of neuromuscular coordination and core stability is also beneficial and important to restore the mechanisms of load transfer and for the avoidance of scapulothoracic dyskinesis.69,70 It is in fact well known that upper extremity motion occurs with consistent synergistic muscle activation patterns in the legs and trunk.71,72 Therefore, it is important to remember that scapular muscle force couples requires core strength and facilitation by the activation of the whole kinetic chain.73,74
As there is not a treatment algorithm for PASTA lesions and no evidence regarding the evolution of non-operative treatment, the outcome of conservative treatment is unknown. However, the results of one study indicate that there was a progression of the rotator cuff tear in 80% of the patients who were treated non-operatively.15 This would suggest that surgical treatment for PASTA lesion should be considered.
SURGICAL TREATMENT
As spontaneous healing of PTRCTs is unlikely or poor,15,75 surgery is often required. Surgical treatment of PTRCTs generally involves one of the following: arthroscopic debridement of the tear, debridement with acromioplasty, and rotator cuff repair with or without acromioplasty.76
There is controversy whether debridement with or without acromioplasty is a sufficient treatment option for PTRCTs. Budoff et al77 reported excellent results while more recent investigations have shown that although pain may get better,78 a large portion of PTRCTs evolve to deterioration of the lesion leading to FTRCTs.79
If a significant articular-sided tear is present and there is a significant healthy portion of the bursal side of the tendon still intact, some surgeons may prefer to repair the tear by making a small perforation in the rotator cuff as a method to place medial anchors. This is a safe and effective modern arthroscopic technique that restores the anatomy of the damaged rotator cuff by securing the articular side of the tendon back to its original footprint while preserving the undamaged bursal side of the tendon.79-81 Attempts to preserve the bursal side footprint of the rotator cuff as in the trans-tendon repair technique has been shown to enhance healing and clinical outcomes.81-85
In some cases when only 25% of supraspinatus tendon remains attached to the bone, surgeons may prefer to complete the tear from a PTRCT to a FTRCT and treat it using suture anchors. However, when conversion to FTRCT is performed, there is a high rate of re-tear. It may be due to formation of scar tissue and lack of restoration of fibro-cartilaginous connection in the bone-tendon attachment.84 Regardless the surgical approach; post-surgical rehabilitative management is key.
POST-SURGICAL TREATMENT
In addition to the surgical technique adopted by the surgeon, knowledge of the histology and biology of the healing process is paramount as it guides the therapist to rehabilitation programs that optimize healing rate and improve clinical outcomes. Authors suggest that tendon healing consists of three overlapping phases: inflammation, proliferative/repair and remodeling.16,86,87 Following surgical tendon-to-bone fixation, there is an inflammatory phase where type-III collagen synthesis is initiated over the surgery site. After a few days, growth factors induce cellular proliferation and matrix deposition. After approximately six weeks, the tissue begins remodeling where there is organization of the scar tissue and a higher proportion of Type-I collagen is synthesized.88 However, remodeling repair tissue does not reach maximal tensile strength before 12-16 weeks after surgery.89 It is important to remember that during the rehabilitation program progression, the mechanical proprieties of the repairing fibrous tissue are weaker than the native tissue90 and that it prone to failure and re-tear may occur in up to 12% of the cases.86
The following sections report the evidence of common post-operative treatment options and present an evidence-supported program for the post-surgery treatment of PASTA lesions.
Immobilization and early versus delayed range of motion
Post-surgical stiffness is one of the most common complications occurring after rotator cuff surgery regardless the surgical technique adopted and it is likely linked to prolonged immobilization.91,92 However, research results supporting immobilization timeframes, or early or delayed ROM after surgical repair of rotator cuff tears are still controversial. Animal studies indicate that immobilization may reduce the tension over the rotator cuff repair and may help improve the collagen orientation93,94 although it can cause deterioration of a tendon as it decreases the protein synthesis95 and increases the collagenase activity.96
The optimal timing for initiation of ROM remains under debate. There are some authors that, regardless of the prolonged healing process required for a tendon-to-bone repair, suggest that early mobilization can be safely applied.97,98 Early mobilization is also considered to help recover ROM more rapidly in those patients who undergo arthroscopy for cuff repair.99 Other authors suggest that there is no difference between early and delayed joint mobilization after arthroscopic cuff repair100,101 for stiffness and ROM and that prolonged immobilization up to six weeks or delayed ROM is not a concern for joint stiffness.102,103
Research has been extensively conducted on repair of FTRCTs but not for PASTA lesions, therefore, there are no recognized indications regarding immobilization and ROM timing. However, patients with PASTA lesions should be mobilized as early as possible as it has been suggested that arthroscopic repair of PASTA lesions is a risk factor for post-surgery stiffness.104
Cryotherapy
Cryotherapy is generally used post-surgery to decrease pain, inflammation and swelling. Adie et al105 examined the effects of cryotherapy after total knee arthroplasty, showing the benefit of reduction of blood loss and pain although the improvement may not have been clinically significant. Authors have also shown that the use of cryotherapy after shoulder surgery decreases the need for narcotics and that patients are better able to tolerate rehabilitation106 and to return to normal sleeping patterns.107 Although the use of cryotherapy is still under debate, most believe it advisable for use it in the immediate post-surgical timeframe.
Regenerative techniques
Tissue regenerative strategies involving the use of mesenchymal stem cells, growth factors and platelet rich-plasma may be potentially effective therapies to enhance bone-to-tendon healing after shoulder surgery. Promising results have been reported in both animal and in vitro studies including: a better orientation of the fibrocartilage fibers, improvement of mechanical resistance108 and tendon healing.109 Ellera Gomes et al110 published the only investigation on the effects of stem cells in rotator cuff tears in humans to date. They investigated 14 patients with a complete tear of the rotator cuff repaired in a trans-osseous fashion thorough a mini-incision augmenting the suture with stem cells. At 12 months, according to clinical and magnetic resonance findings, 12 of the 14 tears had healed. However, the use of these new augmentation techniques on rotator cuff tears should still be considered experimental because both surgical costs and lack of validated basic and clinical research.111-115
PROPOSAL OF A POST-SURGERY PROGRAM FOR PASTA LESIONS
As every PASTA lesion and every patient is unique, several considerations must be taken into account when building a rehabilitation program for optimal results. The rehabilitation program should be evaluation-based and should consider size of the tear, surgical technique, healing process timing, surgical findings, patient age, and the patient's goals. Therefore, the following five-phased program serves as a guideline that should be individualized for each case and adapted to each patient.
Phase I
The main goals of this stage are to enhance the structural repair, control pain and inflammation, increase ROM, and prevent muscular atrophy. During this phase, a sling should be worn for about two weeks in order to maintain integrity of the repair site and to encourage rotator cuff healing116 and it should be removed only for self-care and wound cleansing. It has been suggested that the shoulder should be immobilized in the scapular plane at 45 ° of shoulder abduction as this position enhances regional blood flow and minimizes the passive tension on the repair site by reducing the distance between the origin and the insertion of the supraspinatus muscle.117 It is important to keep good mobility and strength in the elbow, wrist and hand while initiating a preliminary rehabilitation program. As collagen deposition increases 10 days after surgery and reaches a plateau at about 56 days after surgery,118 passive mobilization that excessively stresses the newly formed collagen network should be avoided. However, passive motion in a controlled manner within a safe ROM is beneficial as it positively affect the orientation of the collagen fibers 90,91,119,120 and may minimize potential joint stiffness.121 Exercises should be passive initially and then assisted by tools such a wand. An example of passive ROM consists of repetitions of closed kinetic chain (CKC) shoulder flexion with the support of a table (Figures 1 A-B). While standing in front of a table, place the hands on the table and step away as far as comfortable, hold the position and go back to the initial position. CKC exercises increase joint approximation, stimulation of mechanoreceptors and dynamic stability of shoulder complex,122,123 resulting in an improvement of kinesthesia.124 Pendulum exercises are also usually utilized in this phase. Standing with the trunk bent and the good arm placed on a table for stability, the patient swings the affected arm while drawing circles (Figure 2). An electromyographic analysis demonstrated that the activation of the supraspinatus muscle is less than 10% when small diameter circles are performed.125
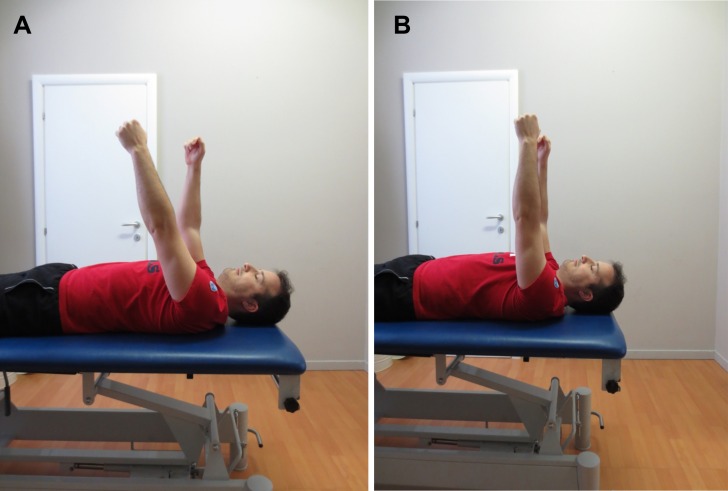
Figure 1 A-B.
CKC shoulder flexion on a table. Initial (A) and final (B) positions.
Figure 2.
Pedulum exercise with the supporting arm on a table.
Manual therapy including glenohumeral distractions and anterior and posterior glides to the glenohumeral joint with the shoulder in the resting position can be used to restore ROM since glides have been shown to be safe during the initial stages of rehab, without altering stress on the repaired supraspinatus tendon.126 Shoulder function and pain may also be improved with sternoclavicular joint mobilization.127 Mobilization of the scapula may be useful in the initial stages as it may help break down adhesions and release muscle guarding, improving general function of the shoulder and decrease pain. However, it does not appear to be more effective than placebo and supervised exercise.128,129
Aquatic therapy (the use of the water for rehabilitation purposes), can be safely introduced once the stitches have been removed and the surgery wound has healed completely. This rehabilitative technique provides a supportive medium, facilitates ROM, and is a method to light initiate resistance training.130-132 Moreover, various exercises performed in water demonstrate less rotator cuff electromyographic activation than when performed on the land,133 aquatic therapy offers a safe environment to perform movements without compromising the healing process of the repair site.
During this phase, attention should be also placed on a good postural awareness and control of the spine and of the scapula by activation of the scapular musculature. Scapular retractions and depressions are appropriate exercises to activate the shoulder girdle musculature with minimal rotator cuff recruitment.134 To improve muscle activation awareness, it is advisable to use an electromyographic biofeedback. Patient education is of the utmost importance for this phase of the rehabilitation program, as the patient may need to carry out the prescribed exercises at home with minimal supervision of the therapist.
Criteria to progress to the next phase are: minimal discomfort when the shoulder is unsupported, pain-free passive flexion to 130 °, pain-free passive internal and external rotation to 50 ° in the scapular plane.
Phase II
The patient may be ready for this phase at 3-4 weeks post-surgery although it may be delayed depending on the quality and size of the repair.135 During this phase the healing process is increasing the tensile strength of the repair site which is now able to withstand higher mechanical loads.136 Exercises during this phase are performed in order to attain full pain-free ROM, improve neuromuscular control, restore normal patterns of muscle contraction and to return to normal ADLs. The use of pulleys, canes, and active assisted ROM (AAROM) are indicated at this point to enhance movement and recover full ROM. Stretching of the pectoralis minor muscle if it restricts upward rotation of the scapula is also advisable. Sub-maximal isometric contractions in all planes and at multiple angles can be initiated at the stage. Activation of the scapulothoracic stabilizers should still be a major focus as it allows neuromuscular control and full pain-free ROM. Attention should be placed to the scapular retractors (rhomboids and medium trapezius muscles), scapular protractors (serratus anterior muscle) and scapular depressors (lower trapezius muscle) which are enhanced with low rows (Figure 3).
Figure 3.
Low rows. The patient is standing with one hand on the edge of a table and pushes backwards retracting and depressing the scapula.
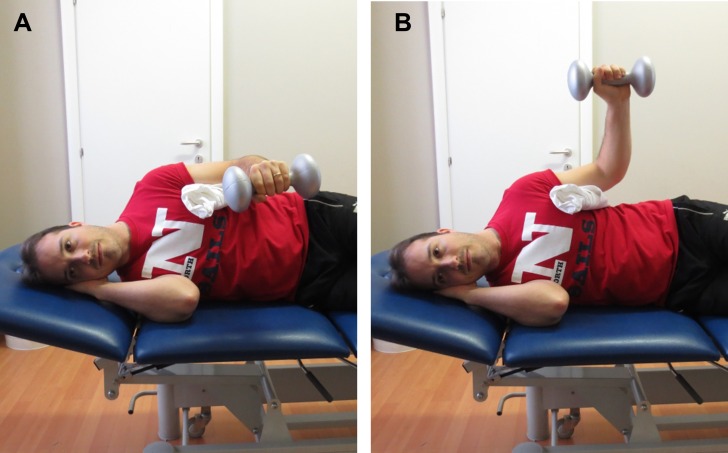
Excess upper trapezius (UT) muscle activity with decreased activation of the lower trapezius (LT) muscle has been proposed to contribute to poor posture, muscle imbalances, and several shoulder pathologies.137,138 Therefore, it is important to assess and address the LT/UT and middle trapezius (MT) muscle/UT activity ratio.139 Exercises that enhance the LT/UT and MT/UT activity ratios are side-lying external rotation with a pillow between the body and the arm140 (Figures 4 A-B), side-lying forward flexion and prone horizontal abduction with the shoulder in external rotation.139
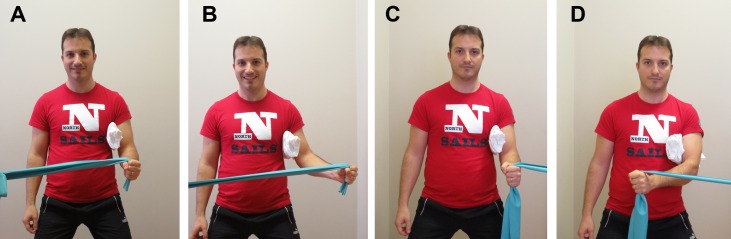
Figure 4 A-B.
External rotation in side-lying. Beginning position (A) and ending position (B).
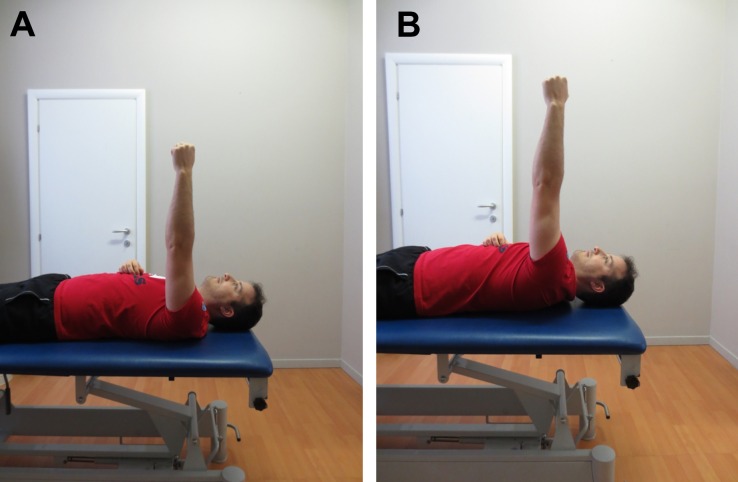
The serratus anterior can be activated in supine by scapular protraction in 90 ° of shoulder flexion (Figures 5 A-B).
Figure 5 A-B.
Activation of serratus anterior in supine by scapular protraction. Initial position (A) and ending position (B).
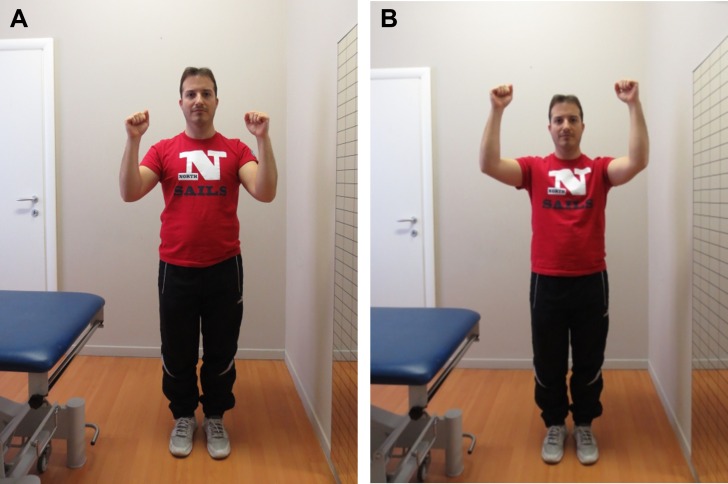
Scaption (scapular plane elevation) can be introduced at this stage to initiate recruitment of the supraspinatus muscle. Initially, it is advisable to perform this exercise with the elbow bent at 90 ° to reduce excessive stress to the repair site by using a shortened lever arm (Figures 6 A-B). Next, this exercise can be progressed to the “full can” exercise (Figures 7 A-B), which is known to demonstrate high activation of the supraspinatus,17,33 minimizing the chance of subacromial impingement.141 Due to the simultaneous activation of multiple muscles, it has been suggested that scaption (full-can) exercises be implemented when preparing a patient to perform tasks that require open chain elevation beyond the shoulder level.142
Figure 6 A-B.
Scapular plane (scaption) exercise with elbows bent at 90 °. Initial (A) and final (B) positions.
Figure 7 A-B.
“Full can” exercise. The patient elevates the arms on the scapular plane from the side (A) to 90 ° of flexion (B), keeping the shoulder in external rotation (thumbs up).
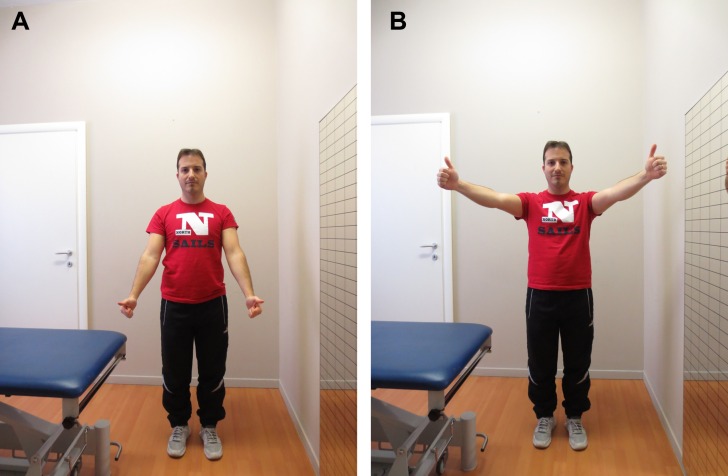
Open chain proprioceptive activities can be initiated during this stage. Examples include joint positioning and mirror repositioning for flexion.143 In supine, the noninvolved shoulder is positioned at a certain angle of flexion and then the patient tries to mirror the same angle with the involved shoulder with and then without visual clue (Figures 8 A-B). This exercise is also important for monitoring the activity of the UT during elevation tasks and avoiding the shoulder shrug position.
Figure 8 A-B.
The patient positions the uninvolved shoulder (right) at certain angle of flexion (A) and then mirrors the same angle with the involved shoulder (left) (B) with and then without visual input (queue).
Criteria to progress to the next phase are: full pain-free ROM, negative impingement tests and no scapular dyskinesia during both static positions and active scaption movements.
Phase III
Phase three generally starts at 6-8 weeks post-surgery, at which time the remodeling phase is nearly complete and soft tissues are reasonably well healed, requiring less protection that during the earlier stages. Exercises during this phase are progressed and directed towards aims such as: improving strength and endurance of the rotator cuff and shoulder girdle muscles.144 Shoulder internal and external rotator muscles are strengthened by motions utilizing graduated elastic bands with the arm in the scapular plane and below the shoulder height. To do so, it would be advisable to use a pillow or towel roll between the upper limb and the trunk as this configuration enlarges the sub-acromial space, reducing the risk of primary impingement (Figures 9 A-D).145
Figure 9 A-D.
Strengthening of shoulder external and internal rotators with elastic band resistance, with a pillow between the trunk and the upper limb. Initial (A) and final (B) position for external rotators. Initial (C) and final (D) position for internal rotators.
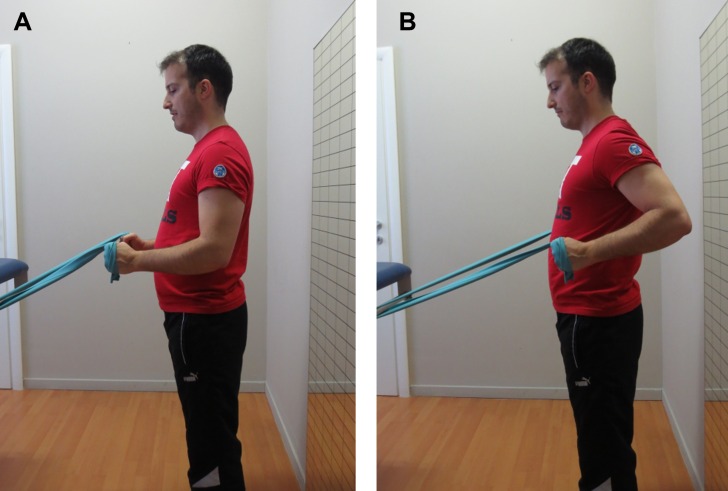
Strengthening of the serratus anterior muscle continues with the dynamic hug exercise as illustrated by Decker et al.146 This exercise is performed in standing, using elastic resistance and mimicking a hugging motion around a cylindrical object with the shoulder internally rotated to 45 ° (Figures 10 A-B). The muscle then is further strengthened via CKC exercises using the “plus” position which is characterized by maximal scapular protraction, generating maximal activation of the muscle.143,146,147 An example is the pointer exercise with balance disc and oscillation device (Figure 11). As increasing upper extremity weight-bearing requires increasing shoulder musculature demand,148 more advanced CKC stability exercises, such as: rhythmic stabilization in the quadruped position with weight shifts and perturbations or prone walkouts on a physioball, are progressively introduced to improve neuromuscular control of the shoulder.
Figure 10 A-B.
Dynamic hug exercise. With the resistance of an elastic band, the patients begins the exercise with the elbows flexed, shoulders abducted and internally rotated (A). Then the patient performs an imaginary arc, while extending the elbows, until maximum protraction is attained (B).
Figure 11.
Pointer exercise with oscillating device and “plus” position on weight-bearing limb (left) for the serratus anterior muscle.
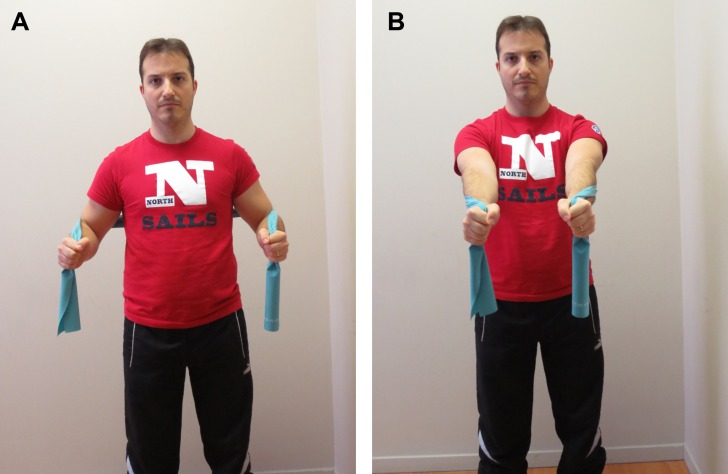
Trapezius and rhomboid muscles are also important and can be strengthened with elastic resistance (Figures 12 A-B).
Figure 12 A-B.
Elastic resistance for strengthening of trapezius and rhomnoid muscles. Initial position (A) and final position (B).
To improve scapulothoracic muscular endurance, it is suggested to utilize exercises with low to moderate resistance, high repetitions (long-duration sets) and minimal rest between sets.149 An upper ergometer may be also beneficial. However, in order to prevent sub-acromial impingement, it should be utilized in standing, with the axis of the ergometer below shoulder level.
Biceps and triceps brachii muscles may be addressed as needed at this time with conventional biceps curls and triceps extension using free weight (isotonic) or elastic resistance.
The therapist should guide the patient during the execution of all exercises in order to avoid substitution patterns (shoulder shrug sign) and encourage proper techniques.
To maximize force generation, utilize the entire kinetic chain during upper extremity movements, and minimize joint loads, incorporation of a core stability-strengthening program is recommended. Although description of specific exercises and progression is beyond the scope of this clinical commentary, addressing the core is important, especially if the patient is an athlete who wishes to go back to sport activities.150
Progression to the last phase is possible once the patient is pain-free with ADLs.
Phase IV
At about 12 weeks post-surgery, the healing process should be complete enough to allow the healed collagen to withstand increasing mechanical forces. This phase is a progression of Phase III, including more demanding strengthening exercises. Rotator cuff muscles are strengthened by using internal and external rotation with elastic resistance in more challenging positions such as: at 45 ° of shoulder abduction, initially, and at 90 ° of shoulder abduction later.
Advanced rhythmic stabilization training in open-kinetic-chain is accomplished by the use of an oscillating blade or device. The patient oscillates the blade vertically and horizontally while maintaining the shoulder in the scapular plane at about 90 ° of flexion (Figure 13). Progressively, the patient is challenged outside of the scapular plane in more demanding positions, for example at 90 ° of abduction and 90 ° of external rotation, and eventually in sport-specific movements.
Figure 13.

Advanced rhythmic stabilization with oscillating blade.
Plyometric training is also paramount and needs to be addressed in the late stages of Phase IV. Plyometrics employ the stretch-shortening cycle with the goals of stimulating the body's proprioceptors and increasing muscle recruitment over a minimal amount of time.151 Usually the patient starts by performing bilateral wall tosses and progresses to unilateral throws against a rebounder with progressively heavier weighted balls. Exercises should begin with positions below shoulder level and progress to overhead positions. An example of advanced plyometric exercise for the internal rotators is performed with the patient in supine with the arm in the 90/90 position, and the patient catches and immediately tosses back the weighted ball to the therapist. Such an exercise can be progressed to upright positions such as half-kneeling and standing.
Phase V (Return to sport)
After completing Phase IV, athletes should complete an interval sport program to safely return to competitive sport activities. Interval sport programs should be sport specific although there should be general exercise prescription focusing on cardiovascular endurance, scapulothoracic and rotator cuff muscle strengthening. Recurrences of injury to the rotator cuff should attempt to be minimized therefore, any reasons thought to facilitate PASTA lesions, such as anterior shoulder micro-instability should be addressed adequately. Once the athlete has completed the progressive return to sport program without complaint of pain or discomfort and has been cleared by the surgeon, return to competitive activity can be initiated.
Patients who are not athletes, should maintain the flexibility, endurance and strength levels achieved during Phase I-IV and may benefit from functional progression programs for activities specific for their function.
CONCLUSIONS
This clinical commentary provides an overview of PASTA lesions, presents options for management of these lesions, analyzes the common treatment approaches utilized to date, and describes a rehabilitation program based on available scientific evidence.
Post-surgical rehabilitation of PASTA lesions should consider surgical findings, patient age, level of activity, and patient-related outcome goals. Moreover, understanding of soft tissue healing timing is paramount as it affects rehabilitation choices and provides the basic foundation for the progression of a rehabilitation program.
Therapeutic modalities and rehabilitative exercises are often based on clinical experience rather than scientific evidence, therefore, future research on PASTA lesions should be focused on providing scientific rationale for the use of therapeutic modalities and exercise programs as well as timelines for progression.
REFERENCES
- 1.Yamamoto A. Takagishi K. Osawa T., et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010. 19(1): 116-120. [DOI] [PubMed] [Google Scholar]
- 2.Lin J.C. Weintraub N Aragaki D.R. Nonsurgical treatment for rotator cuff injury in the elderly. J Am Med Dir Assoc. 2006. 9(9): 626-632. [DOI] [PubMed] [Google Scholar]
- 3.Fukada H. Mikasa M. Yamanaka K. Incomplete thickness rotator cuff tears diagnosed by subcromial bursography. Clin Orthop Relat Res. 1987. 223: 51-58. [PubMed] [Google Scholar]
- 4.Fukada H. Mikasa M. Ogawa K., et al. The color test: an intraoperative staining test for joint-side rotator cuff tearing and its extension. J Shoulder Elbow Surg. 1992. 1(2): 86-90. [DOI] [PubMed] [Google Scholar]
- 5.Oliva F. Via A. G. Maffulli N. Calcific tendinopathy of the rotator cuff tendons. Sports Med Arthrosc. 2011. 19(3): 237-243. [DOI] [PubMed] [Google Scholar]
- 6.Itoi E. Tabata S. Incomplete rotator cuff tears: results of operative treatment. Clin Orthop Relat Res. 1992. 284: 128-135. [PubMed] [Google Scholar]
- 7.Liem D. Bushmann V. E. Schmidt C., et al. The prevalence of rotator cuff tears: is the contralateral shoulder at risk? Am J Sports Med. 2014. 42(4): 826-830. [DOI] [PubMed] [Google Scholar]
- 8.Yang S. Park H.S. Flores S., et al. Biomechanical analysis of bursal-sided partial thickness rotator cuff tears. J shoulder Elbow Surg. 2009. 18(3): 379-385. [DOI] [PubMed] [Google Scholar]
- 9.McConville O. R. Ianotti J. P. Partial thickness tears of the rotator cuff: evaluation and management. J Am Acad Orthop Surg. 1999. 7(1): 32-43. [DOI] [PubMed] [Google Scholar]
- 10.Gartsman G. M. Arthroscopic treatment of rotator cuff disease. J Shoulder Elbow Surg. 1995. 4(3): 228-241. [DOI] [PubMed] [Google Scholar]
- 11.Weber S. C. Arthroscopic debridement and acromioplasty versus mini-open repair in the management of significant partial-thickness tears of the rotator cuff. Orthop Clin North Am. 1997. 28(1): 79-82. [DOI] [PubMed] [Google Scholar]
- 12.Payne L. Z. Altchek D. W. Craig E. V. Arthroscopic treatment of partial rotator cuff tears in young athletes: a preliminary report. Am J Sports Med. 1997. 25(3): 299-305. [DOI] [PubMed] [Google Scholar]
- 13.Gartsman G. M. Milne J. C. Articular surface partial-thickness rotator cuff tears. J Shoulder Elbow Surg. 1995. 4(6): 409-415. [DOI] [PubMed] [Google Scholar]
- 14.Bishop J. Y. Santiago-Torres J. E. Rimmke N., et al. Smoking predisposes to rotator cuff pathology and shoulder dysfunction: a systematic review. Arthroscopy. 2015. 31(8): 1598-1605. [DOI] [PubMed] [Google Scholar]
- 15.Yamanaka K. Matsumoto T. The joint side tear of the rotator cuff. A follow up study by arthrography. Clin Orthop Relat Res. 1994. 304: 68-73 [PubMed] [Google Scholar]
- 16.Van Der MeiJden O. A. Westgard P. Chandker Z., et al. Rehabilitation after arthroscopic rotator cuff repair: current concepts review and evidence-based guidelines. Int J Sports Phys Ther. 2012. 7(2): 197-218. [PMC free article] [PubMed] [Google Scholar]
- 17.Escamilla R. F. Yamashiro K. Paulos L., et al. Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sports Med. 2009. 39(8): 663-685. [DOI] [PubMed] [Google Scholar]
- 18.Vo A. Zhou H. Dumont G., et al. Physical therapy and rehabilitation after rotator cuff repair: a review of current concepts. Int J Phys Med Rehabil. 2013. 1(7): 1-5. [Google Scholar]
- 19.Curtis A. S. Burbank K. M. Tierney J. J., et al. The insertional footprint of the rotator cuff: an anatomic study. Arthroscopy. 2006. 22(6): 603-609. [DOI] [PubMed] [Google Scholar]
- 20.Mochizuki T. Sugaya H. Uomizu M., et al. Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff. J Bone Joint Surg Am. 2008. 90(5): 962-969. [DOI] [PubMed] [Google Scholar]
- 21.Inman V. T. Saunders J. B. Abbott L.C. Observation of the function of the shoulder joint. Clin Orthop Relat Res. 1996. 330: 3-12. [DOI] [PubMed] [Google Scholar]
- 22.Boykin R. E. Heuer H. J. Vaishnav S., et al. Rotator cuff disease: basics of diagnosis and treatment. Rheumatol Rep. 2010. 2(1): 1-12. [Google Scholar]
- 23.Park S. S. Loebenberg M. L. Rokito A. S., et al. The shoulder in baseball pitching: biomechanics and related injuries – Part 2. Bull NYH Hosp Jt Dis. 2003. 61(2): 68-79. [PubMed] [Google Scholar]
- 24.Clark J. M. Harryman D. T. Tendons, ligaments, and capsule of the rotator cuff: gross and microscopic anatomy. J Bone Joint Surg Am. 1992. 74(5): 713-725. [PubMed] [Google Scholar]
- 25.Nakajima T. Rokuuma N. Hamada K., et al. Histologic and biomechanical characteristics of the supraspinatus tendon. Reference to rotator cuff tearing. J Shoulder Elbow Surg. 1994. 3(2): 79-87. [DOI] [PubMed] [Google Scholar]
- 26.Walch G. Boileau P. Noel E., et al. Impingement of the deep surface of the supraspinatus tendon on the posterior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg. 1992. 1(5): 238-245. [DOI] [PubMed] [Google Scholar]
- 27.Jobe C. M. Superior glenoid impingement. Orthop Clin North Am 1997. 28(2): 137-143. [DOI] [PubMed] [Google Scholar]
- 28.Dodson C. C. Brockmeier S. F. Altcheck D. W. Partial-thickness rotator cuff tears in throwing athletes. Oper Tech Sports Med. 2007. 15(3): 124-131. [Google Scholar]
- 29.Sher J. S. Uribe J. W. Posada A., et al. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995. 77(1): 10-15. [DOI] [PubMed] [Google Scholar]
- 30.Fukada H. Hamada K. Nakajima T., et al. Pathology and pathogenesis of the intratendineous tearing of the rotator cuff viewed from en bloc histologic sections. Clin Orthop Relat Res. 1994. 304: 60-67. [PubMed] [Google Scholar]
- 31.Gschwend N. Ivosevic-Radovanovic D. Patte D. Rotator cuff tear: relationship between clinical and anatomopathological findings. Arch Orthop Trauma Surg. 1998. 107(1): 7-15. [DOI] [PubMed] [Google Scholar]
- 32.Gotoh M. Hamada K. Yamakawa H., et al. Increased substance P in the subacromial bursa and shoulder pain in rotator cuff diseases. J Orthop Res. 1998. 16(5): 618-621. [DOI] [PubMed] [Google Scholar]
- 33.Itoi E. Kido T. Sano A., et al. Which is more useful, the “full can test” or the “empty can test,” in detecting the torn supraspinatus tendon? Am J Sports Med. 1999. 27(1): 65-68. [DOI] [PubMed] [Google Scholar]
- 34.Hertel R. Ballmer F. T. Lambert S. M., et al. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg. 1996. 5(4): 307-313. [DOI] [PubMed] [Google Scholar]
- 35.Zaslav K. R. Internal rotation resistance strength test: a new diagnostic test to differentiate intra-articular pathology from outlet (Neer) impingement syndrome in the shoulder. J Shoulder Elbow Surg. 2001. 10(1): 23-27. [DOI] [PubMed] [Google Scholar]
- 36.Tennent T. D. Beach W. R. Mayers J. F. A review of the special tests associated with shoulder examination. Part II: laxity, instability and superior labral anterior and posterior (SLAP) lesion. Am J Sports Med. 2003. 31(2): 301-307. [DOI] [PubMed] [Google Scholar]
- 37.Cools A. M. Witvrouw E. E. Decleroq G. A., et al. Evaluation of isokinetic force production and associated muscle activity in the scapular rotators during a protraction-retraction movement in overhead athletes with impingement symptoms. Br J Sports Med. 2004. 38(1): 64-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meister K. Buckley B. Batts J. The posterior impingement sign: diagnosis of rotator cuff and posterior labral tears secondary to internal impingement in overhead athletes. Am J Orthop. 2004. 33(8): 412-415. [PubMed] [Google Scholar]
- 39.Snyder S. J. Pachelli A. F. Del Pizzo W., et al. Partial-thickness rotator cuff tears: results of arthroscopic treatment. Arthroscopy. 1991. 7(1): 1-7. [DOI] [PubMed] [Google Scholar]
- 40.Snyder S. J. Shoulder Arthroscopy. Philadelphia, Lippincott Williams & Wilkins, 2003. [Google Scholar]
- 41.Wiener S. N. Seitz W. H. Sonography of the shoulder in patients with tears of the rotator cuff, accuracy and value for selecting surgical option. AJR Am J Rroentgenol. 1993. 160(1): 103-107. [DOI] [PubMed] [Google Scholar]
- 42.Smith T., O. Back T. Toms A., P., et al. Diagnostic accuracy of ultrasound for rotator cuff tears in adults: a systematic review and meta-analysis. Clin Radiol. 2011. 66(11): 1036-1048. [DOI] [PubMed] [Google Scholar]
- 43.Roy J. S. Braën C. Leblond J., et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med. 2015. 49(20): 1316-1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lenza M. Buchbinder R. Takwoingi Y., et al. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. 2013. 24(9): 1-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990. 254: 64-74. [PubMed] [Google Scholar]
- 46.Modi C. S. Smith C. D. Drew S. J. Partial-thickness articular surface rotator cuff tears in patient over the age of 35: etiology and intra-articular association. Int J Shoulder Surg. 2012. 6(1): 15-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boudreault J. Desmeules F. Roy J. S., et al. The efficacy of oral non-steroidal anti-inflammatory drugs for rotator cuff tendinopathy: a systematic review and meta-analysis. J Rehabil Med. 2014. 46(4): 294-306. [DOI] [PubMed] [Google Scholar]
- 48.Zheng X. Q. Li K. Wei Y. D., et al. Nonsteroidal anti-inflammatory drugs versus corticosteroid for treatment of shoulder pain: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2014. 95(10): 1824-1831. [DOI] [PubMed] [Google Scholar]
- 49.Magra M. Maffulli N. Nonsteroidal antiinflammatory drugs in tendinopathy: friend or foe? Clinical Journal of Sport Medicine. 2006. 16(1): 1-3. [DOI] [PubMed] [Google Scholar]
- 50.Scutt N. Rolf G. C. Scutt A. Glucocorticoids inhibit tenocyte proliferation and tendon progenitor cell recruitment. J Orthop Res. 2006. 24(2): 173-183. [DOI] [PubMed] [Google Scholar]
- 51.Haslerud S. Magnussen L. H. Joensen J., et al. The efficacy of low-level laser therapy for shoulder tendinopathy: a systematic review and meta-analysis of randomized controlled trials. Physiother Res Int. 2015. 20(2): 108-125. [DOI] [PubMed] [Google Scholar]
- 52.Desmeules F. Boudreault J. Roy J.S., et al. The efficacy of therapeutic ultrasound for rotator cuff tendinopathy: a systematic review and meta-analysis. Phys Ther Sport. 2015. 16(3): 276-284. [DOI] [PubMed] [Google Scholar]
- 53.Yu H. Côté P. Shearer H. M., et al. Effectiveness of passive physical modalities for shoulder pain: systematic review by the Ontario protocol for traffic injury management collaboration. Phys Ther. 2015. 95(3): 306-318. [DOI] [PubMed] [Google Scholar]
- 54.Khan K. M. Cook J. L. Bonar F., et al. Histopathology of common tendinopathies. Update and implication for clinical management. Sports Med. 1999. 27(6): 393-408. [DOI] [PubMed] [Google Scholar]
- 55.Ebenbichler G. R. Erdogmus C. B. Resch K. L., et al. Ultrasound therapy for calcific tendinitis of the shoulder. N Engl J Med. 1999. 340: 1533-1538. [DOI] [PubMed] [Google Scholar]
- 56.Kurtais G. Y. Ulus Y. Bilgic A., et al. Adding ultrasound in the management of soft tissue disorder in the shoulder: a randomized placebo-controlled trial. Phys Ther. 2004. 84(4): 336-343. [PubMed] [Google Scholar]
- 57.Likar R. Molnar M. Pipam W., et al. Postoperative transcutaneous electrical nerve stimulation (TENS) in shoulder surgery (randomized, double blind, placebo controlled pilot trial). Schmerz. 2001. 15(3): 158-163. [DOI] [PubMed] [Google Scholar]
- 58.Hengeveld E. Banks K. Maitland’d Peripheral Manipulation, ed 4th Philadelphia, PA: Elsevier Butterworth Heinemann; 2005. [Google Scholar]
- 59.Kachingwe A. F. Philips B. Sletten E., et al. Comparison of manual therapy techniques with therapeutic exercise in the treatment of shoulder impingement: a randomized controlled pilot clinical trial. J Man Manip Ther. 2008. 16(4): 238-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Camarinos J. Marinko L. Effectiveness of manual physical therapy for painful shoulder conditions: a systematic review. J Man Manip Ther. 2009. 17(4): 206-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Southerst D. Yu H. Randhawa K., et al. the effectiveness of manual therapy for the management of musculoskeletal disorders of the upper and lower extremities: a systematic review by the Ontario protocol for traffic injury management (OPTIMa) collaboration. Chiropr Man Ther. 2015. 23(30): 1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Van der Dolder P. A. Roberts D. L. A trial into the effectiveness of soft tissue massage in the treatment of shoulder pain. Aust J Physiother. 2003. 49(3): 183-188. [DOI] [PubMed] [Google Scholar]
- 63.Yang J. L. Chen S. hsieh C. L., et al. Effects and predictors of shoulder muscle massage for patients with posterior shoulder tightness. BMC Musculoskelet Disord. 2012. 13(46): 1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hains G. Descarreaux M. Hains F. Chronic shoulder pain and myofascial origin: a randomized clinical trial using ischemic compression therapy. J Manip Physiol Ther. 2010. 33(5): 362-369. [DOI] [PubMed] [Google Scholar]
- 65.Solem-Bertoft E. Thuomas K. A. Westerberg C. E., et al. The influence of the scapula retraction and protraction on the width of the subacromial space. An MRI study. Clin Orthop Relat Res. 1993. 296: 99-103. [PubMed] [Google Scholar]
- 66.Reinold M. M. Wilk K. E. Fleisig G. S., et al. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J Orthop Sports Phys Ther. 2004. 34(7): 385-394. [DOI] [PubMed] [Google Scholar]
- 67.Ellenbecker T. S. Roeter E. P. Bailie D. S., et al. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc. 2002. 34(12): 2052-2056. [DOI] [PubMed] [Google Scholar]
- 68.Burkhart S. S. Morgan C. D. Kibler W. B. The disabled throwing shoulder: spectrum of pathology, I: pathoanatomy and biomechanics. Arthroscopy. 2003. 19(4): 404-420. [DOI] [PubMed] [Google Scholar]
- 69.Conway J. E. Arthroscopic repair of partial thickness rotator cuff tears and SLAP lesions in professional baseball players. Orthop Clin North Am. 2001. 32(3): 443-456. [DOI] [PubMed] [Google Scholar]
- 70.Fukada H. The management of partial-thickness tears of the rotator cuff. Bone Joint J. 2003. 85(3): 3-11. [DOI] [PubMed] [Google Scholar]
- 71.Zattara M. Bousset S. Posturo-kinetic organization during the early phase of voluntary upper limb movement, 1: normal subjects. J Neurol Neuro-surg Psychiatry. 1988. 51(7):956-965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.McMullen J. Uhl T. L. A kinetic chain approach for shoulder rehabilitation. J Athl Train. 2000. 35(3): 329-337. [PMC free article] [PubMed] [Google Scholar]
- 73.Sciascia A. Cromwell R. kinetic chain rehabilitation: a theoretical framework. Rehabil Res Pract. 2012. 2012:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kibler B. W. Ludewig P. M. McClure P. W., et al. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘scapular summit’. Br J Sports Med. 2013. 47:977-885. [DOI] [PubMed] [Google Scholar]
- 75.Hawkins R. H. Dunlop R. Nonoperative treatment of rotator cuff tears. Clin Orthop Relat Res. 1995. 321:178-188. [PubMed] [Google Scholar]
- 76.Matava M. J. Purcell D. B. Rudzki J. R. Partial-thickness rotator cuff tears. Ma J Sports Med. 2005. 33(9): 1405-1417. [DOI] [PubMed] [Google Scholar]
- 77.Budoff J. E. Nirschl R. P. Guidi E. J. Debridement of partial-thickness tears of the rotator cuff without acromionplasty: long-term follow-up and review of the literature. J Bone Joint Surg Am. 1998. 80(5): 733-748. [DOI] [PubMed] [Google Scholar]
- 78.Kim K. C. Shin H. D. Cha S. M., et al. Clinical outcomes after arhtroscopic trans-tendon suture-bridge technique in partial thickness articular-sided rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2013. 21(5): 1183-1188. [DOI] [PubMed] [Google Scholar]
- 79.Kartus J. Kartus C. Rostågard-Christensen L., et al. Long-term clinical and ultrasound evaluation after arthroscopic and acromionplasty in patients with partial rotator cuff tears. Arthroscopy. 2006. 22(1): 44-49. [DOI] [PubMed] [Google Scholar]
- 80.Wang Y. I. Lu L. Lu Z., et al. Arthroscopic transtendinous repair of articular-sided pasta (partial articular supraspinatus tendon avulsion) injury. Int J Clin Exp Med. 2015. 8(1): 101-107. [PMC free article] [PubMed] [Google Scholar]
- 81.Duralde X. A. McClelland W. B. The clinical results of arthroscopic transtendinous repair of grade III partial articular-sided supraspinatus tendon tears. Arthroscopy. 2012. 28(2): 160-168. [DOI] [PubMed] [Google Scholar]
- 82.Spencer E. E. Jr. Partial-thickness articular surface rotator cuff tears: an all-inside repair technique. Clin Orthop Relat Res. 2010. 468(6): 1514-1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lo I. K. Burkhart S. S. Transtendon arthroscopic repair of partial-thickness articular surface tears of the rotator cuff. Arthroscopy. 2004. 20(2): 214-220. [DOI] [PubMed] [Google Scholar]
- 84.Shin S. J. A comparison of 2 repair techniques for partial-thickness articular-sided rotator cuff tears. Arthroscopy. 2012. 28(1): 25-33. [DOI] [PubMed] [Google Scholar]
- 85.Ide J. Maeda S. Takagi K. Arthroscopic transtendon repair of partial-thickness articular-side tears of the rotator cuff: anatomical and clinical study. Am J Sports Med. 2005. 33(11): 1672-1679. [DOI] [PubMed] [Google Scholar]
- 86.Gulotta L. V. Rodeo S. A. Growth factors for rotator cuff repair. Clin Sports Med. 2009. 28(1): 13-23. [DOI] [PubMed] [Google Scholar]
- 87.Sharma P. Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005. 87(1): 187-202. [DOI] [PubMed] [Google Scholar]
- 88.Oakes BW. Tissue healing and repair: tendons and ligaments. In: Frontera WR. Rehabilitation of Sports Injuries. Boston, MA: Blackwell Science; 2003: 56-98. [Google Scholar]
- 89.Newsham-West R. Nicholson H. Walton M., et al. Long-term morphology of a healing bone-tendon interface: a histological observation in the sheep model. J Anat. 2007. 210(3): 318-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kovacevic D. Rodeo S. A. Biological augmentation of rotator cuff tendon repair. Clin Orthop Relat Res. 2008. 466: 622-633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tauro J. C. Stifness and rotator cuff tears: incidence, arthroscopic findings, and treatment results. Arthroscopy. 2006. 22(6): 581-586. [DOI] [PubMed] [Google Scholar]
- 92.Koo S. S. Burkhart S. S. Rehabilitation following arthroscopic rotator cuff repair. Clin Sports Med. 2010. 29(2): 203-211. [DOI] [PubMed] [Google Scholar]
- 93.Gerber C. Scneeberger A. G. Perren S. M., et al. Experimental rotator cuff repair. A preliminary study. J Bone Joint Surg Am. 1999. 81(9): 1281-1290. [DOI] [PubMed] [Google Scholar]
- 94.Thomopoulos S. Williams G. R. Soslowsky L. J. Tendon to bone healing: differences in biomechanical, structural, and compositional properties due to a range of activity levels. J Biomech Eng. 2003. 125(1): 106-113. [DOI] [PubMed] [Google Scholar]
- 95.De Boer M. D. Selby A. Atherton P., et al. The temporal responses of protein synthesis, gene expression and cell in human quadriceps muscle and patella tendon to disuse. J Physiol. 2007. 585(Pt1): 241-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lavagnino M. Arnoczky S. P. Egerbacher M., et al. Isolated fibrillar damage in tendons stimulates local collagenase mRNA expression and protein synthesis. J Biomech. 2006. 39(13): 2355-2362. [DOI] [PubMed] [Google Scholar]
- 97.Lastayo P. C. Wright P. Jaffe R., et al. Continuous passive motion after repair of the rotator cuff. A prospective outcome study. J Bone Joint Surg Am. 1998. 80(7): 1002-1011. [DOI] [PubMed] [Google Scholar]
- 98.Raab M. G. Rzeszutko D. O’Connor W., et al. Early results of continuous passive motion after rotator cuff repair: a prospective, randomized, blinded, controlled study. Am J Orthop. 1996. 25(3): 214-220. [PubMed] [Google Scholar]
- 99.Shen C. Tang Z. H. Hu J. Z., et al. Does immobilization after arthroscopy rotator cuff repair increase tendon healing? A systematic review and meta-analysis. Arch Orthop Trauma Surg. 2014. 134(9): 1279-1285. [DOI] [PubMed] [Google Scholar]
- 100.Düzgün I. Baltaci G. Turgut E., et al. Effects of slow and accelerated rehabilitation protocols on range of motion after arthroscopic rotator cuff repair. Acta Orthop Traumatol Turc. 2014. 48(6): 642-648. [DOI] [PubMed] [Google Scholar]
- 101.Keener J. D. Galatz L. M. Yamaguchi K. Rehabilitation following arthroscopic rotator cuff repair: a prospective randomized trial. J Bone Joint Surg Am. 2014. 96(1): 11-19. [DOI] [PubMed] [Google Scholar]
- 102.Parsons B. O. Gruson K. I. Chen D. D., et al. Does slower rehabilitation after arthroscopic rotator cuff repair lead to long-term stiffness? J Shoulder Elbow Surg. 2010. 19(7): 1034-1039. [DOI] [PubMed] [Google Scholar]
- 103.Kim Y. S. Chung S. W. Kim J. Y., et al. Is early passive motion exercise necessary after arthroscopic rotator cuff repair? Am J Sports Med. 2012. 40(4): 815-821. [DOI] [PubMed] [Google Scholar]
- 104.Huberty D. P. Schoolfield J. D. Brady P. C., et al. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009. 25(8): 880-890. [DOI] [PubMed] [Google Scholar]
- 105.Aide S. Kwan A. Naylor J. M., et al. Cryotherapy following total knee replacement. 2012. Cochrane Database of Syst Rev. 9: CD007911. [DOI] [PubMed] [Google Scholar]
- 106.Speer K. P. Warren R. F. Horowitz L. The efficacy of cryotherapy in the postoperative shoulder. J Shoulder Elbow Surg. 1996. 5: 62-68. [DOI] [PubMed] [Google Scholar]
- 107.Singh H. Osbahr D. C. Holovacs T. F., et al. The efficacy of continuous cryotherapy in the postoperative shoulder: a prospective, randomized investigation. J Shoulder Elbow Surg. 2001. 10(6): 522-5255. [DOI] [PubMed] [Google Scholar]
- 108.Gulotta L. V. Kovacevic D. Packer J. D., et al. Bone marrow-derived mesenchymal stem cells transduced with scleraxis improve rotator cuff healing in a rat model. Am J Sports Med. 2011. 39: 1282-1289. [DOI] [PubMed] [Google Scholar]
- 109.Oh J. H. Chung S. W. Kim S. H., et al. 2013 Neer award: effect of the adipose-derived stem cell for the improvement of fatty degeneration and rotator cuff healing in rabbit model. J Shoulder Elbow Surg. 2014. 23(4): 445-455. [DOI] [PubMed] [Google Scholar]
- 110.Ellera Gomes J. L. da Silva R. C. Silla L. M., et al. Conventional rotator cuff repair complemented by the aid of mononuclear autologous stem cells. Knee Surg Sports Traumatol Arthrosc. 2012. 20(2): 373-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Cheung E. V. Silverio L. Yao J. Delivered growth factor therapy to improve healing after rotator cuff repair. Stem Cells Cloning.. 2010. 3: 135-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Beitzel K. Solovyova O. Cote M. P., et al. The future role of mesenchymal stem cells in the management of shoulder disorders. Arthroscopy. 2013. 29(10): 1702-1711. [DOI] [PubMed] [Google Scholar]
- 113.Ahmad Z. Henson F. Wardale J., et al. Review article: regenerative techniques for repair of rotator cuff tears. J Orthop Surg 2013. 21(2): 226-231. [DOI] [PubMed] [Google Scholar]
- 114.Mora M. V. Ibán M. A. R. Heredia J. D., et al. Stem cell therapy in the management of shoulder rotator cuff disorders. World J Stem Cells. 2015. 7(4): 691-699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Randelli P. Randelli F. Ragone V., et al. Regenerative medicine in rotator cuff injuries. BioMed Res Int. 2014. 1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Denard P. J. Ladermann A. Burkhart S. S. Prevention and management of stiffness after arthroscopic rotator cuff repair: systematic review and implication for rotator cuff healing. Arthroscopy. 2011. 27(6): 842-848. [DOI] [PubMed] [Google Scholar]
- 117.Millet p.J. Wilkox R.B. 3rd O’Holleran J.D., et al. rehabilitation of the rotator cuff: an evaluation-based approach. J Am Acad Orthop Surg. 2006. 14(11):599-609. [DOI] [PubMed] [Google Scholar]
- 118.Galatz L. M. Sandell L. J. Rothermich S. Y., et al. Characteristics of the rat supraspinatus tendon during tendon-to-bone healing after acute injury. J Orthop Res. 2006. 24(3): 541-550. [DOI] [PubMed] [Google Scholar]
- 119.Khan K. M. Cook J. L. Bonar F., et al. Histopathology of common tendinopathies. Update and implications for clinical management. Sports Med. 1999. 27(6): 393-408. [DOI] [PubMed] [Google Scholar]
- 120.Kannus P Jozsa L. Natri A et al. Effects of training, immobilization and remobilization on tendons. Scand J Med Sci Sports. 1992. 7(2): 67-71. [DOI] [PubMed] [Google Scholar]
- 121.Brislin K. J. Field L. D. Savoie F. H. 3rd. Complications after arthroscopic rotator cuff repair. Arthroscopy. 2007. 23(2): 124-128. [DOI] [PubMed] [Google Scholar]
- 122.Ubinger M. E. Prentice W. E. Guskiewicz K. M. Effect of closed kinetic chain training on neuromuscular control in the upper extremity. J Sport Rehabil. 1999. 8(3): 184-194. [Google Scholar]
- 123.Wilk K. E. Arrigo C. A. Andrews J. R,. Closed and open kinetic chain for the upper extremity. J Sport Rehabil. 1996. 5(1): 88-102. [Google Scholar]
- 124.Lephart S. M. Henry T. J. Riemann B. L., et al. The effects of neuromuscular control exercises on functional stability in the unstable shoulder. J Athl Train. 1998. 33S:15. [Google Scholar]
- 125.Long J. L. Ruberte Thiele R. A. Skendzel J. D., et al. Activation of the shoulder musculature during pendulum exercises and light activities. J Orthop Sports Phys Ther. 2010. 40(4): 230-237. [DOI] [PubMed] [Google Scholar]
- 126.Muraki T. Aoki M. Uchiyama E., et al. Strain on the repaired supraspinatus tendon during manual traction and translational glide mobilization on the glenohumeral joint: a cadaveric biomechanics study. Man Ther. 2007. 12(3): 231-239. [DOI] [PubMed] [Google Scholar]
- 127.Mischke J. J. Emerson Cavchak A. J. courtnet C. A. The effect of sternoclavicular joint mobilization on pain and function in a patient with massive supraspinatus tear. Physiother Theory Pract. 2016. 32(2): 153-158. [DOI] [PubMed] [Google Scholar]
- 128.Surenkok O. Aytar A. Baltaci G. Acute effects of scapular mobilization in shoulder dysfunction: a double-blind randomized placebo-controlled trial. J Sport Rehabil. 2009. 18(4): 493-501. [DOI] [PubMed] [Google Scholar]
- 129.Aytar A. Baltaci G. Uhl T. L., et al. The effects of scapular mobilization in patients with subacromial impingement syndrome: a randomized, double blind, placebo-controlled clinical trial. J Sport Rehabil. 2015. 24(2): 116-129. [DOI] [PubMed] [Google Scholar]
- 130.Fappiano M. Gangaway J. M. K. Aquatic physical therapy improves joint mobility, strength, and edema in lower extremity orthopedic injuries. J Acquatic Phys Ther. 2008. 16(1): 10-15. [Google Scholar]
- 131.Hinman R. S. Heywood S. E. Day A. R. Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Phys Ther. 2007. 87(1): 32-43. [DOI] [PubMed] [Google Scholar]
- 132.Brady B. Redfern J. MacDougal G., et al. The addition of aquatic therapy to rehabilitation following surgical rotator cuff repair: a feasibility study. Physiother Res Int. 2008. 13(3): 153-161. [DOI] [PubMed] [Google Scholar]
- 133.Kelly B. T. Roskin L. A. Kirkendall D. T., et al. Shoulder muscle activation during aquatic and dry land exercises in nonimpaired subjects. J Orthop Sports Phys Ther. 2000. 30(4): 204-210. [DOI] [PubMed] [Google Scholar]
- 134.Smith J. Dahm D. L. Kaufman K. R., et al. Electromyographic activity in the immobilized shoulder girdle musculature during scapulothoracic exercises. Arch phys Med rehabil. 2006. 87(7): 923-927. [DOI] [PubMed] [Google Scholar]
- 135.Charousset C. Grimberg J. Duranthon L D., et al. The time for functional recovery after arthroscopic rotator cuff repair: correlation with tendon healing controlled by computed tomography arthrography. Arthroscopy. 2008. 24(1): 25-33. [DOI] [PubMed] [Google Scholar]
- 136.Carpenter J. E. Thomopoulos S. Flanagan C. L., et al. Rotator cuff defect healing: a biomechanical and histological analysis in animal model. J Shoulder Elbow Surg. 1998. 7(6): 599-605. [DOI] [PubMed] [Google Scholar]
- 137.Cools A. M. Declercq G. A. Cambier D. C., et al. Trapezius activity in intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand J Med Sci Sports. 2007. 17(1): 25-33. [DOI] [PubMed] [Google Scholar]
- 138.Ludewing P. Cook T. Alteration in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000. 80(3): 276-291. [PubMed] [Google Scholar]
- 139.Cools A. M. Dewitte V. Lanszweert F., et al. Rehabilitation of the scapular muscle imbalance: which exercises to prescribe? Am J Sports Med. 2007. 35(10): 1744-1751. [DOI] [PubMed] [Google Scholar]
- 140.Alizadehkhaiyat O. Hawkes G. H. Kemp G. J., et al. Electromyographic analysis of the shoulder girdle musculature during external rotation exercises. The Orthop J Sports Med. 2015. 3(11): 1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Reinold M. M. Escamilla T. Wilk K. E. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009. 39(2): 105-117. [DOI] [PubMed] [Google Scholar]
- 142.Sciascia A. Kuschinsky N. Nitz A J., et al. Electromyographical comparison of four common shoulder exercises in unstable and stable shoulders. Rehabilitation Research and Practice. 2012. 1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ellenbecker T. S. Shoulder Rehabilitation. Non-Operative Treatment. New York: N. Y. Thieme; 2006. [Google Scholar]
- 144.Kisner C. Colby L. A. Therapeutic Exercise: Foundations and Techniques. 6th Ed Philadelphia: F. A. Davies Company; 2012. [Google Scholar]
- 145.Graichen H. Hinterwimmer S. Von Eisenhart-Roth R. V. R., et al. Effect of abduction and adducting muscle activity on gleno-humeral translation, scapular kinematics and subacromial space width in vivo. J Biomech. 2005. 38(4): 755-760. [DOI] [PubMed] [Google Scholar]
- 146.Decker M. J. Hintermeister R. A. Faber K. J., et al. Serratus anterior muscle activity during selected rehabilitation exercises. Am J Sports Med. 1999. 27(6):784-791. [DOI] [PubMed] [Google Scholar]
- 147.Moseley J. B. Jobe F. W. Pink J., et al. Analysis of the scapular muscles during a shoulder rehabilitation program. Am J Sports Med. 1992. 20(2): 128-134. [DOI] [PubMed] [Google Scholar]
- 148.Uhl T. L. Carver T. J. Mattacola C. G., et al. Shoulder musculature activation during upper extremity weight-bearing exercise. J Orthop Sports Phys Ther. 2003. 33(3): 109-117. [DOI] [PubMed] [Google Scholar]
- 149.American College of Sports Medicine. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009. 41(3): 687-708. [DOI] [PubMed] [Google Scholar]
- 150.Kibler W. B. Press J. Sciascia A. The role of core stability in athletic function. Sports Med. 2006. 36(3): 189-198. [DOI] [PubMed] [Google Scholar]
- 151.Wilk K. E. Voight M. L. Keirns M. A., et al. Stretch-shortening drills for the upper extremities: theory and clinical applications. J Orthop Sports Phys Ther. 1993. 17(5): 225-239. [DOI] [PubMed] [Google Scholar]