Abstract
Patients with chronic kidney disease (CKD) form organized beliefs regarding their illness and treatment. These perceptions influence the coping strategies employed by an individual to manage his/her illness and may act as a predictor for his/her willingness to engage in self-management behaviours. While illness perceptions have been identified as predictors of non-adherence, depression and mortality in dialysis patients, there is a paucity of research in CKD patients not requiring renal replacement therapy. This narrative review synthesizes the existing literature regarding the role of illness perceptions and associated clinical and psychosocial outcomes in non-dialysis CKD patients. Studies were identified following database searches of AMED, BNI, CINAHL, EMBASE, Health Business Elite, HMIC, Medline, PsycINFO and Google Scholar in January 2016. Despite the small evidence base, existing studies indicate that negative illness perceptions are associated with disease progression and a number of psychosocial outcomes in non-dialysis CKD patients. Evidence from other clinical populations suggests that illness perceptions are modifiable through psychological intervention, which may be most effective if delivered early before beliefs have the chance to become more established. Therefore, targeting illness perceptions in the earlier stages of CKD may be optimal. Further studies are now required to ascertain the mechanisms through which illness perceptions predict psychosocial and clinical outcomes in CKD patients and to ultimately test the efficacy of illness perception–based interventions.
Keywords: CKD, depression, illness perception, pre-dialysis, quality of life
Introduction
Chronic kidney disease (CKD) is a leading cause of morbidity and mortality worldwide and is associated with a number of adverse comorbidities and a wide range of debilitating symptoms [1]. The preservation of renal function, as well as the treatment and prevention of comorbidities is the ultimate aim of CKD clinical management, which includes blood pressure and glycaemic control and dietary and lifestyle changes [2]. These therapeutic goals place a number of behavioural demands on the patient, with CKD patients having one of the highest daily medication burdens of all chronic conditions [3]. Given this treatment burden and complexity, non-adherence to treatment remains high [4]. However, with non-adherence ultimately being associated with greater all-cause mortality [5], strategies for improving self-management behaviours are vital for optimal clinical outcome.
The integration of self-management programmes into the current CKD care model is of growing interest [6]. In keeping with this more patient-centred approach, understanding patient's perspectives towards their illness and treatment may improve the effectiveness of such programmes, positively impacting on patient outcomes. Illness perceptions are organized patterns of thought that are generated in response to a health threat. These beliefs are theorized within Leventhal's Common Sense Model (CSM) of self-regulation [7] and inform an individual's coping strategy, including their willingness to engage in self-management behaviours such as dietary control and medication adherence. These ‘illness representations' (termed illness schema) are informed by our lay understanding of the condition, information from others and our perceptions towards past and current symptoms of the condition [8]. This information is conceptualized both cognitively and emotionally into the following six dimensions: identity (the name and symptoms that go with it), cause (the perceived cause of the condition), timeline (whether they believe it to be chronic or not), consequences (how the illness will impact on them physically and socially), curability/controllability (the degree to which the illness can be cured or managed and the role the individual plays in making this happen) and coherence (patients understanding of the condition) [9]. In addition to the cognitive appraisal of symptoms and illness, an individual forms parallel emotional responses to a health threat such as feelings of fear or distress [7].
In an extended model of the CSM, Horne and Weinman [10] included specific beliefs regarding treatment (including beliefs about its necessity and concerns/side effects), suggesting that individuals form perceptions regarding their illness as well as the treatment regimen offered. Understanding the interaction between illness and treatment perceptions is important for targeting non-adherence. The importance of illness and treatment perceptions in the predication of non-adherence, depression and mortality among patients with end stage renal disease (ESRD) has been discussed elsewhere [11–14]. However, less is known regarding the role of illness perceptions in CKD patients not requiring renal replacement therapy (RRT), and the development and testing of interventions informed by the CSM still requires attention.
To the best of our knowledge, no studies have evaluated the effectiveness of illness perception interventions to modify psychosocial or clinical outcomes in patients with CKD. Jansen et al. [15] conducted a small pilot study to test the feasibility of a CSM-framed intervention that aimed to encourage activities of daily living in pre-dialysis and newly dialysing patients. The intervention was deemed feasible to deliver and well received by patients. However, the effectiveness of the intervention to encourage patient engagement in activities of daily living was not assessed and a randomized control trial is now required. In addition, a small number of behavioural interventions have used alternative self-regulation theories to address adherence to fluid restrictions in ESRD patients [16, 17]. Results indicated a trend towards better fluid control among the intervention group, although illness perceptions were not specifically addressed within these interventions.
Evidence from other clinical populations suggests that psychological intervention has the potential to alter negative illness perceptions, showing both psychological and clinical benefits for the patient [18]. Broadbent et al. [19] advise delivering illness perception interventions at an early stage, before beliefs have become fully established. This highlights the importance of altering unhelpful perceptions of CKD and associated behaviours in the pre-dialysis setting. Providing an intervention at this stage may encourage positive illness management regimes that have the potential to modify a number of factors related to disease progression and comorbidity. However, before developing illness perception–focused interventions, it is important to gain an initial understanding of how patients with CKD make sense of their illness and how this influences their coping behaviours and outcomes.
Accordingly, the aim of this narrative review is to synthesize the existing literature on illness perceptions and their associations with psychosocial and clinical outcomes in patients with CKD not requiring RRT, to highlight what is already known and inform the future direction of practise and research in this area.
Search strategy
Studies exploring the role of illness perceptions in patients with CKD not requiring RRT were identified by searching the following databases: AMED, BNI, CINAHL, EMBASE, Health Business Elite, HMIC, Medline, PsycINFO and Google Scholar (January 2016).
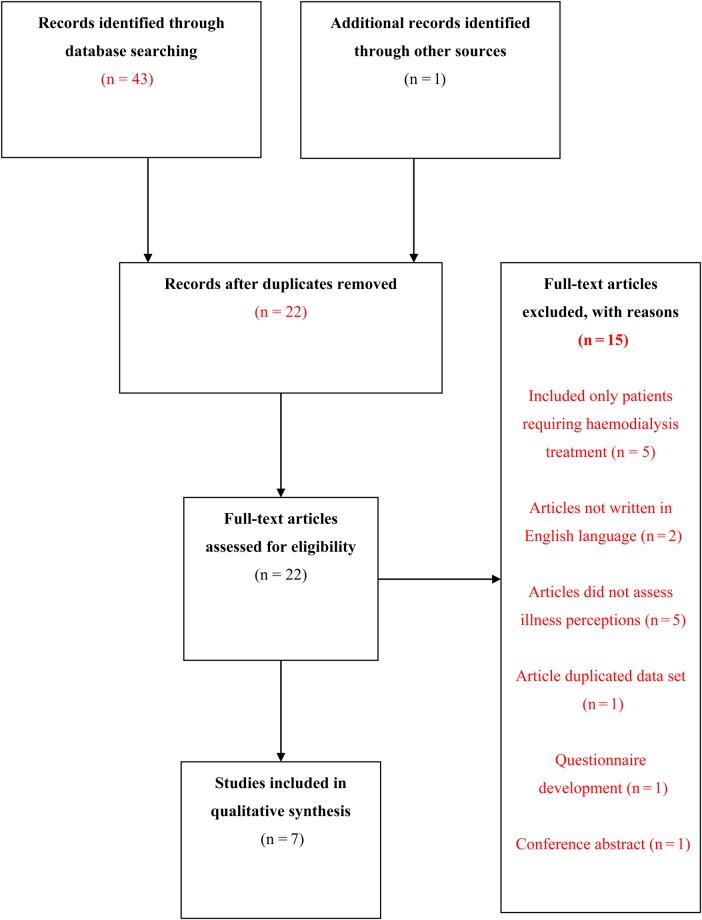
The search terms ‘illness representations’ OR ‘illness representation’ OR ‘disease representations’ OR ‘disease representation’ OR ‘illness perception’ OR ‘illness perceptions’ OR ‘treatment perception’ OR treatment perceptions' OR ‘treatment belief’ OR ‘treatment beliefs' OR ‘disease perceptions’ OR ‘disease perception’ OR ‘illness cognitions’ OR ‘illness cognition’ OR ‘disease cognition’ OR ‘disease cognitions’ OR ‘illness beliefs’ OR ‘illness belief’ and ‘chronic kidney disease’ or ‘CKD’ or ‘pre-dialysis’ or ‘early-stage chronic kidney disease’ or ‘early-stage CKD’ or ‘late-stage CKD’ or ‘late-stage chronic kidney disease’ or ‘moderate CKD’ or ‘moderate chronic kidney disease’ were used to identify relevant studies. Databases were searched individually using both sets of search terms and then combined; references of identified studies were also scanned to identify further studies and duplicates were then removed (Figure 1 shows the flow of information through the search and selection process). We considered English-language articles that included data from patients with CKD stages 1–5 not requiring RRT. Due to the anticipated small evidence base, no search restrictions with regards to time period or study design were imposed.
Fig. 1.
Flow diagram showing literature search and selection.
Findings
The search strategy identified 44 studies, of which 7 met the inclusion criteria and are detailed in Table 1. The majority of studies included participants with moderate to serve CKD. The number of participants in the studies identified ranged from 15 to 416; this is reflective of the qualitative and quantitative approaches included within this narrative review. The studies were mainly cross-sectional in design (n = 5), with the majority of studies eliciting beliefs via validated illness perception questionnaires.
Table 1.
Summary of studies examining the role of illness perceptions in a wide range of outcomes, including psychological well-being, non-adherence, coping strategies and engagement in domains of everyday living
| Study | Objectives | Study design | Participants | Methods | Results |
|---|---|---|---|---|---|
| Knowles et al. 2015, Australia [20] | Examined the relationship between IP, psychological health and coping strategies | Cross-sectional |
N = 29 CKD stages 3b-4 N = 51 End stage kidney disease |
Survey including HPQ, B-IPQ, Brief COPE and HADS | IP directly related to psychological well-being and both maladaptive and adaptive coping strategies |
| Meuleman et al. 2015, The Netherlands [21] | Examined the association between IP at the start of pre-dialysis care and markers of accelerated disease progression | Prospective |
N = 416 CKD stages 4–5 |
Survey IPQ-R and SF-36 at the start of pre-dialysis care; 6-month outcome measure (clinical and biochemical markers of disease progression) and follow-up to the start of dialysis/censoring | After adjustment, IPs (cyclical timeline, negative consequences, personal control, illness coherence and emotional response) were predictors of additional decline in kidney function. Cyclical timeline and negative consequences predicted initiating dialysis sooner |
| Pagels et al. 2015, Sweden [22] | Examined the impact of CKD on patient's IP | Cross-sectional |
N = 7 CKD stages 2–5 N = 54 CKD stages 205 |
Cognitive interviewing to adapt the IPQ-R. Completed the Swedish translation of the IPQ-R | Negative IPs (negative consequences, cyclical, negative emotions, coherence) were associated with greater symptom burden (≥ 8 symptoms) and more advanced stages of disease |
| Wu et al. 2015, Taiwan [23] | Explored lived experiences and IP of patients with advanced CKD | Cross-sectional |
N = 15 CKD stages 4–5 |
Semi-structured interview | IP indicated a strong belief in the chronicity of the illness and positive coping strategies to slow disease progression |
| Lin et al. 2013, Taiwan [24] | Explored the lived experiences and IP of patients in early stages of CKD | Cross-sectional |
N = 15 CKD stages 1–3 |
Semi-structured interview | No renal symptoms/difficulty attributing symptoms to CKD. Consequences related to disease progression and dialysis. Participants who described their illness as incurable more likely to adopt positive coping strategies |
| McManus, 2011, USA [25] | Examined the relationship between IP and adherence to medication | Prospective |
N = 92 CKD stage 3 |
Completed a survey including the IPQ-R and MARS | IP not related to self-reported medication adherence |
| Jansen et al. 2010, The Netherlands [26] | Examined the association between IP, perceived autonomy, self-esteem and labour participation | Cross-sectional |
N = 105 CKD stage 4 |
Survey including B-IPQ, TEQ, autonomy scale of the CAPS-19, current thoughts scale and labour participations defined by Statistical Netherlands Central Agency of Statistics | IPs (consequences, symptoms, concern and emotion) were associated with global autonomy, health-related autonomy and self-esteem. After adjustment, perceived level of treatment disruption was the only significant predictor of self-esteem |
IP, illness perception; B-IPQ, Brief Illness Perceptions Questionnaire; HPQ, Health Perceptions Questionnaire; Brief COPE, Carver Brief Coping Questionnaire; HADS, Hospital Anxiety and Depression Scale; IPQ-R, Revised Illness Perceptions Questionnaire; SF-36, 36-Item Short Form Health Survey; MARS, Medication Adherence Rating Scale; TEQ, Treatment Effects Questionnaire, CAPS-19; Control Autonomy Support Pleasure and Self-realisation Scale.
The Illness Perceptions Questionnaire–Revised (IPQ-R) was used in three of the identified studies and assesses the five agreed domains of illness perceptions as well as measuring properties of some of the subscales (e.g. cure/control is deemed to have multiple components, including personal control and treatment control) [27]. Although widely used, a shorter questionnaire was developed to rapidly assess illness perceptions among very ill patients. The Brief Illness Perception Questionnaire [28] (Brief IPQ) was used in two of the identified studies and is a nine-item scale used to assess illness perceptions and has been shown to have moderate to good associations with the IPQ-R. Semi-structured interviews were utilized by the remaining two studies to elicit illness perceptions. Although illness beliefs are now more commonly assessed using quantifiable measures, qualitative inquiry was employed in the seminal work of Leventhal et al. [29].
Dimensions of illness perceptions and their role in CKD
According to the CSM, patients hold specific beliefs regarding identity, timeline, consequences, cure/control and causes of a disease or illness threat. However, little is known about how patients with CKD represent their illness within these domains. This review will attempt to summarize each dimension as reported within empirical studies identified from the literature (Table 2). These may include extra dimensions to the above list, as the specific domains vary depending on the measurement tool used to assess illness and treatment perceptions. The role of illness perceptions will then be discussed in relation to a wider number of outcomes, including health-related quality of life, psychological well-being, non-adherence, coping strategies, engagement in domains of everyday living and self-regulation (Table 3).
Table 2.
A summary of illness perception domains identified from examining studies of illness perceptions in patients with CKD not requiring RRT
| First author, year of publication, country of origin | Illness identity/symptoms | Timeline acute/chronic | Cyclical timeline | Negative consequences | Emotional identity | Personal control | Illness coherence | Treatment control | Causal identity | Concern |
|---|---|---|---|---|---|---|---|---|---|---|
| Knowles, 2015, Australia | Individual dimensions or illness perception were not reported | |||||||||
| Meuleman, 2015, The Netherlands | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Pagels, 2015, Sweden | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Wu, 2015, Taiwan | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Lin, 2013, Taiwan | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| McManus, 2011, USA | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Jansen, 2010, The Netherlands | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
Table 3.
A summary of the psychosocial and clinical outcomes identified from examining studies of illness perceptions in patients with CKD not requiring RRT
| First author, year of publication, country of origin | Psychological well-being | Disease progression | Coping strategies | Non-adherence | Paid work | Self-regulation |
|---|---|---|---|---|---|---|
| Knowles, 2015, Australia | ✓ | ✓ | ||||
| Meuleman, 2015, The Netherlands | ✓ | |||||
| Pagels, 2015, Sweden | No psychosocial or clinical outcomes were assessed. | |||||
| Wu, 2015, Taiwan | ✓ | ✓ | ||||
| Lin, 2013, Taiwan | ✓ | |||||
| McManus, 2011, USA | ✓ | |||||
| Jansen, 2010, The Netherlands | ✓ | ✓ | ||||
Illness identity—the symptom experience: concurrent symptoms that are attributed to the illness
The findings for this domain were clear: while symptoms were experienced at all stages of disease progression, it was reported that patients in CKD stages 2–3 experience on average 6 symptoms compared with an average of 13 experienced by those with CKD stages 4–5 [22]. This suggests that as CKD progresses, more symptoms are experienced that are perceived by patients to be a consequence of kidney disease. However, patients also report difficulty in attributing their physical symptoms to their CKD [21, 24], which may impact on the strength of their illness identity. Misattributing symptoms of CKD and related treatment regimens could influence self-management behaviours such as medication adherence and physical activity.
Timeline: perceived length of the illness, that is, CKD is chronic, acute or cyclical in nature (variability in symptom experience)
Patients indicated a clear understanding that their illness is chronic, scoring highly on the timeline domain. The presence of chronic symptoms, patient education and learned experiences from other patients contributed to this belief [23]. Patients with advanced CKD were also more likely to perceive their symptoms as more cyclical than those in the earlier stages [22]. This may be due to an increase in various and seemingly unrelated symptoms, which are experienced as a result of disease progression and related comorbidities. Difficultly in attributing symptoms to CKD may lead patients to view their illness as more unpredictable in nature, which could impact upon patients' sense of control and adherence to self-management regimens.
Consequences: the perceived impact of the illness on an individual's life
CKD patients perceived their illness as having a substantial impact on their lives [21, 23–26]. However, participants with an earlier stage of CKD perceived this to a somewhat lesser extent [25]. For example, patients described fears related to the future consequences associated with starting dialysis at a later stage in their disease [24].
Causes: the beliefs regarding the cause of the condition (biological, emotional, environmental and psychological)
Causal beliefs were not homogeneous between the studies reviewed [23–25]. The causes identified included ageing, diet, genetics, stress, long-term use of medication, karma, other chronic diseases, contrast media and use of medication. Differences may be a result of cultural influences, gender, health education level or stage of CKD progression. However, further research will be required to explore this in more detail. Causal beliefs have been shown to impact self-management behaviours in other long-term conditions [30]. For example, early work from Cooper et al. [30] examined the utility of illness perceptions in predicting attendance at cardiac rehabilitation in 137 cardiac patients. Causal perceptions that were not reflective of lifestyle (diet and exercise) and beliefs that the condition was not controllable were predictive of poor attendance [30].
Control/cure: the level to which an individual believes their condition can be controlled or cured by themselves (personal control) or their treatment (treatment control)
The majority of studies reported that CKD patients felt little personal control over their illness [21, 22, 26]. Those who perceived greater personal control were more likely to be male and at an earlier stage of disease progression [25]. In contrast, patients with CKD believe that their treatment positively impacts on their condition, with following medical advice being the best course of management [24, 26]. These review findings support a meta-analysis conducted by French et al. [31] that examined illness perceptions as a predictor of attendance at cardiac rehabilitation in patients following acute myocardial infarction. Patients who perceived their condition as controllable were more likely to attend cardiac rehabilitation.
Coherence: the degree to which an individual understands their illness
Patients with CKD report a moderate understanding of their condition [21]; however, coherence is reduced in patients with more advanced CKD and those who experience more than eight symptoms [22].
Emotional identity: the level to which negative emotions are felt as a result of the illness
Patients reported experiencing moderate feelings of negative emotion as a result of their condition [21, 25, 26]. Perceptions of negative emotions associated with illness increased with symptom burden [22], but the scores reported were not dissimilar to those previously reported in patients with ESRD [32]. This suggests that CKD patients experience emotional distress even in the earlier stages of disease progression.
Concern: the degree to which an individual is concerned about his/her illness
Patients with CKD reported feeling quite worried about their condition [26]; however, concern was only assessed by one study. Levels of concern reported were comparable with a previous study in patients with ESRD requiring dialysis treatment [32]. The identified studies also indicated that patients have a number of concerns regarding the negative effects of treatment, this included concerns related to the potential future need for dialysis treatment [23, 24]. Previous studies have identified additional patient concerns towards medication side effects, beliefs that have been shown to influence medication-taking behaviour.
The relationship between illness perceptions and psychological distress and well-being
Depression has been shown to be associated with progression to dialysis, hospitalization and death in patients with CKD stages 2–5, irrespective of disease severity and the presence of comorbidities [33]. The prevalence of depressive symptoms is high in CKD [34], and insufficient evidence regarding the safety and effectiveness of antidepressants in this group makes it an interesting pathology to investigate.
Illness perceptions have been shown to be important in understanding the trajectory of depression in patients with ESRD [12]. However, illness perceptions and psychological well-being in patients with CKD not requiring RRT is underresearched.
Knowles et al. [20] (Table 1) examined illness perceptions and several measures of psychological well-being, including anxiety and depression, as well as coping strategies in 29 patients with CKD stages 3b–4 and 51 haemodialysis patients. Illness perceptions directly influenced psychological well-being, and correlational analysis showed that depression and anxiety were more highly correlated to illness perceptions than health status. This provides support for the CSM dimensions being a better predictor of psychological distress than a measure of an individual's overall perception of their physical health [20]. Although of interest, this study does not provide information regarding the specific illness perception domains that may underpin this finding. Also, disease severity was not controlled for. Therefore, it is unclear if this finding would remain significant if the study had not included ESRD patients.
Wu et al. [23] (Table 1) explored the lived experiences and illness representations of 15 patients with an advanced stage of CKD. Illness perceptions were elicited using semi-structured interviews in which patients described how feelings of uncertainty regarding ‘if’ and ‘when’ they would have to initiate dialysis contributed to feelings of anxiety and depression. This concern may be indicative of low feelings of personal control and low levels of illness coherence.
Autonomy and its influence on feelings of self-esteem are described within the Self-Determinism Theory [35] as basic psychological needs required for personal growth and well-being. Jansen et al. [26] (Table 1) investigated the relationship between illness perceptions, autonomy, self-esteem and paid work in 109 patients with CKD stage 4. Positive illness and treatment perceptions were associated with perceived greater feelings of autonomy and higher levels of self-esteem. This suggests that the extent to which an individual perceives their illness as a threat may impact on their basic human needs, including autonomy (i.e. freedom to make one's own choices). Findings related to paid employment are discussed later.
Illness perceptions and clinical outcomes
Work in other long-term conditions has shown that negative illness perceptions are associated with greater morbidity over time [36]. A recent study in CKD identified the potential application of illness perceptions as a predictor of disease progression as measured by time to dialysis and loss of kidney function [estimated glomerular filtration rate (eGFR)] during pre-dialysis care. After controlling for a number of clinical covariates [21] (Table 1), five illness perceptions (cyclical timeline, negative consequences, low personal control, low disease coherence and negative feelings) were associated with a greater decline in eGFR. Furthermore, perceived negative consequences and cyclical timeline at baseline were also significant predictors of time to dialysis after scores were adjusted for sociodemographics, clinical and biochemical markers of disease severity and mental health. Even though the mechanism driving this association remains unclear (although non-adherence to self-management regimens is a likely mediator), this research provides novel findings regarding the role of negative illness representations and the detrimental impact these beliefs have on the health of patients with CKD. This work emphasizes the necessity to target negative illness perceptions early in the disease trajectory.
Illness perceptions and treatment non-adherence
As part of the CKD management action plan, patients are required to adhere to a number of treatments [2]. The role of illness perceptions in predicting adherence to medication, diet and fluid intake in patients with ESRD is well acknowledged [14, 37]. However, less is known about how illness perceptions may influence adherent behaviours in CKD patients not requiring RRT.
McManus et al. [25] (Table 1) examined illness perceptions and medication adherence in 92 veterans with CKD stage 3. The authors reported no significant relationship between illness perceptions and medication adherence. However, the sample consisted of predominately males (n = 91) from a single site; therefore, it is unclear if this study is representative of a wider CKD population. This finding also differs from a qualitative study conducted by Rifkin et al. [38] that aimed to explore medication adherence among participants with CKD stages 3–5. While this study did not aim to uncover the role of illness perceptions in a theoretical sense, the findings were reflective of this. For instance, the beliefs that participants held towards their medication were not reflective of conventional medical opinion. Rather, participants described hierarchizing medications based on symptom relief and deprioritizing medications for conditions that were perceived as asymptomatic. In comparison, another qualitative study recently reported that medication adherence was perceived to improve as the illness threat and perceived consequences of non-adherence became stronger [39]. Further research is warranted to explore the role of illness perceptions and non-adherent behaviour in patients with CKD.
Illness perceptions, coping strategies and health behaviour
Patients with CKD often experience a number of stressors as a result of living with a chronic illness, which can cause disruptions to their lives beyond the demands of treatment.
The way in which an individual perceives their illness is likely to inform the cognitive and behavioural strategies undertaken by the patient in order to best manage the health threat or stressor. Knowles et al. [20] (Table 1), in the aforementioned study, reported that illness perceptions were directly linked to methods of coping (adaptive and maladaptive). In particular, maladaptive coping strategies were associated with increased feelings of anxiety and depression. Patients can adopt a number of different coping strategies in an attempt to reduce the health threat; those described among patients with CKD include adopting healthier lifestyle behaviours, the use of complementary or alternative therapies and seeking religious support [23, 24] (Table 1).
Wu et al. [23] (Table 1) reported that patients who had a better understanding of the relationship between CKD and lifestyle factors (illness coherence) described stronger intentions to adopt a healthier lifestyle, including regular physical activity. Similarly, Lin et al. [24] (Table 1), who conducted a qualitative inquiry into the illness representations and coping processes of 15 patients with CKD stages 1–3, reported that participants described changing their lifestyle in hopes of reducing the rate of illness progression. This suggests that patients felt some sense of personal control that they could influence the course of their condition.
There is growing interest in the relationship between illness perceptions and health behaviour change. Illness perceptions (positive identity, cure/control, consequences and coherence) have previously been shown to predict attendance at cardiac rehabilitation in patients following acute myocardial infarction [31] and with structured exercise as the cornerstone of the majority of rehabilitation programmes; this is a theoretically important avenue to explore within the CKD population. Regular exercise has a number of benefits for patients with CKD [40, 41] and is regarded as an integral part of CKD management; however, despite this, patients lead very sedentary lifestyles. We previously explored motivations and barriers to exercise in CKD patients and found that perceptions related to the potential of exercise to cause injury or negatively impact their physical condition (negative treatment perceptions) was a barrier to engagement [42]. Psychological interventions that target negative illness and treatment perceptions have successfully increased physical activity in patients with intermittent claudication [43] and therefore the utility of illness perceptions is likely an important addition to current lifestyle interventions in CKD.
Illness perceptions and engagement in paid work
Psychological well-being is often influenced by participation in various domains of life. However, patients with renal insufficiency report difficulty remaining in paid employment, among other areas [44]. Reduced physical function is a contributor to this, and inability to ambulate has been identified as one of the main factors that renders CKD patients unable to maintain employment [45]. Illness perceptions have been shown to be a predictor of role functions (social, emotional and physical) of the 36-item Short Form Health Survey in patients with rheumatoid arthritis [46] and have also been associated with engagement in paid employment for patients with various illnesses [47]. Currently, however, little is known regarding the relationship between illness perceptions, physical function and engagement in various domains of life (e.g. paid work in patients with CKD).
Jansen et al. [26] (Table 1) investigated whether illness and treatment perception scores of the B-IPQ differed among employed and unemployed CKD patients. No significant association was identified between illness perceptions and employment. Patients who perceived their treatment as more effective and less disruptive to their lives represented a small trend towards being more likely to be in paid employment, but this was not of statistical significance. The small sample size (42% of working age) is likely to have impacted the statistical power; nevertheless, the limited cross-sectional data available make it difficult to determine if illness perceptions are associated with greater engagement in employment. Further research is required to explore the role of illness perceptions and participation in all domains of life. Also, given that physical function is the most pronounced impairment in CKD [48], further research to explore the relationship between illness perceptions and functional ability is warranted to help patients maintain independent living and enjoyment with tasks of everyday living.
Practical implications
Illness perceptions are rarely static and are subject to change with disease progression, as highlighted within this narrative review. Therefore, it is important that illness beliefs be elicited regularly as part of routine practise, which is likely to positively influence disease management strategies, patient quality of life and patient satisfaction during consultations [49]. The use of questionnaires in clinics or open-ended questions such as ‘How do you feel about your symptoms?’ or ‘How well do you feel you understand your condition?’ can be helpful in encouraging patients to describe their illness representations. Simple strategies can be employed to help the patient challenge illness misconceptions or negative thoughts and emotions held towards their chronic disease. For example, for a patient who perceives very little control over his/her condition, it might be useful to help the individual consider the things they do have control over and work together to create an action plan, e.g. taking medication as prescribed, adding regular physical activity into their lives or diet modification as appropriate. This type of psychological intervention has been used successfully to modify illness perceptions in a number of other chronic diseases, including patients recovering from myocardial infarction [18].
Conclusions
This narrative review summarizes what is currently known regarding the role of illness perceptions in patients with CKD. The studies highlight that patients even in the earlier stages of disease experience a number of negative illness perceptions that may ultimately influence their coping actions. Illness perceptions show positive associations with a number of outcomes, including anxiety, depression, coping, autonomy, self-esteem and accelerated disease progression in patients with CKD [20, 21]. Illness perceptions were not related to medication-taking behaviours or paid employment in the studies identified. However, currently there is only a small evidence base within this area, and although this work was carried out methodically, it does not meet the criteria for a full systematic review. To strengthen the evidence base, more longitudinal studies are now required to examine the casual belief mechanisms between illness perceptions and outcomes. The CSM is a dynamic self-regulation model with the potential to inform the development of self-management interventions to target a number of behaviours that will ultimately improve disease management and patient quality of life. With regards to this narrative review, it is clear that the role of illness perceptions is a growing area of interest and early intervention is important in helping patients develop positive disease management strategies that may ultimately slow the rate of disease progression and improve psychosocial outcomes.
Funding
This research was supported by the National Institute for Health Research (NIHR) Diet, Lifestyle & Physical Activity Biomedical Research Unit based at University Hospitals of Leicester and Loughborough University. At the time of writing, A.L.C. was supported by a research grant from Kidney Research UK (IN7/2014).
Conflict of interest statement
None declared.
Acknowledgements
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
References
- 1.Weisbord SD. Symptoms and their correlates in chronic kidney disease. Adv Chronic Kidney Dis 2007; 14: 319–327 [DOI] [PubMed] [Google Scholar]
- 2.Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl 2012; 2: 337–414. [Google Scholar]
- 3.Frishman WH. Importance of medication adherence in cardiovascular disease and the value of once-daily treatment regimens. Cardiol Rev 2007; 15: 257–263 [DOI] [PubMed] [Google Scholar]
- 4.Burnier M, Pruijm M, Wuerzner G et al. Drug adherence in chronic kidney diseases and dialysis. Nephrol Dial Transplant 2015; 30: 39–44 [DOI] [PubMed] [Google Scholar]
- 5.Ricardo AC, Madero M, Yang W et al. Adherence to a healthy lifestyle and all-cause mortality in CKD. Clin J Am Soc Nephrol 2013; 8: 602–609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Welch JL, Johnson M, Zimmerman L et al. Self-management interventions in stages 1 to 4 chronic kidney disease: an integrative review. West J Nurs Res 2015; 37: 652–678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leventhal H, Meyer D, Nerenz D. The common sense representation of illness danger. Contrib Med Psychol 1980; 2: 7–30 [Google Scholar]
- 8.Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychol Health 2003; 18: 141–184 [Google Scholar]
- 9.Hale ED, Treharne GJ, Kitas GD. The common-sense model of self-regulation of health and illness: how can we use it to understand and respond to our patients’ needs? Rheumatology (Oxford) 2007; 46: 904–906 [DOI] [PubMed] [Google Scholar]
- 10.Horne R, Weinman J. Self-regulation and self-management in asthma: exploring the role of illness perceptions and treatment beliefs in explaining non-adherence to preventer medication. Psychol Health 2002; 17: 17–32 [Google Scholar]
- 11.Chilcot J, Wellsted D, Farrington K. Illness perceptions predict survival in haemodialysis patients. Am J Nephrol 2011; 33: 358–363 [DOI] [PubMed] [Google Scholar]
- 12.Chilcot J, Norton S, Wellsted D et al. Distinct depression symptom trajectories over the first year of dialysis: associations with illness perceptions. Ann Behav Med 2013; 45: 78–88 [DOI] [PubMed] [Google Scholar]
- 13.Chilcot J. The importance of illness perception in end-stage renal disease: associations with psychosocial and clinical outcomes. Semin Dial 2012; 25: 59–64 [DOI] [PubMed] [Google Scholar]
- 14.Chilcot J, Wellsted D, Farrington K. Illness representations are associated with fluid nonadherence among hemodialysis patients. J Psychosom Res 2010; 68: 203–212 [DOI] [PubMed] [Google Scholar]
- 15.Jansen DL, Heijmans M, Rijken M et al. The development of and first experiences with a behavioural self-regulation intervention for end-stage renal disease patients and their partners. J Health Psychol 2011; 16: 274–283 [DOI] [PubMed] [Google Scholar]
- 16.Christensen AJ, Moran PJ, Wiebe JS et al. Effect of a behavioral self-regulation intervention on patient adherence in hemodialysis. Health Psychol 2002; 21: 393–397 [DOI] [PubMed] [Google Scholar]
- 17.Howren MB, Kellerman QD, Hillis SL et al. Effect of a behavioral self-regulation intervention on patient adherence to fluid-intake restrictions in hemodialysis: a randomized controlled trial. Ann Behav Med 2015; doi:10.1007/s12160-015-9741-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Petrie KJ, Cameron LD, Ellis CJ et al. Changing illness perceptions after myocardial infarction: an early intervention randomized controlled trial. Psychosom Med 2002; 64: 580–586 [DOI] [PubMed] [Google Scholar]
- 19.Broadbent E, Ellis CJ, Thomas J et al. Further development of an illness perception intervention for myocardial infarction patients: a randomized controlled trial. J Psychosom Res 2009; 67: 17–23 [DOI] [PubMed] [Google Scholar]
- 20.Knowles S, Swan L, Salzberg M et al. Exploring the relationships between health status, illness perceptions, coping strategies and psychological morbidity in a chronic kidney disease cohort. Am J Med Sci 2014; 348: 271–276 [DOI] [PubMed] [Google Scholar]
- 21.Meuleman Y, de Goeij MC, Halbesma N et al. Illness perceptions in patients on predialysis care: associations with time until start of dialysis and decline of kidney function. Psychosom Med 2015; 77: 946–954 [DOI] [PubMed] [Google Scholar]
- 22.Pagels AA, Soderquist BK, Heiwe S. Differences in illness representations in patients with chronic kidney disease. J Ren Care 2015; 41: 146–155 [DOI] [PubMed] [Google Scholar]
- 23.Wu CC, Lin CC, Hsieh HF et al. Lived experiences and illness representation of Taiwanese patients with late-stage chronic kidney disease. J Health Psychol 2015; doi:10.1177/1359105315587134 [DOI] [PubMed] [Google Scholar]
- 24.Lin CC, Chen MC, Hsieh HF et al. Illness representations and coping processes of Taiwanese patients with early-stage chronic kidney disease. J Nurs Res 2013; 21: 120–128 [DOI] [PubMed] [Google Scholar]
- 25.McManus S. Illness representation and medication adherence of patients with chronic kidney disease. PhD thesis Scholar Works, Indiana University-Purdue University Indianapolis (IUPUI) 2011 [Google Scholar]
- 26.Jansen DL, Grootendorst DC, Rijken M et al. Pre-dialysis patients’ perceived autonomy, self-esteem and labor participation: associations with illness perceptions and treatment perceptions. A cross-sectional study. BMC Nephrol 2010; 11: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moss-Morris R, Weinman J, Petrie K et al. The revised illness perception questionnaire (IPQ-R). Psychol Health 2002; 17: 1–16 [Google Scholar]
- 28.Broadbent E, Petrie KJ, Main J et al. The brief illness perception questionnaire. J Psychosom Res 2006; 60: 631–637 [DOI] [PubMed] [Google Scholar]
- 29.Meyer D, Leventhal H, Gutmann M. Common-sense models of illness: the example of hypertension. Health Psychol 1985; 4: 115. [DOI] [PubMed] [Google Scholar]
- 30.Cooper A, Lloyd G, Weinman J et al. Why patients do not attend cardiac rehabilitation: role of intentions and illness beliefs. Heart 1999; 82: 234–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.French DP, Cooper A, Weinman J. Illness perceptions predict attendance at cardiac rehabilitation following acute myocardial infarction: a systematic review with meta-analysis. J Psychosom Res 2006; 61: 757–767 [DOI] [PubMed] [Google Scholar]
- 32.Jansen DL, Heijmans MJ, Rijken M et al. Illness perceptions and treatment perceptions of patients with chronic kidney disease: different phases, different perceptions? Br J Health Psychol 2013; 18: 244–262 [DOI] [PubMed] [Google Scholar]
- 33.Hedayati SS, Minhajuddin AT, Afshar M et al. Association between major depressive episodes in patients with chronic kidney disease and initiation of dialysis, hospitalization, or death. JAMA 2010; 303: 1946–1953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palmer S, Vecchio M, Craig JC et al. Prevalence of depression in chronic kidney disease: systematic review and meta-analysis of observational studies. Kidney Int 2013; 84: 179–191 [DOI] [PubMed] [Google Scholar]
- 35.Deci EL, Ryan RM. Handbook of Self-Determination Research. Rochester, NY: University Rochester Press; 2002 [Google Scholar]
- 36.Norton S, Hughes LD, Chilcot J et al. Negative and positive illness representations of rheumatoid arthritis: a latent profile analysis. J Behav Med 2014; 37: 524–532 [DOI] [PubMed] [Google Scholar]
- 37.O'Connor SM, Jardine AG, Millar K. The prediction of self-care behaviors in end-stage renal disease patients using Leventhal's self-regulatory model. J Psychosom Res 2008; 65: 191–200 [DOI] [PubMed] [Google Scholar]
- 38.Rifkin DE, Laws MB, Rao M et al. Medication adherence behavior and priorities among older adults with CKD: a semistructured interview study. Am J Kidney Dis 2010; 56: 439–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McKillop G, Joy J. Patients’ experience and perceptions of polypharmacy in chronic kidney disease and its impact on adherent behaviour. J Ren Care 2013; 39: 200–207 [DOI] [PubMed] [Google Scholar]
- 40.Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev 2011; 10; CD003236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gould DW, Graham-Brown MP, Watson EL et al. Physiological benefits of exercise in pre-dialysis chronic kidney disease. Nephrology (Carlton) 2014; 19: 519–527 [DOI] [PubMed] [Google Scholar]
- 42.Clarke AL, Young HM, Hull KL et al. Motivations and barriers to exercise in chronic kidney disease: a qualitative study. Nephrol Dial Transplant 2015; 30: 1885–1892 [DOI] [PubMed] [Google Scholar]
- 43.Cunningham MA, Swanson V, O'Carroll RE et al. Randomized clinical trial of a brief psychological intervention to increase walking in patients with intermittent claudication. Br J Surg 2012; 99: 49–56 [DOI] [PubMed] [Google Scholar]
- 44.Tong A, Sainsbury P, Chadban S et al. Patients’ experiences and perspectives of living with CKD. Am J Kidney Dis 2009; 53: 689–700 [DOI] [PubMed] [Google Scholar]
- 45.Muehrer RJ, Schatell D, Witten B et al. Factors affecting employment at initiation of dialysis. Clin J Am Soc Nephrol 2011; 6: 489–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lochting I, Fjerstad E, Garratt AM. Illness perceptions in patients receiving rheumatology rehabilitation: association with health and outcomes at 12 months. BMC Musculoskelet Disord 2013; 14: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hoving J, Van der Meer M, Volkova A et al. Illness perceptions and work participation: a systematic review. Int Arch Occup Environ Health 2010; 83: 595–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chin HJ, Song YR, Lee JJ et al. Moderately decreased renal function negatively affects the health-related quality of life among the elderly Korean population: a population-based study. Nephrol Dial Transplant 2008; 23: 2810–2817 [DOI] [PubMed] [Google Scholar]
- 49.Petrie KJ, Jago LA, Devcich DA. The role of illness perceptions in patients with medical conditions. Curr Opin Psychiatry 2007; 20: 163–167 [DOI] [PubMed] [Google Scholar]