Abstract
BACKGROUND
In the United States, an estimated 48 million individuals live without health insurance. The purpose of the current study was to explore the variation in insurance status by patient demographics and tumor site among nonelderly adult patients with cancer.
METHODS
A total of 688,794 patients aged 18 to 64 years who were diagnosed with one of the top 25 incident cancers (representing 95% of all cancer diagnoses) between 2007 and 2010 in the Surveillance, Epidemiology, and End Results (SEER) database were analyzed. Patient characteristics included age, race, sex, marital status, and rural or urban residence. County-level demographics included percent poverty level. Insurance status was defined as having non-Medicaid insurance, Medicaid coverage, or no insurance.
RESULTS
On multivariate logistic regression analyses, younger age, male sex, nonwhite race, being unmarried, residence in counties with higher levels of poverty, and rural residence were associated with being uninsured versus having non-Medicaid insurance (all P <.001). The highest rates of non-Medicaid insurance were noted among patients with prostate cancer (92.3%), melanoma of the skin (92.5%), and thyroid cancer (89.5%), whereas the lowest rates of non-Medicaid insurance were observed among patients with cervical cancer (64.2%), liver cancer (67.9%), and stomach cancer (70.9%) (P <.001). Among uninsured individuals, the most prevalent cancers were lung cancer (14.9%), colorectal cancer (12.1%), and breast cancer (10.2%) (P <.001). Lung cancer caused the majority of cancer mortality in all insurance groups.
CONCLUSIONS
Rates of insurance coverage vary greatly by demographics and by cancer type. The expansion of health insurance coverage would be expected to disproportionally benefit certain demographic populations and cancer types.
Keywords: insurance, Surveillance, Epidemiology, and End Results (SEER), cancer, disparities
INTRODUCTION
Cancer is the second leading cause of death in the United States, and the leading cause of death among individuals aged 45 to 64 years.1 Previous studies have shown improved outcomes in patients with cancer who have non-Medicaid insurance compared with those with Medicaid coverage or no insurance.2–4 For example, our group recently found that patients with non-Medicaid insurance present at an earlier stage of disease, were more likely to receive cancer-directed surgery and/ or radiotherapy, and were less likely to die of their illness compared with those with non-Medicaid Insurance.4 Nonetheless, 15.4% of the population, or 48 million individuals, live without health insurance,5 with another 62 million having Medicaid coverage.6 The Patient Protection and Affordable Care Act (PPACA) (Public Law 111–148), which was signed into law in March 2010 with full implementation expected by 2020, aims to expand both public and private health insurance.
The Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute assembles information regarding cancer cases, local treatment, patient demographics, and survival in the United States. This past year, the program released information regarding patient-level insurance status. The registries participating in the SEER program capture approximately 97% of incident cases7 and the population residing within the areas served by the SEER cancer registries is comparable to the general US population because the catchments for the 18 SEER registries comprise approximately 28% of the US population.8
To elucidate which populations of patients with cancer might benefit the most from the upcoming expansion of public and private health insurance, we used the SEER database to explore differences in demographics associated with insurance status among nonelderly adults diagnosed with cancer. In addition, we sought to explore the variability in insurance status by cancer type.
MATERIALS AND METHODS
Description of the Study Cohort
A total of 1,481,311 patients who were diagnosed with one of the top 25 types of cancer (breast, lung, colorectal, head and neck, prostate, liver, non-Hodgkin lymphoma, kidney, cervix, endometrium, thyroid, leukemia, pancreas, bladder, ovary, melanoma of the skin, brain, stomach, testicle, esophagus, Hodgkin lymphoma, anus, small intestine, vulva, and thymus) between January 1, 2007 and December 31, 2010 were identified in the public-use SEER database using SEER*Stat software (version 8.1.2).9 The database began collecting information regarding insurance status in 2007. Patients were excluded if their age at the time of diagnosis was <18 years (10,836 patients) or >64 years (778,859 patients), or if the patients were not actively followed (diagnosed using death certificates or autopsy results only) (2822 patients). It is interesting to note that the SEER program considers designation of insurance in patients aged ≥65 years to be unreliable because this is the age at which individuals become eligible for Medicare. Because this data set is within the public domain and all patient information is deidentified, it was deemed exempt from review by the Institutional Review Board.
Key Covariates
Patient characteristics included age, race, sex, marital status, and urban versus rural residence. “Married” status, as defined by the SEER database, includes common-law marriages. “Urban” was defined as big metropolitan, metropolitan, or urban residence and “rural” was defined as less urban or rural residence using SEER definitions. Insurance status was defined as non-Medicaid insurance (“insured” or “insured/no specifics”), Medicaid coverage (“any Medicaid”), or uninsured. The SEER definition for insured includes those with non-Medicaid coverage (managed care, health maintenance organization, or preferred provider organization) or Medicare, as well as coverage from the military or Veterans Affairs at the time of initial diagnosis and/or treatment. Patients with unknown insurance status were excluded from further analysis. Finally, the county-level percent below the federal poverty level was obtained from linked data.10
Statistical Analysis
For each of the top 25 incident cancers, we calculated the percentage of patients with non-Medicaid insurance, Medicaid coverage, and without insurance. Moreover, we calculated the estimated annual national incidence and mortality of each cancer by insurance. We did this by averaging annual incidence and mortality rates for patients with cancer who were diagnosed between 2007 and 2010 on the SEER database and extrapolating these to the US population (the SEER database broadly represents 28% of the US population, and is considered broadly representative of the US population).11 Multivariate logistic regression models were used to determine patient demographic factors (including age, race, sex, marital status, urban vs rural residence, and county poverty level) associated with lack of insurance versus non-Medicaid coverage as well as Medicaid coverage versus non-Medicaid coverage. The estimated odds ratio is reported.
A P value ≤.001 was considered to be statistically significant. Statistical tests were based on a 2-sided significance level. Data analysis was performed using STATA/ IC statistical software (version 12.1; StataCorp, College Station, Tex).
RESULTS
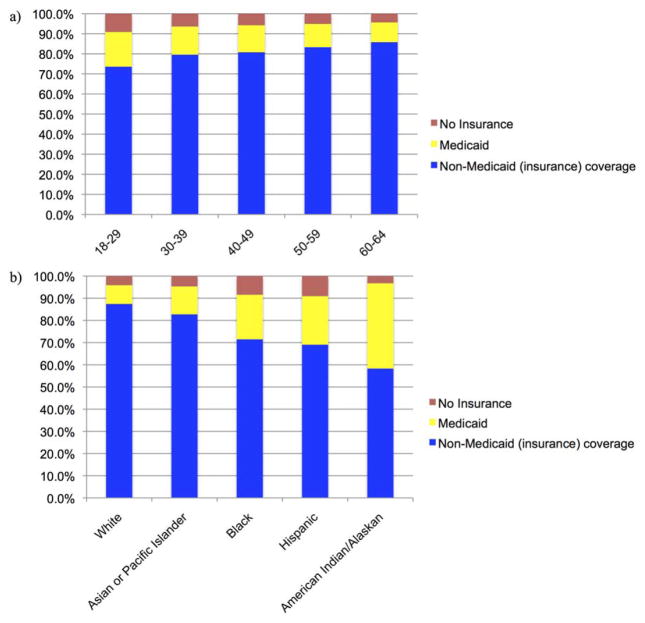
Patient demographics for the top 25 incident cancers are outlined in Table 1. Of the 688,794 eligible patients, 536,297 (77.9%) had non-Medicaid insurance, 76,516 (11.1%) had Medicaid coverage, and 33,798 (4.9%) did not have insurance. A total of 42,183 patients (6.1%) had unknown insurance status and were excluded from further analysis. Males and females demonstrated approximately equal rates of non-Medicaid insurance, but males were more likely to be uninsured (5.8% vs 4.7%) whereas females were more likely to have Medicaid coverage (13.3% vs 10.2%) (P<.001). Non-Medicaid insurance rates were found to increase with age whereas uninsured and Medicaid rates decreased with age (Fig. 1a) (P <.001). Nonwhite individuals represented 45.9% of the uninsured cohort and 50.8% of the Medicaid cohort, but only 27.2% of the non-Medicaid insurance cohort (P <.001). Rates of non-Medicaid insurance were highest among white individuals, whereas uninsured and Medicaid rates were highest among Hispanics and American Indians/Alaska Natives, respectively (Fig. 1b) (P <.001). Rates of non-Medicaid insurance were greater for married individuals (90.5%) compared with unmarried individuals (69.8%) (P <.001), as well as for individuals with urban residence (83.9%) compared with those residing in a rural area (75.8%) (P <.001).
TABLE 1.
Patient Characteristics
| All patients | All Patients No.
|
Non-Medicaid (Insurance) Coverage No.
|
No Insurance No.
|
Medicaid No.
|
P | ||||
|---|---|---|---|---|---|---|---|---|---|
| 646,611 | (100.0%) | 536,297 | (82.9%) | 33,798 | (5.2%) | 76,516 | (11.8%) | ||
| Age, y | NA | ||||||||
| Median (range) | 55 (18–64) | 55 (18–64) | 53 (18–64) | 54 (18–64) | |||||
| 18–29 | 20,523 | (3.2%) | 15,104 | (73.6%) | 1872 | (9.1%) | 3547 | (17.3%) | <.001 |
| 30–39 | 44,170 | (6.8%) | 35,160 | (79.6%) | 2827 | (6.4%) | 6183 | (14.0%) | |
| 40–49 | 125,677 | (19.4%) | 101,488 | (80.8%) | 7263 | (5.8%) | 16,926 | (13.5%) | |
| 50–59 | 273,901 | (42.4%) | 228,106 | (83.3%) | 13,940 | (5.1%) | 31,855 | (11.6%) | |
| ≥60 | 182,340 | (28.2%) | 156,439 | (85.8%) | 7896 | (4.3%) | 18,005 | (9.9%) | |
| Sex | <.001 | ||||||||
| Female | 337,010 | (52.1%) | 276,268 | (82.0%) | 15,832 | (4.7%) | 44,910 | (13.3%) | |
| Male | 309,601 | (47.9%) | 260,029 | (84.0%) | 17,966 | (5.8%) | 31,606 | (10.2%) | |
| Race | <.001 | ||||||||
| White | 441,956 | (68.3%) | 386,265 | (87.4%) | 18,155 | (4.1%) | 37,536 | (8.5%) | |
| Black | 79,336 | (12.3%) | 56,697 | (71.5%) | 6678 | (8.4%) | 15,961 | (20.1%) | |
| Hispanic | 72,714 | (11.2%) | 50,203 | (69.0%) | 6585 | (9.1%) | 15,926 | (21.9%) | |
| Asian or Pacific Islander | 42,644 | (6.6%) | 35,270 | (82.7%) | 1991 | (4.7%) | 5383 | (12.6%) | |
| American Indian/Alaska Native | 3702 | (0.6%) | 2158 | (58.3%) | 121 | (3.3%) | 1423 | (38.4%) | |
| Unknown | 6259 | (1.0%) | 5704 | (91.1%) | 268 | (4.3%) | 287 | (4.6%) | |
| Marital status | <.001 | ||||||||
| Single | 228,095 | (35.3%) | 159,299 | (69.8%) | 19,560 | (8.6%) | 49,236 | (21.6%) | |
| Married | 387,655 | (60.0%) | 351,010 | (90.5%) | 12,659 | (3.3%) | 23,986 | (6.2%) | |
| Unknown | 30,861 | (4.8%) | 25,988 | (84.2%) | 1579 | (5.1%) | 3294 | (10.7%) | |
| Percent of county below federal poverty level | NA | ||||||||
| Mean | 2.5 | 2.4 | 2.8 | 2.9 | |||||
| SD | 1.1 | 1.1 | 1.0 | 1.0 | |||||
| <10% | 153,993 | (23.8%) | 137,916 | (89.6%) | 5588 | (3.6%) | 10,489 | (6.8%) | <.001 |
| 10–12.99% | 153,576 | (23.8%) | 132,736 | (86.4%) | 6168 | (4.0%) | 14,672 | (9.6%) | |
| 13–16.49% | 194,716 | (30.1%) | 155,554 | (79.9%) | 12,039 | (6.2%) | 27,123 | (13.9%) | |
| ≥16.5% | 144,253 | (22.3%) | 110,033 | (76.3%) | 9993 | (6.9%) | 24,227 | (16.8%) | |
| Unknown | 73 | (0.0%) | 58 | (79.5%) | 10 | (13.7%) | 5 | (6.8%) | |
| Residence | <.001 | ||||||||
| Urban | 571,135 | (88.4%) | 479,411 | (83.9%) | 28,139 | (4.9%) | 63,585 | (11.1%) | |
| Rural | 74,650 | (11.6%) | 56,603 | (75.8%) | 5643 | (7.6%) | 12,404 | (16.6%) | |
| Unknown | 73 | (0.0%) | 58 | (79.5%) | 10 | (13.7%) | 5 | (6.8%) | |
| Registries grouped by region | <.001 | ||||||||
| Northeast | 103,553 | (16.0%) | 90,274 | (79.5%) | 6344 | (5.6%) | 6935 | (6.1%) | |
| South | 111,749 | (17.3%) | 86,487 | (72.4%) | 10,075 | (8.4%) | 15,187 | (12.7%) | |
| Midwest | 99,899 | (15.4%) | 83,552 | (78.1%) | 5109 | (4.8%) | 11,238 | (10.5%) | |
| West/Hawaii | 331,410 | (51.3%) | 275,984 | (79.1%) | 12,270 | (3.5%) | 43,156 | (12.4%) | |
| Year of diagnosis | <.001 | ||||||||
| 2007 | 159,044 | (24.6%) | 133,807 | (79.1%) | 8081 | (4.8%) | 17,156 | (10.1%) | |
| 2008 | 161,482 | (25.0%) | 135,008 | (78.6%) | 8098 | (4.7%) | 18,376 | (10.7%) | |
| 2009 | 164,881 | (25.5%) | 136,062 | (77.6%) | 8764 | (5.0%) | 20,055 | (11.4%) | |
| 2010 | 161,204 | (24.9%) | 131,420 | (76.2%) | 8855 | (5.1%) | 20,929 | (12.1%) | |
Abbreviations: NA, not applicable; SD, standard deviation.
Figure 1.
Distribution of insurance status among patients with the top 25 cancer types is shown by a) age and b) race.
Geographic/Time Variations
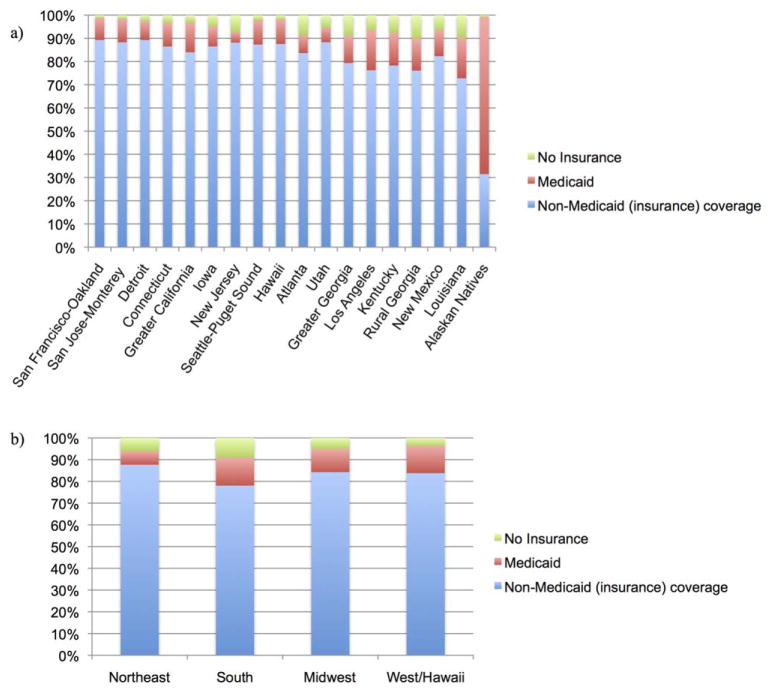
Uninsured individuals and individuals with Medicaid coverage were most likely to have residence in counties with poverty rates >16.5%, whereas individuals with non-Medicaid insurance were most likely to have residence in counties with poverty rates <10.0% (P <.001). Of the 18 SEER registries, the San Francisco-Oakland registry represented the highest rate of non-Medicaid insurance (89.2%), whereas the Alaska Native registry represented the lowest rate of non-Medicaid insurance (Fig. 2a) (29.9%) (P <.001). The highest rates of uninsurance were noted in the Rural Georgia registry (10.2%), whereas the lowest uninsured rates were observed in the Alaska Native registry (0.8%) (P <.001). The Alaska Native registry represented the highest rate of Medicaid coverage (69.3%), whereas the New Jersey registry represented the lowest rate of Medicaid coverage (5.0%) (P <.001). Grouping the registries by region, the rate of non-Medicaid insurance was highest in the Northeastern registries whereas uninsured and Medicaid rates were highest in the Southern registries (Fig. 2b) (P <.001). The rate of non-Medicaid insurance steadily decreased from 79.1% in 2007 to 76.2% in 2010. Over the same time period, uninsured rates increased from 4.8% to 5.1% and rates of Medicaid coverage increased from 10.1% to 12.1% (P < .001).
Figure 2.
Distribution of insurance status among patients with the top 25 cancer types is shown by a) registry and b) region.
Multivariate Analysis
On multivariate analysis, younger age, male sex, nonwhite race, being unmarried, residence in counties with higher levels of poverty, rural residence, residence in a Southern registry, and later year of diagnosis were all found to be associated with being uninsured versus having non-Medicaid insurance (all P <.001) (Table 2). Younger age, female sex, nonwhite race, being unmarried, residence in a county with higher levels of poverty, rural residence, residence in a non-Northeastern registry, and a later year of diagnosis were found to be associated with having Medic-aid coverage versus Non-Medicaid insurance (all P <.001) (Table 3). Younger age, male sex, being married, urban residence, residence in a Northeastern registry, and an earlier year of diagnosis were associated with being uninsured versus having Medicaid coverage (all P <.001) (Table 4).
TABLE 2.
Multivariate Logistic Regression for Predictors of Lack of Insurance Versus Non-Medicaid Insurance
| OR | 95% CI | P | |
|---|---|---|---|
| Age | |||
| Continuous | 0.99 | 0.99–0.99 | <.001 |
| Sex | |||
| Male | 1.31 | 1.28–1.34 | <.001 |
| Female | 1 | ||
| Race | |||
| White | 1 | ||
| Black | 1.52 | 1.47–1.57 | <.001 |
| Hispanic | 3.34 | 3.23–3.45 | <.001 |
| Asian or Pacific Islander | 2.01 | 1.91–2.11 | <.001 |
| American Indian/Alaska Native | 1.43 | 1.18–1.74 | <.001 |
| Unknown | 0.99 | 0.88–1.13 | .93 |
| Marital status | |||
| Single | 3.05 | 2.97–3.12 | <.001 |
| Married | 1 | ||
| Percent of county below federal poverty level | |||
| <10% | 1 | ||
| 10–12.99% | 1.22 | 1.18–1.27 | <.001 |
| 13–16.49% | 1.95 | 1.89–2.03 | <.001 |
| ≥16.5% | 1.61 | 1.55–1.68 | <.001 |
| Residence | |||
| Urban | 1 | ||
| Rural | 1.66 | 1.61–1.72 | <.001 |
| Registries grouped by region | |||
| Northeast | 1 | ||
| South | 1.20 | 1.16–1.25 | <.001 |
| Midwest | 0.72 | 0.69–0.75 | <.001 |
| West/Hawaii | 0.40 | 0.39–0.41 | <.001 |
| Year of diagnosis | |||
| 2007 | 1 | ||
| 2008 | 0.98 | 0.95–1.01 | .16 |
| 2009 | 1.05 | 1.02–1.08 | .006 |
| 2010 | 1.09 | 1.06–1.13 | <.001 |
Abbreviations: 95% CI, 95% confidence interval; OR, odds ratio.
TABLE 3.
Multivariate Logistic Regression for Predictors of Medicaid Insurance Versus Non-Medicaid Insurance
| OR | 95% CI | P | |
|---|---|---|---|
| Age | |||
| Continuous | 0.99 | 0.99–0.99 | <.001 |
| Sex | |||
| Male | 1 | ||
| Female | 1.24 | 1.22–1.26 | <.001 |
| Race | |||
| White | 1 | ||
| Black | 2.12 | 2.07–2.17 | <.001 |
| Hispanic | 3.07 | 3.00–3.15 | <.001 |
| Asian or Pacific Islander | 1.92 | 1.86–1.98 | <.001 |
| American Indian/Alaska Native | 3.36 | 3.09–3.66 | <.001 |
| Unknown | 0.45 | 0.40–0.51 | <.001 |
| Marital status | |||
| Single | 3.90 | 3.83–3.96 | <.001 |
| Married | 1 | ||
| Percent of county below federal poverty level | |||
| <10% | 1 | ||
| 10–12.99% | 1.36 | 1.33–1.40 | <.001 |
| 13–16.49% | 1.74 | 1.70–1.79 | <.001 |
| ≥16.5% | 2.08 | 2.02–2.14 | <.001 |
| Residence | |||
| Urban | 1 | ||
| Rural | 1.82 | 1.77–1.86 | <.001 |
| Registries grouped by region | |||
| Northeast | 1 | ||
| South | 1.31 | 1.26–1.35 | <.001 |
| Midwest | 1.24 | 1.19–1.28 | <.001 |
| West/Hawaii | 1.35 | 1.31–1.39 | <.001 |
| Year of diagnosis | |||
| 2007 | 1 | ||
| 2008 | 1.04 | 1.02–1.06 | .001 |
| 2009 | 1.12 | 1.10–1.15 | <.001 |
| 2010 | 1.20 | 1.17–1.23 | <.001 |
Abbreviations: 95% CI, 95% confidence interval; OR, odds ratio.
TABLE 4.
Multivariate Logistic Regression for Predictors of Lack of Insurance Versus Medicaid Insurance
| OR | 95% CI | P | |
|---|---|---|---|
| Age | |||
| Continuous | 0.995 | 0.994–0.997 | <.001 |
| Sex | |||
| Male | 1.64 | 1.60–1.68 | <.001 |
| Female | 1 | ||
| Race | |||
| White | 1 | ||
| Black | 0.69 | 0.66–0.71 | <.001 |
| Hispanic | 1.06 | 1.02–1.10 | .005 |
| Asian or Pacific Islander | 0.99 | 0.93–1.05 | .774 |
| American Indian/Alaska Native | 0.44 | 0.36–0.54 | <.001 |
| Unknown | 2.04 | 1.71–2.43 | <.001 |
| Marital status | |||
| 1 | |||
| Married | 1.37 | 1.33–1.41 | <.001 |
| Percent of county below federal poverty level | |||
| <10% | 1 | ||
| 10–12.99% | 0.87 | 0.83–0.92 | <.001 |
| 13–16.49% | 1.17 | 1.12–1.23 | <.001 |
| ≥16.5% | 0.78 | 0.74–0.82 | <.001 |
| Residence | |||
| Urban | 1.07 | 1.03–1.12 | <.001 |
| Rural | 1 | ||
| Registries grouped by region | |||
| Northeast | 1 | ||
| South | 0.92 | 0.87–0.97 | .001 |
| Midwest | 0.55 | 0.52–0.58 | <.001 |
| West/Hawaii | 0.28 | 0.27–0.30 | <.001 |
| Year of diagnosis | |||
| 2007 | 1 | ||
| 2008 | 0.93 | 0.89–0.96 | <.001 |
| 2009 | 0.92 | 0.89–0.96 | <.001 |
| 2010 | 0.88 | 9.84–0.91 | <.001 |
Abbreviations: 95% CI, 95% confidence interval; OR, odds ratio.
Distribution by Cancer Type
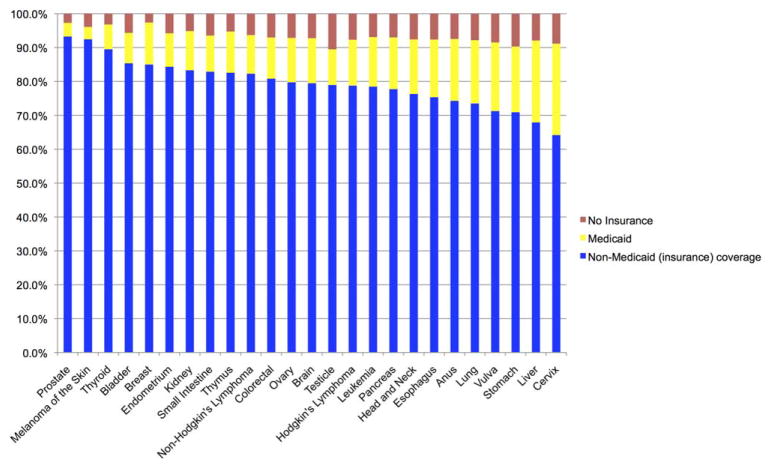
The cancer types with the highest rates of non-Medicaid insurance were prostate cancer (92.3%), melanoma of the skin (92.5%), and thyroid cancer (Fig. 3) (89.5%). The lowest rates of non-Medicaid insurance were observed among individuals with cervical cancer (64.2%), liver cancer (67.9%), and stomach cancer (70.9%). The highest uninsured rates were noted among patients with testicular cancer (10.5%), stomach cancer (9.7%), and cervical cancer (8.9%), whereas the lowest uninsured rates were noted among patients with thyroid cancer (3.2%), prostate cancer (2.7%), and breast cancer (2.6%). The highest rates of individuals with Medicaid coverage were observed in patients with cervical cancer (27.0%), liver cancer (24.1%), and vulvar cancer (20.3%), whereas the lowest rates were noted among patients with thyroid cancer (7.3%), prostate cancer (4.0%), and melanoma of the skin (3.6%) (Fig. 3).
Figure 3.
Distribution of the top 25 incident cancer types is shown by insurance status.
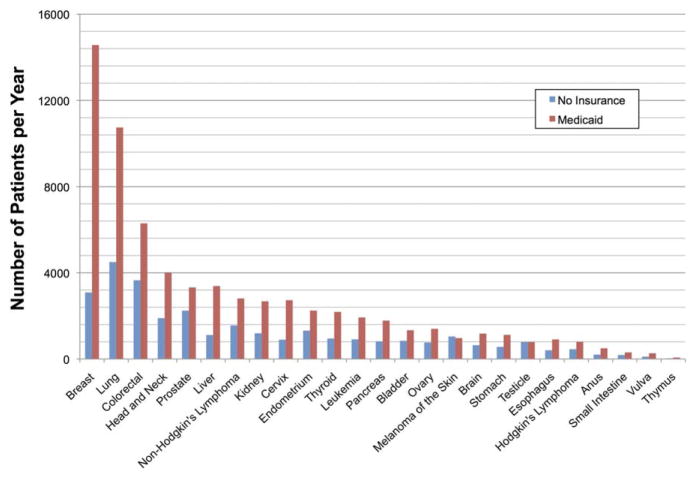
Among individuals with non-Medicaid insurance, the top 3 types of cancer were breast cancer (20.9%), prostate cancer (20.4%), and lung cancer (8.8%). Among those uninsured patients, lung cancer (14.9%), colorectal cancer (12.1%), and breast cancer (10.2%) were most common. Among individuals with Medicaid coverage, the most common cancers were breast cancer (21.3%), lung cancer (15.7%), and colorectal cancer (9.2%) (Fig. 4).
Figure 4.
Estimated annual incidence by cancer type is shown among individuals with Medicaid coverage or those without insurance.
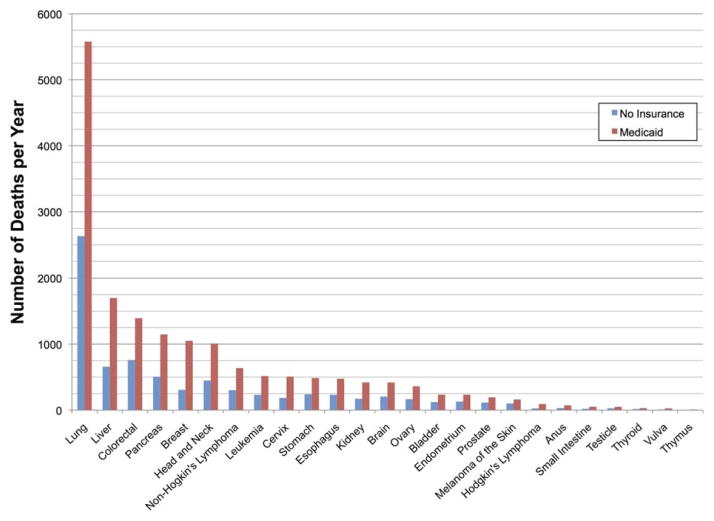
Among individuals with non-Medicaid insurance, the cancers with the highest burden of mortality were lung cancer (18,369 deaths per year), pancreatic cancer (5268 deaths per year), and colorectal cancer (4772 deaths per year). Among those who were uninsured, lung cancer (2631 deaths per year), colorectal cancer (760 deaths per year), and liver cancer (657 deaths per year) were the most common causes of cancer mortality. In addition, among those individuals with Medicaid coverage, the highest burden of mortality was observed with lung cancer (5579 deaths per year), liver cancer (1701 deaths per year), and colorectal cancer (1395 deaths per year). In each of the 3 insurance cohorts, lung cancer mortality exceeded the combined mortality of the next 4 most common causes of cancer death combined (Fig. 5).
Figure 5.
Estimated annual mortality burden by cancer type is shown among individuals with Medicaid coverage or those without insurance.
DISCUSSION
In the current study, we used the SEER data set to investigate the association between patient demographic factors and insurance status among nonelderly adults diagnosed with cancer. We found that younger age, male sex, non-white race, being unmarried, residence in counties with higher levels of poverty, and rural residence were associated with being uninsured versus having non-Medicaid insurance. The same demographic features were found to be associated with having Medicaid versus having non-Medicaid insurance with the exception that female sex was associated with Medicaid coverage. Moreover, we found wide variability in insurance coverage by tumor site, with rates of non-Medicaid insurance ranging from 62% to 93% and rates of Medicaid insurance ranging from 3% to 26%. The highest uninsured rates were noted among patients with testicular cancer, stomach cancer, and cervical cancer, whereas the lowest rates were observed in patients with thyroid cancer, prostate cancer, and breast cancer. Lung cancer was responsible for the overwhelming majority of cancer mortality in all 3 insurance groups.
To our knowledge, the current study is the first to examine variation in insurance status by patient demographic factors using the SEER data set. Although previous studies have explored differences in demographics among patients with cancer,12–17 these were either limited to select populations or cancer sites, or did not correlate their findings with insurance status. Select population-based studies have used the SEER or other data sets to examine insurance status among patients with cancer,4,5,18–25 but these reports focused on patient survival or receipt of guideline therapy rather than patient demographic disparities in insurance status. Nevertheless, the factors that we found to be predictive of a lack of insurance are similarly predictive of higher unemployment rates and/or socioeconomic disadvantage. Moreover, the increasing uninsured rate observed over the years examined (2007–2010) is likely the result of the recent economic downturn.
The association between tumor site and insurance status is complex, with at least 3 possible contributing factors. First, uninsured patients are less likely to use cancer screening tests,26 which can increase the prevalence of certain indolent diseases such as cancer of the prostate and certain types of breast cancer, while decreasing the early detection of potentially aggressive diseases such as cervical cancer, which can be discovered and eliminated in their precancerous stages. Second, the association between younger age and lack of insurance likely contributes to the variation in insurance status noted among certain age-associated cancers, such as testicular cancer (median age at diagnosis, 33 years) and prostate cancer (median age at diagnosis, 66 years).27 Finally, a lack of insurance has been associated with certain cancer risk factors, such as alcohol abuse and tobacco exposure,28,29 thereby increasing the prevalence of aerodigestive and genitourinary cancers.
It is of particular interest to note that the extension of Medicaid eligibility to women diagnosed with breast or cervical cancer was afforded in the Breast and Cervical Cancer Prevention and Treatment Act of 2000. Although every state has adopted this optional Medicaid expansion, there has been variation in coverage and implementation.30 Despite this targeted increase in access, patients with cervical cancer remain one of the groups with the highest uninsured rates. Additional efforts may help to expand access to care among patients with those cancer types and demographic groups with the highest rate of uninsurance.
With such wide discrepancies in insurance coverage, the PPACA will disproportionately benefit certain populations. Signed into law in March 2010, with full implementation expected by 2020, the PPACA aims to expand access to Medicaid and non-Medicaid health insurance. With Medicaid enrollment extending to 133% of the federal poverty level, and subsidies through newly created exchanges made available to uninsured lower-income Americans (133% to 400% of the federal poverty level), experts estimate an additional 32 million individuals will be covered by 2019.31,32 Such an expansion will impact those populations with relatively high rates of uninsurance the most, based on both demographics (ie, unmarried individuals, nonwhite individuals) and tumor site (ie, testicular, stomach, and cervical cancer). Nonetheless, although it is clear that insurance status affects stage of disease at the time of presentation, receipt of cancer-directed therapy, and mortality,4 further research will be needed to determine whether and to what degree cancer care is ultimately impacted by the upcoming changes to insurance coverage.
The current study has certain limitations that need to be addressed. For one, we used county-level income data as a surrogate for patient socioeconomic status because the SEER database does not report patient-level income. Moreover, insurance status is a new variable in the SEER database, the validity of which has not been established to the best of our knowledge. One concern is that some patients who enroll in Medicaid or other insurance after their diagnosis may not have been correctly captured in the SEER data set. Moreover, the SEER insurance variable does not subdivide those with private insurance (managed care, health maintenance organization, or preferred provider organization), Medicare, and coverage from the military or Veterans Affairs, and therefore potential differences between these types of insurance were unable to be examined. In addition, although the SEER database is largely representative of the US population, there exist certain demographical differences.11 Finally, 6.1% of the population in the current study had unknown insurance status and therefore were unable to be analyzed.
In summary, rates of insurance coverage vary greatly by patient demographic factors and by cancer type, suggesting that the expansion of coverage under the PPACA will likely disproportionately impact certain patient populations with cancer more greatly than others. The affect on quality of care and outcomes remains to be seen. Additional studies after further implementation of the PPACA will be warranted to examine these benefits.
Acknowledgments
FUNDING SUPPORT
No specific funding was disclosed.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
Dr. Walker is supported by a training fellowship from the Keck Center for Interdisciplinary Bioscience Training of the Gulf Coast Consortia (grant T15 LM007093) for work performed as part of the current study.
References
- 1.Heron M. Deaths: leading causes for 2010. Natl Vital Stat Rep. 2013;62:1–96. [PubMed] [Google Scholar]
- 2.Smith JK, Ng SC, Zhou Z, et al. Does increasing insurance improve outcomes for US cancer patients? J Surg Res. 2013;185:15–20. doi: 10.1016/j.jss.2013.05.058. [DOI] [PubMed] [Google Scholar]
- 3.Roetzheim RG, Pal N, Tennant C, et al. Effects of health insurance and race on early detection of cancer. J Natl Cancer Inst. 1999;91:1409–1415. doi: 10.1093/jnci/91.16.1409. [DOI] [PubMed] [Google Scholar]
- 4.Walker GV, Grant SR, Guadagnolo BA, et al. Disparities in stage at diagnosis, treatment, and survival in nonelderly adult cancer patients according to insurance status. J Clin Oncol. 2014;32:3118–3125. doi: 10.1200/JCO.2014.55.6258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Census Bureau. Income, Poverty, and Health Insurance Coverage in the United States: 2012. Washington, DC: US Census Bureau; 2013. [Google Scholar]
- 6.Crowley RA, Golden W. Health policy basics: Medicaid expansion. Ann Intern Med. 2014;160:423–425. doi: 10.7326/M13-2626. [DOI] [PubMed] [Google Scholar]
- 7.Zippin C, Lum D, Hankey BF. Completeness of hospital cancer case reporting from the SEER Program of the National Cancer Institute. Cancer. 1995;76:2343–2350. doi: 10.1002/1097-0142(19951201)76:11<2343::aid-cncr2820761124>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 8.National Cancer Institute; Surveillance, Epidemiology, and End Results (SEER) Program. [Accessed July 1, 2014];Number of Persons by Race and Hispanic Ethnicity for SEER Participants (2010 Census Data) seer.cancer.-gov/registries/data.html.
- 9.Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence-SEER 18 Regs Research Data, Nov. 2012 Sub (1973–2010) <Katrina/Rita Population Adjustment>-Linked To County Attributes-Total US, 1969–2010 Counties. Bethesda, MD: National Cancer Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Surveillance Systems Branch; 2013. [Google Scholar]
- 10.Surveillance, Epidemiology, and End Results (SEER) Program. [Accessed July 1, 2014];County Attributes. seer.cancer.gov/seerstat/variables/countyattribs/
- 11.Yu JB, Gross CP, Wilson LD, Smith BD. NCI SEER public-use data: applications and limitations in oncology research. Oncology (Williston Park) 2009;23:288–295. [PubMed] [Google Scholar]
- 12.Bristow RE, Powell MA, Al-Hammadi N, et al. Disparities in ovarian cancer care quality and survival according to race and socioeconomic status. J Natl Cancer Inst. 2013;105:823–832. doi: 10.1093/jnci/djt065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Philips BU, Jr, Belasco E, Markides KS, Gong G. Socioeconomic deprivation as a determinant of cancer mortality and the Hispanic paradox in Texas, USA. Int J Equity Health. 2013;12:26. doi: 10.1186/1475-9276-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Standop J, Kuhn Y, Glowka TR, et al. Association of socioeconomic status and stage of pancreatic cancer at time of surgery in a German setting. Hepatogastroenterology. 2012;59:2614–2617. doi: 10.5754/hge10334. [DOI] [PubMed] [Google Scholar]
- 15.Darmawikarta D, Pole JD, Gupta S, Nathan PC, Greenberg M. The association between socioeconomic status and survival among children with Hodgkin and non-Hodgkin lymphomas in a universal health care system. Pediatr Blood Cancer. 2013;60:1171–1177. doi: 10.1002/pbc.24386. [DOI] [PubMed] [Google Scholar]
- 16.White A, Richardson LC, Krontiras H, Pisu M. Socioeconomic disparities in breast cancer treatment among older women. J Womens Health (Larchmt) 2014;23:335–341. doi: 10.1089/jwh.2013.4460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aizer AA, Wilhite TJ, Chen MH, et al. Lack of reduction in racial disparities in cancer-specific mortality over a 20-year period. Cancer. 2014;120:1532–1539. doi: 10.1002/cncr.28617. [DOI] [PubMed] [Google Scholar]
- 18.Harlan LC, Greene AL, Clegg LX, et al. Insurance status and the use of guideline therapy in the treatment of selected cancers. J Clin Oncol. 2005;23:9079–9088. doi: 10.1200/JCO.2004.00.1297. [DOI] [PubMed] [Google Scholar]
- 19.Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58:9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 20.Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 2008;9:222–231. doi: 10.1016/S1470-2045(08)70032-9. [DOI] [PubMed] [Google Scholar]
- 21.Elchoufani SE, Efird JT, O’Neal WT, Davies SW, Landrine H, Biswas T. The relation of race and type of health insurance to long-term risk of mortality among lung cancer patients in rural Eastern North Carolina. N C Med J. 2013;74:464–469. [PubMed] [Google Scholar]
- 22.Sorlie PD, Johnson NJ, Backlund E, Bradham DD. Mortality in the uninsured compared with that in persons with public and private health insurance. Arch Intern Med. 1994;154:2409–2416. [PubMed] [Google Scholar]
- 23.Cheung MR. Lack of health insurance increases all cause and all cancer mortality in adults: an analysis of National Health and Nutrition Examination Survey (NHANES III) data. Asian Pac J Cancer Prev. 2013;14:2259–2263. doi: 10.7314/apjcp.2013.14.4.2259. [DOI] [PubMed] [Google Scholar]
- 24.Sabik LM, Bradley CJ. Differences in mortality for surgical cancer patients by insurance and hospital safety net status. Med Care Res Rev. 2013;70:84–97. doi: 10.1177/1077558712458158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robbins AS, Pavluck AL, Fedewa SA, Chen AY, Ward EM. Insurance status, comorbidity level, and survival among colorectal cancer patients age 18 to 64 years in the National Cancer Data Base from 2003 to 2005. J Clin Oncol. 2009;27:3627–3633. doi: 10.1200/JCO.2008.20.8025. [DOI] [PubMed] [Google Scholar]
- 26.Levy AR, Bruen BK, Ku L. Health care reform and women’s insurance coverage for breast and cervical cancer screening. Prev Chronic Dis. 2012;9:E159. doi: 10.5888/pcd9.120069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Cancer Institute, Surveillance, Epidemiology, and End Results Program. [Accessed July 1, 2014];Median Age of Cancer Patients at Diagnosis, 2005–2009. seer.cancer.gov/archive/csr/1975_2009_pops09/results_single/sect_01_table.11_2pgs.pdf.
- 28.Wu LT, Kouzis AC, Schlenger WE. Substance use, dependence, and service utilization among the US uninsured nonelderly population. Am J Public Health. 2003;93:2079–2085. doi: 10.2105/ajph.93.12.2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–2069. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 30.Lantz PM, Soliman S. An evaluation of a Medicaid expansion for cancer care: The Breast and Cervical Cancer Prevention and Treatment Act of 2000. Womens Health Issues. 2009;19:221–231. doi: 10.1016/j.whi.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 31.Hofer AN, Abraham JM, Moscovice I. Expansion of coverage under the Patient Protection and Affordable Care Act and primary care utilization. Milbank Q. 2011;89:69–89. doi: 10.1111/j.1468-0009.2011.00620.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schoen C, Doty MM, Robertson RH, Collins SR. Affordable Care Act reforms could reduce the number of underinsured US adults by 70 percent. Health Aff (Millwood) 2011;30:1762–1771. doi: 10.1377/hlthaff.2011.0335. [DOI] [PubMed] [Google Scholar]