Abstract
This study evaluated time to first drink in women being released from jail to determine predictors of early relapse among women with hazardous drinking and HIV risk behaviors. Between February 2004 and June 2007, 245 participants were recruited from the Rhode Island Department of Corrections. Following the baseline assessment, participants were randomized to a motivational intervention group or to a control condition. Follow-up assessments at 1, 3, and 6 months were completed for 210 participants. Alcohol use during follow-up occurred in 86.7% of participants; 42.4% initiated alcohol use on day 1. The rate of initiation was associated with norms favorable to using alcohol (p < .01) and having a partner with an alcohol problem (HR = 1.62, p < .01). The rate of drink initiation decreased significantly (HR = 0.82, p < .05) as length of incarceration increased. The intervention was not associated with decreased drinking. Interventions to maintain abstinence need to reach women within their first days postrelease.
Keywords: alcoholism, jail inmates, women, HIV risk behavior, alcohol intervention
Compared with other industrialized nations, the United States has the highest percentage of the population who are incarcerated. There are approximately 200,000 female inmates in prisons and jails in the United States (Harrison & Karberg, 2006) and the lifetime risk of a woman going to prison is 1.8% (Bonczar, 2003). A lifetime history of alcohol abuse has been reported in approximately one-third of women involved in the criminal justice system (Grella & Greenwell, 2007; Jordan, Schlenger, Fairbank, & Caddell, 1996; Teplin, Abram, & McClelland, 1996). This rate is approximately five times that identified in a national sample of community-dwelling women (Kessler, Chiu, Demler, Merikangas, & Walters, 2005). Estimates of women under the influence of alcohol at the time of arrest suggest even higher rates (el-Bassel, Ivanoff, Schilling, Gilbert, & Chen, 1995; Greenfeld, 1999).
Time in jail is an enforced period of abstinence from alcohol and drug use, as well as other HIV risk behaviors. For women, the first few days after release from prison or jail represent a time of great vulnerability to a return to substance abuse, abusive relationships, criminal activity, and high-risk behavior, particularly among women returning with little support to communities with few resources (Binswanger et al., 2007; Richie, Freudenberg, & Page, 2001). Studies reveal that the first 2 weeks after release are a high-risk time for mortality (Binswanger et al., 2007). Alcohol use is of concern in this population as there is considerable evidence that sexual HIV risk behaviors may be associated with alcohol use (Rees, Saitz, Horton, & Samet, 2001; Smith et al., 1997).
In this study we evaluated time to first drink in a population of incarcerated women being released from jail and we determine predictors of early relapse to alcohol use among women with hazardous drinking and HIV risk behaviors. We hypothesized that the first few days would be the highest risk time for alcohol use postrelease.
Method
Sample
Participants were recruited from the Women’s Facility of the Rhode Island Department of Corrections (RI DOC) between February 2004 and June 2007. During this time there were no major changes in laws or jail policies that would affect the results of this study. The RI DOC is a unified corrections system serving as a combined prison and jail, holding all pretrial and sentenced inmates in the state, and it functions primarily as a jail, with 69% of women being released within 4 days of arrival. Women were recruited as part of a randomized trial evaluating a two-session motivationally based intervention to decrease alcohol use and HIV risk behaviors among women reporting hazardous drinking. Approval for the study was obtained from the Miriam Hospital Institutional Review Board, the Office for Human Research Protection, and the Medical Research Advisory Group at the RI DOC. A certificate of confidentiality was also obtained from the federal government to further ensure participant privacy. The full details regarding the logistical planning for this trial have been published elsewhere (Hebert et al., 2008).
Participants were eligible for the clinical trial of interest if they spoke English and reported having risky sexual behavior (unprotected sex on at least 3 separate days in the 3 months prior to incarceration) and hazardous alcohol consumption (four or more drinks at a time on at least 3 separate days in the previous 3 months or a score of 8 or above on the AUDIT [Saunders, Aasland, Babor, de la Fuente, & Grant, 1993], which was framed to the past year). During the enrollment period, 1,616 women were approached for screening and only 12.4% (n = 201) refused to be screened. Of the remaining 1,415 women, 282 (19.9%) were eligible to participate, of which 245 (86.9%) enrolled. Time-to-event analysis is based on the 210 participants with risk exposure following release from the ACI. Some participants were reincarcerated and released several times during the study period. Only the first release was used in this analysis. Screening was done confidentially with verbal consent. Questionnaires and intervention sessions occurred in unmonitored rooms one-on-one with female research staff.
Schedule of the Intervention
Baseline interviews were conducted in the RI DOC on the first or second day of incarceration and lasted an average of 45 to 60 minutes. Following the baseline assessment, participants were randomized to an intervention group receiving the motivational intervention or to a control condition. Randomization and concealment were overseen by the study methodologist and research staff performing the assessments were blinded to the participant’s assigned condition. All women were scheduled for follow-up assessment at 1, 3, and 6 months following the baseline assessment, regardless of whether the participant was incarcerated. Predictor variables used in this analysis are from the baseline interviews. Time to first drink was assessed using follow-up data collected after participants’ initial return to the community.
The study design was such that interventionists provided the first session during incarceration and the second session in the community, one month after release when participants were reexposed to the availability of alcohol. Participants assigned to the control condition completed the assessment visits only. The intervention followed the five basic principles of motivational interviewing and details have been previously reported (Stein, Caviness, Anderson, Hebert, & Clarke, in press).
Variables
Timeline followback methodology (TLFB) was used to assess incarceration and alcohol use behaviors (Sobell & Sobell, 1992). Baseline behaviors were based on a 90-day TLFB. To summarize prebaseline behaviors we report the percentage of nonincarcerated days on which alcohol use was observed; we included the first night of any incarceration period in this calculation. Follow-up interviews were conducted at 1, 3, and 6 months. TLFB data were collected back to the last available data point (e.g., if a participant was not located for the 1-month assessment the TLFB data obtained at 3 months was extended to baseline).
Norms favorable to alcohol use were assessed using a three-item index. The questions were: “How many of the people you spend time with have an alcohol or drug problem?” “How many of the people you spend time with would support your sobriety or abstinence or efforts to reduce your alcohol use?” And “how many of the people you spend time with encourage your drinking?” Internal consistency reliability for the three-item index was .74. Participants were also asked if they live with a partner or spouse who has an alcohol problem (coded 1 if yes). Individual items taken from the ASI were used to assess the frequency of cocaine and heroin use in the 90 days prior to baseline. Number of nights incarcerated prior to release was calculated from the follow-up TLFB assessments. First night following release on the street or in a shelter was coded 1 if yes.
Statistical Analysis
Descriptive statistics are presented to summarize the background characteristics and alcohol use behaviors observed in this cohort. We used Cox regression to evaluate the effects of selected predictor variables on time (number of days) to first drink following release. We evaluated the adequacy of the proportional hazards assumption by testing for a nonzero slope in the regression of scaled Schoenfeld residuals on time; this test is implemented using estat phtest in Stata 10.1 (StataCorp, 2007) and was evaluated separately for all individual predictors as well as for the final model. We present bivariate models estimating the unadjusted effect of each predictor on time to first drink. The final multivariate model was selected in stages. We first estimated a model that included all predictors with significant (p < .05) bivariate effects on time to first drink. We next examined models in which the contribution of each excluded predictor was individually evaluated when added to the model that included all significant bivariate predictors. Continuous predictor variables were standardized to zero mean and unit variance prior to analysis; the associated coefficients give the expected factor change in the hazard of alcohol use for a one standard deviation increase in the predictor. Confidence interval estimates and tests of significance are based on robust variance estimators.
Results
A total of 245 participants were assessed at baseline; 186 (75.9%), 194 (79.2%), and 193 (78.8%) were located for follow-up assessment at 1, 3, and 6 months, respectively. Fourteen women were continuously incarcerated and had no alcohol exposure risk and 21 women were lost to follow-up, resulting in a final sample for this analysis of 210 (follow-up rate of 90.9%).
Participants averaged 34.6 (± 8.9) years of age, 71.4% were Caucasian, 20.5% were African American, and 8.1% were of other ethnic or racial origins. The mean AUDIT score at screening was 20.6 (± 10.0). Prior to baseline, participants reported using any alcohol on an average of 50.1% (± 32.2) and heavy (≥ 4 drinks) alcohol use on an average of 41.9% (± 33.3) of assessed TLFB days, with 90.4% meeting criteria for a lifetime diagnosis of alcohol dependence. Fifty-seven (27.1%) said they lived with a partner or spouse with an alcohol problem. About 68.1% and 25.2% reported using any cocaine or heroin, respectively, in the 90 days prior to baseline. Injection drug use in the past 90 days was reported by 21.4% of participants. About half (50.5%) reported at least one incarceration in the 90 days prior to baseline. Forty-two (20.0%) participants reported spending one or more nights on the street or in a shelter in the 90 days prior to baseline, and 22 (10.8%) spent their first night following release on the street or in a shelter.
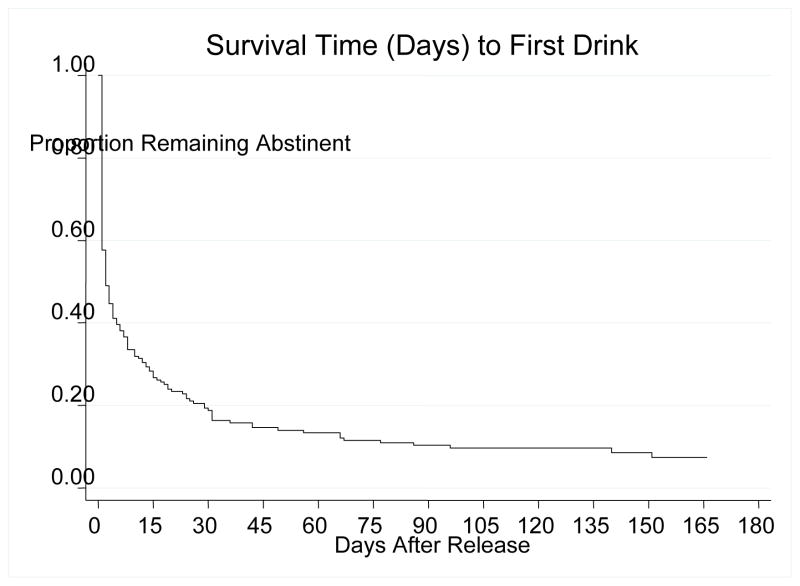
Figure 1 gives survival time to first drink following release. Persons were observed for a total of 3,884 days following release; 182 (86.7%) were observed to initiate alcohol use at some point during follow-up. Median survival time was 2 days. Eighty-nine (42.4%) participants initiated alcohol use on day 1 after release. A total of 119 (56.7%) had initiated alcohol use by the end of week 1, 133 (63.3%) by the end of week 2, and 158 (75.2%) by the end of week 4. Twenty-eight (13.3%) remained abstinent throughout follow-up.
Figure 1.
Survival Time to First Drink Following Release
Participants consumed 4 or more drinks on 81.8% of days that they drank after release. Time to first drink following incarceration was not associated significantly with demographic characteristics such as age, race, or educational attainment (Table 1). Nor was it associated significantly with the percentage of days on which participants used alcohol prior to baseline assessment. The expected hazard of drink initiation increased by a factor of 1.33 for each one standard deviation increase in the index assessing norms favorable to using alcohol (p < .01). The rate of drink initiation was also associated significantly with having a partner with an alcohol problem (HR = 1.62, p < .01). Additionally, the rate of drink initiation decreased significantly (HR = 0.82, p < .05) as the length of incarceration prior to release increased. Rate of alcohol initiation was not associated significantly with reported frequency of cocaine or heroin use, with spending the first night of release on the street or in a shelter, with the index of physical and sexual abuse, or with receipt of the intervention (Table 1).
Table 1.
Background Characteristics (n = 210)
| Mean (± SD) | Median | Range | |
|---|---|---|---|
| Age | 34.57 (8.88) | 35.5 | 18 – 56 |
| AUDIT | 20.58 (10.02) | 20.5 | 3 – 40 |
| % Days used alcohol | 50.10 (32.22) | 45.56 | 2.22 – 100.00 |
| % Days 4+ drinks | 41.93 (33.32) | 31.11 | 0.00 – 100.00 |
| % Days incarcerated (prebaseline) | 3.02 (8.30) | 1.11 | 0.00 – 64.44 |
| Frequency of cocaine use (0–90 days) | 36.29 (38.93) | 12.00 | 0 – 90 |
| Frequency of heroin use (0–90 days) | 9.74 (24.68) | 0.00 | 0 – 90 |
| % Nights on street or in shelter | 12.27 (28.68) | 0.00 | 0.00 – 100.00 |
|
n (%)
|
|||
| Race | |||
| White | 150 (71.4) | ||
| African American | 43 (20.5) | ||
| Other | 17 (8.1) | ||
| Partner has alcohol problem | 57 (27.1) | ||
| 1st Night postrelease street or shelter (yes) | 22 (10.5) | ||
| In the past 90 days: | |||
| Any cocaine use (yes) | 143 (68.1) | ||
| Any heroin use (yes) | 53 (25.2) | ||
| Any injection drug use (yes) | 45 (21.4) | ||
| Any incarceration (yes) | 106 (50.5) | ||
| Any nights street or shelter (yes) | 42 (20.0) | ||
Discussion
The majority of hazardously drinking women relapse to alcohol use within the first week of release from jail. In the Cox regression model, early relapse was associated living with a partner who has an alcohol problem, norms supporting alcohol use, and duration of incarceration. We found no effect of the single motivational interviewing session on time to first drink. Future interventions to maintain abstinence upon return to the community need to reach women within their first days postrelease.
Of interest is that the time to first drink increased with increasing nights spent in jail. This may in part be a reflection of increased substance abuse treatment services obtained by women during longer incarcerations (although we do not have data to confirm this speculation). In addition, longer incarceration may simply allow these mostly alcohol-dependent women to get past the symptoms of withdrawal and have a longer period to reflect on the consequences of alcohol use. Alternatively, it may be that jail offers the opportunity to “dry out” without any treatment. While we do not advocate longer incarcerations, these results emphasize the importance of providing substance abuse treatment during incarceration that focus on the time immediately following release.
Norms supporting alcohol use and having a partner with an alcohol problem were both associated with earlier time to first drink and these findings are consistent with results from other studies (Johnson, Nagoshi, Danko, Honbo, & Chau, 1990; Lemke, Brennan, Schutte, & Moos, 2007; Leonard & Homish, 2008; Wood, Nagoshi, & Dennis, 1992). Covington and Bloom report that women develop relationships that are different than those of men and that incarcerated women are particularly susceptible to being influenced by the behaviors of their partners (Covington, 1998; Covington & Bloom, 2003). An essential part of many substance abuse treatment programs is assessing social supports and environments that support sobriety. For women with longer incarcerations, discharge planning often includes changing one’s living environment to be away from peers and partners who encourage alcohol use. Norms supporting alcohol use can be changed with subsequent decreases in alcohol use (Hagman, Clifford, & Noel, 2007; Reilly & Wood, 2008). In settings with limited resources, interventions for incarcerated women with hazardous drinking may need to focus on women at highest risk for relapse including those with partners with alcohol problems and women with high levels of norms supporting alcohol use. Jails and prisons will need to have staff with expertise in health behavior change dedicated to improving the drinking outcomes of women to apply these findings.
One limitation of this study is that we included only women who drank hazardously and reported HIV risk behaviors. The generalizability of our findings to other populations of incarcerated women, or to men, may be limited. These data rely on self report, but the underestimation of alcohol use seems unlikely as the vast majority (86.7%) reported that they returned to alcohol use, including heavy use. Another limitation is that Rhode Island has a combined prison and jail system and the results of this study may not be applicable to other jail systems.
This study adds to the growing body of literature showing that the time immediately after release is a high-risk time. Additionally, our results are consistent with other studies finding that drinking is associated with partner-related alcohol problems. Women with hazardous drinking who are leaving jail should be encouraged to enter or continue alcohol treatment in the days immediately postrelease. Providing comprehensive substance abuse treatment services prior to release has been shown to decrease relapse, and services should be made available to incarcerated women as incarceration alone has not been shown to decrease substance abuse (Freudenberg, Wilets, Greene, & Richie, 1998; Pelissier, Camp, Gaes, Saylor, & Rhodes, 2003).
Table 2.
Cox Regression Models Giving the Effects of Selected Predictor Variables on Time to Alcohol Use Following Release (n = 210)
| Predictor | Unadjusted HRa (95% CIb) | Adjusted HRa (95% CIb) |
|---|---|---|
| Age | 0.98 (0.87,1.11) | |
| Race | ||
| White | 0.75 (0.53,1.07) | |
| African American | 0.72 (0.48,1.11) | |
| Other [reference] | [1.00] | |
| Education | 0.99 (0.86,1.14) | |
| % days used alcohol (baseline) | 1.09 (0.96,1.25) | |
| Norms supporting alcohol use | 1.33** (1.18,1.50) | 1.29** (1.13,1.46) |
| Partner has alcohol problem | 1.62** (1.25,2.11) | 1.48** (1.14,1.92) |
| Beck Depression Inventory | 1.08 (0.95,1.22) | |
| Cocaine use frequency | 1.03 (0.90,1.18) | |
| Heroin use frequency | 0.95 (0.83,1.09) | |
| # Nights in ACI prior to release | 0.82* (0.69,0.96) | 0.84* (0.73,0.99) |
| 1st night postrelease street or shelter | 1.28 (0.86,1.90) | |
| Index of physical and sexual abuse | 1.09 (0.96,1.24) | |
| Intervention | 0.93 (0.72,1.20) | |
p < .05,
p < .01
Hazard ratio
Confidence interval estimates and tests of significance were based on robust variance estimators.
Adjusted for variables with p < .05
Acknowledgments
Funding
This study was funded by the National Institute on Alcohol Abuse and Alcoholism, AA014495, Clinical Trial #NCT 00237003. Dr. Stein is a recipient of a NIDA Mid-Career Award, DA 000512.
Footnotes
Declaration of Conflicting Interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article. For information about JCHC’s disclosure policy, please see the Self-Study Exam.
References
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, et al. Release from prison–a high risk of death for former inmates. New England Journal of Medicine. 2007;356(2):157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonczar TP. Prevalence of imprisonment in the U.S. population, 1974–2001. Washington, DC: U.S. Department of Justice, Bureau of Justice Statistics; 2003. NCJ 197976. [Google Scholar]
- Covington S. The relational theory of women’s psychological development: Implications for the criminal justice system. Paper presented at the 50th Annual Meeting of the American Society of Criminology; Washington, DC. 1998. Nov, [Google Scholar]
- Covington SS, Bloom BE. Gendered justice: Women in the criminal justice system. In: Bloom BE, editor. Gendered justice: Addressing female offenders. Durham, NC: Carolina Academic Press; 2003. pp. 3–24. [Google Scholar]
- el-Bassel N, Ivanoff A, Schilling RF, Gilbert L, Chen DR. Correlates of problem drinking among drug-using incarcerated women. Addictive Behaviors. 1995;20:359–369. doi: 10.1016/0306-4603(94)00075-a. [DOI] [PubMed] [Google Scholar]
- Freudenberg N, Wilets I, Greene MB, Richie BE. Linking women in jail to community services: Factors associated with rearrest and retention of drug-using women following release from jail. Journal of the American Medical Wome’s Association. 1998;53(2):89–93. [PubMed] [Google Scholar]
- Greenfeld LA. Women offenders. Washington, DC: U.S. Department of Justice, Bureau of Justice Statistics; 1999. NCJ 175688. [Google Scholar]
- Grella CE, Greenwell L. Treatment needs and completion of community-based aftercare among substance-abusing women offenders. Women’s Health Issues. 2007;17(4):244–255. doi: 10.1016/j.whi.2006.11.005. [DOI] [PubMed] [Google Scholar]
- Hagman BT, Clifford PR, Noel NE. Social norms theory-based interventions: Testing the feasibility of a purported mechanism of action. Journal of American College Health. 2007;56:293–298. doi: 10.3200/JACH.56.3.293-298. [DOI] [PubMed] [Google Scholar]
- Harrison PM, Karberg JC. Prison and jail inmates at midyear 2005. Washington, DC: U.S. Department of Justice, Bureau of Justice Statistics; 2006. NCJ 213133. [Google Scholar]
- Hebert MR, Clarke JG, Caviness CM, Ray MK, Friedmann PD, Stein MD. Feasibility of gaining access to women in jail for health interventions. Women and Health. 2008;47(3):79–93. doi: 10.1080/03630240802134159. [DOI] [PubMed] [Google Scholar]
- Johnson RC, Nagoshi CT, Danko GP, Honbo KA, Chau LL. Familial transmission of alcohol use norms and expectancies and reported alcohol use. Alcoholism, Clinical and Experimental Research. 1990;14(2):216–220. doi: 10.1111/j.1530-0277.1990.tb00475.x. [DOI] [PubMed] [Google Scholar]
- Jordan BK, Schlenger WE, Fairbank JA, Caddell JM. Prevalence of psychiatric disorders among incarcerated women. II. Convicted felons entering prison. Archives of General Psychiatry. 1996;53:513–519. doi: 10.1001/archpsyc.1996.01830060057008. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemke S, Brennan PL, Schutte KK, Moos RH. Upward pressures on drinking: Exposure and reactivity in adulthood. Journal of Studies on Alcohol and Drugs. 2007;68:437–445. doi: 10.15288/jsad.2007.68.437. [DOI] [PubMed] [Google Scholar]
- Leonard KE, Homish GG. Predictors of heavy drinking and drinking problems over the first 4 years of marriage. Psychology of Addictive Behaviors. 2008;22(1):25–35. doi: 10.1037/0893-164X.22.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelissier BM, Camp SD, Gaes GG, Saylor WG, Rhodes W. Gender differences in outcomes from prison-based residential treatment. Journal of Substance Abuse Treatment. 2003;24(2):149–160. doi: 10.1016/s0740-5472(02)00353-7. [DOI] [PubMed] [Google Scholar]
- Rees V, Saitz R, Horton NJ, Samet J. Association of alcohol consumption with HIV sex- and drug-risk behaviors among drug users. Journal of Substance Abuse Treatment. 2001;21(3):129–134. doi: 10.1016/s0740-5472(01)00190-8. [DOI] [PubMed] [Google Scholar]
- Reilly DW, Wood MD. A randomized test of a small-group interactive social norms intervention. Journal of American College Health. 2008;57(1):53–60. doi: 10.3200/JACH.57.1.53-60. [DOI] [PubMed] [Google Scholar]
- Richie BE, Freudenberg N, Page J. Reintegrating women leaving jail into urban communities: A description of a model program. Journal of Urban Health. 2001;78:290–303. doi: 10.1093/jurban/78.2.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Smith DK, Warren DL, Vlahov D, Schuman P, Stein MD, Greenberg BL, et al. Design and baseline participant characteristics of the Human Immunodeficiency Virus Epidemiology Research (HER) Study: A prospective cohort study of human immunodeficiency virus infection in US women. American Journal of Epidemiology. 1997;146:459–469. doi: 10.1093/oxfordjournals.aje.a009299. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell M. Timeline followback: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Stein M, Caviness C, Anderson B, Hebert M, Clarke J. A brief alcohol intervention for hazardously drinking women. Addiction. doi: 10.1111/j.1360-0443.2009.02813.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM. Prevalence of psychiatric disorders among incarcerated women. I. Pretrial jail detainees. Archives of General Psychiatry. 1996;53:505–512. doi: 10.1001/archpsyc.1996.01830060047007. [DOI] [PubMed] [Google Scholar]
- Wood MD, Nagoshi CT, Dennis DA. Alcohol norms and expectations as predictors of alcohol use and problems in a college student sample. American Journal of Drug and Alcohol Abuse. 1992;18:461–476. doi: 10.3109/00952999209051042. [DOI] [PubMed] [Google Scholar]