Abstract
All-inside anterior cruciate ligament reconstruction has recently gained popularity, in part because of its bone-sparing socket preparation and reported lower pain levels after surgery. However, because this technique uses suture loops and cortical suspension buttons for graft fixation, it has mostly been limited to looped graft constructs (e.g., hamstring autograft, peroneus longus allograft). Quadriceps tendon autograft offers several advantages in anterior cruciate ligament reconstruction but, until recently, has not been compatible with suture-loop and cortical suspensory fixation. We describe a technique that allows a relatively short (<75 mm) quadriceps tendon autograft (without bone block) to be used with established all-inside anatomic techniques.
The use of quadriceps tendon autograft in anterior cruciate ligament (ACL) reconstruction was first described by Marshall et al.1 in 1979, but it has not gained widespread use like other autograft options. Many surgeons traditionally have limited its use to select cases such as revisions. Recently, however, there has been increased interest in the quadriceps graft, possibly because of the recent body of evidence in support of autograft use for ACL reconstruction in younger patients and contact athletes.
The quadriceps tendon autograft offers several advantages. It contains a denser collagen matrix compared with a patellar tendon graft of the same thickness, with less interstitial tissue and 20% more collagen per unit volume.2 The typical graft diameter is 10 mm; hamstring autografts narrower than 8.0 mm have recently been implicated in higher failure rates.3 The quadriceps tendon autograft is also usually still available in the revision setting, and recent evidence has suggested improved graft survivorship when autografts are used for these patients.4 In addition, the quadriceps autograft avoids some of the morbidity of other graft options, with less reported anterior knee pain and numbness compared with patellar tendon–bone graft, as well as none of the residual cramping that can occur with hamstring tendon harvest.5 The indications for using quadriceps tendon autograft are the same as those for other autografts (younger active patients) but also include use in revision cases, even when a patellar tendon–bone autograft has previously been harvested from the same knee (Table 1). Contraindications include patients with chronic quadriceps tendinopathy or prior rupture.
Table 1.
Indications and Contraindications for Quadriceps Tendon Autograft Use
| Indications |
| Primary ACL reconstruction in any patient, but especially high–athletic demand patients or patients aged <25 yr |
| Revision ACL reconstruction in any highly active or younger patient (prior patellar tendon–bone graft harvest is not a contraindication) |
| Contraindications |
| Prior quadriceps tendon rupture |
| Chronic quadriceps tendinopathy |
ACL, anterior cruciate ligament.
Case series of ACL reconstruction with quadriceps tendon have shown laxity and revision rates that are equivalent to or better than those with patellar tendon–bone autografts.6 Complications such as extensor mechanism rupture have not been reported, but if a bone block is harvested, there is a small risk of patellar fracture and increased pain after surgery.7 Therefore an all–soft tissue quadriceps graft is desirable, but the maximum soft-tissue graft length of 80 to 90 mm may be at risk of being too short for some ACL reconstruction techniques.
For these reasons, an all–soft tissue quadriceps tendon autograft is ideally suited for the all-inside ACL technique, in which a shorter graft length (typically 65 to 70 mm) is not only desirable but mandatory to avoid “bottoming out” of the graft in the sockets before full tension is reached. The advantages of anatomic all-inside ACL reconstruction have been reported elsewhere8 and include bone preservation, less postoperative pain, and independent anatomic socket drilling.
Because of the advantages of both the quadriceps autograft and the all-inside technique, we sought to merge the two. We adapted the GraftLink (Arthrex, Naples, FL) graft preparation method to obtain an all–soft tissue quadriceps tendon autograft and describe our technique in this report. We also detail a few pearls for graft passage and list the general steps for a standard quadriceps tendon harvest and all-inside technique for ACL reconstruction.
Surgical Technique
We describe an open graft harvest technique in this report, but a minimally invasive harvest technique has also recently been described.9 Pearls and pitfalls are listed in Table 2.
Table 2.
Pearls and Pitfalls for All-Inside Anterior Cruciate Ligament Reconstruction With Quadriceps Tendon Autograft
| Pearls and Pitfalls | |
|---|---|
| Graft harvest | Ensure that dissection goes deep enough into the second layer of the quadriceps tendon to avoid harvesting a graft that is too thin. |
| Include fibers dissected sharply off the proximal one-third of the patella to gain length and minimize the need for a more proximal harvest. | |
| Graft preparation | On the femoral side, ensure that the graft is tapered appropriately to slide easily through a graft measurer. |
| On the tibial side, start the FiberLoop whipstitch proximal enough on the graft and loop it around the ABS TightRope 1 time to ensure high pullout strength. | |
| On the tibial side, after tying of the FiberLoop limbs, leave 1 or 2 tails uncut (using color stitches or marked sutures for easy identification) to ensure easy graft passage later. | |
| Graft passage | View button passage from the anteromedial portal to ensure that the button is flipped outside the femoral tunnel but deep to the IT band. |
| When passing tibial sutures, ensure that the ABS TightRope is passed with the finger-trap portion going through the knee first. The extra passing suture can be tied or cinched around the ABS TightRope to assist with this. | |
| To sink the tibial side of the graft into the tibial socket, pull the FiberLoop suture first; then tension the ABS TightRope. |
IT, iliotibial.
Graft Harvest
A 7-cm midline incision is made just proximal to the superior pole of the patella (Video 1). Medial and lateral flaps are developed, and the quadriceps tendon is exposed. Two parallel lines are drawn 10 mm apart, marking the middle third of the tendon. The tendon is incised along the lines, going to a depth of about 7 to 8 mm, using the height of the blade to judge the depth of the cut. The tendon is sharply elevated off the patella and the blunt end grasped with a clamp. The tendon is then sharply dissected proximally, staying deep to the natural divide between the rectus femoris and vastus intermedius layers. If the joint is penetrated, this can be sutured closed to prevent leakage of arthroscopy fluid. The tendon is truncated once a 70-mm graft is obtained. The tendon defect can be closed if desired but may be left open as well.
Graft Preparation
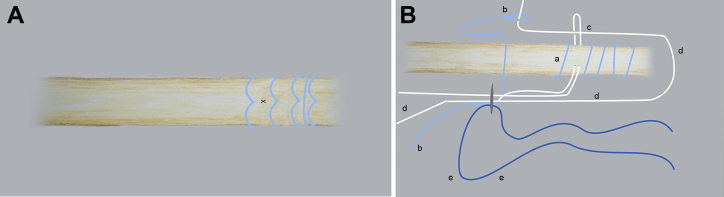
The graft is prepared starting with the (originally) patellar end, which we generally use for the femoral side. In step 1, a No. 2 FiberLoop (Arthrex) is whipstitched through the last 20 mm of graft (Fig 1A). At about 8 mm from the end of the graft, the ends of the FiberLoop are wrapped around the graft, tied, and cut, and the knot is buried in the tendon.
Fig 1.
(A) Distal end of graft after whipstitching with FiberLoop (in blue). The BTB TightRope will be placed at the X. (B) Assembling BTB TightRope through distal end of graft: FiberLoop sutures (a); free end of TightRope limb passed through suture trap and button by blue passing suture (b); TightRope loop passed through graft with straight needle (c; needle removed, not shown); TightRope tensioning limbs (d); and passing suture (e).
In step 2, a BTB TightRope (Arthrex) is placed between the 2 most proximal FiberLoop passes, and the TightRope is assembled according to the manufacturer's instructions (Fig 1B). It is vital to verify that the TightRope is sliding and cinching appropriately at the completion of this step.
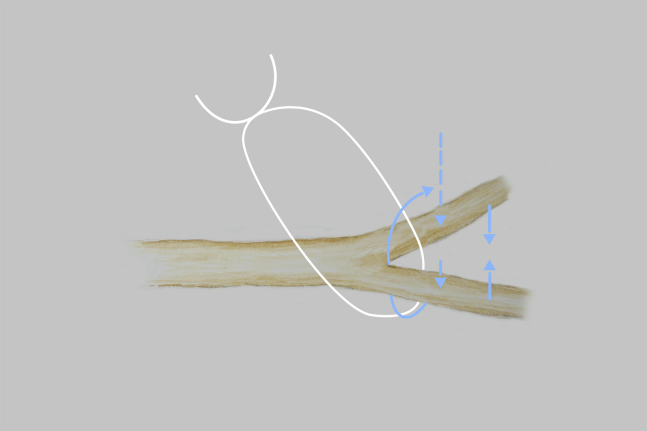
In step 3, the (originally) proximal end of the graft is divided along the natural raphe between the rectus and intermedius layers (Fig 2). An ABS TightRope (Arthrex) is placed between the limbs of the graft.
Fig 2.
The ABS TightRope (in white) is placed between the superficial and deep layers of the (originally) proximal end of the graft. The path of the FiberLoop (in blue) for the whipstitch is shown.
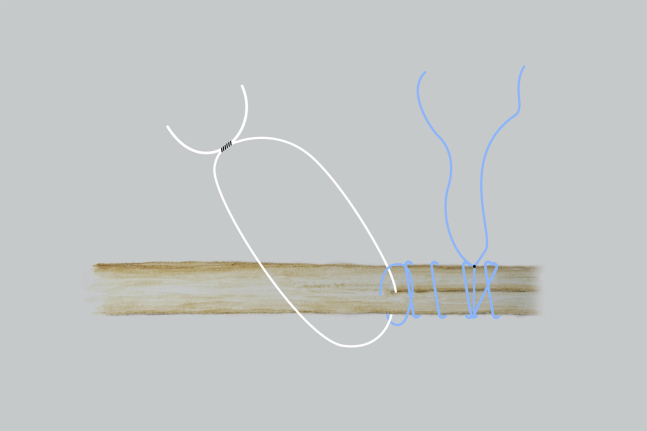
In step 4, a No. 2 FiberLoop is used to whipstitch the tails back together, beginning about 2 cm from the end of the graft. Before proceeding away from the ABS TightRope, 1 complete loop of the FiberLoop is passed around the TightRope, cinching and locking the TightRope in place (Fig 3). The rest of the whipstitch is then completed in the same fashion as on the femoral side. The FiberLoop limbs are tied to themselves, the knot is buried, and one or both limbs are saved for later graft passage.
Fig 3.
Final construct of tibial side of graft with ABS TightRope (in white) and FiberLoop (in blue).
Arthroscopy
In step 5, after graft preparation, the surgeon proceeds to perform standard diagnostic arthroscopy and notch preparation. The tunnel locations are marked according to the surgeon's preferences.
In step 6, the femoral socket is drilled in an antegrade manner and reamed in a retrograde manner with a FlipCutter (Arthrex) of the appropriate size. A FiberStick (Arthrex) is passed through the socket and docked out of the lateral portal.
In step 7, the tibial socket is prepared in the same fashion, and a TigerStick (Arthrex) is passed through the socket. Each socket should be approximately 20 to 25 mm in length.
In step 8, the FiberStick and TigerStick are both retrieved simultaneously and docked out of the anteromedial portal, with the surgeon ensuring that there is no soft-tissue bridge between the 2 sutures. It is critical to ensure that the sum of the socket depths and the intra-articular distance is at least 5 mm longer than the graft. This avoids the possibility of bottoming out of the graft in the sockets before full tension is reached.
In step 9, excess bone from reaming is irrigated and suctioned away before proceeding. In step 10, the graft is marked with the drilled socket depths to serve as arthroscopic indicators when the graft is fully seated.
In step 11, the sutures on the femoral side of the graft are passed using the FiberStick (Fig 4). The cortical button is flipped while the surgeon is viewing arthroscopically from the anteromedial portal. The view is switched back to the anterolateral portal, and the graft is advanced a few millimeters into the femoral socket.
Fig 4.
Right knee (medial is on right and superior is at top of image, with patella shown as dashed line centrally) before passage of BTB TightRope sutures. The sutures are passed using the FiberStick (in blue). Both the FiberStick and TigerStick have been docked out of the anteromedial portal before any sutures are passed.
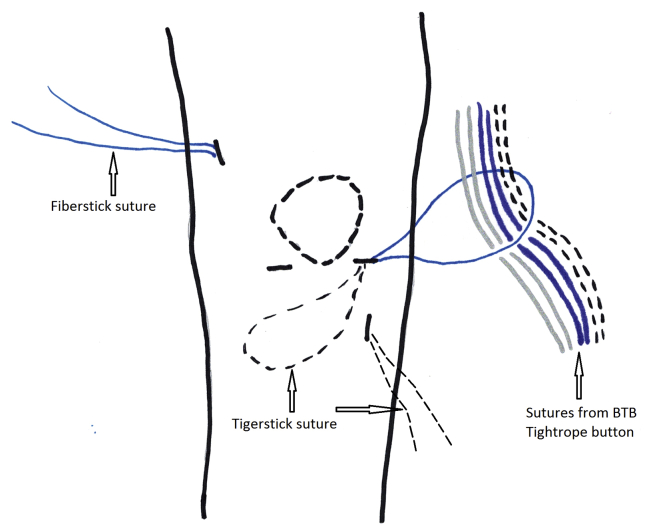
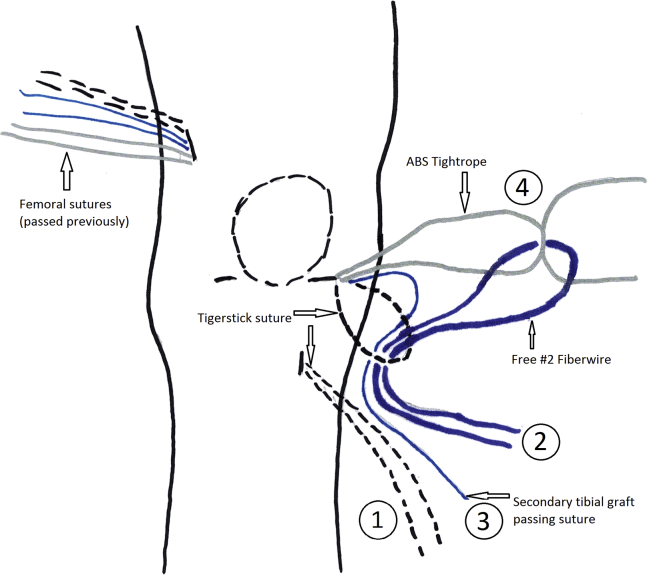
In step 12, a free No. 2 FiberWire (Arthrex) is looped through the ABS TightRope. The TigerStick is used to pass the free ends of this free FiberWire and the tibial-sided graft-passing sutures through the tibia (Fig 5). The surgeon then uses the free FiberWire to pass the ABS TightRope through the tibia, ensuring that the suture-trap part of the ABS goes through the knee first.
Fig 5.
Right knee (medial is on right and superior is at top of image, with patella shown as dashed line centrally) before passing free No. 2 FiberWire, secondary tibial graft-passing suture, and ABS TightRope. The order for suture pulling is marked. The TigerStick (dashed lines) is pulled first, docking the free No. 2 FiberWire (in dark blue) and the secondary tibial graft-passing suture (in light blue) out of the inferior tibial incision. The free No. 2 FiberWire is pulled second, retrieving the ABS TightRope out of the inferior tibial incision. The secondary graft-passing suture is pulled third, docking the tibial side of the graft into the tibial socket. Finally, the ABS TightRope is tensioned, after the external ABS Button has been attached.
In step 13, the surgeon tensions the graft-passing suture first, viewing arthroscopically to ensure that the graft enters the tibial socket “end first.” If it does not, it can be backed out gently with a probe and the passing suture tensioned again. Once the end of the graft has entered the socket, the graft may be completely seated by pulling on the ABS TightRope loop, with the surgeon taking care not to pull on the tensioning tails of the ABS because this will prematurely shorten the closed loop.
Graft Tensioning
In step 14, the ABS Button (Arthrex) is attached to the ABS TightRope. The surgeon tensions the graft with the knee in full extension, viewing arthroscopically to ensure that full seating of both ends of the graft to the previously made marks is achieved. The knee can be cycled and the graft tensioned again if desired. The knee is examined. Intraoperative fluoroscopy can be used if there is any doubt regarding the position of the buttons on bone. The passing sutures are cut and removed, and the TightRope sutures are tied to themselves with a knot pusher.
Discussion
The quadriceps tendon autograft offers several advantages for ACL reconstruction, as described earlier and summarized in Table 3. It is well suited to the all-inside technique because of its relatively short length if harvested without a bone block. In this report we describe a graft preparation technique to allow this graft to be used with suspensory fixation devices and the all-inside technique.
Table 3.
Potential Advantages, Disadvantages, and Complications of Quadriceps Tendon Autograft Use
| Advantages |
| Denser collagen matrix than patellar tendon autograft |
| Larger uniform graft diameter compared with hamstring or patellar tendon autograft |
| Often still available, even in revision setting |
| Harvest causes less morbidity (numbness, anterior knee pain, pain with kneeling) than patellar tendon autograft harvest |
| Autograft use potentially minimizes risk of rerupture in younger active patients compared with allograft use |
| Disadvantages |
| Technically demanding, more time-consuming technique |
| Longer scar compared with hamstring harvest if open technique is used |
| Complications |
| Quadriceps tendon rupture (rare) |
| Synovitis or cyclops formation around graft, limiting full extension |
| Over-tensioning graft with knee in flexion, limiting full extension |
| Quadriceps inhibition or delayed recruitment postoperatively |
The primary weakness of this report is the lack of published literature regarding the use of quadriceps tendon autograft in ACL reconstruction. This body of literature is slowly growing however.10 Biomechanical testing has been performed on our fixation technique, but the fixation needs to be more rigorously tested and the findings published. Future reports are also needed on complications, quadriceps strength recovery after graft harvest, and most importantly, long-term patient outcomes.
Surgeons looking for a robust graft that avoids some of the comorbidity of other autografts should consider using the quadriceps tendon. The described technique is technically challenging, but we believe the advantages of bone-sparing sockets, minimal hardware, and a relatively large graft size justify the challenges.
Footnotes
The authors report the following potential conflict of interest or source of funding: T.S.C. receives support from Smith & Nephew and Arthrex. B.B.G. receives support from Smith & Nephew and Arthrex.
Supplementary Data
First, an open harvest of a quadriceps tendon autograft is shown in a right knee (superior is on the right of the screen). The graft is then prepared on the back table. Finally, arthroscopy of the knee is performed, with most of the video footage viewing from the standard anterolateral viewing portal. The tunnels are drilled, and the graft is passed and secured with suspensory fixation on both the femoral and tibial sides.
References
- 1.Marshall J.L., Warren R.F., Wickiewicz T.L., Reider B. The anterior cruciate ligament: A technique of repair and reconstruction. Clin Orthop Relat Res. 1979;(143):97–106. [PubMed] [Google Scholar]
- 2.Harris N.L., Smith D.A., Lamoreaux L., Purnell M. Central quadriceps tendon for anterior cruciate ligament reconstruction. Part I: Morphometric and biomechanical evaluation. Am J Sports Med. 1997;25:23–28. doi: 10.1177/036354659702500105. [DOI] [PubMed] [Google Scholar]
- 3.Mariscalco M.W., Flanigan D.C., Mitchell J. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: A Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Arthroscopy. 2013;29:1948–1953. doi: 10.1016/j.arthro.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MARS Group Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2014;42:2301–2310. doi: 10.1177/0363546514549005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeAngelis J.P., Fulkerson J.P. Quadriceps tendon—A reliable alternative for reconstruction of the anterior cruciate ligament. Clin Sports Med. 2007;26:587–596. doi: 10.1016/j.csm.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Geib T.M., Shelton W.R., Phelps R.A., Clark L. Anterior cruciate ligament reconstruction using quadriceps tendon autograft: Intermediate-term outcome. Arthroscopy. 2009;25:1408–1414. doi: 10.1016/j.arthro.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Han H.S., Seong S.C., Lee S., Lee M.C. Anterior cruciate ligament reconstruction: Quadriceps versus patellar autograft. Clin Orthop Relat Res. 2008;466:198–204. doi: 10.1007/s11999-007-0015-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lubowitz J.H., Schwartzberg R., Smith P. Randomized controlled trial comparing all-inside anterior cruciate ligament reconstruction technique with anterior cruciate ligament reconstruction with a full tibial tunnel. Arthroscopy. 2013;29:1195–1200. doi: 10.1016/j.arthro.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 9.Fink C., Herbort M., Abermann E., Hoser C. Minimally invasive harvest of a quadriceps tendon graft with or without a bone block. Arthrosc Tech. 2014;3:e509–e513. doi: 10.1016/j.eats.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Slone H.S., Romine S.E., Premkumar A., Xerogeanes J.W. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: A comprehensive review of current literature and systematic review of clinical results. Arthroscopy. 2015;31:541–554. doi: 10.1016/j.arthro.2014.11.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
First, an open harvest of a quadriceps tendon autograft is shown in a right knee (superior is on the right of the screen). The graft is then prepared on the back table. Finally, arthroscopy of the knee is performed, with most of the video footage viewing from the standard anterolateral viewing portal. The tunnels are drilled, and the graft is passed and secured with suspensory fixation on both the femoral and tibial sides.