Abstract
Background
This study examined the incidence and clinical correlates of suicidal ideation (SI) in youth with tic disorders (TD). The independent contribution of tics, anxiety, depressive and externalizing symptoms on SI severity in youth with TD was assessed.
Method
Participants were 75 treatment-seeking youth with a TD (N = 75) aged 6–18. Participants completed diagnostic assessments, clinician-ratings, self- and parent-report measures of emotional functioning and the presence and/or severity of suicidal ideation.
Results
Based on youth-report, 61% of youth endorsed at least some symptoms of SI, and 8% endorsed symptoms that exceeded the clinically significant cut-off. Parents reported SI in 11% of cases, with generally poor agreement between parent- and youth-report. Suicidal ideation correlated with higher anxiety, depressive and externalizing symptoms, affective lability, and with poorer distress tolerance and overall functioning. Anxiety, depressive and externalizing symptoms showed an independent relationship with SI. Tic severity was not associated with SI. Rather, higher tic severity was associated with an increase in anxiety symptoms, which in turn, was associated with greater SI severity.
Limitations
Cross-sectional data limits causal conclusions. Diagnosis was based on unstructured assessments by expert clinicians, including consensus diagnosis, rather than structured clinical interviews.
Conclusions
Around 8–11% of youth with TD experienced SI. Tic severity did not have any direct influence on SI, however the presence of comorbid anxiety and depressive symptoms significantly increases this risk. Results suggest that it is psychiatric comorbidity, rather than tics themselves, that predispose youth with tic disorders to increased risk of suicidality.
Keywords: Tourette’s syndrome, Suicidal ideation, Children, Adolescents, Anxiety, Depression
Chronic Tic Disorders and Tourette’s syndrome (collectively referred to as TD herein) affect around 0.4–1.6% of youth (Knight et al., 2012; Scahill et al., 2014) and are characterized by sudden repetitive motor movements and/or vocalizations for more than a one year duration. Tic symptoms typically fluctuate over time, and subside in early adulthood in many cases (American Psychiatric Association, 2013; Bloch et al., 2006; Leckman et al., 1998). Despite this clinical course, when active, symptoms can be acutely impairing and distressing for both the young person and their family (Conelea et al., 2011; Storch et al., 2007a). Given the often involuntary and uncontrollable nature of their symptoms, many patients experience high levels of frustration and hopelessness surrounding their symptoms. Despite the common co-occurring of anxiety and mood disorders among youth with TD (Freeman et al., 2000; Specht et al., 2011), few studies have examined the phenomenology of suicidal ideation (SI) in this population. Given that suicide is one of the leading causes of death amongst youth (Bridge et al., 2006; Hawton et al.), it is relevant to extend this body of literature to better understand the level of risk present amongst youth with TD, and the clinical features that characterize higher-risk patients.
There is an increasing recognition that TDs are associated with a range of negative outcomes, many of which also represent risk factors for suicidal thoughts and behaviors. For example elevated levels of peer victimization, social deficits and psychiatric comorbidity including depressive symptoms, mood disorders, disruptive behavior disorders, and attention/hyperactivity problems have been documented in youth with TD (Kraft et al., 2012; McGuire et al., 2013; Robertson, 2006; Storch et al., 2007b; Sukhodolsky et al., 2003). In particular, depression, and (less consistently) anxiety, have been associated with increased risk of suicidal ideation and attempts in children and adolescents (Gould et al., 1998; O’Neil-Rodriguez and Kendall, 2014b; Reinherz et al., 1995). Despite these parallels, there remains a paucity of research examining the experience of SI in youth with TD.
Of the few studies that have examined SI in patients with TD, there has been some variability in incidence, likely due to differing age ranges, sampling methodology and measurement. For example, studies often utilize dichotomously coded measures of SI either derived from single-item responses to depressive symptom measures, clinical interview questions about depression, or clinician notes/ratings of SI as a construct that is present/absent. These formats may differ from a continuous measure of SI as a construct that varies in presence, frequency, and severity. Methodology also becomes more complex when considering informant issues, such as whether parents or youth provide the report. An archival review study examined clinical notes of patients with Tourette’s disorder attending a specialist tic disorder clinic, and documented SI in .06% of cases with .05% having made a suicide attempt (Gharatya et al., 2014). This study found that patients with TD who endorsed SI experienced higher levels of tic severity, and had a greater prevalence of comorbid anxiety disorders, comorbid depressive disorders, and comorbid OCD in comparison to individuals with TD who did not endorse SI (Gharatya et al., 2014). Rates of SI may be even higher amongst severe cases, with an archival review study in a specialist clinic setting finding that around 5% of TD cases were classified as ‘malignant’ cases that were characterized by severe tics, rage episodes, and symptoms of SI or self-injurious behaviors (Cheung et al., 2007). Another study compared severe cases of ‘malignant’ TD, where symptoms had resulted in more than 2 emergency room visits or more than one hospitalizations, and documenting SI in 35.3% of these severe cases, compared to 7.6% in ‘nonmalignant’ cases (Cheung et al., 2007).
Few studies have focused on SI exclusively on pediatric TD samples, with most studies using a wide age-range (Cheung et al., 2007; Davila et al., 2010; Gharatya et al., 2014). In the only study of SI in children and adolescents with TD to date, around 10% of children had experienced SI over the past year, significantly higher than rates endorsed by community controls (Storch et al., 2015a). Suicidal ideation was associated with higher tic severity, impairment, depressive symptoms, anxiety symptoms, hyperactivity/impulsivity, and oppositional behaviors (Storch et al., 2015a). Importantly, anxiety and depressive symptoms (collectively) fully mediated the relationship between tic severity and SI, theoretically suggesting that it is the presence of these symptoms that increases youth risk rather than their TD per se. This study combined single-item ratings from multiple informants (parent, child, and clinician) on symptoms measures (e.g., depression) to identify SI. While there are some strengths to this method, specific continuous measure of SI presence and severity have been developed for youth (Reynolds, 1988) that may allow for a more nuanced examination about not only the clinical features associated with the presence/absence of SI, but the severity of these symptoms as well. Overall, there appears to be a general consensus in the literature that there is a relationship between tic severity, psychiatric comorbidity and SI (Davila et al., 2010). In particular, anxiety and depressive symptoms may increase the risk of SI; however the differential impact of these symptoms has not been fully elucidated. There is evidence to suggest an independent relationship between anxiety symptoms and SI (Carter et al., 2008; Gould et al., 1998; Hawgood and De Leo, 2008; Hill et al., 2011; O’Neil-Rodriguez and Kendall, 2014b; O’Neil et al., 2012; Sareen et al., 2005), depressive symptoms and SI (Carlson and Cantwell, 1982; Gould et al., 1998; O’Neil-Rodriguez and Kendall, 2014b; O’Neil et al., 2012), and externalizing symptoms and SI (Kumar and Steer, 1995; Lewinsohn et al., 1993; Sourander et al., 2009), however it is unclear whether these have a differential impact on SI in pediatric TD populations.
Given the lack of studies assessing the relationship between TD and SI in youth, and the limitations in current assessment methods of SI, this study is novel in examining the presence and severity of SI in a pediatric TD sample, using a specific measure of SI in children and adolescents with CTD. This study had three aims. Firstly, this study aimed to examine the incidence of suicidal ideation in treatment-seeking youth with TD, and to examine the agreement between parent and child reports. We expected that, similar to Storch et al. (2015a), around 10% of youth with TD would experience SI as endorsed by either parent or child report. Given existing findings suggesting limitations to parental insight into these symptoms (e.g., Achenbach, 2011; Breton et al., 2002; Klaus et al., 2009; Walker et al., 1990), we anticipated higher rates of SI to be endorsed by youth than their parents. Secondly, this study aimed to assess demographic and clinical correlates of SI in youth with TD. We hypothesized that SI would be positively associated with tic severity, anxiety symptoms, depressive symptoms, and affective lability, and negatively associated with distress tolerance and global functioning. Third, we aimed to extend the model proposed by Storch et al. (2015a) to examine whether tics impacted SI by increasing anxiety, depressive and/or externalizing symptoms. Our hypothesis was that that tics would have no direct impact on SI, but would indirectly influence SI severity by increasing anxiety, depressive and externalizing symptoms. To enhance previous study designs, we included a specific and empirically validated measure of SI, as well as a separate measures of anxiety and depressive symptoms. Finally, we examined whether the above relationships differed in pre-pubertal and post-pubertal youth, given increased risk of suicide in older youth (Shaffer and Fisher, 1981; Tishler et al., 2007).
Method
Participants
Participants were 75 treatment-seeking youth aged 6–18 (M = 10.68, SD = 2.82) who were diagnosed with a tic disorder and their parent or primary caregiver. Participants were recruited from two specialty programs for OCD and Tic Disorders in Florida, United States. To be included, youth were required to meet DSM-IV criteria for a tic disorder with current tic symptoms present. Participants were excluded if they experienced active psychosis, mania, active suicidality, intellectual disability, or a psychiatric condition that would impede parent or youth report for the purposes of this study. See Storch et al. (2015b) and McGuire et al. (2015b) for a full discussion of methods. Demographic characteristics and diagnostic information for the sample are summarized in Table 1.
Table 1.
Participant demographic and diagnostic information.
| n | % | |
|---|---|---|
| Male | 45 | 60.0 |
| Ethnicity | ||
| White | 63 | 84.0 |
| Hispanic/Latin American | 8 | 10.7 |
| Asian | 4 | 5.3 |
| Household Income | ||
| Under $20,000 | 2 | 2.7 |
| $20,001 – $59,999 | 12 | 16.0 |
| $60,000 – $99,999 | 25 | 33.3 |
| Over $100,000 | 30 | 40.0 |
| Not Available | 6 | 8.0 |
| Tic Disorder | ||
| Tourette’s Disorder | 63 | 84.0 |
| Transient Tic Disorder | 6 | 8.0 |
| Chronic Motor Tics | 4 | 5.3 |
| Chronic Vocal Tics | 2 | 2.7 |
| Comorbid Diagnoses | ||
| Any Anxiety Disorder | 56 | 74.7 |
| Depressive Disorder | 9 | 12.0 |
| Disruptive Behavior Disorder | 13 | 17.3 |
| ADHD | 29 | 38.7 |
Measures
Yale Global Tic Severity Scale (YGTSS; Leckman et al., 1989)
The YGTSS is a semi-structured clinical interview administered to parents and children jointly to assess the presence of a variety of motor and phonic tics, as well as their severity and interference. The YGTSS has demonstrated good internal consistency, strong convergent validity with other measures of tic severity and good divergent validity from measures of internalizing and externalizing problems, and depression and anxiety severity in children and adolescents with TD (Leckman et al., 1989; Storch et al., 2007c; Storch et al., 2005; Walkup et al., 1992). The YGTSS Total Tic Severity score was used in this study and represents the combination of Motor and Vocal Tic Severity. Scores range from 0–50 with higher scores indicating greater tic severity. This index demonstrated acceptable internal consistency in our sample (α = .79).
Suicidal Ideation Questionnaire – Junior (SIQ-Jr; Reynolds, 1988)
The SIQ-Jr is a 15-item abbreviated child-report form of the 30-item SIQ. This measure provides an assessment of the presence and severity of suicidal thoughts and plans in youth. Youth rate the extent to which they have experienced symptoms over the past month on a 7-point scale from 0 = I never had this thought to 6 = Almost every day. The SIQ-Jr has demonstrated very high internal consistency, test-retest reliability and concurrent validity, with youth who had attempted suicide reporting higher scores than youth who had not attempted suicide. A raw score cut-off of 31 (89th percentile of normative sample) is indicative of significantly elevated levels of SI (Reynolds, 1988). Internal consistency was high in this sample (α = .96).
Parent-reported Suicidal Ideation
Consistent with previous studies (e.g., McBride et al., 2015; O’Neil-Rodriguez and Kendall, 2014b; Storch et al., 2015a), parent-reported SI was determined based on responses to items on the well-validated Child Behavior Checklist (CBCL; Achenbach and Rescorla, 2001). Parents who positively endorsed item 18 (“deliberately harms self or attempts suicide”) or item 91 (“talks about killing self”) as “somewhat true” or “very true” were coded as having endorsed SI symptoms in their child.
Child Behavior Checklist (CBCL; Achenbach and Rescorla, 2001)
The CBCL is a widely-used measure of emotional functioning in children and adolescents. The Externalizing Problems domain score was used in this study, which assesses aggressive, hyperactive, noncompliant and under-controlled behaviors in youth.
Children’s Depression Rating Scale-Revised (CDRS-R; Poznanski and Mokros, 1996)
The CDRS-R is a 17-item clinician-rated interview that assesses the severity of depressive symptoms in children and adolescents. This measure has shown good internal consistency, inter-rater reliability, convergent validity with measures of depressive severity and global functioning, ability to discriminate between depressed an non-depressed children, and sensitivity to change over treatment (Jain et al., 2007; Mayes et al., 2010; Poznanski et al., 1984; Poznanski and Mokros, 2005). Internal consistency was good in this sample (α = .82), with higher scores indicating greater depressive symptom severity.
Screen for Child Anxiety Related Emotional Disorders, Parent and Child Report (SCARED; Birmaher et al., 1997)
The SCARED-P/C is a 41-item parent and child-report measure respectively, that assesses the presence and frequency of a range of anxiety symptoms, including generalized anxiety, separation anxiety, panic, school phobias and social anxiety symptoms. Higher scores indicate greater anxiety severity. The SCARED-P/C has demonstrated good internal consistency, test-retest reliability, parent-child agreement and discriminant validity between anxiety and other disorders (Birmaher et al., 1999; Birmaher et al., 1997). The parent and child-report versions showed excellent internal consistency in the current study (α = .94 and α = .93 respectively).
Rage Outbursts and Anger Rating Scale (ROARS; Budman et al., 2008)
The ROARS is a 3-item clinician-rated measure of the frequency, intensity, and duration of rage episodes over the past week. Items are rated on a 4-point scale (0 = none/absent to 3 = >1 rage outburst per day/severe). This measure has shown good internal consistency and convergent validity in children with OCD and anxiety, and good divergent validity from other measures of disorder severity (Johnco et al., 2015; Storch et al., 2012a).
Distress Tolerance Scale (DTS; Simons and Gaher, 2005)
The DTS is a 15-item child-report measure of their ability to tolerate distressing emotions. This measure has demonstrated good internal consistency, and one higher order factor, as well as good convergent validity with measures of affective distress and regulation (Rezapour et al., 2013; Simons and Gaher, 2005). Higher scores indicate greater distress tolerance. Internal consistency was excellent in the current sample (α = .94).
Children’s Affective Lability Scale (CALS; Gerson et al., 1996)
The CALS is a 20-item parent-report measure that assesses children’s ability to regulate their emotions. This measure has shown good internal-consistency, test-retest reliability over a two-week-period, and inter-rater reliability (Gerson et al., 1996). In addition, clinical samples of children have shown higher scores (indicative of greater lability) in comparison to normative samples (Gerson et al., 1996). Internal consistency was excellent in the current sample (α = .92).
Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983)
The CGAS is a clinician-rated measure of functioning and impairment in children that demonstrated generally adequate inter-rater reliability, concurrent and discriminant validity (Bird et al., 1987; Lundh et al., 2010; Shaffer et al., 1983). Scores range from 0–100 with higher scores indicating better functioning.
Procedure
This study was approved by the relevant institutional review board. Written consent was obtained from parents and assent from youth. Youth and parents were interviewed by an experienced child and adolescent psychologist or board certified child and adolescent psychiatrist. Psychiatric diagnoses were determined based on best estimate procedures (Leckman et al., 1982) that included consensus diagnosis between two Ph.D.-level investigators (EAS and ABL). Parents and youth completed self-report measures listed above. No compensation was provided to subjects.
Data Analysis
There was less than 10% of data missing on any individual scale. We used a single imputation method that utilizes maximum likelihood estimation including the expectation maximization algorithm, a two-step iterative process to obtain missing values (Peugh and Enders, 2004). This method accurately reproduces the internal consistency of the scale and is appropriate when there is less than 15% missing data (Enders, 2003, 2010).
Descriptive statistics were used to examine sample demographics and clinical characteristics. Given the skewed distribution of the SIQ-JR results, Mann-Whitney U tests were used for comparing gender differences and Spearman’s Rho was used to examine correlations between the SIQ-JR and continuous variables. We examined the mediation model proposed by Storch et al. (2015a) to examine whether tic symptoms were associated with SI by increasing anxiety and depressive symptoms. We conducted a path analysis using IBM AMOS version 23 using 5000 bootstrap samples. Model fit was evaluated initially using the global fit χ2 statistic, where a non-significant value indicates that the model is likely to fit the data. However, given the limitations of this fit index (Steiger, 2007), we also evaluated model fit using relative fit and non-centrality-based indices. We evaluated model fit using criteria of Tucker Lewis Index (TLI) and Comparative Fit Index (CFI) ≥ .95, and Root Mean Squared Error of Approximation (RMSEA) ≤ .05 (Hu and Bentler, 1999). The relationship between SI and anxiety, depression, externalizing symptoms and tic symptom severity for youth under and above the age of 12 were examined using a hierarchical regression.
Results
Phenomenology
On the SIQ-JR, 61.33% (n = 46) of youth endorsed at least some symptoms of SI. Based on a cut-off score of 31 on the SIQ-JR, 8% (n = 6) of youth with CTD endorsed clinically significant levels of SI. Parents reported SI in 10.7% (n = 8) of cases. Although parent and child-report was consistent in 86.7% of cases (n = 65), there were 10 cases where parent- and child report varied. In 8% of cases (n = 6) parents reported symptoms of SI while their child did not. In 5.3% of cases (n = 4), children reported significant levels of SI while their parents did not identify SI symptoms in the child. Overall, there was poor inter-rater reliability between parent and child reports (k = .21).
Demographic and Clinical Correlates
When examining the distribution of SIQ-JR scores, there were 3 participants who showed scores greater than 3 standard deviations above the sample mean, including standardized z-score values greater than 3.29, indicating that these scores were outliers. These extreme values in relation to other participants were confirmed via visual inspection of the histogram. Given that results of this paper are intended to describe the average child with CTD, scores from these three participants are unusual and are not likely to reflect the result for the ‘average’ participant. Given the potential for these extreme values to unduly influence results, these participants were excluded from bivariate and multivariate analyses. Despite removal of these outliers, the distribution was still skewed, so nonparametric statistics were used to examine group differences and clinical correlates.
There was no gender difference in SI severity on the SIQ-JR (U = 589.50, p = .751), and no relationship between SIQ-JR and child age (rs = .06, p = .601). Greater tic severity (YGTSS) was associated with greater child-rated anxiety severity (rs = .30, p = .011) and affective lability (rs = .35, p = .002), although the relationship with parent-rated anxiety failed to reach significance (rs = .23, p = .055). There was no relationship between tic severity and depressive symptoms, distress tolerance, externalizing symptoms or global functioning (all p’s > .05).
Clinical correlates of SI severity on the SIQ-Jr as well as group differences between youth whose parents reported that they experienced SI and those who did not are summarized in Table 2. Child-rated SI severity on the SIQ-JR was not related to tic severity on the YGTSS, although it showed a moderate to strong relationship with child- and parent-rated anxiety severity on the SCARED and a strong relationship with depressive symptoms on the CDRS. Greater SI symptoms were associated with poorer distress tolerance on the DTS and greater affective lability on the CALS. Higher SIQ-JR scores were also associated with increased externalizing behaviors, and poorer global functioning on the CGAS, but not with rage. Using parent-reports of SI, youth who experienced SI had higher depressive symptoms, externalizing behaviors and lower global functioning on the CGAS, although there were no significant differences between children whose parents reported that the child experienced SI symptoms and those who did not in terms of their tic severity, anxiety, rage, distress tolerance or affective lability.
Table 2.
Clinical differences and correlates of suicidal ideation in youth with tic disorders
| Child-Rated | Parent-rated | ||||
|---|---|---|---|---|---|
|
| |||||
| SIQ-JR | No-SI (n = 64) | SI (n = 8) | |||
|
| |||||
| rs | Range | Mrank | Mrank | U | |
| YGTSS | −.01 | 7–43 | 37.30 | 30.13 | 205.00 |
| SCARED-C | .49*** | 0–66 | 36.31 | 38.00 | 244.00 |
| SCARED-P | .28* | 0–51 | 36.06 | 40.00 | 288.00 |
| CGAS | −.29* | 35–81 | 38.25 | 22.50 | 144.00* |
| DTS | −.39** | 22–75 | 38.05 | 23.88 | 155.00 |
| CALS | .35** | 0–75 | 35.28 | 46.25 | 178.00 |
| CDRS | .49*** | 17–57 | 34.45 | 52.88 | 125.00* |
| CBCL Externalizing | .24* | 0–36 | 34.55 | 52.06 | 131.50* |
| ROARS | .11 | 0–9 | 36.12 | 39.56 | 231.50 |
CALS = Children’s Affective Lability Scale; CDRS = Children’s Depression Rating Scale-Revised; CGAS = Children’s Global Assessment Scale; DTS = Distress Tolerance Scale; SCARED = Screen for Child Anxiety Related Emotional Disorders - Parent and Child Report; SI = Suicidal Ideation; YGTSS = Yale Global Tic Severity Scale.
Multivariate Analysis
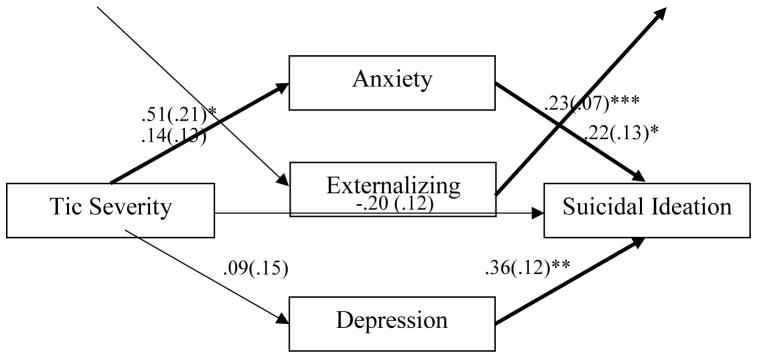
We initially examined the path model proposed by Storch et al. (2015a), to examine whether tic severity influenced SI via increasing anxiety, depressive and/or externalizing symptoms in youth with CTD, although were able to separate anxiety and depressive symptom severity in the current model (see Figure 1).
Figure 1.
Path model examining whether tic severity increased suicidal ideation in youth with chronic tic disorders via increasing anxiety and depressive symptoms. Values are unstandardized regression coefficients and numbers in parentheses are standard errors. Bolded lines represent significant pathways. *p < .05, **p < .01, ***p < .001.
This model showed a good fit for the data (χ2 = .15, p = .695; CFI = 1.00, TLI = 1.18, RMSEA < .001). Results suggest that greater anxiety, depressive and externalizing symptom severity was associated with increased SI. There was no direct relationship between tic severity and SI. Greater severity of tics was associated with an increase in anxiety, which in turn, was associated with an increase in SI severity (indirect pathway B = .11, SE(B) = .06, p = .017).
Differences in Suicidal Ideation between Children and Adolescents
We examined separately the bivariate and multivariate relationships between symptom measures and SI in children under the age of 12 (n = 52) and adolescents aged 12 or above (n = 20). Clinical correlates of SI and group differences based on parent-rated SI are reported separately for child and adolescent samples in Table 3. For children under the age of 12, SIQ-JR scores were associated with greater child and parent-rated anxiety, affective lability, depressive symptoms and externalizing symptoms, as well as lower global function on the CGAS, and poorer distress tolerance. There was no relationship between SIQ-JR scores and tic severity or rage. When examining parent-rated SI, youth who experienced SI showed higher levels of depressive and externalizing symptoms, and lower global functioning. For adolescents over the age of 12, there was a significant positive relationship between SIQ-JR scores and depressive symptoms, and an inverse relationship with distress tolerance. These results were the same when examining parent-rated SI.
Table 3.
Differences in clinical correlates of suicidal ideation in children and adolescents.
| Child (<12 years) | Adolescents (≥ 12 years) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Child-Rated | Parent-rated | Child-Rated | Parent-rated | |||||
|
| ||||||||
| SIQ-JR | No-SI (n=48) | SI (n=4) | SIQ-JR | No-SI (n=16) | SI (n=4) | |||
|
| ||||||||
| rs | Mrank | Mrank | U | rs | Mrank | Mrank | U | |
|
| ||||||||
| YGTSS | .08 | 37.30 | 30.13 | 205.00 | −.30 | 11.13 | 8.00 | 22.00 |
| SCARED-C | .50*** | 36.31 | 38.00 | 244.00 | .43 | 10.44 | 10.75 | 31.00 |
| SCARED-P | .42** | 36.06 | 40.00 | 228.00 | −.01 | 10.25 | 11.50 | 28.00 |
| CGAS | −.41** | 38.25 | 22.50 | 144.00* | .03 | 11.81 | 5.25 | 11.00 |
| DTS | −.34* | 38.08 | 23.88 | 155.00 | −.65** | 12.19 | 3.75 | 5.00** |
| CALS | .49*** | 35.28 | 46.25 | 178.00 | .05 | 9.91 | 12.88 | 22.50 |
| CDRS | .47*** | 34.45 | 52.88 | 125.00* | .58** | 8.94 | 16.75 | 7.00* |
| CBCL | .36** | 34.55 | 52.06 | 131.50* | −.07 | 9.69 | 13.75 | 19.00 |
| Externalizing | ||||||||
| ROARS | .15 | 36.12 | 39.56 | 231.50 | .02 | 10.25 | 11.50 | 28.00 |
We conducted a hierarchical regression to predict SI entering tic severity on the first step and anxiety, depressive and externalizing symptoms on the second step. For children under the age of 12, the first step containing only tic severity was not significant, F(1,50) = .06, p = .803. The second step was significant, and predicted 42.5% of the variance in SIQ-JR scores, F(4,47) = 8.67, p < .001. Greater anxiety (β = .49, p < .001) and externalizing symptoms (β = .39, p = .002), and lower tic severity (β = −.25, p = .045) predicted increased SI in youth under the age of 12, but not depressive symptoms (β = .07, p = .588).
For youth aged 12 or above, tic severity alone did not predict SI, F(1,18) = .42, p = .523. The second step including anxiety, depressive and externalizing symptoms was significant and explained 76.9% of the variance in SIQ-JR scores, F(4,15) = 12.45, p < .001. Greater depressive symptoms (β = .94, p < .001) and lower externalizing symptoms (β = −.38, p = .015) predicted SI severity on the SIQ-JR, but tic severity and anxiety symptoms did not (β =-.17, p = .195 and β = −.07, p = .600 respectively).
Discussion
The rate of parent-reported SI (11%) was similar to rates of overall SI reported by parents on in the previous child-focused study of SI in TD (9.7%; Storch et al., 2015a). Overall, 61% of youth with TD endorsed at least some level of SI. Using a clinical cut-off on the SIQ-JR, rates of clinically significant SI reported by youth (8%) were similar to that of parents, however our findings suggested poor agreement between parent and child reports of SI. This finding may reflect the differing methodology of identifying SI using specific continuous measures of SI rather than utilizing single-item responses to symptoms measures that results in a present/absent coding rather than a variable assessment of severity of these symptoms. However, these results suggesting discrepant findings between parents and youth are consistent with previous studies (Achenbach, 2011; Breton et al., 2002; Klaus et al., 2009; Walker et al., 1990) and are also likely to reflect differences in insight, knowledge and reporting between youth and parents. Youth may fail to share their SI symptoms with their parent for a number of reasons, limiting parental awareness. Conversely, youth may have variable accuracy and willingness to report these symptoms when presenting to treatment. In most cases, a combined methodological approach is ideal for assessing risk in this population. Interestingly, the rates of SI in youth were considerably lower than those reported in studies of children with anxiety disorders (27–58%; Carter et al., 2008; McBride et al., 2015; O’Neil-Rodriguez and Kendall, 2014b; Walkup et al., 1992) and depressive disorders 63% (30–63%; Carlson and Cantwell, 1982; March et al., 2007). It may be that the externalizing and often unusual nature of tics results in earlier treatment-seeking for youth with Tics that may limit or curtail higher levels of distress in comparison to internalizing problems such as anxiety and depression, where treatment-seeking is often delayed until youth are significantly impaired and distressed.
Higher SI severity was noted amongst youth with greater anxiety, depressive and externalizing symptoms, poorer distress tolerance and greater affective lability. Although externalizing symptoms showed a relationship with SI, rage did not. This is likely a result of low variability in the rage measure (more than half the sample scored 0). Contrary to earlier studies (e.g., Storch et al., 2015a), we did not find any direct relationship between tic severity and SI using either parent or child-report. However the direct pathway in (Storch et al., 2015a) was weak (B = .05) and anxiety and depressive symptoms mediated this relationship. Methodological difference with other studies may account for other inconsistencies, for example, using dichotomously coded measures of SI derived from parent, child, clinicians (or a combination) rather than a continuous measure specifically constructed to assess SI, as used in the current study. Using this methodology allows for increased variability in scores, and may enhance the potential to elucidate the role of emotional symptoms and tics on SI in a more nuanced way. Findings suggest that there was no direct relationship between tic severity and SI. Rather, greater tic severity was associated with an increase in anxiety symptoms, which, in turn, was associated with an increase in SI severity. Taken together, these findings encourage the careful assessment of youth with TD who present with co-occurring anxiety, depressive and/or externalizing symptoms. Indeed, these results contribute to the existent literature (e.g., Storch et al., 2015a) to suggest that interventions that directly target these comorbid symptoms may help to mitigate risk.
Suicide is less common in younger children, with increased risk often noted post-puberty (Shaffer and Fisher, 1981; Tishler et al., 2007). As such, we conducted exploratory analyses in children above and below the age of 12 to assess whether predictors of SI differed. We found that increased anxiety and externalizing symptoms, but not depressive symptoms, predicted higher SI in younger children. A relationship between anxiety and increased risk of SI has been noted in younger children without TD, although the independent contribution above and beyond the effect of depressive symptoms has been inconsistent (Carter et al., 2008; O’Neil-Rodriguez and Kendall, 2014a; O’Neil et al., 2012). This may be an artifact of depressive symptoms also being less common in younger children. We also found that lower level of tic symptoms predicted SI in children with TD, consistent with our overall findings that it is co-occurring mental health symptoms that appear to be influencing SI in youth with TD, rather than the tics themselves.
In youth aged 12 and over, our findings are consistent with a large body of existing literature suggesting that increased levels of depressive symptoms predicted greater SI severity (Brent et al., 1999; Cash and Bridge, 2009; Shaffer et al., 1996). While externalizing symptoms are often cited as a risk factor for SI (Sourander et al., 2009), we found that lower levels of externalizing behaviors were associated with SI after accounting for the influence of anxiety, depressive and tic symptoms in our adolescent sample. Although unexpected, this result has been found previously (Prinstein et al., 2008). Overall, there appears to be some differences between children and adolescents in regards to the impact of comorbidity on SI in youth with TD. Namely, anxiety (and to some extent externalizing) symptoms appears to play a greater role in SI severity amongst children with TD, while depressive symptoms appear to be more important amongst adolescents. On the whole, results from this study suggest that it is the impact of comorbid psychopathology symptoms that impacts on SI in youth with TD, rather than the tic symptoms per se.
There are several study limitations. First, although we used a continuous SI-specific measure to examine child-rated SI severity, we utilized single-item parent-responses from symptoms measures to identify SI cases. Although consistent with a number of other studies (e.g., O’Neil-Rodriguez and Kendall, 2014b; Storch et al., 2015a), this methodology results in a dichotomous outcome that fails to account for severity and frequency of symptoms. Responding on these items may also be influenced by responding on the symptom measure from which they were drawn (e.g., depressive symptoms). Second, this study was cross-sectional in nature, and structural models should be considered quasi-meditational in nature. Third, although clinical diagnoses were made by experienced child and adolescent psychologists and/or board certified child and adolescent psychiatrists, and incorporated consensus diagnostic procedures, the lack of a structured clinical diagnostic assessment is a limitation. Fourth, data was based on current symptoms of tics and SI given potential for bias in retrospective recall of worst-ever symptoms. However, it is possible that worst-ever tic symptoms may show a greater relationship with SI given the potential increase in helpless/hopelessness. It is also possible that SI is related to duration of TD illness, however we were unable to examine this relationship in our sample. Finally, it is possible that discrepancies between raters may have influenced some results given parent and child ratings of anxiety, and clinician-rated measures of tic severity and depressive symptoms.
This study was one of the first to examine the clinical phenomenology of SI in children and adolescents with TD. Results suggest than a minority (8–11%) of youth experience symptoms of SI, and this was most likely related to their experience of anxiety and depressive symptoms, rather than their tics per se. These clinical features may highlight specific vulnerability factors for youth with TD who are more likely to experience SI, and support the importance of assessing emotional functioning in this population. While behavior therapy is efficacious in reducing tic severity (McGuire et al., 2014), tic severity was not associated with SI in this sample of youth with TD. Thus, there is a need for more comprehensive interventions to reduce the distress, impairment and associated problems experienced by youth with TD (e.g., social problems, social deficits, peer victimization, self-concept) that may be contributing to the development of anxiety and/or depressive symptoms. Although recognized as important in practice parameter guidelines (Murphy et al., 2013), there have been only two studies that have sought to address these co-occurring concerns (McGuire et al., 2015a; Storch et al., 2012b). Beyond interventions to address these problems, future longitudinal data are needed to conclusively assesses the relative impact of tics, anxiety and depressive symptoms on SI in youth in order to fully elucidate the level of risk posed by these emotional symptoms, as well as evaluate the impact of evidence-based interventions on tic severity and emotional symptoms.
Highlights.
61% of youth with tic disorders endorsed some symptoms of suicidal ideation
8% of youth endorsed clinically significant suicidal ideation
Parents reported suicidal ideation in 11% of youth with tic disorder
Anxiety, depressive and externalizing symptoms (but not tics) were associated with higher suicidal ideation
Tics were associated with increased anxiety, which in turn increased suicidal ideation.
Acknowledgments
The contributions of Elysse Arnold, Erika Crawford, Amanda Collier, Brittney Dane, and Morgan King at University of South Florida with data collection are gratefully acknowledged.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Commentary: Definitely More Than Measurement Error: But How Should We Understand and Deal With Informant Discrepancies? J Clin Child Adolesc. 2011;40:80–86. doi: 10.1080/15374416.2011.533416. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms & profiles: Child Behavior Checklist for Ages 6–18, Teacher’s Report Form, & Youth Self-Report. University of Vermont; Burlington: 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association; Washington, DC: 2013. [Google Scholar]
- Bird HR, Canino G, Rubio-Stipec M, Ribera JC. Further measures of the psychometric properties of the children's global assessment scale. Arch Gen Psychiatry. 1987;44:821–824. doi: 10.1001/archpsyc.1987.01800210069011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Bloch MH, Peterson BS, Scahill L, et al. ADulthood outcome of tic and obsessive-compulsive symptom severity in children with tourette syndrome. Arch Pediat Adol Medicine. 2006;160:65–69. doi: 10.1001/archpedi.160.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age- and sex-related risk factors for adolescent suicide. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1497–1505. doi: 10.1097/00004583-199912000-00010. [DOI] [PubMed] [Google Scholar]
- Breton JJ, Tousignant M, Bergeron L, Berthiaume C. Informant-Specific Correlates of Suicidal Behavior in a Community Survey of 12- to 14-Year-Olds. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:723–730. doi: 10.1097/00004583-200206000-00012. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. Journal of child psychology and psychiatry, and allied disciplines. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Budman CL, Coffey BJ, Shechter R, Schrock M, Wieland N, Spirgel A, Simon E. Aripiprazole in children and adolescents with Tourette disorder with and without explosive outbursts. Journal of Child and Adolescent Psychopharmacology. 2008;18:509–515. doi: 10.1089/cap.2007.061. [DOI] [PubMed] [Google Scholar]
- Carlson GA, Cantwell DP. Suicidal Behavior and Depression in Children and Adolescents. J Amer Acad Child Ps. 1982;21:361–368. doi: 10.1016/s0002-7138(09)60939-0. [DOI] [PubMed] [Google Scholar]
- Carter R, Silverman WK, Allen A, Ham L. Measures matter: The relative contribution of anxiety and depression to suicidal ideation in clinically referred anxious youth using brief versus full length questionnaires. Depression and anxiety. 2008;25:E27–E35. doi: 10.1002/da.20468. [DOI] [PubMed] [Google Scholar]
- Cash SJ, Bridge JA. Epidemiology of Youth Suicide and Suicidal Behavior. Current opinion in pediatrics. 2009;21:613–619. doi: 10.1097/MOP.0b013e32833063e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung MYC, Shahed J, Jankovic J. Malignant Tourette syndrome. Movement Disorders. 2007;22:1743–1750. doi: 10.1002/mds.21599. [DOI] [PubMed] [Google Scholar]
- Conelea CA, Woods DW, Zinner SH, Budman C, Murphy T, Scahill LD, Compton SN, Walkup J. Exploring the impact of chronic tic disorders on youth: results from the Tourette Syndrome Impact Survey. Child psychiatry and human development. 2011;42:219–242. doi: 10.1007/s10578-010-0211-4. [DOI] [PubMed] [Google Scholar]
- Davila G, Berthier ML, Kulisevsky J, Jurado Chacon S. Suicide and attempted suicide in Tourette’s syndrome: a case series with literature review. The Journal of clinical psychiatry. 2010;71:1401–1402. doi: 10.4088/JCP.09l05669blu. [DOI] [PubMed] [Google Scholar]
- Enders CK. Using the expectation maximization algorithm to estimate coefficient alpha for scales with item-level missing data. Psychological methods. 2003;8:322–337. doi: 10.1037/1082-989X.8.3.322. [DOI] [PubMed] [Google Scholar]
- Enders CK. Applied Missing Data Analysis. The Guilford Press; New York: 2010. [Google Scholar]
- Freeman RD, Fast DK, Burd L, Kerbeshian J, Robertson MM, Sandor P. An international perspective on Tourette syndrome: selected findings from 3,500 individuals in 22 countries. Developmental medicine and child neurology. 2000;42:436–447. doi: 10.1017/s0012162200000839. [DOI] [PubMed] [Google Scholar]
- Gerson AC, Gerring JP, Freund L, Joshi PT, Capozzoli J, Brady K, Denckla MB. The Children’s Affective Lability Scale: a psychometric evaluation of reliability. Psychiatry Res. 1996;65:189–198. doi: 10.1016/s0165-1781(96)02851-x. [DOI] [PubMed] [Google Scholar]
- Gharatya A, Stern J, Man C, Williams D, Simmons H, Robertson M. Suicidality in patients with tourette’s syndrome. J Neurol Neurosur Ps. 2014;85:e3. [Google Scholar]
- Gould MS, King R, Greenwald S, Fisher P, Schwab-Stone M, Kramer R, Flisher AJ, Goodman S, Canino G, Shaffer D. Psychopathology Associated With Suicidal Ideation and Attempts Among Children and Adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:915–923. doi: 10.1097/00004583-199809000-00011. [DOI] [PubMed] [Google Scholar]
- Hawgood J, De Leo D. Anxiety disorders and suicidal behaviour: an update. Current Opinion in Psychiatry. 2008;21:51–64. doi: 10.1097/YCO.0b013e3282f2309d. [DOI] [PubMed] [Google Scholar]
- Hawton K, Saunders KEA, O’Connor RC. Self-harm and suicide in adolescents. The Lancet. 379:2373–2382. doi: 10.1016/S0140-6736(12)60322-5. [DOI] [PubMed] [Google Scholar]
- Hill RM, Castellanos D, Pettit JW. Suicide-related behaviors and anxiety in children and adolescents: a review. Clinical psychology review. 2011;31:1133–1144. doi: 10.1016/j.cpr.2011.07.008. [DOI] [PubMed] [Google Scholar]
- Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- Jain S, Carmody T, Trivedi MH, Hughes C, Bernstein I, Morris DW, Emslie GJ, Rush AJ. A Psychometric Evaluation of the CDRS and MADRS in Assessing Depressive Symptoms in Children. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1204–1212. doi: 10.1097/chi.0b013e3180cc2575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnco C, Salloum A, De Nadai AS, McBride N, Crawford EA, Lewin AB, Storch EA. Incidence, clinical correlates and treatment effect of rage in anxious children. Psychiatry Res. 2015;229:63–69. doi: 10.1016/j.psychres.2015.07.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaus NM, Mobilio A, King CA. Parent-Adolescent Agreement Concerning Adolescents’ Suicidal Thoughts and Behaviors. J Clin Child Adolesc. 2009;38:245–255. doi: 10.1080/15374410802698412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight T, Steeves T, Day L, Lowerison M, Jette N, Pringsheim T. Prevalence of tic disorders: a systematic review and meta-analysis. Pediatric neurology. 2012;47:77–90. doi: 10.1016/j.pediatrneurol.2012.05.002. [DOI] [PubMed] [Google Scholar]
- Kraft JT, Dalsgaard S, Obel C, Thomsen PH, Henriksen TB, Scahill L. Prevalence and clinical correlates of tic disorders in a community sample of school-age children. Eur Child Aadolescent Psychiatry. 2012;21:5–13. doi: 10.1007/s00787-011-0223-z. [DOI] [PubMed] [Google Scholar]
- Kumar G, Steer RA. Psychosocial Correlates of Suicidal Ideation in Adolescent Psychiatric Inpatients. Suicide and Life-Threatening Behavior. 1995;25:339–346. [PubMed] [Google Scholar]
- Leckman JF, Riddle MA, Hardin MT, Ort SI, Swartz KL, Stevenson J, Cohen DJ. The Yale Global Tic Severity Scale: initial testing of a clinician-rated scale of tic severity. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28:566–573. doi: 10.1097/00004583-198907000-00015. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Sholomskas D, Thompson D, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: A methodological study. Arch Gen Psychiatry. 1982;39:879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Zhang H, Vitale A, Lahnin F, Lynch K, Bondi C, Kim YS, Peterson BS. Course of tic severity in Tourette syndrome: the first two decades. Pediatrics. 1998;102:14–19. doi: 10.1542/peds.102.1.14. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Psychosocial characteristics of adolescents with a history of suicide attempt. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:60–68. doi: 10.1097/00004583-199301000-00009. [DOI] [PubMed] [Google Scholar]
- Lundh A, Kowalski J, Sundberg CJ, Gumpert C, Landén M. Children’s Global Assessment Scale (CGAS) in a naturalistic clinical setting: Inter-rater reliability and comparison with expert ratings. Psychiatry Res. 2010;177:206–210. doi: 10.1016/j.psychres.2010.02.006. [DOI] [PubMed] [Google Scholar]
- March JS, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, Burns B, Domino M, McNulty S, Vitiello B, Severe J. The Treatment for Adolescents With Depression Study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64:1132–1143. doi: 10.1001/archpsyc.64.10.1132. [DOI] [PubMed] [Google Scholar]
- Mayes TL, Bernstein IH, Haley CL, Kennard BD, Emslie GJ. Psychometric Properties of the Children’s Depression Rating Scale–Revised in Adolescents. J Child Adol Psychopharm. 2010;20:513–516. doi: 10.1089/cap.2010.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride NM, Johnco C, Salloum A, Lewin AB, Storch EA. Suicidality in pediatric anxiety. 2015 Manuscript in preparation. [Google Scholar]
- McGuire JF, Arnold E, Park JM, Nadeau JM, Lewin AB, Murphy TK, Storch EA. Living with tics: reduced impairment and improved quality of life for youth with chronic tic disorders. Psychiatry Res. 2015a;225:571–579. doi: 10.1016/j.psychres.2014.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire JF, Hanks CE, Lewin AB, Storch EA, Murphy TK. Social deficits in children with chronic tic disorders: Phenomenology, clinical correlates and quality of life. Compr Psychiat. 2013;54:1023–1031. doi: 10.1016/j.comppsych.2013.04.009. [DOI] [PubMed] [Google Scholar]
- McGuire JF, McBride NM, Piacentini J, Johnco C, Lewin AB, Murphy TK, Storch EA. The Premonitory Urge Revisited: An Evaluation of Tic Urge Phenomenology Using an Individualized Premonitory Urge for Tics Scale. 2015b doi: 10.1016/j.jpsychires.2016.09.007. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire JF, Piacentini J, Brennan EA, Lewin AB, Murphy TK, Small BJ, Storch EA. A meta-analysis of behavior therapy for Tourette Syndrome. Journal of psychiatric research. 2014;50:106–112. doi: 10.1016/j.jpsychires.2013.12.009. [DOI] [PubMed] [Google Scholar]
- Murphy TK, Lewin AB, Storch EA, Stock S. Practice Parameter for the Assessment and Treatment of Children and Adolescents With Tic Disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:1341–1359. doi: 10.1016/j.jaac.2013.09.015. [DOI] [PubMed] [Google Scholar]
- O’Neil-Rodriguez KA, Kendall PC. Suicidal ideation in anxiety-disordered youth: identifying predictors of risk. Journal of Clinical Child & Adolescent Psychology. 2014a;43:51–62. doi: 10.1080/15374416.2013.843463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neil-Rodriguez KA, Kendall PC. Suicidal Ideation in Anxiety-Disordered Youth: Identifying Predictors of Risk. J Clin Child Adolesc. 2014b;43:51–62. doi: 10.1080/15374416.2013.843463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neil KA, Puleo CM, Benjamin CL, Podell JL, Kendall PC. Suicidal ideation in anxiety-disordered youth. Suicide & life-threatening behavior. 2012;42:305–317. doi: 10.1111/j.1943-278X.2012.00091.x. [DOI] [PubMed] [Google Scholar]
- O’Neil KA, Puleo CM, Benjamin CL, Podell JL, Kendall PC. Suicidal ideation in anxiety-disordered youth. Suicide and life-threatening behavior. 2012;42:305–317. doi: 10.1111/j.1943-278X.2012.00091.x. [DOI] [PubMed] [Google Scholar]
- Peugh JL, Enders CK. Missing data in educational research: A review of reporting practices and suggestions for improvement. Rev Educ Res. 2004;74:525–556. [Google Scholar]
- Poznanski EO, Grossman JA, Buchsbaum Y, Banegas M, Freeman L, Gibbons R. Preliminary studies of the reliability and validity of the children’s depression rating scale. J Am Acad Child Ps. 1984;23:191–197. doi: 10.1097/00004583-198403000-00011. [DOI] [PubMed] [Google Scholar]
- Poznanski EO, Mokros HB. Children’s depression rating scale, Revised (CDRS-R) Western Psychological Services; Los Angeles: 1996. [Google Scholar]
- Poznanski EO, Mokros HB. Psychometric properties of the CDRS-R. In: Mokros HB, Poznanski EO, editors. Children’s Depression Rating Scale, Revised (CDRS-R) Western Psychological Services; Los Angeles, CA: 2005. pp. 52–53. [Google Scholar]
- Prinstein MJ, Nock MK, Simon V, Aikins JW, Cheah CS, Spirito A. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. Journal of consulting and clinical psychology. 2008;76:92–103. doi: 10.1037/0022-006X.76.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinherz HZ, Giaconia RM, Silverman AB, Friedman A, Pakiz B, Frost AK, Cohen E. Early Psychosocial Risks for Adolescent Suicidal Ideation and Attempts. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:599–611. doi: 10.1097/00004583-199505000-00012. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. Suicidal Ideation Questionnaire: Professional manual. Psychological Assessment Resources; Odessa, FL: 1988. [Google Scholar]
- Rezapour Z, Basharpour S, Abolghasemi A. The effects of effortful control and distress in tolerance in predicting externalizing problems. Int J Psychol Behav Res. 2013;2:325–331. [Google Scholar]
- Robertson MM. Mood disorders and Gilles de la Tourette’s syndrome: an update on prevalence, etiology, comorbidity, clinical associations, and implications. Journal of psychosomatic research. 2006;61:349–358. doi: 10.1016/j.jpsychores.2006.07.019. [DOI] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Afifi TO, de Graaf R, Asmundson GJ, ten Have M, Stein MB. Anxiety disorders and risk for suicidal ideation and suicide attempts: a population-based longitudinal study of adults. Archives of General Psychiatry. 2005;62:1249–1257. doi: 10.1001/archpsyc.62.11.1249. [DOI] [PubMed] [Google Scholar]
- Scahill L, Specht M, Page C. The Prevalence of Tic Disorders and Clinical Characteristics in Children. Journal of obsessive-compulsive and related disorders. 2014;3:394–400. doi: 10.1016/j.jocrd.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P. The Epidemiology of Suicide in Children and Young Adolescents. Journal of the American Academy of Child Psychiatry. 1981;20:545–565. doi: 10.1016/s0002-7138(09)61644-7. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A children’s global assessment scale (CGAS) Arch Gen Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Fisher P, Trautman P, Moreau D, Kleinman M, Flory M. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry. 1996;53:339–348. doi: 10.1001/archpsyc.1996.01830040075012. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The Distress Tolerance Scale: Development and Validation of a Self-Report Measure. Motiv Emot. 2005;29:83–102. [Google Scholar]
- Sourander A, Klomek AB, Niemela S, Haavisto A, Gyllenberg D, Helenius H, Sillanmaki L, Ristkari T, Kumpulainen K, Tamminen T, Moilanen I, Piha J, Almqvist F, Gould MS. Childhood predictors of completed and severe suicide attempts: findings from the Finnish 1981 Birth Cohort Study. Arch Gen Psychiatry. 2009;66:398–406. doi: 10.1001/archgenpsychiatry.2009.21. [DOI] [PubMed] [Google Scholar]
- Specht MW, Woods DW, Piacentini J, Scahill L, Wilhelm S, Peterson AL, Chang S, Kepley H, Deckersbach T, Flessner C, Buzzella BA, McGuire JF, Levi-Pearl S, Walkup JT. Clinical Characteristics of Children and Adolescents with a Primary Tic Disorder. Journal of developmental and physical disabilities. 2011;23:15–31. doi: 10.1007/s10882-010-9223-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger JH. Understanding the limitations of global fit assessment in structural equation modeling. Pers Indiv Differ. 2007;42:893–898. [Google Scholar]
- Storch EA, Hanks CE, Mink JW, McGuire JF, Adams HR, Augustine EF, Vierhile A, Thatcher A, Bitsko R, Lewin AB, Murphy TK. Suicidal thoughts and behaviors in children and adolescents with chronic tic disorders. Depression and anxiety. 2015a doi: 10.1002/da.22357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Johnco C, McGuire JF, Wu MS, McBride NM, Lewin AB. Family Accommodation in Children and Adolescents with Chronic Tic Disorders. 2015b doi: 10.1007/s00787-016-0879-5. Manuscript in preparation. [DOI] [PubMed] [Google Scholar]
- Storch EA, Jones AM, Lack CW, Ale CM, Sulkowski ML, Lewin AB, De Nadai AS, Murphy TK. Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. Journal of the American Academy of Child and Adolescent Psychiatry. 2012a;51:582–592. doi: 10.1016/j.jaac.2012.02.016. [DOI] [PubMed] [Google Scholar]
- Storch EA, Lack CW, Simons LE, Goodman WK, Murphy TK, Geffken GR. A Measure of Functional Impairment in Youth with Tourette’s Syndrome. J Pediatr Psychol. 2007a;32:950–959. doi: 10.1093/jpepsy/jsm034. [DOI] [PubMed] [Google Scholar]
- Storch EA, Morgan JE, Caporino NE, Brauer L, Lewin AB, Piacentini J, Murphy TK. Psychosocial Treatment to Improve Resilience and Reduce Impairment in Youth With Tics: An Intervention Case Series of Eight Youth. J Cog Psychother. 2012b;26:57–70. [Google Scholar]
- Storch EA, Murphy TK, Chase RM, Keeley M, Goodman WK, Murray M, Geffken GR. Peer Victimization in Youth with Tourette’s Syndrome and Chronic Tic Disorder: Relations with Tic Severity and Internalizing Symptoms. J Psychopathol Behav. 2007b;29:211–219. [Google Scholar]
- Storch EA, Murphy TK, Fernandez M, Krishnan M, Geffken GR, Kellgren AR, Goodman WK. Factor-analytic study of the Yale Global Tic Severity Scale. Psychiatry Res. 2007c;149:231–237. doi: 10.1016/j.psychres.2006.03.017. [DOI] [PubMed] [Google Scholar]
- Storch EA, Murphy TK, Geffken GR, Sajid M, Allen P, Roberti JW, Goodman WK. Reliability and validity of the Yale Global Tic Severity Scale. Psychological assessment. 2005;17:486–491. doi: 10.1037/1040-3590.17.4.486. [DOI] [PubMed] [Google Scholar]
- Sukhodolsky DG, Scahill L, Zhang H, Peterson BS, King RA, Lombroso PJ, Katsovich L, Findley D, Leckman JF. Disruptive Behavior in Children With Tourette’s Syndrome: Association With ADHD Comorbidity, Tic Severity, and Functional Impairment. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:98–105. doi: 10.1097/00004583-200301000-00016. [DOI] [PubMed] [Google Scholar]
- Tishler CL, Reiss NS, Rhodes AR. Suicidal behavior in children younger than twelve: a diagnostic challenge for emergency department personnel. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2007;14:810–818. doi: 10.1197/j.aem.2007.05.014. [DOI] [PubMed] [Google Scholar]
- Walker M, Moreau D, Weissman MM. Parents’ awareness of children’s suicide attempts. The American journal of psychiatry. 1990;147:1364–1366. doi: 10.1176/ajp.147.10.1364. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Rosenberg LA, Brown J, Singer HS. The validity of instruments measuring tic severity in Tourette’s syndrome. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:472–477. doi: 10.1097/00004583-199205000-00013. [DOI] [PubMed] [Google Scholar]