Abstract
Background
Pelvic tilt can affect the presence of the ischial spine sign and crossover sign. Numerous studies of pelvic tilt on radiographic measurements of pincer impingement have shown that increasing anterior tilt is associated with more radiographic signs of pincer impingement. However, to our knowledge, no study has directly compared supine and standing plain radiographs in patients with respect to lateral center-edge (LCE) angle, acetabular inclination, crossover sign, and ischial spine sign.
Questions/purposes
The purpose of this study was to evaluate the differences in supine and standing AP pelvis radiographs as they relate to the radiographic parameters of pincer impingement in an adult population evaluated for femoroacetabular impingement, specifically intrapelvic distances (sacrococcygeal to symphysis [SC-S] and coccyx tip to symphysis [T-S]), crossover sign (presence and percentage), LCE angle, inclination, and ischial spine sign.
Methods
Between August 2013 and June 2014, we obtained supine and standing radiographs for all new patients younger than 60 years who were evaluated for hip pain, when the diagnosis of fracture was not being considered; these formed the basis of this retrospective study. Patients were excluded if they had arthritis (Tönnis grade ≥ 2), lumbar fusion, previous hip surgery, or malrotated films. Forty-six hips, symptomatic side, met the inclusion criteria (age of patients, 33 ± 14 years; 13 males, 33 females). Radiographic data that were collected included SC-S distance, T-S distance, LCE angle, acetabular inclination, presence and percentage of crossover sign, and presence of ischial spine sign. A paired t-test was used to compare continuous variables and chi-square test was used for categorical variables. Two independent readers performed measurements.
Results
From supine to standing films, the T-S distance decreased from 19 ± 18 mm to 6 ± 19 mm (p < 0.001), and SC-S distance decreased from 47 ± 19 mm to 32 ± 20 mm (p < 0.001), indicating less pelvic tilt in the standing position. The number of hips that had crossover signs decreased from supine (n = 18, 39%) to standing (n = 9, 20%) (p = 0.039). The amount of crossover decreased from 23% ± 10% to 11% ±13% (p < 0.001). LCE angle did not change (27° ± 7° to 27° ± 8°) (p = 0.64) and inclination angle increased by a small amount (4.2° ± 5° to 5.3° ± 5°) (p = 0.002). The ischial spine sign decreased from supine (n = 20, 43%) to standing (n = 7, 15%) position (p = 0.003).
Conclusions
There is a decrease in the amount of pelvic tilt on standing AP pelvis radiographs resulting in a decrease in the incidence and amount of crossover sign and ischial spine sign, and a small increase in inclination. Standing radiographs should be the standard in evaluation of nonarthritic hip pain, specifically pincer femoroacetabular impingement. Surgeons should use caution in interpreting supine AP radiographs in the evaluation of pincer impingement, specifically the crossover sign.
Level of Evidence
Level III, diagnostic study.
Introduction
Femoroacetabular impingement (FAI) has become an increasingly recognized cause of hip pain and dysfunction, particularly in young, active individuals [3]. Pincer impingement is caused by global overcoverage of the acetabulum or focal overcoverage from acetabular retroversion. Determining the presence and severity of pincer impingement can be more difficult than cam impingement, especially in very subtle cases, because of variability in measurement and positioning, and correlation of radiographic measurements to in vivo conditions. There are many radiographic criteria that define pincer impingement; some parameters that have been well established in the evaluation of pincer impingement include the lateral center-edge angle (LCE), acetabular inclination, and crossover sign [2, 9, 13]. In 2003, Siebenrock et al. [9] reported that pelvic tilt can affect the presence of the ischial spine sign and crossover sign. Since then, a couple studies have shown the effect of pelvic tilt on radiographic measurements of pincer impingement with increasing anterior tilt associated with more radiographic signs of pincer impingement [4, 7]. These changes in radiographic parameters highlight the importance of pelvic position as it relates to pincer impingement.
Pelvis radiographs can be obtained with the patient in the supine or standing position. Standing radiographs may represent a more natural, functional pelvic position and may be more clinically relevant in the diagnosis and treatment of FAI, more specifically in patients who may have pincer impingement. The difference between supine and standing AP pelvis radiographs on pelvic tilt and these effects on the evaluation of pincer impingement have been studied in patients with dysplasia and more recently in patients with FAI [4, 8]. In a comparison of supine CT versus standing radiographs, Ross et al. [8] found an increase in anteversion in the supine reconstructed CT scans; however, they were unable to show a difference in crossover sign, ischial spine sign, and posterior wall sign. They did not measure LCE angle or inclination [8]. A cadaveric laboratory study showed differences in LCE angle, inclination, and crossover sign with increasing pelvic tilt [4]. However, we are not aware of any study that has directly compared supine and standing plain radiographs in patients with respect to LCE angle, acetabular inclination, crossover sign, and ischial spine sign.
The purpose of this study was to evaluate the differences in supine and standing AP pelvis radiographs as they relate to the radiographic parameters of pincer impingement in an adult population evaluated for FAI, specifically intrapelvic distances (sacrococcygeal to symphysis [SC-S] and coccyx tip to symphysis [T-S]), crossover sign, LCE angle, inclination, and ischial spine sign.
Patients and Methods
A retrospective radiographic review, from August 2013 to June 2014, of all patients who had supine and standing AP radiographs taken during evaluation for hip pain was done. During this study period, all patients younger than 60 years who were evaluated for hip pain when the diagnosis of fracture was not being considered received supine and standing radiographs and formed the basis of this retrospective study. Patients were excluded if the sacrococcygeal joint or coccyx tip was not observed owing to a lead shield or bowel gas obstruction (n = 31), if they had arthritis of Tönnis grade 2 or greater (n = 26), malrotation greater than 5 mm [5, 11] (n = 24), previous hip or proximal femoral surgery (n = 5), or previous lumbar fusion (n = 2). Malrotation was measured by drawing a vertical line through the center of the symphysis and the sacrum and measuring the distance between these two. Although there is no precedent set, a distance greater than 5 mm was considered to be overrotated. After exclusions, there were 46 patients (46 hips) of a possible 134 in the study group, symptomatic side only. The mean age of the patients at the time the radiographs were obtained was 33 ± 14 years (range, 14–56 years). There were 33 females (72%) and 13 males (28%).
Supine and standing radiographs were taken with the patients’ lower extremities internally rotated 15°. In the standing radiographs, patients were instructed to bear equal weight on both extremities. In both positions, no other specific instructions were given that might influence pelvic tilt. All radiographs were taken at one facility.
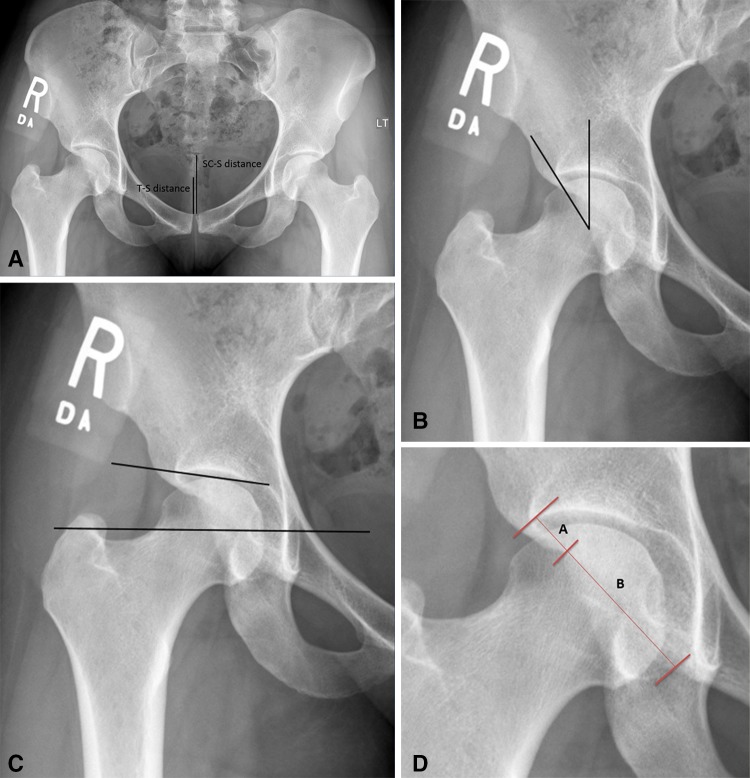
The supine and standing pelvic radiographs were evaluated for SC-S distance [9, 10], T-S distance [10], LCE angle [2], acetabular inclination [12], ischial spine sign, and presence and percentage of crossover sign [9] (Fig. 1). Radiographs were read by the senior author (TJJ) and an orthopaedic sports medicine fellow (AAE). Interobserver correlation was performed for all measurements. The value used for analysis was the mean of the two measurements from both observers. The interclass correlation coefficient between the two examiners was 0.98 for SC-S and T-S distances, 0.78 for inclination, 0.79 for LCE angle, 0.97 for amount of crossover sign, and 1 for presence or absence of crossover sign and presence of ischial spine sign.
Fig. 1A–D.
The radiographs show how measurements were performed for (A) SC-S distance and T-S distance; (B) LCE angle; (C) acetabular inclination; and (D) crossover sign and crossover percentage. The percentage of crossover is measured as A/(A + B). SC-S = sacrococcygeal to symphysis; T-S = coccyx tip to symphysis; LCE = lateral center edge.
Descriptive statistics were used for patient demographics. Student’s paired t-test was used to compare supine with standing T-S, SC-S, LCE, inclination, and amount of crossover. Presence of crossover sign was compared with the chi-square test. A p value less than 0.05 was considered significant.
Results
Intrapelvic distances (SC-S and T-S) decreased when measured on standing radiographs compared with supine radiographs, and these findings were observed in males and females. For all patients, the mean supine SC-S distance was 47 ± 19 mm and mean standing SC-S distance was 32 ± 20 mm (Table 1) (p < 0.001). In males, the mean SC-S distance was 38 ± 16 mm for supine and 22 ± 23 mm for standing (p < 0.001). In the females, the mean SC-S distance was 50 ± 19 mm for supine and 36 ± 17 mm for standing (p < 0.001). For all patients, the mean supine T-S distance was 19 ± 18 mm and mean standing T-S distance was 6 ± 19 mm (p < 0.001). In males, the mean T-S distance was 11 ± 21 mm for supine and −3 ± 25 mm for standing (p < 0.001). In females, the mean T-S distance was 22 ± 17 mm for supine and 9 ± 15 mm for standing (p < 0.001).
Table 1.
Pincer impingement values obtained on supine and standing AP radiographs
| Measurement (n = 46 patients; 46 hips) | Supine | Standing | p value |
|---|---|---|---|
| Tip-symphysis distance | 19 ± 18 | 6 ± 19 | p < 0.001 |
| Sacrococcygeal-symphysis distance | 47 ± 19 | 32 ± 20 | p < 0.001 |
| Acetabular inclination | 4 ± 5 | 5 ± 5 | p = 0.002 |
| Lateral center-edge angle | 27 ± 7 | 27 ± 8 | p = 0.64 |
| Ischial spine sign | 20 (43%) | 7 (15%) | p = 0.003 |
| Crossover sign (yes/no) | 18 (39%) | 9 (9%) | p = 0.039 |
| Crossover percentage | 23 ± 10 | 11 ± 13 | p = 0.001 |
The number of hips with a crossover sign present decreased from the supine (18 of 46, 39%) to the standing position (nine of 46, 9%; p < 0.001). In the measurement of percentage of crossover sign, the crossover percentage decreased from 23% ± 10% to 11% ± 13% (p = 0.001).
The LCE angle did not change 27° ± 7° to 27° ± 8° (p = 0.64) and the acetabular inclination angle increased a small amount, from 4.2° ± 5° to 5.3° ± 5° (p = 0.002) from the supine to standing position. The ischial spine sign was present in 20 of 46 (43%) hips on the supine radiograph and seven of 46 (15%) on the standing radiograph (p = 0.003).
Discussion
Awareness of the effect of pelvic tilt on the radiographic signs of pincer impingement is critical to accurate recognition and treatment of pincer FAI. The functional position of the pelvis in the standing position can change the radiographic signs of pincer impingement and by not appreciating this difference, initiating pincer impingement treatment based on a supine film can lead to inaccurate treatments, with potential bad outcomes. Our study showed differences in pelvic tilt when patients were in the supine and standing positions for AP radiographs. The decrease in pelvic tilt seen on a standing AP pelvis radiograph corresponded to less incidence and severity of the radiographic parameters for pincer impingement as shown by decreased presence and percentage of crossover sign, ischial spine sign, and even small increases in acetabular inclination.
This study has several limitations, the first of which is the small sample size. Although 46 hips were used for analysis, the inclusion of more hips can allow for more accurate analysis and detect trends and correlations. The reason for a small cohort was attributable to strict exclusion criteria, mainly malrotated films, which can have an effect on the presence or absence of a crossover sign [5]. The limitation of the quality of radiographs is important. The effect of rotation on the accuracy of the measured parameters is well known [6]. We sought to minimize this effect by limiting the amount of acceptable rotation, although we had no means of measuring rotation by degrees. We calculated rotation by the difference in a line through the symphysis and a line through the center of the sacrum. This difference was limited to 5 mm. Siebenrock et al. [9] reported a 6° rotation to the right would produce retroversion signs on the right acetabulum and disappearance of retroversion on the contralateral side if present at neutral. This corresponded to a 16-mm deviation of a line described in the current study, through the symphysis and sacrum. Based on those values, our 5-mm cutoff should have mitigated any measurement errors based on malrotation. During the study period, the senior author (TJJ) routinely obtained supine and standing radiographs as part of an imaging protocol that did not involve CT scans. To further understand pelvic tilt and the possible implications on pincer impingement, especially in females, both views were obtained. This exposes the patient to more radiation; however, this was thought to be acceptable because preoperative CT scans are not used. We now use only standing AP pelvis radiographs.
Siebenrock et al. [9] measured the distance from the sacrococcygeal joint and coccygeal tip to the pubic symphysis on 86 supine AP radiographs. Their values were similar to those in our study, indicating reproducible measurements. They reported SC-S distance of 32 mm in males and 47 mm in females, compared with our results of 38 mm and 50 mm, respectively. They also were able to show the effects of pelvic tilt on crossover and posterior wall signs in a cadaveric model. With increased pelvic inclination, they showed an increased crossover sign and with reclination, they showed less crossover sign. The major difference between their study and our study is the reclination and inclination that were artificially manipulated in the cadaveric model. We used standing films as the functional position and compared values from that position with values from the supine position. In another study [5], the ischial spine was found to be more prominent with forward tilt. Through these studies, it has been shown that increased forward tilt of the pelvis results in more-prominent crossover and ischial spine signs, both signs of acetabular retroversion and a cause for pincer impingement. This was further examined by Ross et al. [7] who used CT scans and specialized software to make pincer impingement measurements. They showed that increased pelvic tilt leads to increased presence and percentage of crossover signs, increased LCE angle, and decreased inclination. The limitation to these studies lies in the artificial manipulation of the pelvis to create this effect. With increased pelvis tilt causing increased pincer impingement findings being well known, the true functional tilt of a pelvis and how this affects pincer FAI is less known.
More recently, in an attempt to study supine and standing changes, Ross et al. [8] studied reformatted preoperative CT scans and compared them with standing AP radiographs. They measured percentage of anteversion, ischial spine signs, crossover sign, and posterior wall sign and showed only a significant difference in the amount of cranial and central anteversion measurements. They were unable to reach significance in the other variables with an additional limitation in that they did not measure inclination or LCE angle. To our knowledge, the current study is the first to compare supine and standing in vivo radiographs as they relate to pelvic tilt and pincer impingement values as they relate to LCE angle, inclination, presence and percentage of crossover sign, and ischial spine sign. The advantage of the current study is that the measurements and evaluation were done with tools used in a routine clinical setting without advanced imaging needs. This allows for easy reproducibility.
The observed effect sizes in terms of increased inclination in the standing position were small, and probably are not clinically important. Although it is interesting to find that these parameters do change significantly with changing tilt, they are unlikely to change clinical decision-making. By contrast, the large changes seen with the crossover sign probably are clinically important. Based on the decrease in crossover signs seen, if supine radiographs are used as the measure for pincer evaluation, this could lead to rim resections in patients who do not require them and possibly devastating consequences if acetabular surface area is removed when not needed [1].
We found that there is a decrease in the amount of pelvic tilt on standing AP pelvis radiographs resulting in a decrease in the incidence and amount of crossover sign and ischial spine sign, and a small increase in inclination. Standing radiographs should be the standard in evaluation of nonarthritic hip pain, specifically pincer FAI. Surgeons should use caution in interpreting supine AP radiographs in the evaluation of pincer impingement, specifically the crossover sign.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bhatia S, Lee S, Shewman E, Mather RC, 3rd, Salata MJ, Bush-Joseph CA, Nho SJ. Effects of acetabular rim trimming on hip joint contact pressures: how much is too much? Am J Sports Med. 2015;43:2138–2145. doi: 10.1177/0363546515590400. [DOI] [PubMed] [Google Scholar]
- 2.Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Domb BG, Stake CE, Botser IB, Jackson TJ. Surgical dislocation of the hip versus arthroscopic treatment of femoroacetabular impingement: a prospective matched-pair study with average 2-year follow-up. Arthroscopy. 2013;29:1506–1513. doi: 10.1016/j.arthro.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Henebry A, Gaskill T. The effect of pelvic tilt on radiographic markers of acetabular coverage. Am J Sports Med. 2013;41:2599–2603. doi: 10.1177/0363546513500632. [DOI] [PubMed] [Google Scholar]
- 5.Kakaty DK, Fischer AF, Hosalkar HS, Siebenrock KA, Tannast M. The ischial spine sign: does pelvic tilt and rotation matter? Clin Orthop Relat Res. 2010;468:769–774. doi: 10.1007/s11999-009-1021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Monazzam S, Agashe M, Hosalkar HS. Reliability of overcoverage parameters with varying morphologic pincer features: comparison of EOS® and radiography. Clin Orthop Relat Res. 2013;471:2578–2585. doi: 10.1007/s11999-013-3001-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ross JR, Nepple JJ, Philippon MJ, Kelly BT, Larson CM, Bedi A. Effect of changes in pelvic tilt on range of motion to impingement and radiographic parameters of acetabular morphologic characteristics. Am J Sports Med. 2014;42:2402–2409. doi: 10.1177/0363546514541229. [DOI] [PubMed] [Google Scholar]
- 8.Ross JR, Tannenbaum EP, Nepple JJ, Kelly BT, Larson CM, Bedi A. Functional acetabular orientation varies between supine and standing radiographs: implications for treatment of femoroacetabular impingement. Clin Orthop Relat Res. 2015;473:1267–1273. doi: 10.1007/s11999-014-4104-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 10.Tannast M, Murphy SB, Langlotz F, Anderson SE, Siebenrock KA. Estimation of pelvic tilt on anteroposterior X-rays: a comparison of six parameters. Skeletal Radiol. 2006;35:149–155. doi: 10.1007/s00256-005-0050-8. [DOI] [PubMed] [Google Scholar]
- 11.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 12.Tönnis D, Brunken D. Differentiation of normal and pathological acetabular roof angle in the diagnosis of hip dysplasia: evaluation of 2294 acetabular roof angles of hip joints in children [in German] Arch Orthop Unfallchir. 1968;64:197–228. doi: 10.1007/BF02171260. [DOI] [PubMed] [Google Scholar]
- 13.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]