Abstract
Objective
To evaluate double-bundle reconstruction of the medial patellofemoral ligament (MPFL) using a graft from the semitendinosus tendon and fixation with metal anchors over the medium term.
Methods
This was a prospective cross-sectional study. After approval from the research ethics committee, 31 patients with patellofemoral instability who underwent MPFL reconstruction by means of the anatomical double-bundle technique, with fixation using metal anchors, were analyzed between May 2010 and January 2015. To evaluate the effectiveness of the MPFL reconstruction surgery, the Kujala scale and the Tegner–Lysholm score were assessed before the procedure and one year afterwards, along with clinical data such as pain levels, range of motion and J sign. The data were tabulated in the Excel® software and were analyzed using the SPSS Statistics® software, version 21. The statistical analysis was performed using the Wilcoxon T test and the McNemar test.
Results
The mean preoperative score from the Kujala test was 45.64 ± 1.24 and the postoperative score was 94.03 ± 0.79 (p < 0.001). The preoperative Tegner–Lysholm score was 40.51 ± 1.61 and the postoperative score was 91.64 ± 0.79 (p < 0.001). The preoperative range of motion was 125.96 ± 2.11 and the postoperative range was 138.38 ± 1.49 (p < 0.05).
Conclusion
MPFL reconstruction by means of the anatomical double-bundle technique is easily reproducible, without episodes of recurrence, with satisfactory results regarding restoration of stability and function of the patellofemoral joint.
Keywords: Ligament patellar, Patellar dislocation, Patella, Knee, Reconstructive surgical procedures
Resumo
Objetivo
Avaliar, em médio prazo, a reconstrução do ligamento patelofemoral medial (LPFM) com duplo-feixe com enxerto do tendão semitendíneo e fixação com âncoras metálicas.
Métodos
Estudo prospectivo de corte transversal. De maio de 2010 a janeiro de 2015, após aprovação do comitê de ética em pesquisa, foram analisados 31 pacientes com instabilidade patelofemoral, submetidos à cirurgia de reconstrução do ligamento patelofemoral medial (LPFM) com a técnica anatômica do duplo-feixe com fixação com âncoras metálicas. Para avaliar a eficácia da cirurgia de reconstrução do LPFM, foram utilizadas a escala de Kujala e o escore de Tegner-Lysholm, antes do procedimento e após um ano. Foram avaliados os dados clínicos como o arco de movimento, presença do Sinal do J e nível de dor. Os dados foram tabulados no programa Excel® e analisados com o programa SPSS Statistics® versão 21. A análise estatística foi feita com o teste T de Wilcoxon e o teste de McNemar.
Resultados
A média dos resultados obtidos no pré-operatório com o teste de Kujala foi de 45,64 ± 1,24 e no pós-operatório de 94,03 ± 0,79 (p < 0,001). O escore do joelho de Tegner-Lysholm alcançado foi de 40,51 ± 1,61 no pré-operatório, para 91,64 ± 0,79 (p < 0,001) no pós-operatório. O arco de movimento obteve média de 12,596 ± 2,11 no pré-operatório e 13,838 ± 1,49 no pós-operatório (p < 0,05).
Conclusão
A reconstrução do LPFM com duplo-feixe é uma técnica de fácil reprodução, sem episódios de recidiva, e com resultados adequados para a restauração da estabilidade.
Palavras-chave: Ligamento patelar, Luxação patelar, Patela, Joelho, Procedimentos cirúrgicos reconstrutivos
Introduction
Patellar dislocation is a very common condition in orthopedics. It primarily affects young patients of both sexes, with a higher incidence in females, although in males, cases tend to be more severe.1
Recurrent patellar dislocation is defined as two or more episodes of dislocation, or symptoms of patellar instability that last for more than three months after the first dislocation episode.2
The medial patellofemoral ligament (MPFL) was described by Conlan et al.3 as the major restraint to lateral displacement of the patella, accounting for approximately 53% of the resistance, and controlling its trajectory during the execution of the full range of motion.3, 4 In most patients, this ligament is ruptured during acute patellar dislocation.5
Camanho et al.6 demonstrated that specific MPFL reconstruction after the dislocation episode leads to more favorable results when compared with conservative treatment, with lower chance of recurrence.
Therefore, it is known that surgical treatment is necessary to restore the patellar stability.7 A number of surgical techniques for MPFL reconstruction have been described for the treatment of this condition.8
Despite its biomechanical importance, the value of MPFL reconstruction has only recently been acknowledged, mostly in the last two decades.9 Despite the wide range of techniques described for its reconstruction, with different graft sources and fixation methods, there is growing evidence of good clinical outcomes for this surgery, but there are still important unsatisfactory results, around 12.5%, as in the findings of Singhal et al.10 The main complication after reconstruction is joint stiffness and pain after the procedure.
One cause of this complication is the non-anatomical graft positioning in MPFL reconstruction. It was observed that small errors of up to 5 mm from the ideal position or excessive tensioning of the graft (>2 N), cause an increase in the pressure forces on the medial aspect of the patella. This creates the need for techniques that can properly distribute graft tension on the patella and closer reproduction of the anatomy.11, 12, 13
From the mean and maximum flexion, Sandmeier et al.14 and Parker et al.15 demonstrated that isolated MPFL reconstruction was not able to restore normal patellar tracking. Failure to restore proper MPFL anatomy or isometry may cause this result and, therefore, limit the success for longer follow-ups.13
Kang et al.16 introduced the concept of functional bundles of the MPFL. The ligament has a thin layer that connects the femoral condyle to the superomedial border of the patella. The inferior fibers act as a static stabilizer, and the superior fibers act in the dynamic stabilization of the patella, due to their close relationship with the tendon of the vastus medialis obliquus.
The key to achieving favorable long-term results is attaching the graft in the most anatomical form possible. However, the ideal fixation method remains a matter of discussion. Different fixation methods have been described, such as fixation by bone tunnels, internal buttons, and anchors.17
Song et al.18 described a MPFL fixation method with two metal anchors without creating bone tunnels in the patella, in order to avoid complications such as patellar fractures. It has been postulated that clinical results with the use of metal anchors are comparable with published previous data regarding anatomic double-bundle MPFL reconstruction using bone tunnels in the patella.10, 19, 20, 21, 22, 23
This study aimed to assess the effectiveness of anatomic double-bundle MPFL reconstruction using the semitendinosus and fixation with metal anchors in the medial border of the patella.
Material and methods
The prospective study was conducted from May 2010 to January 2015, after approval of the Research Ethics Committee via Plataforma Brasil. The study included 31 patients with patellofemoral instability who underwent anatomic double-bundle MPFL reconstruction and fixation with metal anchors.
All patients had history of more than two episodes of patellar dislocation, and were selected to undergo surgical MPFL reconstruction through the double-bundle technique described by Song et al.,18 using Y-shaped metal anchors in the patella.21
Patients were attended in a referral orthopedics hospital by the institutions’ knee surgery group. They were assessed preoperatively and 12 months after the procedure. The physical examination was documented through the patellar apprehension test, J-sign, and range of motion. To evaluate the effectiveness of the reconstruction, the Kujala et al.24 clinical and functional questionnaires were applied, as well as the Lysholm–Tegner scores25; they were applied pre- and postoperatively.
The Kujala scale24 addresses symptoms related to anterior knee pain (patellofemoral disorders). It evaluates subjective symptoms, such as pain and function limitations, which are scored from 0 to 100, according to the complaints of the patient; 100 represents the complete absence of pain and limitations and 0, constant pain and several limitations. The assessed parameters are: pain, claudication, patellar subluxation, walking, stair climbing, and staying seated for long periods with the knees bent.
The Lysholm–Tegner score25 consists of eight questions with closed answers. Each question has an assigned value, which are then added. The final result is expressed both nominally and ordinally: “Excellent,” 95–100 points; “Good,” 84–94 points; “Regular,” 65–83 points; and “Bad,” for scores equal to or less than 64.
Patients with recurrent patellar dislocation (over two episodes), aged less than 45 years (mean 29 years), and with magnetic resonance imaging showing extensive rupture of the medial patellar stabilizers without osteochondral lesion were included.
The exclusion criteria comprised patients with congenital diseases; those with osteochondral lesions of the patella; those with distance between the anterior tibial tuberosity and trochlear groove (ATT-TG) greater than 20 mm, indicating medialization of the anterior tibial tuberosity (ATT); those older than 45 years; and those with inflammatory or post-traumatic arthritis.
No patient underwent further treatment with release of the lateral retinaculum, trochleoplasty, osteotomy, or cartilage procedures. All patients were assessed by medical history-taking, physical examination, radiographic assessments, and computed tomography in the preoperative period. The patellar height was measured using the Caton–Deschamps index26 and trochlear dysplasia, by the Dejour et al. classification.27
A semitendinosus tendon graft was used for MPFL reconstruction. The fixation was performed with two 5-mm metal anchors in the patella and an Y-shaped interference screw in the femur, for creating both ligament bundles and fixation in independent knee flexion angles.16
Surgical technique
The patient was placed in the dorsal decubitus position, under spinal anesthesia. Initially, an arthroscopy was performed in the affected knee for the identification of associated injuries or removal of intra-articular debris. Lateral retinacular release was not performed.
The semitendinosus tendon was then resected through a 2–3-cm incision over the insertion of the pes anserinus tendons. The fascia of the sartorius muscle was pushed out through an oblique incision, and the tendon was exposed and resected. The semitendinosus tendon was used, as its greater length and volume allowed for a better graft manipulation.
The point of graft fixation in the femur was identified with the aid of profile radioscopy, according to the parameters described by Schöttle et al.28 The medial approach to the femur was performed after the anatomical point was identified. Then, a guide-wire, anterior- and proximal-directed, was inserted, avoiding penetration into the posterior region of the femoral condyle.
After confirming the proper placement of the guide-wire, a tunnel was drilled with a power drill of the same diameter as the double graft. The folded semitendinosus tendon graft was inserted through the femoral tunnel (Fig. 1), and fixed with an interference screw (Fig. 2).
Fig. 1.
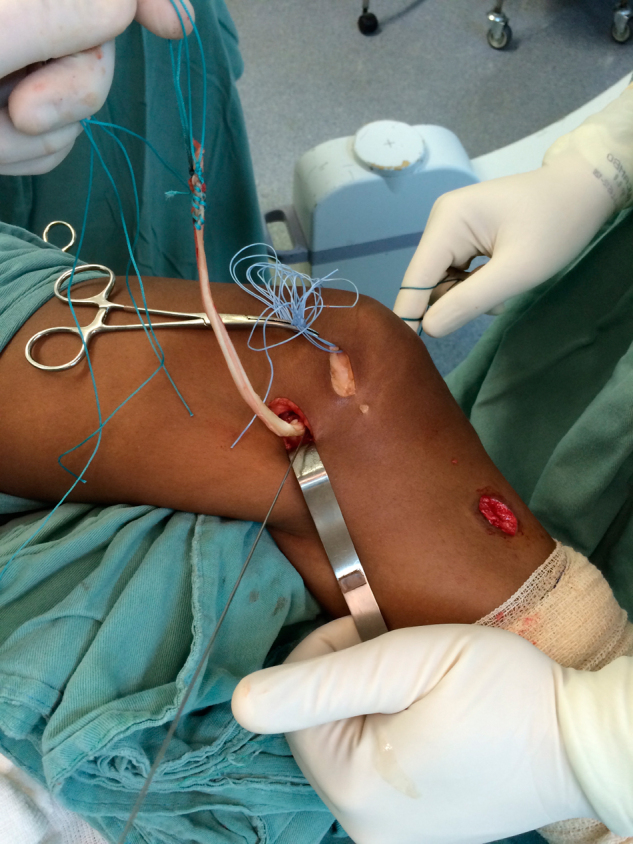
After the semitendinosus tendon was passed through the femoral tunnel, marked at 30 mm at the distal end.
Fig. 2.
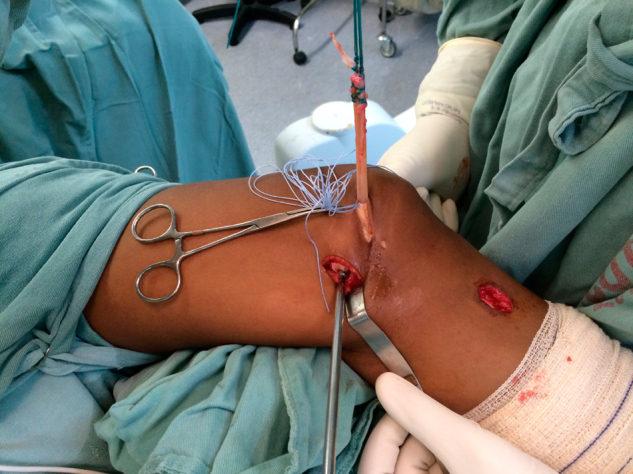
Passage of the graft in the femoral tunnel and fixation with metallic interference screw.
A longitudinal third incision was made under the medial border of the patella.29 The groove on the medial border of the patella was created above the transition with the posterior chondral face of the patella with the aid of a curette to accommodate the graft. Two 5-mm metal anchors were introduced and positioned in the two proximal thirds of the patella, 10–15 mm of the joint, with a distance of 15 mm between them. The most distal bundle, the inferior-straight (IS), was first established with the patella at approximately 30° of knee flexion; then, the most proximal bundle, the superior-oblique (SO), at about 60° of flexion, in accordance with the studies by Sadigursky et al.30 and Stephen et al.13 The remaining medial retinaculum was sutured under the tendon (Fig. 3).
Fig. 3.
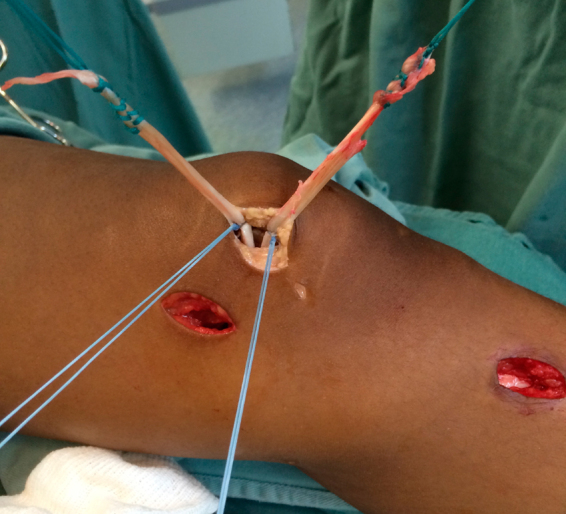
Fixation of the inferior-straight (IS) bundle, followed by the superior-oblique (SO) at independent knee flexion angles, 30° and 60°, respectively.
After fixation, the patellar position was verified through arthroscopic image and by the mobility of the patella at around one-quarter of its size.21
Postoperative period
The knee was immobilized in extension for two weeks. From the second day onwards, a physical therapy procedure was initiated, with progressive movement arc gain and isometric exercises. During the first three weeks, partial load was allowed as tolerated, with crutches. After the third week, full load was allowed as tolerated. Exercises in closed kinetic chain were allowed from the fourth week after surgery onwards.31
Contact sports and rotation were allowed after six months of the surgery.31
Statistical analysis
Data were tabulated in Excel® for Mac OSX and analyzed using SPSS Statistics® for Mac OSX, version 21. Categorical data were presented as proportions and quantitative data as medians, means, and standard deviations. Statistical analysis was performed with the Wilcoxon T test with alpha error of 0.05 and McNemar test, also with alpha error of 0.05.
Results
Table 1 describes the study sample. The study included 31 subjects, with a mean age of 29.38 and standard deviation (SD) of 8.11. Sixteen patients were female (51.6%), and 15 were male (48.4%). The most affected knee was the right, in 18 cases (58.06%); 13 subjects (41.9%) had the left knee affected.
Table 1.
Sociodemographic description.
| Variable | N (%) | Mean ± SD |
|---|---|---|
| Age | 31 | 29.38 ± 8.11 |
| Sex | ||
| Male | 15 (48.4) | |
| Female | 16 (51.6) | |
| Affected knee | ||
| Right | 18 (58.06) | |
| Left | 13 (41.9) | |
The patellar apprehension test was positive in all 31 (100%) patients preoperatively, and it was negative in 31 (100%) postoperatively. The J-sign was positive in 24 cases (77.4%) preoperatively and negative in seven (22.6%); positive in five cases (16.1%) and negative in 26 (83.9%) postoperatively. The Caton–Deschamps index was less than or equal to 1 in 21 cases (67.7%); it remained between 1.1 and 1.2 in five cases (16.1%), and was greater than or equal to 1.3 in five patients (16.1%). Eighteen cases (58.1%) had ATT-TG between 12 and 15 mm; 13 (41.9%), between 15 and 20 mm; and no case had ATT-TG above 20 mm. Dejour type A trochlear dysplasia was present in 14 subjects (45.2%); type B, in eight (25.8%); type C, in two (6.5%); and seven patients did not present any degree of dysplasia (22.5%). These findings are presented in Table 2.
Table 2.
Clinical data in the pre- and postoperative period.
| Variable | Preoperative N (%) | Postoperative N (%) |
|---|---|---|
| Patellar apprehension test | ||
| Positive | 31 (100) | 0 |
| Negative | 0 | 31 (100) |
| J-sign | ||
| Positive | 24 (77.4) | 5 (16.1) |
| Negative | 7 (22.6) | 26 (83.9) |
| Caton–Deschamps (mean ± SD) | 1.01 ± 0.17 | |
| ≤1.0 | 21 (67.7) | – |
| 1.1–1.2 | 5 (16.1) | – |
| ≥1.3 (high) | 5 (16.1) | – |
| ATT-TG (mean ± SD) | 15.4 ± 0.19 | |
| 12–15 mm (normal) | 18 (58.1) | – |
| 15–20 mm (high) | 13 (41.9) | – |
| >20 | 0 | – |
| Trochlear dysplasia | ||
| A | 14 (45.2) | – |
| B | 8 (25.8) | – |
| C | 2 (6.5) | – |
| Zero | 7 (22.6) | – |
The mean preoperative Kujala score24 was 45.64 (SD: 1.24; median: 49); the post-operative mean was 94.03 (SD: 0.79; median: 96), with statistical significance of p = 0.001. In the categorized analysis of the score, 31 (100%) subjects presented a poor preoperative score, and all subjects (100%) presented a good/excellent post-operative score. The mean preoperative Lysholm–Tegner25 score was 40.51 (SD: 1.61; median: 43) the postoperative mean was 91.64 (SD 0.79; median: 90), with statistical significance of 0.001. Table 3 presents the findings from the questionnaires. Additionally, no patient (100%) presented recurrence. The mean postoperative range of motion was 138.38 ± 1.49, and the mean preoperative range of motion was 125.96 ± 2.11, with statistical significance (p < 0.05).
Table 3.
Surgical and clinical scores.
| Variable | Preoperative N (%) | Postoperative N (%) | pa |
|---|---|---|---|
| Range of motion (median/mean ± SD) | 125/125.96 ± 2.11 | 140/138.38 ± 1.49 | 0.1 |
| Kujala score (median/mean ± SD) | 49/45.64 ± 1.24 | 96/94.03 ± 0.78 | 0.001 |
| Poor | 31 (100) | 0 | |
| Regular | 0 | 0 | |
| Good/excellent | 0 | 31 (100) | |
| Lysholm score | 43/40.51 ± 1.61 | 90/91.64 ± 0.79 | 0.001 |
| Poor | 31 (100) | 0 | |
| Regular | 0 | 0 | |
| Good | 0 | 18 (58.1) | |
| Excellent | 0 | 13 (41.9) | |
Wilcoxon T test, considered significant when p < 0.05.
Table 4 shows the analytical relationship between the pre- and postoperative patellar apprehension test. The difference between these results was statistically significant (p < 0.05).
Table 4.
Pre- and postoperative patellar apprehension test scores.
| Patellar apprehension test | |||
|---|---|---|---|
| Preoperative | Postoperative |
p | |
| Absent | Present | ||
| Present | 31 | 0 | 0.001 |
| Absent | 0 | 31 | |
The McNemar test was also applied to the J-sign ratio in both moments (pre- and postoperative), and a statistically significant difference in the periods studied was observed (Table 5).
Table 5.
Pre- and postoperative J-sign.
| J-sign | |||
|---|---|---|---|
| Preoperative | Postoperative |
pa | |
| Absent | Present | ||
| Present | 5 | 19 | 0.001 |
| Absent | 0 | 7 | |
McNemar test, considered significant when p < 0.05.
Discussion
From the 1990s onwards, MPFL reconstruction has become the technique of choice by most authors.32 Except in cases where ATT-TG is above 20 mm, or in cases of trochlear dysplasia with supratrochlear spur above 5 mm, isolated MPFL reconstruction has been proven to be a suitable and effective technique for the correction of patellar instability.33 Hopper et al.,34 when assessing 72 patients, proposed that isolated MPFL reconstruction should not be performed in patients with severe trochlear dysplasia. In over half of patients, a mild to moderate trochlear dysplasia was identified, but it was found not to influence the results. Patients with Dejour type D trochlear dysplasia27 were excluded from this study. Of the selected patients, eight (25.8%) had type B dysplasia, but without supratrochlear spurs above 5 mm.
This finding is similar to those by Arendt35 and Steiner et al.,36 who observed good results in patients with trochlear dysplasia who underwent isolated MPFL reconstruction. The postoperative range of motion improved by 15° in the median and 12° in the mean. The p-value was statistically significant.
In 2009, Kang et al.16 described the anatomy and function of both MPFL bundles. The SO bundle, along with the vastus medialis obliquus, tracks the kneecap medially and promotes a dynamic constraint. In turn, the IS bundle acts as static restraint to balance the resulting lateral forces acting on the patella. Thus, the reconstruction of both bundles could increase the stability during the first flexion angles and above 30° of knee flexion, which would allow for tension maintenance during the movement arc, promoted by each bundle independently.
Philippot et al.37 described the role of the medial stabilizing ligaments of the patella, medial patellotibial (MPTL) and medial patellomeniscal (MPML), which present their highest performance at angles above 45° of knee flexion. The reconstruction of MPTL has been gaining popularity in patients both in the growth phase (with open physis) and adults.38, 39, 40 During the movement arc, from the total length (0°) to 90° flexion, the MPTL and MPML contribute with 28% and 48% against the lateralization of the patella, 23% and 71% against inclination, and 32% and 92% against rotation, respectively. This finding cannot be disregarded when planning the correction of patellar instability.37, 38 However, despite the growing interest in MPTL reconstruction, in order to decrease the displacement of the patella at higher angles of flexion, possibly eliminating the inverted J-sign, to date there is no data proving the superiority of the clinical results in combined double-bundle reconstruction of the MPTL and MPML.37, 39
The fixation of MPFL bundles at different angles (the IS bundle at 0° and the OS at 30°) was suggested by Kang et al.41 However, the authors believe that the OS bundle should be fixated at 60° with minimal tension, and the IS bundle at around 30°, based on the studies by Sadigursky et al.30 and Han et al.,20 in order to prevent overpressure in the medial aspect of the patella and, consequently, anterior knee pain. Stephen et al.13 demonstrated that the anatomical reconstruction positioned with a 2-N tension under the graft, fixed at 30° or 60° of knee flexion, restores normal contact pressure in the lateral patellar aspect as well as its appropriate flexion-extension path. Song et al.,42 in a biomechanical study, demonstrated that the length of the MPFL fibers varies with the degree of knee flexion. The superior fibers reach their maximum length at smaller angles; the inferior fibers, at greater flexion angles.
The authors observed improvements in patellar subluxation at around 20° to 30° of knee flexion, demonstrated through negative results in the apprehension test. The inverted J-sign was positive in 24 patients (77.4%) preoperatively and in only five (16.1%) postoperatively. The five patients (16.1%) whose Caton–Deschamps index was greater than 1.3, which characterized high patella, showed the persistence of the J-sign, confirming this as a factor of poor prognosis in isolated MPFL reconstruction regarding the persistence of residual subluxation of the patella in knee flexion angles above 45°.
In a meta-analysis conducted by Singhal et al.,10 a persistent patellar instability was observed, from subtle to frank, in around 4.6% of cases postoperatively. Stiffness was the most frequent complication (30%). However, the attachment of the double-bundle graft was made in the same angle and under the same tension. In this case, the procedure is performed by initially fixating the patella. This C-shaped graft fixation technique could lead to worse outcomes, with increased restriction of normal patellar mobility. Kang et al.21, 41 demonstrated that Y-shaped graft fixation, which starts in the femur, followed by fixation of each bundle independently, can improve patellar function and reduce possible complications.43
Through the Kujala24 and Lysholm–Tegner scores,25 the effectiveness of double-bundle MPFL reconstruction can be demonstrated. The results show a recovery of the biomechanical function of the patella. The mean Kujala score24 increased from 45.64 preoperatively to 94.03 postoperatively. In the Lysholm–Tegner,25 there was an increase from 40.51 preoperatively to 91.64 postoperatively. Of the 31 patients, 18 (58.1%) moved to “good” and 13 patients (41.9%) to “excellent” outcomes. These results are very close to those found in the meta-analysis by Singhal et al.,10 but with fewer complications.
In that study, the authors used metal anchors for graft fixation in the patella. An advantage of the use of anchors is the possibility of using shorter graft, such as the gracilis tendon, although the semitendinosus tendon was chosen due to its greater length, which allows for a better handling and control of its strength, in addition to its larger volume, with better fixation in the femoral tunnel with interference screw.17 Furthermore, the use of anchors allows for smaller incisions, with improved cosmetic results. A reduced exposure of the patella is possible. By not using bone tunnels in the patella, the risk of fractures or patellar cartilage injury is reduced. It can be regarded as a relatively simple technique, resulting in reduced surgical time.18 The fixation anchors also allow for the closest possible reproduction of the MPFL anatomy and independent fixation of the ligament bundles, at 30° and 60° of knee flexion.
Several authors have shown that a non-anatomical positioning of the femoral tunnel interferes with patellofemoral kinematics. Elias and Cosgarea11 found that a tunnel positioning error, more proximal in the femur, can overload the medial compartment of the patella and lead to degeneration of the medial aspect, in addition to graft rupture or reconstruction failure. Similarly, Thaunat and Erasmus43 suggested that a non-anatomic graft placement leads to hypertensioning and hence greater incidence of postoperative stiffness. In turn, a more distal position would be incapable of tensioning the graft enough to restrict patellar dislocation.15 Amis et al.9 demonstrated that a positioning error in the frontal plane is better tolerated, i.e., positioning the graft more anteriorly or posteriorly is less harmful than a more proximal or distal position. For graft positioning, radioscopy was used in all cases, identifying the anatomical femoral insertion point described by Schöttle et al.28 Thus, complications due to positioning errors could be identified and corrected at the time of surgery.
Based on experimental and anatomical studies, the authors argue that MPFL reconstruction should be made both isometrically and anatomically.10, 22 Given the results of this study, as well as those by Wang et al.,22 MPFL reconstruction should be performed anatomically, with independent fixation of both bundles.16, 21, 41
In this study, it was observed that the double-bundle MPFL reconstruction using semitendinosus tendon graft and fixation with metal anchors in independent flexion angles presented favorable results, without recurrence episodes, pain, or overload in the patellofemoral joint, and with satisfactory range of motion and possibility of return to previous activities.
A weakness of the study was the fact that it was conducted at a single center, without a comparison group using other correction techniques for patellar instability. Nonetheless, the present sample was very close to that of studies on double-bundle MPFL reconstruction in the literature.5, 7, 8, 10
Conclusion
Double-bundle MPFL reconstruction using fixation with metal anchors and independent bundle fixation was shown to be effective by the results observed in this study, such as the significant improvement in the score of the protocols used without relapse episodes and the reduction of subluxation at angles above 45° of knee flexion.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
To the members of the knee surgery group of the Clínica Ortopédica Traumatológica (COT).
Footnotes
Study conducted at Clínica Ortopédica Traumatológica (COT), Salvador, BA, Brazil.
References
- 1.Bitar A.C., Demange M.K., D’Elia C.O., Camanho G.L. Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med. 2012;40(1):114–122. doi: 10.1177/0363546511423742. [DOI] [PubMed] [Google Scholar]
- 2.Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23(5):260–263. doi: 10.1007/s002640050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conlan T., Garth W.P., Lemons J.E. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682–693. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Desio S.M., Burks R.T., Bachus K.N. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 5.Colvin A.C., West R.V. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751–2762. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 6.Camanho G.L., Viegas A.C., Bitar A.C., Demange M.K., Hernandez A.J. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy. 2009;25(6):620–625. doi: 10.1016/j.arthro.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Redziniak D.E., Diduch D.R., Mihalko W.M., Fulkerson J.P., Novicoff W.M., Sheibani-Rad S. Patellar instability. J Bone Joint Surg. 2009;91(9):2264–2275. [PubMed] [Google Scholar]
- 8.Shah J.N., Howard J.S., Flanigan D.C., Brophy R.H., Carey J.L., Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amis A.A., Firer P., Mountney J., Senavongse W., Thomas N.P. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10(3):215–220. doi: 10.1016/s0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 10.Singhal R., Rogers S., Charalambous C.P. Double-bundle medial patellofemoral ligament reconstruction with hamstring tendon autograft and mediolateral patellar tunnel fixation: a meta-analysis of outcomes and complications. Bone Joint J. 2013;95(7):900–905. doi: 10.1302/0301-620X.95B7.31417. [DOI] [PubMed] [Google Scholar]
- 11.Elias J.J., Cosgarea A.J. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34(9):1478–1485. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 12.Servien E., Fritsch B., Lustig S., Demey G., Debarge R., Lapra C. In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med. 2011;39(1):134–139. doi: 10.1177/0363546510381362. [DOI] [PubMed] [Google Scholar]
- 13.Stephen J.M., Kaider D., Lumpaopong P., Deehan D.J., Amis A.A. The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am J Sports Med. 2014;42(2):364–372. doi: 10.1177/0363546513509230. [DOI] [PubMed] [Google Scholar]
- 14.Sandmeier R.H., Burks R.T., Bachus K.N., Billings A. The effect of reconstruction of the medial patellofemoral ligament on patellar tracking. Am J Sports Med. 2000;28(3):345–349. doi: 10.1177/03635465000280031001. [DOI] [PubMed] [Google Scholar]
- 15.Parker D.A., Alexander J.W., Conditt M.A., Uzodinma O.N., Bryan W.J. Comparison of isometric and anatomic reconstruction of the medial patellofemoral ligament: a cadaveric study. Orthopedics. 2008;31(4):339–343. doi: 10.3928/01477447-20080401-28. [DOI] [PubMed] [Google Scholar]
- 16.Kang H.J., Wang F., Chen B.C., Su Y.L., Zhang Z.C., Yan C.B. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1511–1516. doi: 10.1007/s00167-010-1090-8. [DOI] [PubMed] [Google Scholar]
- 17.Lenschow S., Schliemann B., Gestring J., Herbort M., Schulze M., Kösters C. Medial patellofemoral ligament reconstruction: fixation strength of 5 different techniques for graft fixation at the patella. Arthroscopy. 2013;29(4):766–773. doi: 10.1016/j.arthro.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Song S.Y., Kim I.S., Chang H.G., Shin J.H., Kim H.J., Seo Y.J. Anatomic medial patellofemoral ligament reconstruction using patellar suture anchor fixation for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2431–2437. doi: 10.1007/s00167-013-2730-6. [DOI] [PubMed] [Google Scholar]
- 19.Schöttle P.B., Hensler D., Imhoff A.B. Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):147–151. doi: 10.1007/s00167-009-0868-z. [DOI] [PubMed] [Google Scholar]
- 20.Han H., Xia Y., Yun X., Wu M. Anatomical transverse patella double tunnel reconstruction of medial patellofemoral ligament with a hamstring tendon autograft for recurrent patellar dislocation. Arch Orthop Trauma Surg. 2011;131(3):343–351. doi: 10.1007/s00402-010-1173-5. [DOI] [PubMed] [Google Scholar]
- 21.Kang H., Cao J., Yu D., Zheng Z., Wang F. Comparison of 2 different techniques for anatomic reconstruction of the medial patellofemoral ligament: a prospective randomized study. Am J Sports Med. 2013;41(5):1013–1021. doi: 10.1177/0363546513480468. [DOI] [PubMed] [Google Scholar]
- 22.Wang C., Ma L., Zhou J., Ji G., Wang H., Wang F. Double-bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop. 2013;37(4):617–624. doi: 10.1007/s00264-013-1788-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zanon G., Marullo M., Benazzo F. Double-bundle medial patellofemoral ligament reconstruction with a single patellar tunnel. Arthrosc Tech. 2013;2(4):e401–e404. doi: 10.1016/j.eats.2013.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kujala U.M., Osterman K., Kormano M., Nelimarkka O., Hurme M., Taimela S. Patellofemoral relationships in recurrent patellar dislocation. J Bone Joint Surg Br. 1989;71(5):788–792. doi: 10.1302/0301-620X.71B5.2584248. [DOI] [PubMed] [Google Scholar]
- 25.Lysholm J., Tegner Y. Knee injury rating scales. Acta Orthop. 2007;78(4):445–453. doi: 10.1080/17453670710014068. [DOI] [PubMed] [Google Scholar]
- 26.Phillips C.L., Silver D.T., Schranz P.J., Mandalia V. The measurement of patellar height: a review of the methods of imaging. J Bone Joint Surg Br. 2010;92(8):1045–1053. doi: 10.1302/0301-620X.92B8.23794. [DOI] [PubMed] [Google Scholar]
- 27.Dejour H., Walch G., Nove-Josserand L., Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 28.Schöttle P.B., Schmeling A., Rosenstiel N., Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 29.Mochizuki T., Nimura A., Tateishi T., Yamaguchi K., Muneta T., Akita K. Anatomic study of the attachment of the medial patellofemoral ligament and its characteristic relationships to the vastus intermedius. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):305–310. doi: 10.1007/s00167-012-1993-7. [DOI] [PubMed] [Google Scholar]
- 30.Sadigursky D., Gobbi R.G., Pereira C.A.M., Pécora J.R., Camanho G.L. Método de ensaio biomecânico para análise da isometricidade na reconstrução do ligamento patelofemoral medial. Rev Bras Ortop. 2012;47(5):598–605. doi: 10.1016/S2255-4971(15)30010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fisher B., Nyland J., Brand E., Curtin B. Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy. 2010;26(10):1384–1394. doi: 10.1016/j.arthro.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 32.Mulford J.S., Wakeley C.J., Eldridge J.D. Assessment and management of chronic patellofemoral instability. J Bone Joint Surg Br. 2007;89(6):709–716. doi: 10.1302/0301-620X.89B6.19064. [DOI] [PubMed] [Google Scholar]
- 33.Schöttle P., Schmeling A., Romero J., Weiler A. Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg. 2009;129(3):305–309. doi: 10.1007/s00402-008-0712-9. [DOI] [PubMed] [Google Scholar]
- 34.Hopper G.P., Leach W.J., Rooney B.P., Walker C.R., Blyth M.J. Does degree of trochlear dysplasia and position of femoral tunnel influence outcome after medial patellofemoral ligament reconstruction? Am J Sports Med. 2014;42(3):716–722. doi: 10.1177/0363546513518413. [DOI] [PubMed] [Google Scholar]
- 35.Arendt E.A., Dejour D. Patella instability: building bridges across the ocean a historic review. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):279–293. doi: 10.1007/s00167-012-2274-1. [DOI] [PubMed] [Google Scholar]
- 36.Steiner T.M., Torga-Spak R., Teitge R.A. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34(8):1254–1261. doi: 10.1177/0363546505285584. [DOI] [PubMed] [Google Scholar]
- 37.Philippot R., Boyer B., Testa R., Farizon F., Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):331–336. doi: 10.1007/s00167-011-1598-6. [DOI] [PubMed] [Google Scholar]
- 38.Sobhy M.H., Mahran M.A., Kamel E.M. Midterm results of combined patellofemoral and patellotibial ligaments reconstruction in recurrent patellar dislocation. Eur J Orthop Surg Traumatol. 2013;23(4):465–470. doi: 10.1007/s00590-012-0999-7. [DOI] [PubMed] [Google Scholar]
- 39.Zaffagnini S., Grassi A., Marcheggiani Muccioli G.M., Luetzow W.F., Vaccari V., Benzi A. Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2491–2498. doi: 10.1007/s00167-013-2751-1. [DOI] [PubMed] [Google Scholar]
- 40.Giordano M., Falciglia F., Aulisa A.G., Guzzanti V. Patellar dislocation in skeletally immature patients: semitendinosous and gracilis augmentation for combined medial patellofemoral and medial patellotibial ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1594–1598. doi: 10.1007/s00167-011-1784-6. [DOI] [PubMed] [Google Scholar]
- 41.Kang H.J., Cao J.H., Pan S., Wang X.J., Yu D.H., Zheng Z.M. The horizontal Y-shaped graft with respective graft tension angles in anatomical two-bundle medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2445–2451. doi: 10.1007/s00167-014-3005-6. [DOI] [PubMed] [Google Scholar]
- 42.Song S.Y., Pang C.H., Kim C.H., Kim J., Choi M.L., Seo Y.J. Length change behavior of virtual medial patellofemoral ligament fibers during in vivo knee flexion. Am J Sports Med. 2015;43(5):1165–1171. doi: 10.1177/0363546514567061. [DOI] [PubMed] [Google Scholar]
- 43.Thaunat M., Erasmus P.J. Management of overtight medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17(5):480–483. doi: 10.1007/s00167-008-0702-z. [DOI] [PubMed] [Google Scholar]


