Abstract
Because of the anatomical peculiarities of the subtrochanteric region, treatment of fractures in this region remains challenging. The undeniable evolution of implants has not been accompanied by the expected decrease in the complication rate.
The aim of this study was to discuss critical points in detail, such as preoperative planning, reduction tactics and the current scientific evidence concerning treatment of subtrochanteric fractures of the femur.
Keywords: Hip fractures/etiology, Hip fractures/diagnosis, Hip fractures/surgery, Hip fractures/classification
Resumo
Devido às particularidades anatômicas da região subtrocantérica, o tratamento das fraturas nessa região permanece desafiador. A incontestável evolução dos implantes não foi acompanhada pela esperada diminuição no índice de complicações.
O objetivo do presente estudo é discutir, minuciosamente, pontos críticos como planejamento pré-operatório, táticas de redução e evidências científicas atuais no tratamento das fraturas subtrocantéricas do fêmur.
Palavras-chave: Fraturas do quadril/etiologia, Fraturas do quadril/diagnóstico, Fraturas do quadril/cirurgia, Fraturas do quadril/classificação
Introduction
Subtrochanteric fractures take place in the proximal region of the femur, whose anatomical definition is difficult and controversial. Fielding1 proposed a definition that is still frequently used: the subtrochanteric region corresponds to the interval between the lesser trochanter and around 5–7.5 cm below it, toward the femoral isthmus. The fractures can extend to the proximal region (trochanteric or femoral neck) or distal region (diaphyseal).1, 2
They account for 25% of the proximal fractures of the femur and their distribution is bimodal. Young male adults involved in high-energy traumas present complex fracture patterns; whereas old patients, predominantly females, generally present spiral fractures.1
Due to the anatomical peculiarity and, especially, due to the difficulty in reduction, the treatment of subtrochanteric fractures is still a great challenge to the traumatologist, not only because of the osteosynthesis difficulties, but also for the still frequent complications. The next section addresses important aspects that will help to explain the peculiarities of the treatment of the subtrochanteric fractures.
Why are their anatomical and biomechanic characteristics unique?
The subtrochanteric region of the femur is an area of great stress concentration and, due to its muscular insertions, is subjected to several deforming forces. The classic deformities are flexion (provoked by the iliopsoas), abduction (by the gluteus medius), and external rotation (by the external rotators) of the proximal fragment of the femur. The adductors, inserted in the distal region of the femur, are responsible for the varus deformity.2, 3
Due to the predominance of cortical bone, the subtrochanteric region presents a more precarious vascularization than the transtrochanteric region, which makes the consolidation of the fractures difficult. Complex fractures with medial support failure present elevated rates of fixation failure and reoperation.2
Is there an ideal classification system for subtrochanteric fractures?
There are over 15 described classifications for subtrochanteric fractures.1, 3, 4, 5 The Fielding1 classification subdivides the fractures according to their anatomical location: type 1 fractures are those at the lesser trochanter level; type 2 fractures are those located between 2.5 and 5 cm below the lesser trochanter; and type 3 fractures are those located between 5 and 7.5 cm below the lesser trochanter. Its value is only historical, due to its low reproducibility on account of ethnic variations.
The classification by Russell-Taylor takes into account the entirety of the piriformis fossa (more appropriately termed trochanteric fossa).1 Type I fractures do not extend into the trochanteric fossa (IA: without extension to the lesser trochanter; IB: with extension to the lesser trochanter). Type II fractures extend into the trochanteric fossa (IIA: without comminution of the lesser trochanter; IIB: serious comminution of the lesser trochanter). When the classification was created, the authors searched for a guideline for the method of fracture fixation with the implants available at the time. Type I fractures, without involvement of the trochanteric fossa, could be treated with first-generation intramedullar implants using the trochanteric fossa as an entry point. Type II fractures, with involvement of the trochanteric fossa, should be treated with extramedullary implants. With the development and enhancement of intramedullary devices – second- and third-generation intramedullary (IM) nails – this classification lost its prognostic and therapeutic guidance value, since the involvement of the trochanteric fossa was no longer a counterindication for intramedullar fixation.
The classification by Seinsheimer is perhaps the most used and practical for subtrochanteric fractures of the femur, since it is characterized by the number of fractured fragments and emphasizes not only the involvement of the medial cortex, but also of the lateral cortex.2
Loizou et al.4 also described a classification system based on the degree of comminution of the subtrochanteric fracture. However, this classification did not gain popularity in the field.
The AO classification takes into account the bone (femur = 3), the location (diaphysis = 2), the energy of the trauma (A, B, or C), and the mechanism (1, 2, or 3). Per convention, the subtrochanteric fracture is characterized as “1”.
Although it is widely used and recommended by the OTA, the AO classification has the disadvantage of including the subtrochanteric fracture in a group of fractures with different mechanical and biological behavior: the diaphyseal fractures.2
Recently, Guyver et al.5 proposed a classification called MCG. This system is subdivided into three types: type I: lesser and greater trochanter are preserved; type II: the greater trochanter is involved, but the lesser trochanter is intact; type III: the lesser trochanter is involved (most unstable).
In their original work, these authors also assessed the intra- and inter-observer reproducibility of the MCG, Russell-Taylor, AO, and Seinsheimer classifications. Despite the poor intra- and inter-observer reproducibility of all the classifications (Kappa 0.35), the MCG system presented the highest agreement, followed by the Russell-Taylor, AO, and Seinsheimer classifications.5
The authors believe that there is not yet an ideal classification system for the subtrochanteric fractures of the femur that is able to guide treatment and establish prognosis with satisfactory inter-observer reproducibility. In their practice, the authors have adopted the AO classification for ease of communication and because it is the reference in current publications.
Surgical vs. non-surgical treatment
The non-surgical treatment of subtrochanteric fractures leads to deformities caused by shortening and rotational deviation, hindering the return to the functional activities prior to the injury. However, the critical point of non-surgical treatment is related to the morbimortality increase caused by extended periods of immobilization and decubitus. Atelectasis, pneumonia, thromboembolic events, and bedsores are complications frequently associated with extended periods of decubitus.
Currently, the non-surgical treatment of subtrochanteric fractures of the femur is an exception, and must be performed only in patients with extremely serious clinical co-morbidities that counterindicate anesthetic and/or surgical procedures.6
When to operate a patient with subtrochanteric fracture of the femur?
Patient victims of high-energy trauma must be assessed according to the ATLS protocol. After clinical stabilization, the local conditions, such as skin integrity, neurovascular status, and the degree of soft tissue injury, must be thoroughly assessed.
In severely polytraumatized cases, in which even after initial resuscitation maneuvers the patient remains hemodynamically unstable, immediate external fixation is indicated for damage control.
In stable patients, the ideal period for the definitive fixation of the fracture is within the first 48 h. If, for any reason, definitive fixation of the fracture is not possible within this period, skeletal traction or, preferably, external fixation is indicated for temporary stabilization.2
Khan et al.7 reviewed 52 studies, with a total of 291,413 patients, and demonstrated that surgery conducted within the first 48 h reduces complications and mortality.
The authors opt for early fixation of subtrochanteric fractures of the femur (within the first 48 h after the trauma) whenever possible.
Which the best fixation method for subtrochanteric fractures? The evolution of the implants
The plates
Although it was developed for the treatment of transtrochanteric fractures, DHS has also been widely used for the fixation of subtrochanteric fractures. However, due to the characteristic biomechanics of the subtrochanteric fractures, several authors reported unsatisfactory results in nearly 70% of the cases in which this implant was used.2 As DHS is a dynamic system, progressive medialization of the diaphysis and fixation failure can occur.
The blade plate and the DCS, developed by the AO group, are viable options for the treatment of subtrochanteric fractures, especially when techniques of indirect reduction and biological fixation are used.2
Boopalan et al.8 reported the results of 22 patients with 23 subtrochanteric fractures of the femur treated with blade plates using the minimally invasive biological technique. Nineteen patients did not need additional surgeries. Two patients were reoperated due to varus reductions, and one patient underwent surgical debridement due to infection. The functional results were considered excellent in ten patients, good in one patient, and poor in two patients.
Due to its low cost and the familiarity of surgeons with both the DCS and blade plates, these implants persist as important and frequent fixation options for subtrochanteric fractures in Brazil. However, it is worth noting that, when using blade plates or DCS, minimally invasive techniques should be preferred in order to preserve the biological integrity of the region. The conventional approach (open) promotes important local devascularization and increases the rates of infection, pseudarthrosis, and osteosynthesis failure.
Recently, some authors reported the use of plates with fixed angle screws in the treatment of subtrochanteric fractures of the femur.
Saini et al.,9 using proximal femur-locking compression plate (PF-LCP – Sharma Surgicals, India) for the treatment of comminuted subtrochanteric fractures in 35 patients, achieved consolidation in all cases. Two patients presented infection, two presented 1-cm shortening, and one evolved with vicious consolidation in external rotation. The authors concluded that biological fixation with PF-LCP in comminuted subtrochanteric fractures promotes stable fixation, with a high rate of consolidation and low rate of complications.
Recently, Wirtz et al.10 reported a high rate of complications with the open reduction technique and internal fixation with PF-LCP (Synthes, West Chester PA, USA). Of 19 patients with subtrochanteric fractures who underwent fixation with PF-LCP, seven presented important complications, such as infection, cut-out, and varus collapse, requiring new surgical procedures. Those authors emphasized that, contrary to intramedullary implants, PF-LCPs do not allow for fracture accommodation, which is critical for consolidation in fractures with loss of posteromedial support.
Amit et al.11 described the use of the Less Invasive Stabilization System (LISS – DePuy Synthes) plate, originally developed for distal fractures of the femur, in the fixation of subtrochanteric fractures. In a non-conventional manner, those authors performed osteosynthesis with the contralateral reverse plate and emphasized the potential advantages of the described technique: the easiness of accommodation of the plate in the proximal region of the femur, the fact that the femoral radius curvature is followed by the plate curvature, and the possibility of fixation of osteoporotic bones with the use of multiplanar fixed-angle screws.
IM nails
In 1964, Zickel12 developed an IM nail specifically for the treatment of subtrochanteric fractures. This system is considered the precursor of the intramedullary implants currently used for subtrochanteric fractures.
Wiss and Brien13 revolutionized the treatment of subtrochanteric fractures with the use of IM nails on the contralateral side. When inverted, the nail hole for proximal blockage allowed for the positioning of a screw directed toward the femoral neck. Thus, those authors could treat fractures that, according to the Russel-Taylor classification, were counterindicated for intramedullary fixation due to trochanteric fossa involvement.
Although initially developed for the treatment of transtrochanteric fractures, cephalomedullary nails were, naturally, used in subtrochanteric fractures. They quickly gained popularity and, due to their favorable biomechanical properties and minimally invasive application techniques, presented satisfactory results with low reoperation rates.
Umer et al.14 reported the results of the treatment of subtrochanteric fractures with IM nails with spiral slides for cephalic blockage. In their study, with 33 patients, the authors obtained consolidation in 94% of the cases up to six months after surgery, with mean surgical time of 2.4 h and mean hospitalization of seven days.
Borens et al.15 treated 90 patients with subtrochanteric fracture of the femur using Gamma Nail (Stryker) IM nails. With a mean follow-up of two years, no infections were reported. One patient presented a fracture below the nail, which was exchanged for a longer nail. Two patients presented osteosynthesis failure due to varus reduction. One of them was treated with nail replacement and bone graft, while the other was treated with removal of the nail, blade-plating osteosynthesis, and bone graft. All 87 other patients presented consolidation with primary surgery. The authors emphasized that, due to the favorable biomechanical properties of the implant (intramedullary tutor), early rehabilitation and load are allowed even in osteoporotic patients.
Is there an ideal entry point for cephalomedullary nails?
The definition of the nail's entry point depends on the implant chosen for the fixation. Classically, straight nails utilize the piriformis fossa (more appropriately called trochanteric fossa) as entry point16; nails with 6° lateral inclination enter through the top of the greater trochanter; and nails with 10° lateral inclination enter laterally to the greater trochanter.
However, Streubel et al.,17 when analyzing 50 X-rays of normal hips, demonstrated that the ideal entry point for nails with 6° lateral inclination was slightly medial to the top of the greater trochanter in 70% of the studied patients and lateral in 23%.
The authors believe that preoperative surgical planning is essential to prevent additional deformities caused by an unsuitable entry point.
Current evidence
Herscovici et al.18 conducted a retrospective study in which they compared intra- and extra-medullary implants in the treatment of subtrochanteric fractures of the femur. The authors demonstrated that, although intramedullary fixation was quicker and had less bleeding, the functional results and the complication rates were similar. They emphasized that the surgeon must carefully assess the fracture pattern to identify when the most familiar technique will lead to satisfactory functional results with low complication rates.
Mirbolook et al.19 compared functional results and rate of complications in the treatment of subtrochanteric fractures of the femur with two surgical techniques: open reduction and internal fixation with trochanteric PF-LCP (DePuy Synthes), and fixation with cephalomedullary nails using the biological technique (indirect reduction). There was no statistically significant difference between both groups regarding function, consolidation, and complications.
Kuzyk et al.20 assessed studies that compared intra- and extra-medullary fixations for the treatment of subtrochanteric fractures of the femur. The systematic revision consisted of three studies with level of evidence I and nine with level IV. Those authors reported a level of recommendation B favorable to intramedullary implants regarding the surgery time and the rate fixation failure.
In the treatment of subtrochanteric fractures, the authors of the present study prefer fixation with long cephalomedullary nails due to their biomechanical properties and to the possibility of minimally invasive fixation.
However, much more important than the choice of the implant is the quality of fracture reduction.
In a well-reduced fracture, the literature demonstrates that the results of intra- and extra-medullary fixation using the biological technique (minimally invasive) are similar.
Traction table or conventional radiolucent table?
There are several possible positions for the fixation of subtrochanteric fractures. The choice should be based on the type of fixation (intra- or extra-medullary) and on the experience of the surgeon with the chosen technique. The most important factors are that appropriate images can be obtained and that the positioning of the trunk and limbs does not hinder the surgical procedure.
Traction table
The patient can be positioned in the “banana” position, with the trunk adducted, the superior ipsilateral limb fixed in shoulder adduction, and the inferior contralateral limb in inferior position (“scissors” position).
This positioning facilitates the placing of the image intensifier both for creating the entry point and the proximal and distal blockages of the IM nail.
The adduction of the fractured inferior limb to facilitate the entry point should be avoided due to the varus deviation caused by this positioning.
Conventional table
Fixation is possible both in supine position and in complete lateral decubitus or oblique lateral decubitus. In lateral decubitus, although the entry point is easier, the surgeon must be careful that the fracture is not in medial angulation (varus) due to the action of gravity and muscular traction.
In the supine position, a cushion can be placed to facilitate the creation of the entry point and the proximal blockage in intramedullary fixation. The disadvantage of the supine position is the need for an assistant to traction the member for fracture reduction. As an option to manual traction, the surgeon can use an AO distractor.
Baratz et al.21 assessed radiation exposure, comparing the lateral and supine positioning for the treatment of subtrochanteric fractures, and observed lower radiation exposure in the supine position.
There is no consensus in the literature regarding the best positioning of the patient and the need for a traction table. The surgeon should position the patient based on the technique with which he/she is most familiar.
In this practice, the authors prefer to use the traction table with the patient in the “banana” position (adducted trunk and inferior limbs in “scissors” position). With this positioning, both the intra- and extra-medullary fixations are possible, and the surgeon has an open surgical field for the acquisition of perioperative images.
How to reduce subtrochanteric fractures?
Despite the evolution of the fixation methods, all authors recognize that the reduction is the most important isolated factor in the prognosis of subtrochanteric fractures. The authors emphasize the need to aim for fracture reduction with restoration of the cervico-diaphyseal angle and of the shaft, in addition to the correction of the rotation and flexion of the proximal fragment, using methods that do not cause greater biological damage.
Riehl et al.,22 in a retrospective study assessing the results of intramedullary fixation in 35 patients, observed that unsatisfactory reductions – those with over 10° in any plane – led to problems in the consolidation.
Miedel et al.,6 when analyzing the results of intramedullary fixation in the treatment of subtrochanteric fractures in the elderly, observed good reduction in 50% and acceptable reduction in 50%. In the group whose reduction was considered by the surgeons as good, no patients were reoperated, while in the group with acceptable reduction, 23% needed reoperation. Those authors emphasized the importance of a satisfactory reduction, since an “acceptable” reduction can lead to the need for a new surgery in one-quarter of the patients.
Due to the countless deforming forces that act in the subtrochanteric region, the indirect reduction of the fractures is usually difficult.
However, the evolution of implants has been accompanied by the evolution in reduction instruments. Currently, there are instruments that allow for an effective reduction of the fracture with minimally invasive techniques.
Yoon et al.23 reported the results of the fixation of subtrochanteric fractures of the femur using Weber clamps for the reduction. In fractures with predominance of flexion of the proximal fragment, the authors performed a 5 cm lateral incision for introducing the clamps. In fractures with a long spiral component in the sagittal plan, the authors recommend a lateral incision and introduction of a hemostat rested on the anterior cortex of the femur, toward the medial cortex. Subsequently, the clamps must be lifted to correct the flexion and the external rotation of the proximal fragment of the femur. A new anterior transquadricipital incision is performed for the introduction of the Weber clamp. In a study with ten patients operated with this technique, the mean time for reduction was 12 min (between six and 21 min) and all fractures consolidated with only a partial loss of reduction. It is important to point out that the reduction forceps must be maintained until the end of the proximal and distal blockages of the nail.
Ball-spike pushers, Schanz screws, or Steinmann pins, placed through an anterior punctiform access route, can be used as a joystick to reduce the flexion of the proximal fragment in subtrochanteric fractures of the femur.
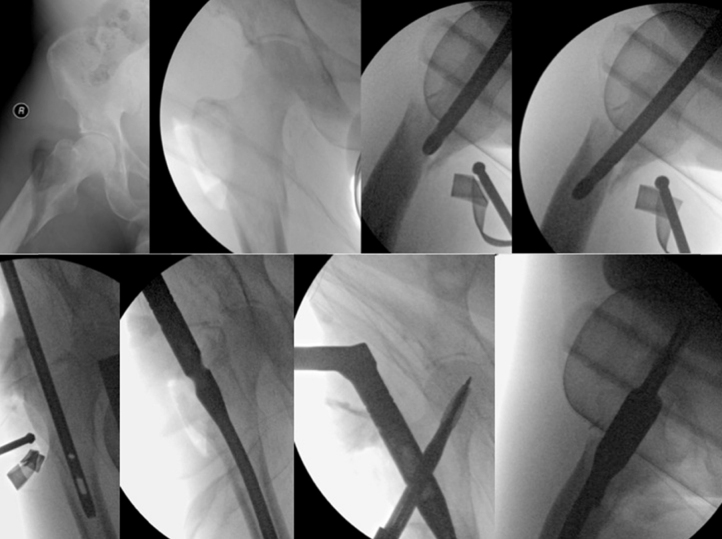
In patients with good bone quality and integrity of the posterior cortex of the femur, the nail itself can be used as an instrument to reduce the flexion of the proximal femoral fragment (Fig. 1).
Fig. 1.
Reduction of the subtrochanteric fracture with cephalomedullary nail.
For the correction of varus, ball-spike pushers or Schanz screws can be used, as illustrated in Fig. 2.
Fig. 2.
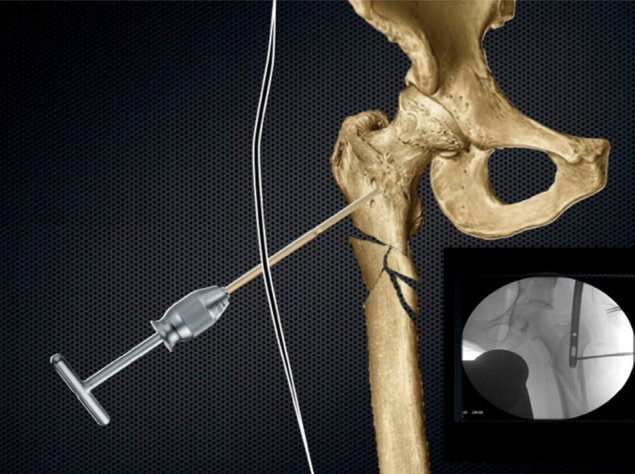
Use of a Schanz screw to reduce varus.
Some authors add cerclage to maintain the reduction of the fracture.24, 25 Nonetheless, there are questions regarding the potential bone devascularization caused by cerclage.
Tomás et al.24 performed cerclage in 12 patients who underwent osteosynthesis with cephalomedullary nails for the fixation of subtrochanteric fractures. All the fractures were consolidated and there were no superficial or deep infections.
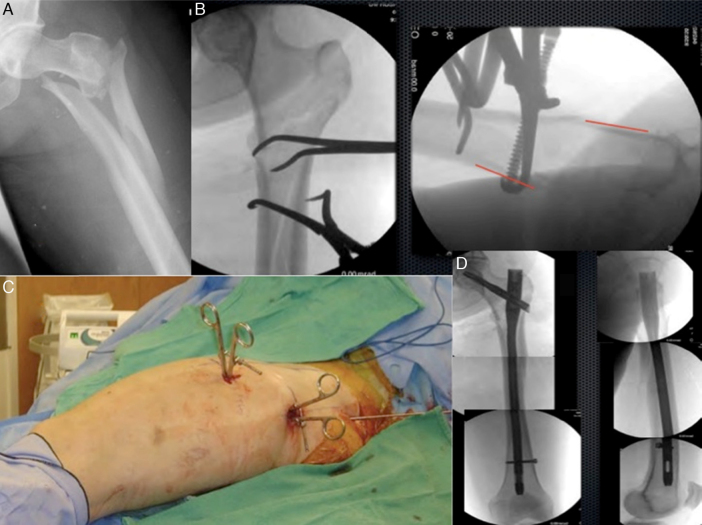
Fig. 3 illustrates the treatment of a complex subtrochanteric fracture reduced with percutaneous clamps and fixed with a long cephalomedullary nail.
Fig. 3.
Images kindly shared by Professor Gerald Lang, from the University of Wisconsin. (A) Complex subtrochanteric fracture; (B) X-rays of the proximal femur in anteroposterior and profile showing the reduction with forceps; (C) Images of the thigh of the patient showing percutaneous introduction of the forceps, anterior and laterally; (D) Images of the post-operative period showing fixation with long cephalomedullary nail (trochanteric fixation nail [TFN] – DePuy Synthes).
Seyhan et al.25 compared the results of the treatment of subtrochanteric fractures of the femur with IM nails and three reduction techniques: forceps, cerclage, and Poller screws. The group in which the reduction forceps were used had the longest interval until total load (p = 0.032) and lowest Harris hip score after one year (p = 0.02). Conversely, the Poller group presented longest surgical time. There was no difference among the groups regarding the quality of the reduction, consolidation time, complications, and the rate of reoperations.
Complications
Even with modern implants, the complication rates in the treatment of the subtrochanteric fractures remain high (around 21%). Infection, pseudarthrosis, vicious consolidation, and loss of the reduction are the most frequent complications.2
Regardless of the fixation method, the quality of the reduction lowers the stress on the implant, increases the bone contact, and makes the consolidation easier.
Early fixation failure generally results from technical problems related with the surgical procedure. Late failures occur as a consequence of unsatisfactory reduction, low bone stock, inadequate choice of implant, complex fracture patterns, smoking, and poor local vascularization.2
Z-effect and reverse Z-effect are complications resulting from the treatment of proximal fractures of the femur with cephalomedullary implants that have two cephalic blockage screws. These complications have been described as migrations of the cephalic screws in opposite directions due to factors such as low bone stock, excessively lateral entry point, varus reductions, and severe medial comminution.26
Another described complication is the impingement of the nail in the anterior cortex in the distal third of the femur. Studies have demonstrated that patients of low stature (<1.6 m, especially women and Asians) have increased radius of curvature of the femur, which might predispose them to distal femoral fractures due to the impingement of the nail in the anterior cortex in the distal third of the femur. Nails with unsuitable radial curvature, as well as incorrect entry point, are also risk factors for this complication.27, 28
Final considerations
Due to the unfavorable anatomical peculiarities, despite the development of new implants, the treatment of subtrochanteric fractures of the femur still presents an elevated rate of complications and remains challenging.
Regardless of the stability principle and of the method chosen for treatment of the subtrochanteric fracture, the key point to reduce the risk of complications is the quality of the reduction.
Whenever possible, indirect reduction with preservation of the soft-tissue envelope must be attempted. If not possible, reduction techniques with percutaneous clamps or cerclage can be used.
Even though blade plates, DCS, or blocked trochanteric plates remain as viable options for the treatment of subtrochanteric fractures, the IM nails, due to their biomechanical properties and minimally invasive fixation technique, present advantages such as lower surgery time and lower rate of reoperations.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Fielding J.W. Subtrochanteric fractures. Clin Orthop Relat Res. 1973;(92):86–99. doi: 10.1097/00003086-197305000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Joglekar S.B., Lindvall E.M., Martirosian A. Contemporary management of subtrochanteric fractures. Orthop Clin North Am. 2015;46(1):21–35. doi: 10.1016/j.ocl.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Rocha L.R. Fratura subtrocantérica. Fixação com haste intramedular. OrtoTrauma: SBOT. 2013:19–22. [Google Scholar]
- 4.Loizou C.L., McNamara I., Ahmed K., Pryor G.A., Parker M.J. Classification of subtrochanteric femoral fractures. Injury. 2010;41(7):739–745. doi: 10.1016/j.injury.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 5.Guyver P.M., McCarthy M.J., Jain N.P., Poulter R.J., McAllen C.J., Keenan J. Is there any purpose in classifying subtrochanteric fractures? The reproducibility of four classification systems. Eur J Orthop Surg Traumatol. 2014;24(4):513–518. doi: 10.1007/s00590-011-0780-3. [DOI] [PubMed] [Google Scholar]
- 6.Miedel R., Törnkvist H., Ponzer S., Söderqvist A., Tidermark J. Musculoskeletal function and quality of life in elderly patients after a subtrochanteric femoral fracture treated with a cephalomedullary nail. J Orthop Trauma. 2011;25(4):208–213. doi: 10.1097/BOT.0b013e3181eaaf52. [DOI] [PubMed] [Google Scholar]
- 7.Khan S.K., Kalra S., Khanna A., Thiruvengada M.M., Parker M.J. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40(7):692–697. doi: 10.1016/j.injury.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Boopalan P.R., Jepegnanam T.S., Nithyananth M., Venkatesh K., Cherian V.M. Functional outcome of biological condylar blade plating of subtrochanteric fractures. J Orthop Sci. 2012;17(5):567–573. doi: 10.1007/s00776-012-0244-6. [DOI] [PubMed] [Google Scholar]
- 9.Saini P., Kumar R., Shekhawat V., Joshi N., Bansal M., Kumar S. Biological fixation of comminuted subtrochanteric fractures with proximal femur locking compression plate. Injury. 2013;44(2):226–231. doi: 10.1016/j.injury.2012.10.037. [DOI] [PubMed] [Google Scholar]
- 10.Wirtz C., Abbassi F., Evangelopoulos D.S., Kohl S., Siebenrock K.A., Krüger A. High failure rate of trochanteric fracture osteosynthesis with proximal femoral locking compression plate. Injury. 2013;44(6):751–756. doi: 10.1016/j.injury.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 11.Amit S., Shehkar A., Vivek M., Shekhar S., Biren N. Fixation of subtrochanteric fractures in two patients with osteopetrosis using a distal femoral locking compression plate of the contralateral side. Eur J Trauma Emerg Surg. 2010;36:263–269. doi: 10.1007/s00068-009-8237-7. [DOI] [PubMed] [Google Scholar]
- 12.Zickel R.E. A new fixation device for subtrochanteric fractures of the femur: a preliminary report. Clin Orthop Relat Res. 1967;(54):115–123. [PubMed] [Google Scholar]
- 13.Wiss D.A., Brien W.W. Subtrochanteric fractures of the femur. Results of treatment by interlocking nailing. Clin Orthop Relat Res. 1992;(283):231–236. [PubMed] [Google Scholar]
- 14.Umer M., Rashid H., Shah I., Qadir I. Use of femoral nail with spiral blade in subtrochanteric fractures. Acta Orthop Traumatol Turc. 2014;48(1):32–36. doi: 10.3944/AOTT.2014.3084. [DOI] [PubMed] [Google Scholar]
- 15.Borens O., Wettstein M., Kombot C., Chevalley F., Mouhsine E., Garofalo R. Long gamma nail in the treatment of subtrochanteric fractures. Arch Orthop Trauma Surg. 2004;124(7):443–447. doi: 10.1007/s00402-004-0711-4. [DOI] [PubMed] [Google Scholar]
- 16.Ansari Moein C.M., Gerrits P.D., ten Duis H.J. Trochanteric fossa or piriform fossa of the femur: time for standardised terminology? Injury. 2013;44(6):722–725. doi: 10.1016/j.injury.2012.08.049. [DOI] [PubMed] [Google Scholar]
- 17.Streubel P.N., Wong A.H., Ricci W.M., Gardner M.J. Is there a standard trochanteric entry site for nailing of subtrochanteric femur fractures? J Orthop Trauma. 2011;25(4):202–207. doi: 10.1097/BOT.0b013e3181e93ce2. [DOI] [PubMed] [Google Scholar]
- 18.Herscovici D., Jr., Pistel W.L., Sanders R.W. Evaluation and treatment of high subtrochanteric femur fractures. Am J Orthop (Belle Mead NJ) 2000;29(9 Suppl.):27–33. [PubMed] [Google Scholar]
- 19.Mirbolook A., Siavashi B., Jafarinezhad A.E., Jahromi S.K., Farahmand M., Rad M.R. Subtrochanteric fractures: comparison of proximal femur locking plate and intramedullary locking nail fixation outcome. Indian J Surg. 2013:1–5. doi: 10.1007/s12262-013-1004-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuzyk P.R., Bhandari M., McKee M.D., Russell T.A., Schemitsch E.H. Intramedullary versus extramedullary fixation for subtrochanteric femur fractures. J Orthop Trauma. 2009;23(6):465–470. doi: 10.1097/BOT.0b013e3181acfdfd. [DOI] [PubMed] [Google Scholar]
- 21.Baratz M.D., Hu Y.Y., Zurakowski D., Appleton P., Rodriguez E.K. The primary determinants of radiation use during fixation of proximal femur fractures. Injury. 2014;45(10):1614–1619. doi: 10.1016/j.injury.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Riehl J.T., Koval K.J., Langford J.R., Munro M.W., Kupiszewski S.J., Haidukewych G.J. Intramedullary nailing of subtrochanteric fractures – does malreduction matter? Bull Hosp Jt Dis (2013) 2014;72(2):159–163. [PubMed] [Google Scholar]
- 23.Yoon Y.C., Jha A., Oh C.W., Durai S.K., Kim Y.W., Kim J.H. The pointed clamp reduction technique for spiral subtrochanteric fractures: a technical note. Injury. 2014;45(6):1000–1005. doi: 10.1016/j.injury.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 24.Tomás J., Teixidor J., Batalla L., Pacha D., Cortina J. Subtrochanteric fractures: treatment with cerclage wire and long intramedullary nail. J Orthop Trauma. 2013;27(7):e157–e160. doi: 10.1097/BOT.0b013e31826fc03f. [DOI] [PubMed] [Google Scholar]
- 25.Seyhan M., Unay K., Sener N. Comparison of reduction methods in intramedullary nailing of subtrochanteric femoral fractures. Acta Orthop Traumatol Turc. 2012;46(2):113–119. doi: 10.3944/AOTT.2012.2639. [DOI] [PubMed] [Google Scholar]
- 26.Pires R.E., Santana E.O., Jr., Santos L.E., Giordano V., Balbachevsky D., Dos Reis F.B. Failure of fixation of trochanteric femur fractures: clinical recommendations for avoiding Z-effect and reverse Z-effect type complications. Patient Saf Surg. 2011;5:17. doi: 10.1186/1754-9493-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tyagi V., Yang J.H., Oh K.J. A computed tomography-based analysis of proximal femoral geometry for lateral impingement with two types of proximal femoral nail anterotation in subtrochanteric fractures. Injury. 2010;41(8):857–861. doi: 10.1016/j.injury.2010.04.018. [DOI] [PubMed] [Google Scholar]
- 28.Ostrum R.F., Levy M.S. Penetration of the distal femoral anterior cortex during intramedullary nailing for subtrochanteric fractures: a report of three cases. J Orthop Trauma. 2005;19(9):656–660. doi: 10.1097/01.bot.0000154481.46693.69. [DOI] [PubMed] [Google Scholar]