Abstract
Background
The recent discovery of cell cycle arrest biomarkers, tissue inhibitor of metalloproteinases (TIMP)-2 and insulin-like growth factor binding protein 7 (IGFBP7), has led to a newly available clinical test for acute kidney injury. The performance of these markers in preclinical studies has not been established. Therefore, we sought to evaluate the performance of TIMP-2 and IGFBP7 in rats undergoing cecal ligation and puncture.
Methods
In this secondary analysis, we analyzed banked urine samples from 60 Sprague-Dawley rats undergoing cecal ligation and puncture (CLP). Samples were obtained from baseline, 18 h after CLP, at the end of fluid resuscitation (22 h after CLP), and again 24 h later. We measured TIMP-2 and IGFBP7 and compared the results to acute kidney injury by RIFLE criteria for creatinine using area under the receiver operating characteristic curve (AUC). The primary endpoint was moderate-to-severe acute kidney injury (AKI) (I or F criteria), and the primary time point was immediately after fluid resuscitation. Secondary outcomes included mortality and comparisons with other biomarkers: cystatin C and neutrophil gelatinase-associated lipocalin (NGAL) in both urine and plasma.
Results
After fluid resuscitation, urine [TIMP-2] and [IGFBP7] were significantly higher in animals developing moderate-to-severe AKI (p = 0.002 and p = 0.01). AUC of [TIMP-2]·[IGFBP7] for AKI was 0.89 (95 % CI 0.80–0.98). By contrast, the next best AUC was seen with plasma cystatin C (0.78; 95 % CI 0.65–0.90). [TIMP-2]·[IGFBP7] also predicted mortality (AUC 0.69; 95 % CI 0.53–0.85).
Conclusions
In this experimental model of sepsis in the rat, cell cycle arrest biomarkers TIMP-2 and IGFBP7 are valid predictors of acute kidney injury.
Keywords: Acute kidney injury, Sepsis, Tissue inhibitor of metalloproteinases (TIMP)-2, Insulin-like growth factor binding protein 7 (IGFBP7), Cell cycle arrest, Biomarkers
Background
Recently, two novel urinary biomarkers, tissue inhibitor of metalloproteinases-2 (TIMP-2) and insulin-like growth factor-binding protein 7 (IGFBP7), were validated for predicting moderate-to-severe acute kidney injury (AKI) (stages 2 and 3 by Kidney Disease Improving Global Outcome (KDIGO) [1] criteria) in critically ill patients [2, 3]. Both TIMP-2 and IGFBP7 are markers of G1 cell-cycle arrest, which prevents cells from dividing when potentially injured [4], and both appear to respond to a wide variety of cellular stressors including inflammation, ischemia, oxidative stress, drugs, and toxins [5–7]. Furthermore, both molecules also act as “alarm” proteins exerting paracrine effects on adjacent cells [8]. Novel AKI biomarkers may play important roles clinically [9], but they also have great potential to transform clinical trials [10, 11]. As such, it is important to understand how these markers perform in preclinical models of AKI. Sepsis is the most common cause of AKI in critically ill patients [12, 13], and cecal ligation and puncture (CLP) in small animals is a commonly used preclinical model.
Thus, we sought to evaluate the performance of [TIMP-2]·[IGFBP7] in an rat model of sepsis. In order to be consistent with the human trials that were used to discover and validate these biomarkers [2, 3], we used moderate-to-severe AKI (equivalent to KDIGO stages 2–3 or RIFLE I-F) as the primary outcome. We assessed biomarker performance at various time points, but we used the immediate post-resuscitation time point as primary because it most closely matches the time when patients were enrolled in these trials.
Methods
For this analysis, we used banked samples from 60 animals used in a prior laboratory experiment involving rats subject to cecal ligation and puncture and randomized to resuscitation with two different crystalloids: 0.9 % saline and plasmalyte. Complete details of the parent study have been published [14]. Briefly, 24- to 28-week-old (weight 400–600 g) male, Sprague-Dawley rats were anesthetized with intraperitoneal injection of pentobarbital sodium (50 mg/kg) and subjected to CLP with a predetermined 25 % ligated length of cecum and 18-gauge needle: two punctures inferior to the ileocecal valve. Eighteen hours after CLP animals were re-anesthetized, vascular cannula were placed and animals received 10 ml/kg fluid resuscitation in the first hour with either 0.9 % saline or plasmalyte. For the next 3 h, animals received the same fluid at 5 ml/kg/h. Animals were observed for survival over an additional 24 h. Blood (1 ml) was drawn from the arterial line, and urine (1–2 ml) was taken from the bladder at 0 (baseline), 18 (before fluid resuscitation), 22 (end of fluid resuscitation), and 24 h after fluid resuscitation (46 h after CLP). Isolated plasma and urine was kept at −80 °C for subsequent neutrophil gelatinase-associated lipocalin (NGAL), cystatin C, and creatinine (Cr) measurements and the remainder stored.
Plasma NGAL and urine NGAL were determined using ELISA (BioPorto Diagnostics, Gentofte, Denmark). Plasma creatinine was detected with a creatinine enzymatic assay kit (BioVision Technologies, Mountain View, CA). Plasma cystatin C and urine cystatin C were measured by ELISA (BioVendor LLC, Candler, NC). Frozen urine samples were used for measurement of TIMP-2 and IGFBP7 by ELISA. The ELISA for TIMP-2 was made using capture and detect antibodies from R&D Systems (Minneapolis, MN) and the ELISA for IGFBP7 using capture and detect antibodies from Thermo Fisher Scientific (Waltham, MA) and R&D Systems, respectively. TIMP-2 and IGFBP7 protein from Abcam (Cambridge, UK) and U-Protein Express (Utrecht, Netherlands), respectively, were used for calibration. The calibration range for both assays was 0.0156 to 2 μg/mL.
We determined the severity of AKI using the serum creatinine portion of the RIFLE criteria [15], which classified risk (R), injury (I), and failure (F), on the basis of maximum creatinine increase of 150, 200, and 300 %, respectively, in the 2 days following CLP. For the primary analysis, we compared I and F to R and no AKI. Biomarker data are expressed as means ± standard error (SE). Student’s t tests were applied to compare means. Biomarker concentrations were compared across the first three time points using repeated measures ANOVA with Huynh-Feldt correction. The fourth time point was not included because only 19 rats had both TIMP-2 and IGFBP7 results for all four time points. Dunnett’s test was used for pairwise comparisons with the baseline time point as the control. We calculated area under the receiver operator characteristic curve (AUC) and 95 % confidence intervals [16]. Analyse-it (Analyse-it Software, Ltd., UK) and XLSTAT (Addinsoft, Paris, France) software were used for statistical analysis. A two-sided P < 0.05 was considered statistically significant.
Results
TIMP-2, IGFBP7, and AKI
Samples were available at 18 and 22 h (right before and after fluid resuscitation) from 48 animals. Of these, 30 developed RIFLE I/F (18 I and 12 F) and 18 either had no AKI (8) or R (10). For animals developing AKI, creatinine peaked most often, at the 48-h time point. Immediately after fluid resuscitation, 22 h after CLP, urine concentrations of both TIMP-2 and IGFBP7 were greater in animals who ultimately manifested RIFLE I/F compared to those who did not (Fig. 1). The AUC for [TIMP-2]·[IGFBP7] for AKI was 0.89 (95 % CI 0.80–0.98). Interestingly, the AUCs for individual markers were significantly (p < 0.05) lower than the composite (0.76 and 0.72 for TIMP-2 and IGFBP7, respectively). There were no significant differences between the performance of TIMP-2 and IGFBP7 in animals receiving saline or plasmalyte. Mean [TIMP-2]·[IGFBP7] at 18 and 22 h were similar for animals receiving plasmaltye compared to saline (at 18 h 0.034 (95 % CI 0.023–0.046) vs. 0.028 (μg/ml)2 (95 % CI 0.017–0.039), p = 0.43 or at 22 h 0.034 (95 % CI 0.025–0.042) vs. 0.029 (μg/ml)2 (95 % CI 0.022–0.037), p = 0.43). However, fewer animals developed the endpoint in the plasmalyte group as reported previously [14]. At baseline, [TIMP-2]·[IGFBP7] results were not different between those animals who ultimately developed AKI compared to those who did not (Fig. 2). Both TIMP-2 and IGFBP7 increased 18 h after CLP compared to baseline (p = 0.01 and p < 0.0001, respectively). However, neither [TIMP-2]·[IGFBP7] (Fig. 2) nor individual markers (data not shown) discriminated well for AKI at the 18-h (pre-resuscitation) time point.
Fig. 1.
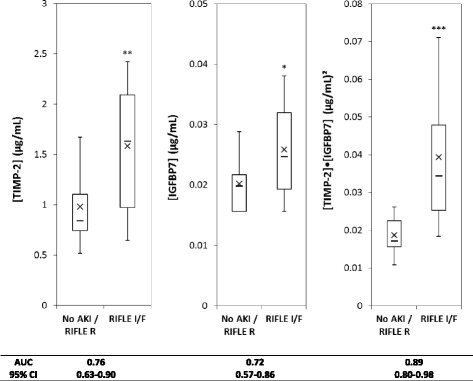
Urinary [TIMP-2], [IGFPB7], or [TIMP-2]·[IGFPB7] levels from animals with no AKI (or only RIFLE R) (n = 18) compared to RIFLE I or F (n = 30). Box and whiskers show interquartile range and 5th to 95th percentiles, respectively. Horizontal dash shows the median, and X shows the mean. *P = 0.01, **P = 0.002, ***P < 0.001
Fig. 2.
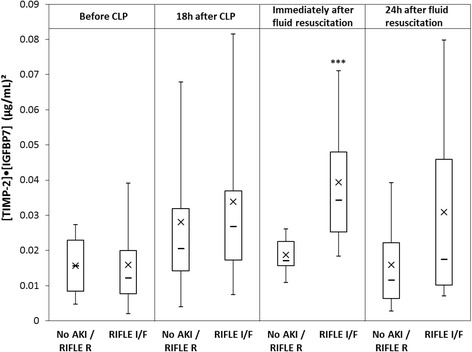
Box-and-whisker plots for [TIMP-2]·[IGFPB7] at various time points comparing no AKI or RIFLE R versus RIFLE I or F. ***p < 0.001 for immediately after fluid resuscitation
Comparison with other urine biomarkers
Performances for various AKI biomarkers are shown in Table 1. The same time point (immediately after resuscitation) and same outcome, RIFLE I/F, were used for all comparisons. The AUC for [TIMP-2]·[IGFBP7] was significantly greater than for urine NGAL (0.89 vs. 0.71, P < 0.05) or plasma NGAL (0.89 vs. 0.62, P < 0.05; Table 1).
Table 1.
Comparison of biomarkers for predicting RIFLE I/F
| Biomarker | No AKI | AKI | p value | AUC |
|---|---|---|---|---|
| [TIMP-2]·[IGFBP7] (μg2/mL2) | 0.019 ± 0.001 | 0.039 ± 0.003 | <0.0001 | 0.89 (0.80–0.98) |
| Urine NGAL (IU/mL) | 2157.6 ± 102.4 | 2472.8 ± 123 | 0.04 | 0.71 (0.63–0.80) |
| Plasma NGAL (IU/mL) | 2143.3 ± 29.6 | 2077 ± 44.5 | 0.21 | 0.62 (0.46–0.79) |
| Urine cystatin C (IU/mL) | 1609.8 ± 284.6 | 2572.8 ± 353.6 | 0.03 | 0.75 (0.56–0.93) |
| Plasma cystatin C (IU/mL) | 1027.3 ± 185.8 | 2344.9 ± 462.5 | <0.01 | 0.78 (0.65–0.90) |
All comparisons are for the post-resuscitation (primary) time point. Shown are means ± standard error and areas under the receiver operating characteristic curves (AUC) with 95 % confidence intervals. P values are for two-sided t test
Mortality
Early mortality (prior to day 2 after CLP) was observed in 19 animals. All deaths exhibited AKI. Immediately after fluid resuscitation, 22 h after CLP, urine concentrations of IGFBP7 (P = 0.002) but not TIMP-2 (P = 0.48) were greater in animals who died prior to day 2 compared to those who did not (Fig. 3). The AUC for [IGFBP7] alone was 0.76 (95 % CI 0.63–0.90) whereas the AUC for [TIMP-2]·[IGFBP7] for AKI was 0.69 (95 % CI 0.53–0.85).
Fig. 3.
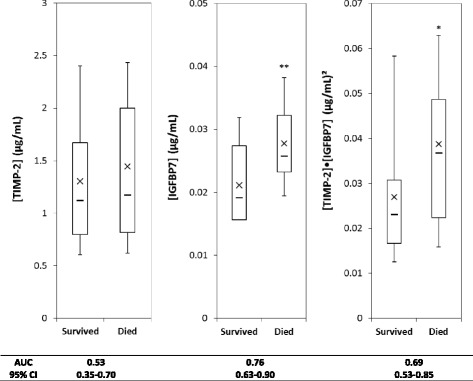
Urinary [TIMP-2], [IGFPB7], or [TIMP-2]·[IGFPB7] levels from animals that survived (n = 29) compared to those that died (n = 19). Box and whiskers show interquartile range and 5th to 95th percentiles, respectively. Horizontal dash shows the median, and X shows the mean. *P = 0.03, **P = 0.002
Discussion
Prior animal studies have examined TIMP-2 in relation to AKI [17, 18], and several studies have examined IGF binding proteins in renal disease [19] but none have directly determined the performance of [TIMP-2]·[IGFBP7] for the prediction of RIFLE I/F AKI in an experimental model. Thus, to our knowledge, this is the first cross-species validation of [TIMP-2]·[IGFBP7] for AKI and establishes the test as a viable tool in the preclinical space. This is important because clinical trials that use [TIMP-2]·[IGFBP7] for enrichment will benefit from preclinical data that closely matches the trial design. For this reason, we designed this laboratory investigation to simulate the clinical situation as much as possible. We used moderate-to-severe AKI (RIFLE I/F = KDIGO 2/3) as the endpoint, and we tested biomarkers at a time that closely mimics enrolment in clinical trials as well as clinical use in general.
There were several unexpected results of our investigation. First, earlier measurement of [TIMP-2]·[IGFBP7] (at 18 h after CLP and prior to fluids), while demonstrating an increase compared to baseline, was not predictive of RIFLE I/F AKI. We speculate that early increases in TIMP-2 and IGFBP7 might have been protective for some animals while sustained elevations were consistently associated with development of AKI. This result may help explain recent findings in humans where early release of TIMP-2 and IGFBP7 was associated with the protection from AKI in the setting of remote ischemic preconditioning and subsequent cardiac surgery [11]. The mechanisms responsible for this effect are still unclear, but we have proposed that limb ischemia releases damage-associated molecular patterns that signal the kidney to release TIMP-2 and IGFBP7 as part of an “alarm” that protects cells from subsequent injury [20]. Since temporary cell cycle arrest is a protective mechanism, it is reasonable to expect that under certain circumstances the mechanism works and release of TIMP-2 and IGFBP7 is not followed by AKI [9]. We speculate that pre-resuscitation levels may identify “renal stress” but not necessarily predict the effectiveness of the resuscitation. Whereas post-resuscitation levels may be more predictive of the pathologic (as opposed to adaptive) state. Alternatively, animals at pre-resuscitation may in fact already have renal injury but it may still be reversible. For animals that responded to resuscitation, they rapidly resolved this injury and no longer exhibited biomarker signatures nor did they manifest clinical AKI. Further study will be necessary to test these hypotheses. However, the finding does have implications for clinical trials and clinical care. For example, the test may have less utility in the pre-hospital arena. Second, it may point to a need to retest patients if clinical evaluation suggests that they were not resuscitated on initial testing.
Another unexpected finding was the wide separation between the AUCs for TIMP-2 and IGFBP7 compared to [TIMP-2]·[IGFBP7] for AKI. These differences were much greater than what was observed in humans [2]. Interestingly, in the clinical study by Kashani et al., TIMP-2 had a superior AUC compared to IGFBP7 in patients with sepsis, whereas the opposite was seen in surgical patients [2]. We observed better performance for TIMP-2 in this experimental model of sepsis (Fig. 1). These findings suggest that sepsis-induced AKI may have a unique underlying pathobiology.
Finally, we observed that while TIMP-2 was a better performing marker for AKI, it was a very poor predictor of mortality and IGFBP7 was better for this outcome (AUC 0.76 vs. 0.53); though not quite significant (p = 0.06) (Fig. 3). This uncoupling of predictors of AKI and mortality was unexpected and may warrant further investigation.
Our study also showed that urine [TIMP-2]·[IGFBP7] was superior to NGAL. NGAL derivation and validation studies were primarily performed in ischemic or nephrotoxic AKI, while investigations of NGAL in septic AKI have demonstrated variable results [21]. NGAL is known to be released by activated neutrophils and appears to be elevated in sepsis, which may complicate its diagnostic value for AKI in patients with sepsis. Our study also used RIFLE I/F AKI criteria (creatinine only) as the primary endpoint so as to more closely model the clinical scenario in humans. Of note, we have previously shown that in antibiotic-treated animals using this exact model, 1-week mortality for RIFLE-F was 36.4 % [22]. This is remarkably similar to 40.3 % crude hospital mortality reported for critically ill patients with KDIGO stage 3 AKI (using creatinine alone) [23] or the 32.4 % covariate-adjusted hospital mortality for KDIGO stage 3 AKI (using both creatinine and urine output) [13].
Our study has important limitations. As a secondary analysis, we were limited in what time points were available. It would have been useful, for example, to have measurements every 1–2 h. However, it is unlikely that we could have obtained this frequency of monitoring in our rats even if we would have tried. Secondly, we chose a relatively high severity model with substantial early mortality (40 % by day 2). It is not known whether a less severe model would have resulted in similar or different results. Finally, our model involved fluid resuscitation with saline in half of the animals, and indeed, the majority of animals reaching the AKI endpoint received saline. Therefore, the exposure is “sepsis plus saline” rather than sepsis alone. However, this mirrors the clinical reality in much of the world especially North America where sepsis patients are invariably resuscitated with saline [24].
Conclusions
In conclusion, we have validated the [TIMP-2]·[IGFBP7] test in an experimental model of sepsis-associated AKI using CLP. Our results establish the test in the preclinical space.
Financial support
This work was funded in part by Astute Medical. The content is solely the responsibility of the authors.
Footnotes
Competing interests
ZYP and FZ report no related interests. JAK has received consulting fees and grant support from Astute Medical and has licensed unrelated technologies through the University of Pittsburgh to Astute Medical.
Authors’ contributions
JAK and ZYP designed the study. FZ and ZYP performed the experiments, and ZYP performed the analysis. JAK and ZYP interpreted the data, and JAK drafted the manuscript. All authors participated in revising the manuscript. All authors read and approved the final manuscript.
References
- 1.KDIGO AKIWG Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline for acute kidney injury. Kidney Inter. 2012;2(Suppl 2012):1–138. [Google Scholar]
- 2.Kashani K, Al-Khafaji A, Ardiles T, et al. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care. 2013;17:R25. doi: 10.1186/cc12503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bihorac A, Chawla LS, Shaw AD, et al. Validation of cell-cycle arrest biomarkers for acute kidney injury using clinical adjudication. Am J Respir Crit Care Med. 2014;189:932–939. doi: 10.1164/rccm.201401-0077OC. [DOI] [PubMed] [Google Scholar]
- 4.Yang Q-H, Liu D-W, Long Y, et al. Acute renal failure during sepsis: potential role of cell cycle regulation. J Infect. 2009;58:459–464. doi: 10.1016/j.jinf.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Price PM, Safirstein RL, Megyesi J. The cell cycle and acute kidney injury. Kidney Int. 2009;76:604–613. doi: 10.1038/ki.2009.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boonstra J, Post JA. Molecular events associated with reactive oxygen species and cell cycle progression in mammalian cells. Gene. 2004;337:1–13. doi: 10.1016/j.gene.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 7.Seo D-W, Li H, Qu C-K, et al. Shp-1 mediates the antiproliferative activity of tissue inhibitor of metalloproteinase-2 in human microvascular endothelial cells. J Biol Chem. 2006;281:3711–3721. doi: 10.1074/jbc.M509932200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seo D-W, Li H, Guedez L, et al. TIMP-2 mediated inhibition of angiogenesis: an MMP-independent mechanism. Cell. 2003;114:171–180. doi: 10.1016/S0092-8674(03)00551-8. [DOI] [PubMed] [Google Scholar]
- 9.Kellum JA, Chawla LS. Cell-cycle arrest and acute kidney injury: the light and the dark sides. Nephrol Dial Transplant. 2015;31:16–22. doi: 10.1093/ndt/gfv130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kellum JA, Devarajan P. What can we expect from biomarkers for acute kidney injury? Biomark Med. 2014;8:1239–1245. doi: 10.2217/bmm.14.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zarbock A, Schmidt C, Van Aken H, et al. Effect of remote ischemic preconditioning on kidney injury among high-risk patients undergoing cardiac surgery: a randomized clinical trial. JAMA. 2015;313:2133–2141. doi: 10.1001/jama.2015.4189. [DOI] [PubMed] [Google Scholar]
- 12.Uchino S, Kellum JA, Bellomo R, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–818. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- 13.Hoste EAJ, Bagshaw SM, Bellomo R, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41:1411–1423. doi: 10.1007/s00134-015-3934-7. [DOI] [PubMed] [Google Scholar]
- 14.Zhou F, Peng Z-Y, Bishop JV, et al. Effects of fluid resuscitation with 0.9% saline versus a balanced electrolyte solution on acute kidney injury in a rat model of sepsis*. Crit Care Med. 2013;42:e270–e278. doi: 10.1097/CCM.0000000000000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bellomo R, Ronco C, Kellum JA, et al. Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–R212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. doi: 10.2307/2531595. [DOI] [PubMed] [Google Scholar]
- 17.Yang Y-L, Liu DD, Hsieh N-K, Chen HI. Endothelin and gelatinases in renal changes following blockade of nitric oxide synthase in hypertensive rats. Chin J Physiol. 2008;51:186–195. [PubMed] [Google Scholar]
- 18.Douthwaite JA, Johnson TS, Haylor JL, et al. Effects of transforming growth factor-beta1 on renal extracellular matrix components and their regulating proteins. J Am Soc Nephrol. 1999;10:2109–2119. doi: 10.1681/ASN.V10102109. [DOI] [PubMed] [Google Scholar]
- 19.Bach LA, Hale LJ. Insulin-like growth factors and kidney disease. Am J Kidney Dis. 2015;65:327–336. doi: 10.1053/j.ajkd.2014.05.024. [DOI] [PubMed] [Google Scholar]
- 20.Zarbock A, Kellum JA. Remote ischemic preconditioning and protection of the kidney—a novel therapeutic option. Crit Care Med. 2015;44:607–16. doi: 10.1097/CCM.0000000000001381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Basu RK, Standage SW, Cvijanovich NZ, et al. Identification of candidate serum biomarkers for severe septic shock-associated kidney injury via microarray. Crit Care. 2011;15:R273. doi: 10.1186/cc10554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peng Z-Y, Wang H-Z, Srisawat N, et al. Bactericidal antibiotics temporarily increase inflammation and worsen acute kidney injury in experimental sepsis*. Crit Care Med. 2012;40:538–543. doi: 10.1097/CCM.0b013e31822f0d2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kellum JA, Sileanu FE, Murugan R, et al. Classifying AKI by urine output versus serum creatinine level. J Am Soc Nephrol. 2015;26:2231–2238. doi: 10.1681/ASN.2014070724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kellum JA, Chawla LS, Keener C, et al. The effects of alternative resuscitation strategies on acute kidney injury in patients with septic shock. Am J Respir Crit Care Med. 2016;193:281–287. doi: 10.1164/rccm.201505-0995OC. [DOI] [PMC free article] [PubMed] [Google Scholar]


