Abstract
Background:
The prevalence of comorbid knee pathology has been examined for sports-related anterior cruciate ligament (ACL) injuries, but it has not been examined in ice hockey players.
Purpose:
To compare concomitant bone bruising, collateral ligament injuries, and intra-articular injuries in ACL injuries suffered during ice hockey versus other sports.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A total of 20 patients with ACL injuries sustained during ice hockey were identified from a prospective registry, of which 95% were male and 90% had a contact mechanism of injury (MOI). Thirteen cases and 46 controls who sustained ACL injuries from ice hockey and other sports, respectively, were included. Inclusion criteria for cases and controls were male sex, contact MOI, no prior knee surgery, magnetic resonance imaging (MRI) within 6 weeks of injury, and surgery within 3 months of injury. Age, body mass index (BMI), MRI findings (bone bruising, medial and lateral collateral ligament [MCL, LCL] injuries), and arthroscopic findings (meniscus tears, chondral injuries) were compared for cases versus controls using t tests or exact chi-square tests.
Results:
Age (22.9 ± 8.8 vs 23.4 ± 10.4 years, P = .88) and BMI ≥25 kg/m2 (50% vs 65.9%, P = .66) did not differ between cases and controls. Cases had less lateral bone bruising (lateral femoral condyle: 54.6% vs 93%, P = .01; lateral tibial plateau: 72.7% vs 93%, P = .09) and no medial bone bruising (medial femoral condyle: 0% vs 7%, P = .06; medial tibial plateau: 0% vs 32.6%, P = .05) compared with controls. Cases had less frequent lateral meniscus tears than controls (23.1% vs 58.5%, P = .05). There were no significant differences in MCL (40% vs 31.2%, P = .77), LCL (0% vs 3.9%, P > .999), medial meniscus tears (7.7% vs 37%, P = .08), and chondral injuries (10% vs 9.4%, P > .999) for cases versus controls.
Conclusion:
Male ice hockey players with ACL injuries had less lateral femoral condyle and medial tibial plateau bone bruising compared with other sports injuries. They also had fewer lateral meniscus tears, and there was a trend toward fewer medial meniscus tears. These differences may reflect different MOIs, or the ability to dissipate energy, for contact ACL injuries that occur during ice hockey versus other sports.
Keywords: anterior cruciate ligament, ice hockey, sport, bone bruise, collateral ligament, intra-articular
Ice hockey is a high-speed, high-impact sport that is associated with increased risk of concussions, shoulder, ankle, and knee injuries, often resulting from contact with other players (eg, collisions) or objects (eg, boards, goal post).1,15,20,25 Knee injuries in hockey players primarily involve the medial collateral ligament (MCL), meniscus, and less commonly, the anterior cruciate ligament (ACL).24,25 Soligard et al20 and Tuominen et al25 reported the prevalence of ACL injuries to be 11.4% in female ice hockey players, and 16% of unspecified ligament sprains/ruptures at the Sochi 2014 Olympic Winter Games occurred during ice hockey. ACL injuries are more common in other types of sports, and soccer has one of the highest ACL injury rates (0.06 to 1.0 injuries per 1000 game hours).2,5,8,19 Basketball, football, and volleyball also frequently cause ACL tears, typically resulting from noncontact mechanisms.3,19
Comorbid knee pathology has been examined for various sports, except for ice hockey.12,21,23 Basketball players with ACL ruptures have increased odds of concomitant lateral meniscus tears and cartilage damage compared with soccer and football players.12,23 A study of National Football League (NFL) players by Bradley et al4 found that of 209 ACL injuries, approximately half were isolated ACL tears, while 22.5% had concomitant meniscal pathology and 23.9% had other ligament or cartilage damage. Granan et al12 found that skiers had slightly greater odds of an isolated ACL tear than soccer players but were almost twice as likely to have associated posterior cruciate ligament (PCL) tears, MCL tears, or multiligament injuries. Also, bone bruising was observed on magnetic resonance imaging (MRI) in a case series of recreational skiers and was most commonly found in the lateral aspect of the knee.21
To date, no studies have documented collateral ligament injuries, bone bruising on MRI, and intra-articular findings after ACL ruptures in ice hockey and compared them with other sports. We hypothesized that there would be differences in comorbid knee pathology for ACL-ruptured ice hockey players versus other sports players.
Methods
Sample Selection
Patients were selected from a prospective registry of 937 ACL reconstructions performed between January 2005 and June 2015 at a single institution. This study was approved by an institutional review board. There were 20 patients who suffered an ACL tear during ice hockey, of which 19 were male and 18 had a contact mechanism of injury. Of these, 13 cases met the following inclusion criteria and were included in this study: (1) male sex, (2) no previous surgery on the injured knee, (3) MRI within 6 weeks of injury, (4) surgery within 3 months of injury, and (5) had a contact mechanism of injury, defined as the injured knee being struck by another player or hitting the boards, goalposts, or other equipment. Forty-six males who sustained an ACL injury during other sports met the inclusion criteria and were included in the control group.
Data Collection
The patient’s surgeon documented demographics, injury characteristics, and MRI findings preoperatively as well as arthroscopic findings immediately after surgery on standard data collection forms. Preoperative data included sex (male/female), date of injury, age at injury, body mass index (BMI), injured side (right/left), history of knee surgery (yes/no), mechanism of injury (contact/noncontact), and sport played during injury. BMI was categorized as normal (≤24.99 kg/m2), overweight (25-29.99 kg/m2), and obese (≥30 kg/m2).26 Sports-related injuries were divided into 2 groups: ice hockey (N = 13) and all other sports (N = 46), which included football (43.5%), soccer (15.2%), basketball (13%), skiing (6.5%), martial arts (6.5%), volleyball (2.2%), lacrosse (2.2%), wrestling (2.2%), rugby (2.2%), floor hockey (2.2%), sparring (2.2%), and baseball (2.2%). MRIs were performed within 6 weeks of injury at various locations and were read by the study surgeons. The presence of bone bruising on sagittal and coronal MRI images was documented for each of the following anatomic sites: lateral tibial plateau (LTP), medial tibial plateau (MTP), lateral femoral condyle (LFC), and medial femoral condyle (MFC). Medial and lateral collateral ligament injuries (MCL and LCL, respectively) seen on MRI were also documented. The presence and location of meniscal and chondral injuries observed during arthroscopy were also documented.
Statistical Analysis
Descriptive statistics were calculated for age, BMI, injured side, MRI findings, and arthroscopic findings stratified by ACL injuries that occurred during ice hockey versus other sports. Group comparisons were done using t tests for continuous data and exact chi-square tests for categorical data. Data are presented as mean ± standard deviation or n (%). Statistical significance was defined as P < .05, and all statistical analyses were performed using SAS 9.4 (SAS Institute Inc).
Results
There were no statistically significant differences in mean age at injury (22.9 ± 8.8 vs 23.4 ± 10.4 years, P = .88) or the ratio of right- to left-sided injuries (9:4 vs 25:19, P = .53) for ice hockey– versus other sports-related injuries. The prevalence of normal weight (6 [50%] vs 15 [34.1%]), overweight (5 [41.7%] vs 23 [52.3%]), and obese (1 [8.3%] vs 6 [13.6%]) athletes also did not differ significantly for injuries related to ice hockey versus other sports (P = .66).
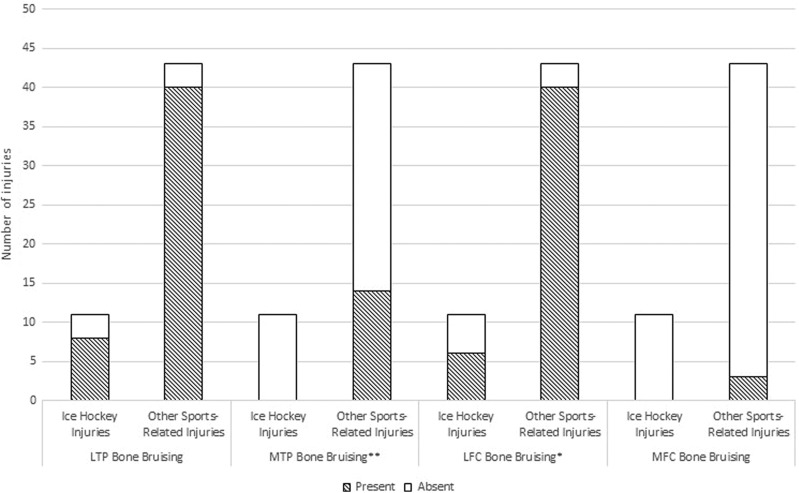
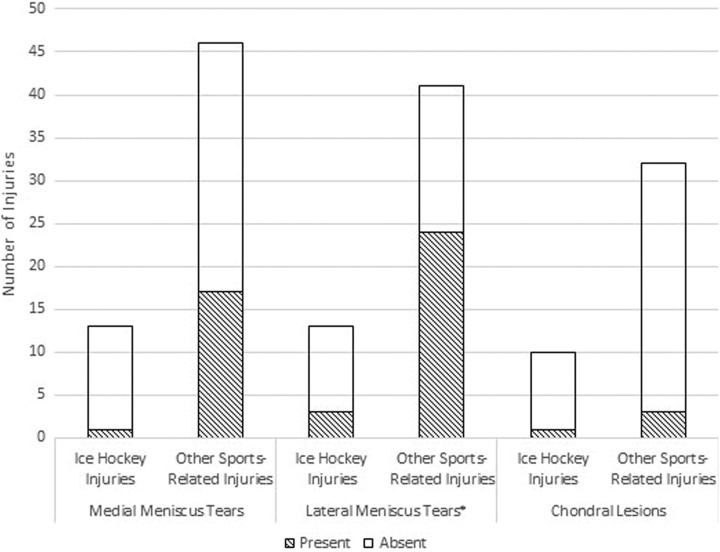
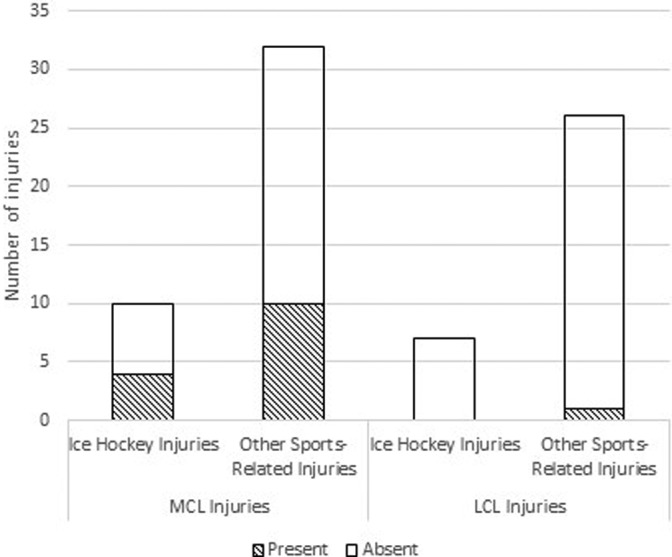
As shown in Figure 1, there was significantly less bone bruising on the LFC for injuries related to ice hockey versus other sports (6 [54.6%] vs 40 [93%], P = .01). The prevalence of MTP bruising was also decreased for injuries in ice hockey versus other sports and was borderline statistically significant (0 [0%] vs 14 [32.6%], P = .05). The prevalence of bone bruising on the LTP (8 [72.7%] vs 40 [93%], P = .09) and MFC (0 [0%] vs 3 [7%], P = .60) did not differ significantly for injuries in ice hockey versus other sports. As shown in Figure 2, there was no significant difference in the prevalence of MCL (4 [40%] vs 10 [31.2%], P = .77) and LCL (0 [0%] vs 1 [3.9%], P > .999) injuries for ice hockey versus other sports. Lateral meniscus tears were less frequent in ice hockey players, which was borderline statistically significant (3 [23.1%] vs 24 [58.5%], P = .05). There were no statistically significant differences in the prevalence of medial meniscus tears (1 [7.7%] vs 17 [37%], P = .08) and chondral injuries (1 [10%] vs 3 [9.4%], P > .999) at the time of arthroscopy for ice hockey versus other sports (Figure 3).
Figure 1.
The presence of bone bruising in anterior cruciate ligament–ruptured ice hockey versus other sports players. *There was significantly less LFC bruising for injuries related to ice hockey versus other sports (P = .01). **There was less MTP bruising for injuries related to ice hockey versus other sports, which was borderline statistically significant (P = .05). There were no statistically significant differences in the presence of LTP (P = .09) or MFC (P = .60) bruising for ice hockey versus other sports. LFC, lateral femoral condyle; LTP, lateral tibial plateau; MFC, medial femoral condyle; MTP, medial tibial plateau.
Figure 2.
The presence of medial collateral ligament (MCL) and lateral collateral ligament (LCL) injuries in anterior cruciate ligament–ruptured ice hockey versus other sports players. There were no statistically significant differences in the presence of MCL (P = .77) and LCL (P > .999) injuries for injuries related to ice hockey versus other sports.
Figure 3.
Presence of meniscal tears and chondral lesions in anterior cruciate ligament–ruptured ice hockey versus other sports players. *There were less lateral meniscal tears for injuries related to ice hockey versus other sports, which was borderline statistically significant (P = .05). There were no statistically significant differences in the presence of medial meniscus tears and chondral lesions for injuries related to ice hockey versus other sports.
Discussion
While several studies have investigated the frequency and pattern of comorbid injuries in sports players with acute ACL ruptures, no such studies have been conducted for ice hockey players.4,9,11,12,21,23 Ice hockey and other sports players with contact ACL injuries were included in this study because this is the most common mechanism of injury in ice hockey players.15 Because of the decreased contact with the playing surface and the decreased friction of the ice surface, there is the potential for a difference in injury mechanism or ability to attenuate the energy of injury to the knee of a hockey player.15 We hypothesized that there would be differences in concomitant knee injuries in ACL-ruptured ice hockey players compared with other sports players, and this hypothesis was supported by our findings. We found that ice hockey players had less concomitant bone bruising on the LFC compared with other sports players. There was also less MTP bruising and lateral meniscus tearing in ice hockey versus other sports players; however, these associations were borderline statistically significant.
The reported prevalence of bone bruising in ACL-ruptured patients is approximately 80% and is observed primarily on the LFC and LTP.16 Speer et al21 evaluated patterns of bone bruising on MRI in 42 recreational Alpine skiers who sustained an acute and complete ACL rupture and found that bone bruising primarily occurred on the LTP (81%) and LFC (40%). However, this study did not include a comparison group. In the current study, lateral bone bruising was more prevalent than medial bone bruising for both ice hockey and other sports players. Both LFC and LTP bone bruising were reduced in ice hockey compared with other sports; however, this difference was only statistically significant for LFC bone bruising. Ice hockey players did not have any medial bone bruising, which could suggest a different mechanism of injury in this subgroup that involves more force to the lateral side of the knee. Contact ACL injuries usually result from sudden deceleration or change in direction, hyperextension, or a shearing mechanism resulting from collision while varus or valgus stress is applied to the knee.6 Furthermore, ice hockey players maintain more of an edge for skating and have their leg in external rotation and their knee in valgus for more time during the sport.15
MCL injuries are the most common ligament injuries in ice hockey players and result from collisions that involve a valgus stress to the knee or when a player catches the edge of their skate on the ice and incurs a twisting force.14 We found that ice hockey players with ACL ruptures had slightly more MCL injuries than other sports players; however, there were no statistically significant differences between these groups. Several other studies have examined comorbid MCL and ACL injuries in other sports.11,12,23 Friden et al11 examined 59 patients with ACL ruptures resulting from contact sports, mainly soccer and handball, of which 39% had a comorbid MCL tear. Using data from 2 large registries of ACL reconstructions in Norway (The Norwegian Knee Ligament Registry) and the United States (Kaiser Permanente ACLR Registry), Granan et al12 found that skiers and American football players were more likely to have MCL injuries while team handball players were less likely to have MCL injuries than soccer players. Tan et al23 found that among college students, MCL injuries were less likely to occur during badminton compared with soccer in patients undergoing ACL reconstruction. On the other hand, LCL injuries are rare in ice hockey players because most contact injuries occur when the knee is in valgus rather than varus.15 Our results are consistent with this theory, as none of the ice hockey players had LCL injuries and the prevalence was low in other sports players (4%). Two studies examined multiligament injuries in sports players, defined as an ACL injury plus a PCL, MCL, and/or LCL injury, but did not report the prevalence of combined ACL and LCL injuries, which was likely low.12,23
Our study found that ice hockey players had a trend toward fewer medial and lateral meniscus tears as well as equal amounts of chondral injuries compared with other sports players, with decreased frequency of lateral meniscus tears being borderline statistically significant. Previous studies have examined the associations between comorbid intra-articular and ACL injuries for various sports but not for ice hockey.4,9,11,12,23 In ACL-injured players of the National Football League (NFL), comorbid meniscal pathology and other ligamentous or chondral pathology was observed in 22.5% and 23.9%, respectively.4 Among 59 contact ACL sport injuries, mainly soccer and handball athletes, 8.5% had medial meniscus tears and 39% had lateral meniscus tears.11 Tan et al23 found increased odds of lateral meniscus and chondral injuries for basketball and sprinting versus soccer injuries.23 Granan et al12 found that compared with soccer, lateral meniscus tears occurred more often in basketball and handball players and chondral injuries occurred more often in basketball players. Feucht et al9 did not find an association between lateral meniscus tears and high- or low-impact sports in ACL-injured patients. However, lateral meniscus tears were more prevalent for contact versus noncontact injuries, although nonsports injuries were included in this analysis (P < .001).9 Different variations in patterns of comorbid intra-articular pathology by type of sport may be due to different mechanisms of injury and/or the amount of force at the time of injury. Granan et al also noted that older age might have resulted in more intra-articular injuries in basketball players compared with other sports players because they had longer time to develop these injuries.12
Comorbid knee pathology in ACL-injured sports players can affect patient outcomes and thus should be considered when planning treatment, especially for patients wanting to return to sport. LaPrade et al15 recommended ACL reconstruction when significant instability observed during physical examination or meniscus tears is present. Meniscus tears observed during ACL reconstruction are commonly treated with meniscectomy; however, meniscectomy is associated with increased risk of later degenerative changes.17 The presence of chondral lesions or meniscus tears at the time of ACL reconstruction has been shown to be associated with worse long-term clinical outcome scores.7 Also, a recent study of National Hockey League (NHL) Injury Surveillance System data found that ACL-injured players with comorbid meniscus tears had a shorter career compared with players with isolated ACL injuries and controls.10 Bone bruising in ACL-injured patients has been associated with increased pain, delayed recovery of range of motion, and longer time to unaided ambulation after ACL reconstruction.13,18,22
There are several strengths and limitations of this study. To our knowledge, this is the first study to compare comorbid pathology in ACL-ruptured ice hockey players with other sports players. The principal limitation of this study was the small sample size, which limits the statistical power. A small sample size also did not allow for multivariate analyses or stratification. The results of this study may not be generalizable to female athletes, ACL ruptures that did not occur during sports (eg, motor vehicle accident), noncontact injuries, and to patients undergoing nonoperative management. However, we found that ACL injuries sustained during ice hockey primarily occurred in males and involved a contact mechanism of injury. We were unable to examine the effects of different levels of sports participation (eg, high school, collegiate, professional) in this study. Also, MRIs were obtained from multiple facilities, which could have resulted in random error due to variations in equipment and the skill level of different radiology technicians.
Conclusion
ACL-injured males who sustained ice hockey injuries had less LFC and MTP bone bruising than other sports injuries. There was also a trend toward fewer medial and lateral meniscus tears in ice hockey players. Differences in patterns of comorbid knee pathology for ice hockey versus other sports players may be due to different mechanisms of injury and may reflect different prognoses.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Ralph C. Wilson Jr Foundation.
References
- 1. Agel J, Harvey EJ. A 7-year review of men’s and women’s ice hockey injuries in the NCAA. Can J Surg. 2010;53:319–323. [PMC free article] [PubMed] [Google Scholar]
- 2. Bjordal JM, Arnly F, Hannestad B, Strand T. Epidemiology of anterior cruciate ligament injuries in soccer. Am J Sports Med. 1997;25:341–345. [DOI] [PubMed] [Google Scholar]
- 3. Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573–578. [DOI] [PubMed] [Google Scholar]
- 4. Bradley JP, Klimkiewicz JJ, Rytel MJ, Powell JW. Anterior cruciate ligament injuries in the National Football League: epidemiology and current treatment trends among team physicians. Arthroscopy. 2002;18:502–509. [DOI] [PubMed] [Google Scholar]
- 5. Brophy RH, Stepan JG, Silvers HJ, Mandelbaum BR. Defending puts the anterior cruciate ligament at risk during soccer: a gender-based analysis. Sports Health. 2015;7:244–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Childs SG. Pathogenesis of anterior cruciate ligament injury. Orthop Nurs. 2002;21:35–40. [DOI] [PubMed] [Google Scholar]
- 7. Cox CL, Huston LJ, Dunn WR, et al. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med. 2014;42:1058–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fauno P, Wulff Jakobsen B. Mechanism of anterior cruciate ligament injuries in soccer. Int J Sports Med. 2006;27:75–79. [DOI] [PubMed] [Google Scholar]
- 9. Feucht MJ, Bigdon S, Bode G, et al. Associated tears of the lateral meniscus in anterior cruciate ligament injuries: risk factors for different tear patterns. J Orthop Surg Res. 2015;10:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Flint JH, Wade AM, Giuliani J, Rue JP. Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med. 2014;42:235–241. [DOI] [PubMed] [Google Scholar]
- 11. Friden T, Erlandsson T, Zatterstrom R, Lindstrand A, Moritz U. Compression or distraction of the anterior cruciate injured knee. Variations in injury pattern in contact sports and downhill skiing. Knee Surg Sports Traumatol Arthrosc. 1995;3:144–147. [DOI] [PubMed] [Google Scholar]
- 12. Granan LP, Inacio MC, Maletis GB, Funahashi TT, Engebretsen L. Sport-specific injury pattern recorded during anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:2814–2818. [DOI] [PubMed] [Google Scholar]
- 13. Johnson DL, Bealle DP, Brand JC, Jr, Nyland J, Caborn DN. The effect of a geographic lateral bone bruise on knee inflammation after acute anterior cruciate ligament rupture. Am J Sports Med. 2000;28:152–155. [DOI] [PubMed] [Google Scholar]
- 14. LaPrade RF, Surowiec RK, Sochanska AN, et al. Epidemiology, identification, treatment and return to play of musculoskeletal-based ice hockey injuries. Br J Sports Med. 2014;48:4–10. [DOI] [PubMed] [Google Scholar]
- 15. LaPrade RF, Wijdicks CA, Griffith CJ. Division I intercollegiate ice hockey team coverage. Br J Sports Med. 2009;43:1000–1005. [DOI] [PubMed] [Google Scholar]
- 16. Nakamae A, Engebretsen L, Bahr R, Krosshaug T, Ochi M. Natural history of bone bruises after acute knee injury: clinical outcome and histopathological findings. Knee Surg Sports Traumatol Arthrosc. 2006;14:1252–1258. [DOI] [PubMed] [Google Scholar]
- 17. Noyes FR, Barber-Westin SD. Treatment of meniscus tears during anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:123–130. [DOI] [PubMed] [Google Scholar]
- 18. Quelard B, Sonnery-Cottet B, Zayni R, Ogassawara R, Prost T, Chambat P. Preoperative factors correlating with prolonged range of motion deficit after anterior cruciate ligament reconstruction. Am J Sports Med. 2010;38:2034–2039. [DOI] [PubMed] [Google Scholar]
- 19. Ristić V, Ninković S, Harhaji V, Milankov M. Causes of anterior cruciate ligament injuries. Med Pregl. 2010;63:541–545. [DOI] [PubMed] [Google Scholar]
- 20. Soligard T, Steffen K, Palmer-Green D, et al. Sports injuries and illnesses in the Sochi 2014 Olympic Winter Games. Br J Sports Med. 2015;49:441–447. [DOI] [PubMed] [Google Scholar]
- 21. Speer KP, Warren RF, Wickiewicz TL, Horowitz L, Henderson L. Observations on the injury mechanism of anterior cruciate ligament tears in skiers. Am J Sports Med. 1995;23:77–81. [DOI] [PubMed] [Google Scholar]
- 22. Szkopek K, Warming T, Neergaard K, Jorgensen HL, Christensen HE, Krogsgaard M. Pain and knee function in relation to degree of bone bruise after acute anterior cruciate ligament rupture. Scand J Med Sci Sports. 2012;22:635–642. [DOI] [PubMed] [Google Scholar]
- 23. Tan Y, Zhou P, Ma C. Analysis of sport-injured pattern of anterior cruciate ligament injuries in the reconstruction period of chinese college students [published online ahead of print September 2, 2015]. J Sports Med Phys Fitness. 2015. [PubMed] [Google Scholar]
- 24. Tegner Y, Lorentzon R. Evaluation of knee braces in Swedish ice hockey players. Br J Sports Med. 1991;25:159–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tuominen M, Stuart MJ, Aubry M, Kannus P, Tokola K, Parkkari J. Injuries in women’s international ice hockey: an 8-year study of the World Championship tournaments and Olympic Winter Games [published online July 7, 2015]. Br J Sports Med. doi:10.1136/bjsports-2015-094647. [DOI] [PubMed] [Google Scholar]
- 26. World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Geneva, Switzerland: World Health Organization; 2000. [PubMed] [Google Scholar]