Abstract
Ascorbic acid (A) has been demonstrated to exhibit anti-cancer activity in association with chemotherapeutic agents. Potassium (K) is a regulator of cellular proliferation. In the present study, the biological effects of A and K bicarbonate, alone or in combination (A+K), on breast cancer cell lines were evaluated. The survival of cancer cells was determined by sulforhodamine B cell proliferation assay, while analysis of the cell cycle distribution was conducted via fluorescence-activated cell sorting. In addition, the expression of signaling proteins was analyzed upon treatment. The results indicated that there was a heterogeneous response of the different cell lines to A and K, and the best effects were achieved by A+K and A treatment. The interaction between A+K indicated an additive or synergistic effect. In addition, A+K increased the percentage of cells in the sub-G1 phase of the cell cycle, and was the most effective treatment in activating the degradation of poly(adenosine diphosphate-ribose) polymerase-1. In the breast cancer cell line MCF-7, A+K induced the appearance of the 18 kDa isoform of B-cell lymphoma-2-associated X protein (Bax), which is a more potent inducer of apoptosis than the full-length Bax-p21. The effects of A and K on the phosphorylation of extracellular signal-regulated kinase (ERK)1 and ERK2 were heterogeneous. In addition, treatment with K, A and A+K inhibited the expression of nuclear factor-κB. Overall, the results of the present study indicated that K potentiated the anti-tumoral effects of A in breast cancer cells in vitro.
Keywords: ascorbic acid, potassium, breast cancer, apoptosis
Introduction
The use of ascorbic acid (A) as an anti-cancer agent has been analyzed in the last 50 years (1,2). Previous epidemiological studies have demonstrated that dietary administration of A exerts a preventive effect on multiple tumors (1,2). However, Cameron and Pauling (3) have argued its role as a therapeutic anti-cancer agent, in agreement with previous studies disproving its potential role as an anti-cancer agent (4,5). These studies were performed supplementing the diet with high doses of orally administered vitamin C, which allows to reach saturation at plasma concentrations of 1 g/day, while higher doses of vitamin C are excreted (6,7). Blood concentrations of vitamin C at mM levels are only possible to obtain via intravenous injections of high doses of the compound (8,9). In recent years, the interest on A and its effects on cancer growth has increased (10). A has been recently demonstrated to be highly effective in cancer therapy in association with commonly used chemotherapeutic agents in ovarian tumors (11).
Similarly to the case of A, the role of potassium (K) in cancer has remained unclear since Cone (12) reported in 1971 higher levels of Na+ and lower levels of K+, Ca2+ and Zn in cancer cells, compared with healthy cells. K+ is capable of acting as an anti-apoptotic and as a pro-apoptotic agent (13,14), and is also a regulator of cell proliferation (15–17). The intracellular homeostasis of Na+ and K+ is disregulated in cancer cells (18–20). Altered expression and activity of Na+/K+ adenosine triphosphate (ATP)ase has been observed in cancer cells, which may explain the differences in concentration of Na+ and K+ observed in these cells, compared with normal cells (21,22). Furthermore, K+ is essential to fold and stabilize G-quadruplexes (23). Agents that stabilize or target G-quadruplexes may act as anti-tumor agents (24); thus, physiological concentrations of K+ are likely to be required for normal cell behavior (25,26). K ascorbate has been proposed as an anti-degenerative agent (27). Previous studies reported a strong antioxidant effect of K ascorbate on red blood cell oxidation (28,29). In addition, it has been suggested that K ascorbate may act as a K intracellular carrier and may be able to inhibit the cell cycle in tumor cells (30).
In order to clarify the potential role of K ascorbate as an anti-tumor agent, the effects of A, K and A+K on different breast cancer cell lines were analyzed in the present study.
Materials and methods
Reagents
K bicarbonate and A were obtained from AEIE Biochemical Research (Oviedo, Spain). Sulforhodamine B (SRB) was purchased from Sigma-Aldrich (St. Louis, MO, USA). Rabbit anti-human polyclonal B-cell lymphoma-2 (Bcl-2)-associated X protein (Bax; cat. no. 554104) and mouse anti-human monoclonal Bcl-2 (cat. no. 610538) antibodies were obtained from Transduction Laboratories (BD Biosciences, Franklin Lakes, NJ, USA). Anti-human mouse monoclonal p53 (cat. no. sc-126), rabbit anti-rat polyclonal extracellular signal-regulated kinase (ERK)1/2 (C-14; cat. no. sc-154), mouse anti-human monoclonal phosphorylated (p)-ERK (E-4, which recognizes the phosphorylated and active form of ERK1 and ERK2; cat. no. sc-7383), nuclear factor (NF)-κB p65 (cat. no. sc-8008) and mouse anti-human monoclonal poly(adenosine diphosphate-ribose) polymerase-1 (PARP-1; F-2; cat. no. sc-8007) antibodies were obtained from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA). Rabbit anti-human polyclonal antibody against actin (cat. no. A5060) and peroxidase-conjugated goat anti-mouse polyclonal (cat. no. A2554) or anti-rabbit polyclonal (cat. no. A6154) immunoglobulin (Ig)G were obtained from Sigma-Aldrich.
Cell lines and treatments
Human breast cancer cell lines MDA-MB-231, MDA-MB-453, MDA-MB-468, T47-D and MCF-7 were maintained in Dulbecco's modified Eagle medium - high glucose containing 10% fetal bovine serum, 100 U/ml penicillin and 100 µg/ml streptomycin (complete medium) (all purchased from Aurogene, Rome, Italy). Cells were cultured at 37°C in a humidified incubator with 5% CO2.
For treatments, cells were incubated for the indicated times in the presence of K and A, alone or in combination (A+K), or in the presence of culture medium (CTRL). The stock solutions (150 mM) of K, A and A+K were obtained by diluting K and A, alone or in combination, in distilled water. Thus, K stock solution was obtained by dissolving 300 mg K in 20 ml distilled water; A stock solution was obtained by dissolving 150 mg A in 20 ml distilled water; and A+K stock solution was obtained combining 300 mg K and 150 mg A in 20 ml distilled water. The concentrations used for cell treatment were reached by diluting the stock solutions in complete CTRL.
SRB cell proliferation assay
Cells were seeded in 96-well plates at a density of 5×103 cells/well, and incubated at 37°C to allow cell attachment. Following 24 h, the medium was changed, and the cells were treated with K and A, alone or in combination (A+K), at a dose range of 1.5–15 mM, or with CTRL, and incubated for 24, 48 or 72 h. Subsequently, cells were fixed with cold trichloroacetic acid (final concentration, 10%; Sigma-Aldrich) for 1 h at 4°C. Following 4 washes with distilled water, the plates were air-dried and stained for 30 min with 0.4% (w/v) SRB in 1% acetic acid (Sigma-Aldrich). Following 4 washes with 1% acetic acid to remove the unbound dye, the plates were air-dried, and cell-bound SRB was dissolved with 10 mM unbuffered Tris base solution (100 µl/well; Sigma-Aldrich). The optical density (OD) of the samples was determined at 540 nm using a spectrophotometric plate reader (Wallac 1420 Victor; Perkin Elmer Inc., Waltham, MA, USA). The percentage survival of the cultures treated with the aforementioned compounds was calculated by normalizing their OD values to those of the control cultures (31,32). The experiments were performed in triplicate and repeated three times.
Fluorescence-activated cell sorting (FACS) analysis
Asynchronized, log-phase growing cells (60% confluent, ~1.5×105 cells/well in 6-well plates) were treated with 10 mM K and A, alone or in combination (A+K), or with CTRL. Following 24 h, adherent and suspended cells were harvested, centrifuged (5417R centrifuge; Eppendorf, Hamburg, Germany) at 300 × g for 10 min and washed twice with cold phosphate-buffered saline (PBS). Cell pellets were resuspended in 70% ethanol and incubated for 1 h at −20°C. Cells were then washed twice with cold PBS, centrifuged at 300 × g for 10 min, incubated for 1 h in the dark with propidium iodide (Sigma-Aldrich) at a final concentration of 25 µg/ml in 0.1% citrate (Sigma-Aldrich) and 0.1% Triton X-100 (Sigma-Aldrich), and analyzed by flow cytometry using a FACSCalibur™ cytometer (BD Biosciences) with CellQuest Pro 5.2 software (BD Biosciences) (31,32).
Preparation of cell lysates and western blotting
Cells (~1×106 cells/plate) were seeded into 100-mm tissue culture plates for 24 h prior to the addition of 10 mM K and A, alone or in combination (A+K), or CTRL. MCF-7 and MDA-MB-231 cells were selected for western blotting analysis of signaling pathway proteins as these two cell lines were most sensitive to A+K treatment. Following incubation for 24-h, the MCF-7 and MDA-MB-231 cells were harvested, washed twice with cold PBS and lysed in radioimmunoprecipitation assay lysis buffer [1% Triton X-100, 0.1% sodium dodecyl sulfate (SDS), 200 mM NaCl, 50 mM Tris-HCl pH 7.5, 1 mM phenylmethylsulfonyl fluoride and 1 mM Na3VO4]. Following 30-min incubation at 4°C, the mixtures were centrifuged at 12,000 × g for 15 min, and the supernatants were analyzed by western blotting (33,34). Handcast gels were prepared from acrylamide and bisacrylamide monomer solutions (cat. no. A3574; Sigma-Aldrich). SDS-PAGE and western blot analysis were performed using Mini-PROTEAN Tetra Cell apparatus (Bio-Rad, Milan, Italy) according to the manufacturer's instructions. Electrophoresis (cat. no. 161-0732) and blot transfer (cat. no. 161-0734) buffers were purchased from Bio-Rad. Hyper PAGE prestained markers (cat. no. BIO-33066; Bioline, London, UK) were used. For immunoblotting analysis, 50 µg cell lysates were resolved in 10% SDS-polyacrylamide gel electrophoresis (150 V for 1 h), and then transferred to nitrocellulose membranes (30 V for 90 min; GE Healthcare, Piscataway, NJ, USA) (35). After blocking with 5% skimmed dry milk in PBS overnight at 4°C, the membranes were incubated overnight at 4°C with specific primary antibodies at a concentration of 1–2 µg/ml. Upon washing, the membranes were incubated with peroxidase-conjugated goat anti-mouse or anti-rabbit IgG antibodies diluted in PBS for 1 h at room temperature, and developed by chemiluminescence (LiteABlot Plus; Euroclone, Milan, Italy), as previously described (36–38). Densitometric analysis of the autoradiographic bands was performed using ImageJ 1.42q software (National Institutes of Health, Bethesda, MD, USA) following blot scanning (HP Scanjet 4890 Photo Scanner; Hewlett-Packard, Palo Alto, CA, USA) (39).
Statistical analysis
Data distribution of cell survival and FACS analyses were initially verified by the Kolmogorov-Smirnov test, and data sets were analyzed by one-way analysis of variance, followed by Newman-Keuls test. Differences between the intensity of immunoreactive bands were evaluated by two-tailed Student's t test. P≤0.05 was considered to indicate a statistically significant difference.
Results
Inhibition of breast cancer cell lines survival by K and A, alone or in combination
Survival of breast cancer cell lines (MDA-MB-231, MDA-MB-453, MDA-MB-468, T47-D and MCF-7) was evaluated by SRB assay following exposure to increasing doses (1.5, 5, 10 and 15 mM) of K and A, alone or in combination (A+K), for 24, 48 and 72 h (Table I). The effect of the compounds on cell growth was determined and compared with the growth of cells incubated with CTRL. The effect of A was dose- and time-dependent on all cell lines, with the exception of MDA-MB-231. K significantly inhibited cell growth of MCF-7 cells only at the highest concentration tested following 48-h incubation. The effect obtained with equimolar combinations of A+K was significantly higher than the effect of treatment with the highest concentration tested of A on MCF7 (P<0.01), MDA-MB-231 (P<0.05 at 10 mM for 48 h; P<0.001 at 15 mM for 48 h and 10–15 mM for 72 h) and MDA-MB-453 (P<0.05 at 10–15 mM for 48 h; P<0.01 at 10 mM for 72 h; P<0.001 at 15 mM for 72 h) cells following incubation for 48 or 72 h. The effect obtained with equimolar combinations of A+K was significantly higher than the effect obtained with 10 mM (P<0.01) and 15 mM (P<0.001) A on T47-D cells following incubation for 24 or 72 h, respectively. Conversely, the effects with A+K were not significantly different from those obtained with A in MDA-MB-468 cells. In addition, treatment with A was more effective than treatment with A+K on MDA-MB-468 cells at the lowest concentration tested. Overall, these results indicate that there is a heterogeneous response of the different cell lines toward the treatment with A and/or K, and revealed that the maximum effect was achieved with the combined treatment A+K.
Table I.
Effects of K and A, alone or in combination, on the survival of breast cancer cells.
| 15 mM | 10 mM | 5 mM | 1.5 mM | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cell line | Treatment | Mean % cell growth (±SD) | P-value | Mean % cell growth (±SD) | P-value | Mean % cell growth (±SD) | P-value | Mean % cell growth (±SD) | P-value | |
| MCF-7 | K | 24 h | 90±7 | – | 96±1 | – | 98±4 | – | 100±0 | – |
| K | 48 h | 85±1 | 1a | 91±5 | – | 90±0 | – | 93±2 | – | |
| K | 72 h | 99±2 | – | 100±0 | – | 100±0 | – | 100±0 | – | |
| A | 24 h | 70±5 | 1a | 85±1 | – | 93±9 | – | 96±6 | – | |
| A | 48 h | 55±4 | 1c, 2c | 69±9 | 1b, 2a | 84±6 | – | 92±3 | – | |
| A | 72 h | 30±4 | 1c, 2c | 70±2 | 1c, 2c | 99±2 | – | 100±0 | – | |
| A+K | 24 h | 52±6 | 1c, 2b | 78±3 | 1a | 95±4 | – | 97±5 | – | |
| A+K | 48 h | 37±5 | 1c, 2c, 3b | 64±8 | 1c, 2b | 84±2 | – | 87±1 | – | |
| A+K | 72 h | 25±1 | 1c, 2c | 48±3 | 1c, 2c, 3b | 90±4 | – | 100±1 | – | |
| T47-D | K | 24 h | 95±5 | – | 100±0 | – | 100±1 | – | 99±1 | – |
| K | 48 h | 96±0 | – | 96±6 | – | 98±1 | – | 99±2 | – | |
| K | 72 h | 95±0 | – | 99±2 | – | 100±0 | – | 100±0 | – | |
| A | 24 h | 75±6 | 1b, 2a | 87±1 | – | 90±4 | 1c, 2b | 97±5 | – | |
| A | 48 h | 30±7 | 1c, 2c | 68±7 | 1c, 2c | 92±0 | 100±1 | – | ||
| A | 72 h | 13±0 | 1c, 2c, | 28±4 | 1c, 2c | 87±4 | – | 96±6 | – | |
| A+K | 24 h | 36±4 | 1c, 3c | 77±7 | 1c, 2b | 89±4 | 1c, 2b | 96±3 | – | |
| A+K | 48 h | 25±3 | 1c, 2c | 61±6 | 1c 2c | 83±4 | 1c, 2a | 98±2 | – | |
| A+K | 72 h | 11±1 | 1c, 2c | 15±2 | 1c, 2c, 3b | 98±4 | – | 95±7 | – | |
| MDA-MB-231 | K | 24 h | 93±10 | – | 92±4 | – | 95±5 | – | 95±7 | – |
| K | 48 h | 91±8 | – | 92±8 | – | 93±6 | – | 90±8 | – | |
| K | 72 h | 94±1 | – | 96±6 | – | 99±2 | – | 93±0 | – | |
| A | 24 h | 80±5 | – | 95±6 | – | 97±1 | – | 93±7 | – | |
| A | 48 h | 67±7 | 1c, 2b | 92±6 | – | 96±7 | – | 98±2 | – | |
| A | 72 h | 60±2 | 1c, 2c | 92±6 | – | 94±1 | – | 97±1 | – | |
| A+K | 24 h | 46±10 | 1c, 3c | 76±11 | 1c, 3b, 2a | 93±3 | – | 94±7 | – | |
| A+K | 48 h | 29±8 | 1c, 3c | 73±7 | 1c, 2b, 3a | 92±9 | – | 90±10 | – | |
| A+K | 72 h | 18±8 | 1c, 3c | 59±3 | 1c, 3c | 93±10 | – | 95±7 | – | |
| MDA-MB-453 | K | 24 h | 95±7 | – | 100±1 | – | 100±1 | – | 100±0 | – |
| K | 48 h | 99±2 | – | 100±0 | – | 96±6 | – | 100±0 | – | |
| K | 72 h | 100±0 | – | 100±0 | – | 100±0 | – | 100±0 | – | |
| A | 24 h | 74±4 | 1a | 85±9 | – | 92±7 | – | 96±6 | – | |
| MDA-MB-453 | A | 48 h | 47±4 | 1c, 2c | 56±4 | 1c, 2c | 74±3 | 1a | 90±14 | – |
| A | 72 h | 37±1 | 1c, 2c | 47±9 | 1c, 2c | 74±4 | 1c, 2a | 98±3 | – | |
| A+K | 24 h | 65±5 | 1c, 2a | 72±13 | – | 94±7 | – | 95±7 | – | |
| A+K | 48 h | 39±2 | 1c, 2c, 3a | 46±4 | 1c, 2c, 3a | 68±6 | 1c, 2a | 92±12 | – | |
| A+K | 72 h | 26±1 | 1c, 3c | 33±4 | 1c, 2c, 3b | 67±11 | 1c, 2a | 82±12 | – | |
| MDA-MB-468 | K | 24 h | 100±0 | – | 98±4 | – | 96±5 | – | 100±0 | – |
| K | 48 h | 94±9 | – | 100±0 | – | 100±0 | – | 100±0 | – | |
| K | 72 h | 84±9 | – | 83±7 | – | 82±11 | – | 82±12 | – | |
| A | 24 h | 41±1 | 1c, 2c | 43±6 | 1c, 2b | 56±16 | 1c, 2b | 95±8 | – | |
| A | 48 h | 40±2 | 1c, 2c | 41±0 | 1c, 2c | 39±3 | 1c, 2c | 88±17 | – | |
| A | 72 h | 38±2 | 1c, 2c | 35±3 | 1c, 2b | 35±2 | 1c, 2c | 58±1 | 1c, 2b | |
| A+K | 24 h | 46±8 | 1c, 2c | 53±14 | 1c, 2b | 63±6 | 1c, 2a | 100±0 | – | |
| A+K | 48 h | 43±2 | 1c, 2c | 56±9 | 1c, 2c | 100±0 | – | 100±0 | – | |
| A+K | 72 h | 39±1 | 1c, 2c | 50±10 | 1c, 2b | 100±0 | – | 100±0 | – | |
Dose-response effect of K and A on breast cancer cells. The percentage of cell growth in the presence of A and/or K was calculated in comparison with the growth of cells incubated with CTRL, which was normalized to 100%. The results reported are the mean values of three independent experiments performed in triplicate. The statistical significance of the effects obtained with compounds A and K, alone or in combination, was calculated vs. those obtained with (1) CTRL, (2) K and (3) A
P<0.05
P<0.01
P<0.001. CTRL, culture medium; K, potassium; A, ascorbic acid; SD, standard deviation.
The concentration of compound that inhibits 50% of the cell growth (IC50) was also determined (Table II). The IC50 of A+K was significantly reduced, compared with that of A, in MCF-7 (P<0.05 for 72 h), MDA-MB-231 (P<0.01 for 24 h; P<0.001 for 48 and 72 h) and MDA-MB-453 (P<0.05 for 24 and 48 h) cells. This effect was observed only upon 24-h incubation in T47-D cells (P<0.001). By contrast, a lower IC50 value was observed in MDA-MB-468 cells following treatment with A alone, compared with A+K (P<0.001 for 48 and 72 h).
Table II.
IC50 values of A, alone or in combination with K, in breast cancer cells.
| Cell line | Treatment | IC50 ± SD (mM) | P-value | |
|---|---|---|---|---|
| MCF-7 | A | 24 h | 25.79±1.23 | – |
| A | 48 h | 18.23±1.17 | – | |
| A | 72 h | 12.22±1.01 | – | |
| A+K | 24 h | 15.51±1.04 | – | |
| A+K | 48 h | 12.16±1.09 | – | |
| A+K | 72 h | 9.96±1.02 | <0.050 | |
| MDA-MB-231 | A | 24 h | 22.65±1.23 | – |
| A | 48 h | 18.00±1.07 | – | |
| A | 72 h | 16.25±1.04 | – | |
| A+K | 24 h | 14.37±1.06 | <0.010 | |
| A+K | 48 h | 12.30±1.05 | <0.001 | |
| A+K | 72 h | 10.69±1.04 | <0.001 | |
| MDA-MB-453 | A | 24 h | 36.87±1.55 | – |
| A | 48 h | 12.88±1.12 | – | |
| A | 72 h | 9.91±1.04 | – | |
| A+K | 24 h | 21.28±1.27 | <0.050 | |
| A+K | 48 h | 9.37±1.09 | <0.050 | |
| A+K | 72 h | 6.71±1.12 | – | |
| T47-D | A | 24 h | 47.84±1.44 | – |
| A | 48 h | 12.01±1.03 | – | |
| A | 72 h | 7.99±1.02 | – | |
| A+K | 24 h | 13.14±1.04 | <0.001 | |
| A+K | 48 h | 10.78±1.05 | – | |
| A+K | 72 h | 7.86±1.07 | – | |
| MDA-MB-468 | A | 24 h | 8.40±1.17 | – |
| A | 48 h | 5.47±1.23 | <0.001 | |
| A | 72 h | 2.29±1.38 | <0.001 | |
| A+K | 24 h | 11.09±1.17 | – | |
| A+K | 48 h | 12.39±1.07 | – | |
| A+K | 72 h | 10.79±1.06 | – |
Data are presented as the mean ± SD of three independent experiments performed in triplicate. P-values of the IC50 values obtained following treatment with A+K were calculated in comparison with the IC50 values obtained upon treatment with A alone. IC50, inhibitory concentration that causes 50% cell growth reduction; A, ascorbic acid; K, potassium; SD, standard deviation.
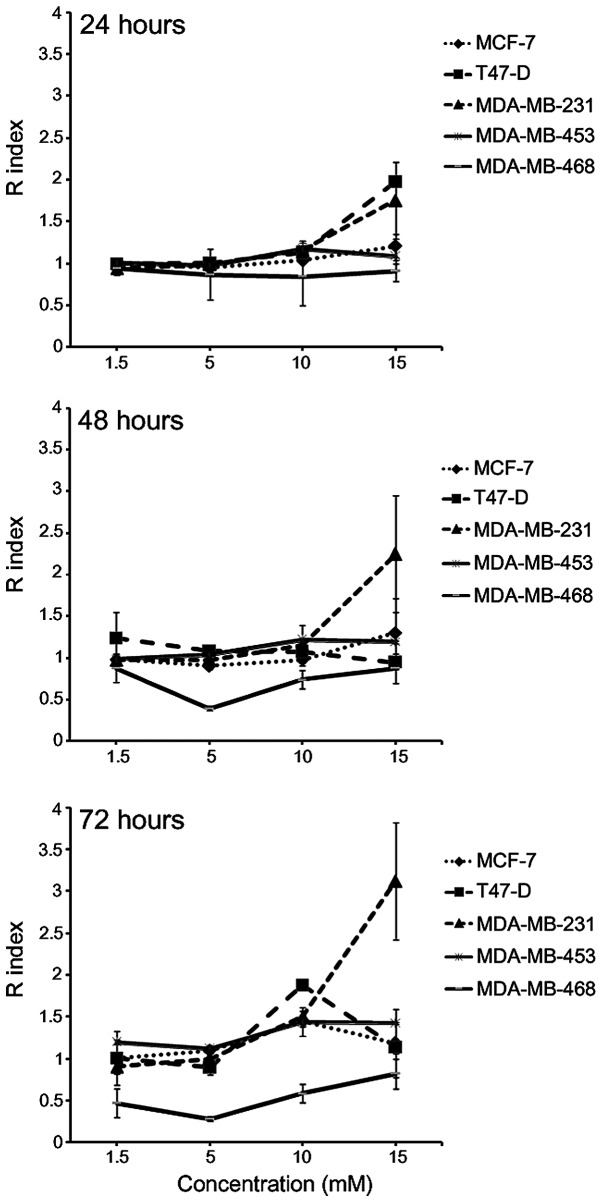
The model of interaction between A and K when used in combination was determined using the Kern's method (40) (Fig. 1). The results indicated that the interaction between A+K was lower than the additive effect in MDA-MB-468 cells following incubation for 24, 48 and 72 h at all the concentrations tested, whereas it was the result of additive effect in MCF-7 and MDA-MB-453 cells at all the concentrations tested following 24 and 48-h incubation. In addition, the R index >1 obtained indicated the onset of a synergistic effect of the two compounds, compared with the corresponding single treatment, at a concentration of 15 mM in T47-D cells following 24-h incubation (P=0.0003), and in MDA-MB-231 cells following 24 and 48-h incubation (P<0.05). The combination of A+K resulted in a synergistic effect in MDA-MB-231 and MDA-MB-453 cells at concentrations of 10–15 mM (P<0.01), and in MCF-7 and T47-D cells at 10 mM concentration (P<0.001), following 72-h incubation.
Figure 1.
Effect of the interaction between potassium and ascorbic acid on the growth of breast cancer cell lines aftter 24, 48 and 72 h. The graphs represent the Kern's R index following treatment with the aforementioned compounds. R>1 represents a synergistic effect; R<1 indicates that the effect of the combined treatment is less than additive; and R=1 indicates that the effect is additive.
K potentiates the apoptotic effect of A in breast cancer cell lines
In order to determine the effect of K and A, alone or in combination, on the apoptosis and cell cycle distribution of breast cancer cells, a FACS analysis of their DNA content was performed. Cells were incubated for 24 h with the aforementioned compounds, alone or in combination, at a concentration of 10 mM, or with CTRL. Compared with CTRL, K treatment did not affect the cell cycle distribution in any of the cell lines evaluated (Table III). Compared with CTRL, treatment with 10 mM A induced a significant increase in the percentage of cells in the sub-G1 phase of the cell cycle in all the cell lines tested (P<0.001), except in T47-D and MDA-MB-468. This effect was associated with a significant decrease in the percentage of cells in G0/G1, S and G2/M phases in MDA-MB-231 (P<0.001), while a significant decrease in the percentage of cells in the G2/M phase was observed in MCF-7 cells (P<0.001). Treatment with A+K significantly increased the percentage of cells in the sub-G1 phase in MCF-7, MDA-MB-231, MDA-MB-453 and MDA-MB-468 cells, compared with treatment with A alone (P<0.001).
Table III.
Effects of 24-h treatment with 10 mM K and A, alone or in combination, on the cell cycle of breast cancer cell lines.
| Sub-G1 | G0/G1 | S | G2/M | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Cell line | Treatment | Cells (%) ±SD | P-value | Cells (%) ±SD | P-value | Cells (%) ±SD | P-value | Cells (%) ±SD | P-value |
| MCF-7 | CTRL | 6.32±2.09 | – | 38.42±2.35 | – | 16.77±1.85 | – | 37.13±0.15 | – |
| K | 5.85±1.81 | – | 36.57±2.76 | – | 17.07±2.74 | – | 38.56±0.52 | – | |
| A | 27.28±0.66 | 1c, 2c | 41.26±2.91 | – | 13.72±0.49 | – | 18.32±4.20 | 1c, 2c | |
| A+K | 51.05±0.91 | 1c, 3c | 36.76±0.86 | – | 3.97±0.16 | 1c, 2c, 3b | 8.42±2.38 | 1c, 2c, 3b | |
| T47-D | CTRL | 7.40±1.55 | – | 42.43±1.18 | – | 11.74±0.54 | – | 38.29±0.68 | – |
| K | 6.82±0.05 | – | 41.34±5.18 | – | 12.67±1.16 | – | 38.97±5.11 | – | |
| A | 17.86±5.12 | – | 39.26±5.27 | – | 12.43±1.68 | – | 30.36±1.86 | – | |
| A+K | 26.12±7.19 | 1c, 2a | 33.98±3.22 | – | 13.96±0.98 | – | 25.54±3.59 | – | |
| MDA-MB-231 | CTRL | 18.89±1.47 | – | 39.83±0.23 | – | 16.49±0.28 | – | 24.61±0.76 | – |
| K | 16.59±0.18 | – | 39.22± 0.48 | – | 17.23±0.09 | – | 26.17±0.64 | – | |
| A | 68.58±3.87 | 1c, 2c | 14.14±3.08 | 1c, 2c | 7.92±0.79 | 1c, 2c | 8.98±0.01 | 1c, 2c | |
| A+K | 91.07±3.45 | 1c, 3c | 5.39±1.81 | 1c, 2c, 3b | 2.58±1.22 | 1c, 2c, 3b | 0.91±0.35 | 1c, 2c, 3a | |
| MDA-MB-453 | CTRL | 7.14±1.09 | – | 50.98±3.79 | – | 12.03±1.45 | – | 28.43±3.15 | – |
| K | 6.85±1.28 | – | 51.59±1.76 | – | 11.55±1.06 | – | 29.17±1.75 | – | |
| A | 24.12±3.14 | 1c, 2a | 41.38±1.06 | 1c, 2a | 11.24±0.30 | – | 22.46±3.24 | – | |
| A+K | 43.36±11.03 | 1c, 3c | 30.30±4.76 | 1c, 2c, 3b | 8.83±0.90 | 1c, 2a | 16.96±4.33 | 1b, 2c | |
| MDA-MB-468 | CTRL | 6.74±0.73 | – | 52.04±4.75 | – | 15.86±2.70 | – | 25.66±3.12 | – |
| K | 7.65±1.07 | – | 51.12±5.13 | – | 16.81±3.35 | – | 24.74±4.83 | – | |
| A | 13.95±2.57 | – | 43.31±5.91 | – | 16.85±4.59 | – | 26.18±3.85 | – | |
| A+K | 37.30±6.10 | 1c, 3c | 34.18±2.60 | 1c, 2b | 14.23±2.66 | – | 14.55±5.55 | 1c, 3a | |
The percentage of cells in the sub-G1, G0/G1, S and G2/M phases of the cell cycle was calculated using CellQuest Pro software. The data represent the mean of three independent experiments. The statistical significance of the effects obtained following treatment with compounds A and K, alone or in combination, was calculated vs. those obtained following treatment with (1) CTRL, (2) K and (3) A
P<0.05
P<0.01
P<0.001. CTRL, culture medium; K, potassium; A, ascorbic acid; SD, standard deviation.
In particular, the apoptotic rate obtained with the combined treatment was 1.87, 1.46, 1.33, 1.80 and 2.67 times higher than that obtained following treatment with A in MCF-7, T47-D, MDA-MB-231, MDA-MB-453 and MDA-MB-468 cells, respectively.
In addition, a significant decrease in the percentage of MCF-7 cells in S and G2/M phases was observed following treatment with A+K, compared with A alone (P<0.01). Treatment with A+K reduced the percentage of MDA-MB-231 cells in G0/G1 (P<0.01), S (P<0.01) and G2/M (P<0.05) phases, compared with A. Treatment with A+K resulted in a significant decrease in the percentage of cells in G0/G1 phase, compared with treatment with A, in MDA-MB-453 (P<0.01) and MDA-MB-468 (P<0.05) cells. Overall, these results indicated an heterogeneous response of different cell lines to treatment with A and/or K, with the maximum effect achieved following combined treatment with A and K.
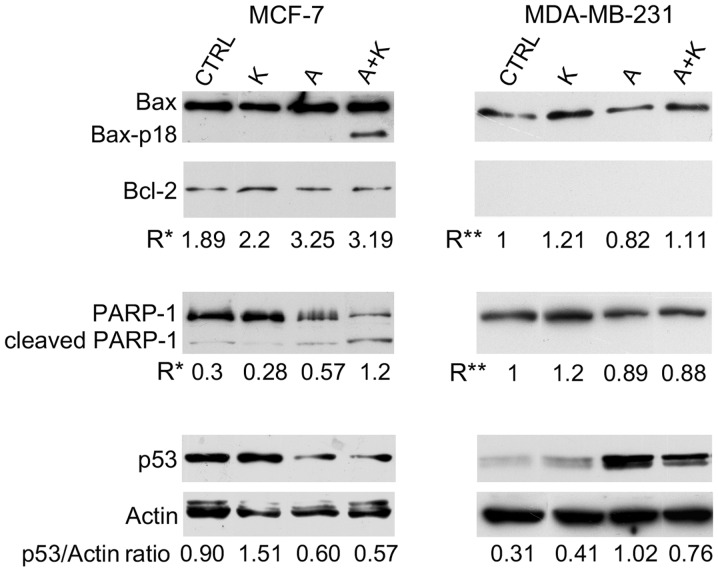
Effect of K and A, alone or in combination, on signaling proteins associated with apoptosis
The expression levels of signaling proteins associated with apoptosis were investigated by western blotting in MCF-7, MDA-MB-231 and MDA-MD-435 cells treated for 24 h with 10 mM A and K, alone or in combination. A representative experiment is illustrated in Fig. 2.
Figure 2.
Effect of A and K, alone or in combination, on signaling proteins associated with apoptosis. The expression levels of Bax, Bax-p18 (molecular weight, 18 kDa), Bcl-2, cleaved PARP-1 and p53 were assessed by western blotting in MCF-7 and MDA-MB-231 cells treated for 24 h with 10 mM A and K, alone or in combination, or with CTRL. Actin was used as an internal control. The intensity of the bands obtained in two independent experiments was quantified using ImageJ software following blot scanning. R* represents the densitometry ratios between the expression levels of Bax and Bcl-2 or between the levels of cleaved vs. full-length PARP-1. R** represents the increase in the expression levels of Bax following treatment with A and/or K respect to CTRL, or the decrease in the expression levels of full-length PARP-1 following treatment with A and/or K, compared with CTRL. The expression levels of p53 vs. actin are also reported. The faint higher molecular weight products observed with the anti-actin antibody and the lower molecular weight product observed with the anti-p53 antibody may be due to non-specific antibody reactions in these cell lines. CTRL, culture medium; K, potassium; A, ascorbic acid; Bcl-2, B-cell lymphoma-2; Bax, Bcl-2-associated X protein; PARP-1, poly(adenosine diphosphate-ribose) polymerase-1.
Treatment with A alone (P=0.0028), and in combination with K (P=0.0025) increased the Bax/Bcl-2 ratio (R*), compared with CTRL, in MCF-7 cells. Notably, A+K induced the appearance of the 18 kDa Bax isoform (Bax-p18) in MCF-7 cells, which is known to be a more potent inducer of apoptotic cell death than the full-length Bax-p21 (41). Bcl-2 was not detected in MDA-MB-231 cells; thus, only the expression of Bax following treatment with A and/or K vs. CTRL was evaluated. Treatment with A decreased Bax expression in MDA-MB-231 cells, compared with CTRL (R=0.82 vs. R=1.00, P=0.0017). Conversely, in this cell line, treatment with K increased Bax expression, and A+K combination was more effective than A (R=1.11 vs. R=0.82; P=0.0015).
To further corroborate that the effect of the aforementioned compounds on the increased number of cells in the sub-G1 phase of the cell cycle was due to the induction of apoptosis, the cleavage of PARP-1 was analyzed by western blotting. As represented in Fig. 2, treatment with A, alone or in combination with K, resulted in considerable proteolytic cleavage of PARP-1 or in decreased expression of full-length PARP-1, compared with CTRL, in MCF-7 cells. A+K was the most effective treatment in activating the degradation of PARP-1, compared with CTRL (R=1.20 vs. R=0.30, P=0.0045) and A (R=1.20 vs. R=0.57, P=0.0072). Decreased expression of PARP-1, possibly due to degradation of the protein, was observed in MDA-MB-231 cells following treatment with A, alone or in combination with K. Treatment with K alone did not decrease the expression of PARP-1 or induced its degradation.
To determine whether the apoptosis induced by A in MCF-7 and MDA-MB-231 cells was p53-dependent, the expression levels of p53 were analyzed. A (R=0.60) and A+K (R=0.57) reduced the expression of p53 in MCF-7 cells, compared with CTRL (R=0.90, P<0.01) and K (R=1.51, P<0.001). In addition, K and A increased p53 expression in MDA-MB-231 cells, compared with CTRL (R=0.41 vs. R=0.31, P=0.014 and R=1.02 vs. R=0.31, P=0.001, respectively). However, the combination of the two compounds was less effective than treatment with A alone in increasing the expression of p53 (R=0.76 vs. R=1.02, P=0.014).
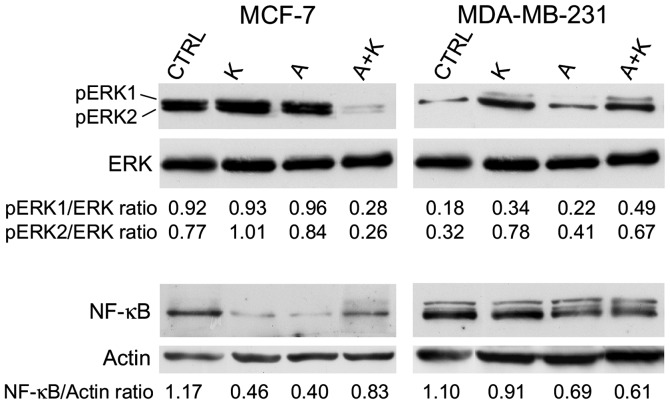
Effect of K and A, alone or in combination, on ERK1/ERK2 and NF-κB signaling proteins
The effect of A and K on ERK phosphorylation was investigated. The expression levels of p-ERK1 and p-ERK2 were compared with those of total ERK. The results are presented in Fig. 3. The expression of ERK was not altered following different treatments in any of the cell lines assessed. K increased the phosphorylation of ERK2 in MCF-7 cells. However, when A was administered in combination with K, it was able to counteract the phosphorylation of ERK1/ERK2 observed upon treatment with A or K alone (R=0.28 vs. R=0.93, P=0.0008 for K and R=0.28 vs. R=0.96, P=0.0005 for A, in the case of ERK1; and R=0.26 vs. R=1.01, P=0.0001 for K and R=0.26 vs. R=0.84, P=0.0004 for A, in the case of ERK2). Similarly, while A did not affect ERK1/ERK2 phosphorylation, K increased ERK1 and ERK2 phosphorylation, compared with CTRL (R=0.34 vs. R=0.18, P=0.024 for ERK1 and R=0.78 vs. R=0.32, P=0.006 for ERK2) in MDA-MB-231 cells.
Figure 3.
Effect of treatment with A and K, alone or in combination, on pro-survival signaling proteins. Western blotting was performed on MCF-7 and MDA-MB-231 cells treated with A or K, alone or in combination, for 24 h. The levels of phosphorylated ERK1/ERK2 were compared with the total protein levels of ERK, and the ratio values are reported. Quantitative densitometric analysis of the expression levels of nuclear factor-κB, compared with the levels of actin, is provided. The faint higher molecular weight product observed with the NF-κB antibody in the MDA-MB-231 cells may be due to non-specific reactions in this cell line. CTRL, culture medium; K, potassium; A, ascorbic acid; ERK, extracellular signal-regulated kinase; p, phosphorylated; NF-κB, nuclear factor-κB.
Next, the effect of A and K, alone or in combination, on NF-κB expression was investigated. Treatment with K, A and A+K inhibited NF-κB expression, compared with CTRL, in all cell lines (P=0.0017 for K, P=0.0017 for A and P=0.016 for A+K in MCF-7 cells; P=0.0084 for K, P=0.0015 for A and P=0.001 for A+K in MDA-MB-231 cells). A+K inhibited the expression of NF-κB in MDA-MB-231 cells, compared with A or K alone (A+K vs. K, R=0.61 vs. 0.91, P=0.0014; A+K vs. A, R=0.61 vs. 0.69, P=0.008).
Discussion
The use of A as an anti-cancer agent has been extensively analyzed during the last 50 years (1,2). Previous epidemiological studies have demonstrated the preventive effect of A in several human tumors when A was ingested through the diet (1,2). The intake of A in the diet was associated with lower mortality and lower incidence of numerous human malignancies, including cancer of the esophagus, oral cavity, stomach, pancreas, cervix, rectum, breast and lung (1,2).
A possesses both pro-oxidant and anti-oxidant properties (42–50). Although the preventive anti-cancer effect of A results from its anti-oxidant properties (42), previous in vitro studies and mouse models have demonstrated that A is able to inhibit cell proliferation in various types of cancer due to its ability to induce the production of H2O2 (43–49) without being toxic to non-cancerous cells (43,50). A also possesses anti-metastatic (51), anti-angiogenic (42) and immuno-stimulatory properties (52). In addition, previous epidemiological studies have confirmed that A in combination with chemotherapy or radiation does not cause side effects in patients with breast cancer (53), and is able to extend survival (54) and improve the quality of life (55) of cancer patients.
Similarly, it has been previously demonstrated that K is both an anti-apoptotic and a pro-apoptotic agent (13,14), as well as a regulator of cell proliferation (15–17). The intracellular homeostasis of Na+ and K+ is disregulated in cancer cells (27). This is due to an alteration in the expression and activity of Na+/K+ ATPase in tumor cells, which modifies the active transport of Na+ and K+, leading to a diffusion of intracellular K+ outside the membrane and a consequent increase of the intracellular levels of Na+ (27,56,57). This mechanism causes the release of calcium from its intracellular deposits and a simultaneous increase in glucose uptake, thus enhancing mitogenic stimulation (27,56,57). It has been previously demonstrated that the administration of K ascorbate produced anticancer effects in vitro (30,58), possibly due to the carrier properties of A, which allows a rapid diffusion of K into the cells, leading to the inhibition of tumor cell proliferation (27,30).
The results of the present study confirm that A exerts an inhibitory effect on the survival of various breast cancer cell lines. K alone exhibited an inhibitory effect only at the highest concentration tested and following 48-h incubation in MCF-7 cells. The effect of A was dose- and time-dependent in all the cell lines evaluated, with the exception of MDA-MB-231. K ascorbate (formed by combining A+K) significantly increased the apoptotic rate of all cell lines, with the exception of MDA-MB-468, whose apoptotic rate did not significantly differ from that of cells treated with A. The combination of A+K resulted in a synergistic effect in MDA-MB-231 and MDA-MB-453 cells at 10–15 mM concentration (P<0.01), and in MCF-7 and T47-D cells at 10 mM concentration (P<0.001), following 72-h incubation.
The results of FACS analysis further supported a synergic effect of A+K, since treatment with A+K significantly increased the percentage of cells in the sub-G1 phase of the cell cycle, compared with A alone, in MCF-7, MDA-MB-231, MDA-MB-453 and MDA-MB-468 cells (P<0.001). The increase in the apoptotic rate observed upon treatment with A+K indicated an anti-tumoral effect of the compound K in the majority of the cell lines tested. A+K was the most effective treatment in activating the degradation of PARP-1, compared with CTRL and A alone, thus corroborating the activation of apoptosis caused by A+K. The mechanisms responsible for the markedly positive but heterogeneous effects observed in the different cell lines analyzed in the present study, coupled with the variable results obtained upon different exposure times, require further investigation, possibly by evaluating the effect of the aforementioned treatments at longer times. A possible explanation for the heterogeneous effect of the compounds A and K on the different cell lines tested in the present study may be the intrinsic biological characteristics of the breast cancer cell lines used, since all cell lines, with the exception of MCF-7, exhibit a mutated p53 (59), while MCF-7 and T47-D cell lines are positive for estrogen and progesterone receptors, whereas MDA-MB-453 overexpresses ErbB2 (60).
Another potential explanation for the heterogeneous effect observed in different breast cancer cell lines upon treatment with A and K in the present study may be the cell length and conformation of telomeres, which may be affected by the concentration of K+ in the different cell lines tested (61). In healthy cells, each cell replication results in 50–200 bp loss of the telomere (62). When a critical shortening of the telomeric DNA is reached, the cell undergoes apoptosis (62). Telomeres of cancer cells do not shorten following replication, due to the activation of a reverse transcriptase telomerase, which is activated in 80–85% of human cancer cells and extends the telomeric sequence at the chromosome ends (63). G-rich telomeres may fold into G-quadruplexes, which are DNA secondary structures consisting of stacked G-tetrad planes connected by a network of Hoogsteen hydrogen bonds and stabilized by monovalent cations such as Na+ and K+ (64). The formation of G-quadruplexes by single-stranded human telomeric DNA inhibits the activity of the aforementioned reverse transcriptase telomerase (64). Compounds that stabilize the intramolecular DNA G-quadruplexes formed in the human telomeric sequence have been demonstrated to inhibit the activity of this telomerase, thus disrupting the capping and maintenance of the telomeres. Therefore, intramolecular human telomeric DNA G-quadruplexes are considered an attractive target for cancer therapeutic intervention (65–67). G-quadruplexes may adopt different shapes depending on the type of mineral content that they are exposed to (23). The K+ structure of G-quadruplexes is considered to be biologically more relevant than Na+ structure, due to the higher physiological intracellular concentration of K+ (68–71). Previous studies have revealed that hybrid-type intramolecular G-quadruplexes appear to be the predominant conformation formed in human telomeric sequences in solution in the presence of K+ (72,73). It has been reported that the increase of K+ transported into the cells alters the shape of G-quadruplexes (30). Therefore, the time-dependent effect observed in the present study upon treatment with A and K may reflect the time required for G-quadruplexes in tumor cells to shift from the Na+ to the K+ form. This would allow the generation of reactive oxygen species leading to oxidative DNA damage (74).
Overall, the present results indicated that K potentiated the anti-tumor effects of A in certain breast cancer cell lines. However, further in vitro and in vivo analyses are required to understand the mechanisms of action of K ascorbate, a natural compound with promising potential as an anti-cancer drug.
Acknowledgements
The present study was partly funded by a grant from the University of Rome ‘Sapienza’ (Rome, Italy; grant no. C26A14T57T).
References
- 1.Khaw KT, Bingham S, Welch A, Luben R, Wareham N, Oakes S, Day N. Relation between plasma ascorbic acid and mortality in men and women in EPIC-Norfolk prospective study: A prospective population study. European Prospective Investigation into Cancer and Nutrition. Lancet. 2001;357:657–663. doi: 10.1016/S0140-6736(00)04128-3. [DOI] [PubMed] [Google Scholar]
- 2.Block G. Epidemiologic evidence regarding vitamin C and cancer. Am J Clin Nutr. 1991;54(Suppl 6):1310S–1314S. doi: 10.1093/ajcn/54.6.1310s. [DOI] [PubMed] [Google Scholar]
- 3.Cameron E, Pauling L. The orthomolecular treatment of cancer. I. The role of ascorbic acid in host resistance. Chem Biol Interact. 1974;9:273–283. doi: 10.1016/0009-2797(74)90018-0. [DOI] [PubMed] [Google Scholar]
- 4.Creagan ET, Moertel CG, O'Fallon JR, Schutt AJ, O'Connell MJ, Rubin J, Frytak S. Failure of high-dose vitamin C (ascorbic acid) therapy to benefit patients with advanced cancer. A controlled trial. N Engl J Med. 1979;301:687–690. doi: 10.1056/NEJM197909273011303. [DOI] [PubMed] [Google Scholar]
- 5.Ohno S, Ohno Y, Suzuki N, Soma G, Inoue M. High-dose vitamin C (ascorbic acid) therapy in the treatment of patients with advanced cancer. Anticancer Res. 2009;29:809–815. [PubMed] [Google Scholar]
- 6.Levine M, Conry-Cantilena C, Wang Y, Welch RW, Washko PW, Dhariwal KR, Park JB, Lazarev A, Graumlich JF, King J, Cantilena LR. Vitamin C pharmacokinetics in healthy volunteers: Evidence for a recommended dietary allowance. Proc Natl Acad Sci USA. 1996;93:3704–3709. doi: 10.1073/pnas.93.8.3704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levine M, Wang Y, Padayatty SJ, Morrow J. A new recommended dietary allowance of vitamin C for healthy young women. Proc Natl Acad Sci USA. 2001;98:9842–9846. doi: 10.1073/pnas.171318198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Padayatty SJ, Sun H, Wang Y, Riordan HD, Hewitt SM, Katz A, Wesley RA, Levine M. Vitamin C pharmacokinetics: Implications for oral and intravenous use. Ann Intern Med. 2004;140:533–537. doi: 10.7326/0003-4819-140-7-200404060-00010. [DOI] [PubMed] [Google Scholar]
- 9.Hoffer LJ, Levine M, Assouline S, Melnychuk D, Padayatty SJ, Rosadiuk K, Rousseau C, Robitaille L, Miller WH., Jr Phase I clinical trial of i.v. ascorbic acid in advanced malignancy. Ann Oncol. 2008;19:1969–1974. doi: 10.1093/annonc/mdn377. [DOI] [PubMed] [Google Scholar]
- 10.Parrow NL, Leshin JA, Levine M. Parenteral ascorbate as a cancer therapeutic: A reassessment based on pharmacokinetics. Antioxid Redox Signal. 2013;19:2141–2156. doi: 10.1089/ars.2013.5372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma Y, Chapman J, Levine M, Polireddy K, Drisko J, Chen Q. High-dose parenteral ascorbate enhanced chemosensitivity of ovarian cancer and reduced toxicity of chemotherapy. Sci Transl Med. 2014;6:222ra18. doi: 10.1126/scitranslmed.3007154. [DOI] [PubMed] [Google Scholar]
- 12.Cone CD., Jr Unified theory on the basic mechanism of normal mitotic control and oncogenesis. J Theor Biol. 1971;30:151–181. doi: 10.1016/0022-5193(71)90042-7. [DOI] [PubMed] [Google Scholar]
- 13.Hughes FM, Jr, Cidlowski JA. Potassium is a critical regulator of apoptotic enzymes in vitro and in vivo. Adv Enzyme Regul. 1999;39:157–171. doi: 10.1016/S0065-2571(98)00010-7. [DOI] [PubMed] [Google Scholar]
- 14.Wang Z. Roles of K+ channels in regulating tumour cell proliferation and apoptosis. Pflugers Arch. 2004;448:274–286. doi: 10.1007/s00424-004-1258-5. [DOI] [PubMed] [Google Scholar]
- 15.DeCoursey TE, Chandy KG, Gupta S, Cahalan MD. Voltage-gated K+ channels in human T lymphocytes: A role in mitogenesis? Nature. 1984;307:465–468. doi: 10.1038/307465a0. [DOI] [PubMed] [Google Scholar]
- 16.Pardo LA. Voltage-gated potassium channels in cell proliferation. Physiology (Bethesda) 2004;19:285–292. doi: 10.1152/physiol.00011.2004. [DOI] [PubMed] [Google Scholar]
- 17.Wonderlin WF, Strobl JS. Potassium channels, proliferation and G1 progression. J Membr Biol. 1996;154:91–107. doi: 10.1007/s002329900135. [DOI] [PubMed] [Google Scholar]
- 18.Boros LG, Lee PW, Brandes JL, Cascante M, Muscarella P, Schirmer WJ, Melvin WS, Ellison EC. Nonoxidative pentose phosphate pathways and their direct role in ribose synthesis in tumors: Is cancer a disease of cellular glucose metabolism? Med Hypotheses. 1998;50:55–59. doi: 10.1016/S0306-9877(98)90178-5. [DOI] [PubMed] [Google Scholar]
- 19.Smith NK, Stabler SB, Cameron IL, Medina D. X-Ray microanalysis of electrolyte content of normal, preneoplastic, and neoplastic mouse mammary tissue. Cancer Res. 1981;41:3877–3880. [PubMed] [Google Scholar]
- 20.Arrebola F, Fernández-Segura E, Campos A, Crespo PV, Skepper JN, Warley A. Changes in intracellular electrolyte concentrations during apoptosis induced by UV irradiation of human myeloblastic cells. Am J Physiol Cell Physiol. 2006;290:C638–C649. doi: 10.1152/ajpcell.00364.2005. [DOI] [PubMed] [Google Scholar]
- 21.Mobasheri A, Fox R, Evans I, Cullingham F, Martín-Vasallo P, Foster CS. Epithelial Na, K-ATPase expression is down-regulated in canine prostate cancer; a possible consequence of metabolic transformation in the process of prostate malignancy. Cancer Cell Int. 2003;3:8. doi: 10.1186/1475-2867-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen JQ, Contreras RG, Wang R, Fernandez SV, Shoshani L, Russo IH, Cereijido M, Russo J. Sodium/potassium ATPase (Na+, K+-ATPase) and ouabain/related cardiac glycosides: A new paradigm for development of anti-breast cancer drugs? Breast Cancer Res Treat. 2006;96:1–15. doi: 10.1007/s10549-005-9053-3. [DOI] [PubMed] [Google Scholar]
- 23.Parkinson GN, Lee MP, Neidle S. Crystal structure of parallel quadruplexes from human telomeric DNA. Nature. 2002;417:876–880. doi: 10.1038/nature755. [DOI] [PubMed] [Google Scholar]
- 24.Salvati E, Rizzo A, Iachettini S, Zizza P, Cingolani C, D'Angelo C, Porru M, Mondello C, Aiello A, Farsetti A, et al. A basal level of DNA damage and telomere deprotection increases the sensitivity of cancer cells to G-quadruplex interactive compounds. Nucleic Acids Res. 2015;43:1759–1769. doi: 10.1093/nar/gkv006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dai J, Carver M, Yang D. Polymorphism of human telomeric quadruplex structures. Biochimie. 2008;90:1172–1183. doi: 10.1016/j.biochi.2008.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelland LR. Overcoming the immortality of tumour cells by telomere and telomerase based cancer therapeutics - current status and future prospects. Eur J Cancer. 2005;41:971–979. doi: 10.1016/j.ejca.2004.11.024. [DOI] [PubMed] [Google Scholar]
- 27.Paoli G. The Bio-magnetic nature of cancer and the role of potassium ascorbate and ribose against cellar degeneration. J Nucl Energy. 2003;7:114–119. [Google Scholar]
- 28.Croci S, Pedrazzi G, Passeri G, Delsignore R, Ortalli I. Red cell Hb oxidation of healthy subjects compared to breast cancer patients. Anticancer Res. 2002;22:2903–2906. [PubMed] [Google Scholar]
- 29.Croci S, Pedrazzi G, Passeri G, Piccolo P, Ortalli I. Acetylphenylhydrazine induced haemoglobin oxidation in erythrocytes studied by Mössbauer spectroscopy. Biochim Biophys Acta. 2001;1568:99–104. doi: 10.1016/S0304-4165(01)00205-7. [DOI] [PubMed] [Google Scholar]
- 30.Croci S, Bruni L, Bussolati S, Castaldo M, Dondi M. Potassium bicarbonate and D-ribose effects on A72 canine and HTB-126 human cancer cell line proliferation in vitro. Cancer Cell Int. 2011;11:30. doi: 10.1186/1475-2867-11-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Masuelli L, Marzocchella L, Quaranta A, Palumbo C, Pompa G, Izzi V, Canini A, Modesti A, Galvano F, Bei R. Apigenin induces apoptosis and impairs head and neck carcinomas EGFR/ErbB2 signaling. Front Biosci (Landmark Ed) 2011;16:1060–1068. doi: 10.2741/3735. [DOI] [PubMed] [Google Scholar]
- 32.Masuelli L, Marzocchella L, Focaccetti C, Tresoldi I, Palumbo C, Izzi V, Benvenuto M, Fantini M, Lista F, Tarantino U, et al. Resveratrol and diallyl disulfide enhance curcumin-induced sarcoma cell apoptosis. Front Biosci (Landmark Ed) 2012;17:498–508. doi: 10.2741/3940. [DOI] [PubMed] [Google Scholar]
- 33.Bei R, Masuelli L, Moriconi E, Visco V, Moretti A, Kraus MH, Muraro R. Immune responses to all ErbB family receptors detectable in serum of cancer patients. Oncogene. 1999;18:1267–1275. doi: 10.1038/sj.onc.1202442. [DOI] [PubMed] [Google Scholar]
- 34.Bei R, Budillon A, Masuelli L, Cereda V, Vitolo D, Di Gennaro E, Ripavecchia V, Palumbo C, Ionna F, Losito S, et al. Frequent overexpression of multiple ErbB receptors by head and neck squamous cell carcinoma contrasts with rare antibody immunity in patients. J Pathol. 2004;204:317–325. doi: 10.1002/path.1642. [DOI] [PubMed] [Google Scholar]
- 35.Faggioni G, Pomponi A, De Santis R, Masuelli L, Ciammaruconi A, Monaco F, Di Gennaro A, Marzocchella L, Sambri V, Lelli R, et al. West Nile alternative open reading frame (N-NS4B/WARF4) is produced in infected West Nile Virus (WNV) cells and induces humoral response in WNV infected individuals. Virol J. 2012;9:283. doi: 10.1186/1743-422X-9-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Masuelli L, Budillon A, Marzocchella L, Mrozek MA, Vitolo D, Di Gennaro E, Losito S, Sale P, Longo F, Ionna F, et al. Caveolin-1 overexpression is associated with simultaneous abnormal expression of the E-cadherin/α-β catenins complex and multiple ErbB receptors and with lymph nodes metastasis in head and neck squamous cell carcinomas. J Cell Physiol. 2012;227:3344–3353. doi: 10.1002/jcp.24034. [DOI] [PubMed] [Google Scholar]
- 37.Masuelli L, Bei R, Sacchetti P, Scappaticci I, Francalanci P, Albonici L, Coletti A, Palumbo C, Minieri M, Fiaccavento R, et al. Beta-catenin accumulates in intercalated disks of hypertrophic cardiomyopathic hearts. Cardiovasc Res. 2003;60:376–387. doi: 10.1016/j.cardiores.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 38.Masuelli L, Pompa G, Fabrizi M, Quaranta A, Vozza I, Piccoli L, Antonelli A, Marzocchella L, Di Carlo S, Perrotti V, et al. Patients with peri-implantitis, unlike those with a healthy periimplant microenvironment, display antibodies to more than one heat shock protein (HSP 27, HSP 65 and HSP 90) linear epitope. Eur J Inflamm. 2011;9:257–267. [Google Scholar]
- 39.Ingrosso G, Fantini M, Nardi A, Benvenuto M, Sacchetti P, Masuelli L, Ponti E, Frajese GV, Lista F, Schillaci O, et al. Local radiotherapy increases the level of autoantibodies to ribosomal P0 protein but not to heat shock proteins, extracellular matrix molecules and EGFR/ErbB2 receptors in prostate cancer patients. Oncol Rep. 2013;29:1167–1174. doi: 10.3892/or.2012.2197. [DOI] [PubMed] [Google Scholar]
- 40.Palumbo C, Albonici L, Bei R, Bocci C, Scarpa S, Di Nardo P, Modesti A. HMBA induces cell death and potentiates doxorubicin toxicity in malignant mesothelioma cells. Cancer Chemother Pharmacol. 2004;54:398–406. doi: 10.1007/s00280-004-0838-6. [DOI] [PubMed] [Google Scholar]
- 41.Toyota H, Yanase N, Yoshimoto T, Moriyama M, Sudo T, Mizuguchi J. Calpain-induced Bax-cleavage product is a more potent inducer of apoptotic cell death than wild-type Bax. Cancer Lett. 2003;189:221–230. doi: 10.1016/S0304-3835(02)00552-9. [DOI] [PubMed] [Google Scholar]
- 42.Du J, Cullen JJ, Buettner GR. Ascorbic acid: Chemistry, biology and the treatment of cancer. Biochim Biophys Acta. 2012;1826:443–457. doi: 10.1016/j.bbcan.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen Q, Espey MG, Krishna MC, Mitchell JB, Corpe CP, Buettner GR, Shacter E, Levine M. Pharmacologic ascorbic acid concentrations selectively kill cancer cells: Action as a pro-drug to deliver hydrogen peroxide to tissues. Proc Natl Acad Sci USA. 2005;102:13604–13609. doi: 10.1073/pnas.0506390102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Du J, Martin SM, Levine M, Wagner BA, Buettner GR, Wang SH, Taghiyev AF, Du C, Knudson CM, Cullen JJ. Mechanisms of ascorbate-induced cytotoxicity in pancreatic cancer. Clin Cancer Res. 2010;16:509–520. doi: 10.1158/1078-0432.CCR-09-1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen P, Yu J, Chalmers B, Drisko J, Yang J, Li B, Chen Q. Pharmacological ascorbate induces cytotoxicity in prostate cancer cells through ATP depletion and induction of autophagy. Anticancer Drugs. 2012;23:437–444. doi: 10.1097/CAD.0b013e32834fd01f. [DOI] [PubMed] [Google Scholar]
- 46.Martinovich GG, Golubeva EN, Martinovich IV, Cherenkevich SN. Redox regulation of calcium signaling in cancer cells by ascorbic acid involving the mitochondrial electron transport chain. J Biophys. 2012;2012:921653. doi: 10.1155/2012/921653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Han SS, Kim K, Hahm ER, Lee SJ, Surh YJ, Park HK, Kim WS, Jung CW, Lee MH, Park K, et al. L-ascorbic acid represses constitutive activation of NF-kappaB and COX-2 expression in human acute myeloid leukemia, HL-60. J Cell Biochem. 2004;93:257–270. doi: 10.1002/jcb.20116. [DOI] [PubMed] [Google Scholar]
- 48.Park S, Ahn ES, Lee S, Jung M, Park JH, Yi SY, Yeom CH. Proteomic analysis reveals upregulation of RKIP in S-180 implanted BALB/C mouse after treatment with ascorbic acid. J Cell Biochem. 2009;106:1136–1145. doi: 10.1002/jcb.22097. [DOI] [PubMed] [Google Scholar]
- 49.Ranzato E, Biffo S, Burlando B. Selective ascorbate toxicity in malignant mesothelioma: A redox Trojan mechanism. Am J Respir Cell Mol Biol. 2011;44:108–117. doi: 10.1165/rcmb.2009-0340OC. [DOI] [PubMed] [Google Scholar]
- 50.Chen Q, Espey MG, Sun AY, Lee JH, Krishna MC, Shacter E, Choyke PL, Pooput C, Kirk KL, Buettner GR, Levine M. Ascorbate in pharmacologic concentrations selectively generates ascorbate radical and hydrogen peroxide in extracellular fluid in vivo. Proc Natl Acad Sci USA. 2007;104:8749–8754. doi: 10.1073/pnas.0702854104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cha J, Roomi MW, Ivanov V, Kalinovsky T, Niedzwiecki A, Rath M. Ascorbate supplementation inhibits growth and metastasis of B16FO melanoma and 4T1 breast cancer cells in vitamin C-deficient mice. Int J Oncol. 2013;42:55–64. doi: 10.3892/ijo.2012.1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim JE, Cho HS, Yang HS, Jung DJ, Hong SW, Hung CF, Lee WJ, Kim D. Depletion of ascorbic acid impairs NK cell activity against ovarian cancer in a mouse model. Immunobiology. 2012;217:873–881. doi: 10.1016/j.imbio.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 53.Riordan HD, Riordan NH, Jackson JA, Casciari JJ, Hunninghake R, González MJ, Mora EM, Miranda-Massari JR, Rosario N, Rivera A. Intravenous vitamin C as a chemotherapy agent: A report on clinical cases. P R Health Sci J. 2004;23:115–118. [PubMed] [Google Scholar]
- 54.Shimpo K, Nagatsu T, Yamada K, Sato T, Niimi H, Shamoto M, Takeuchi T, Umezawa H, Fujita K. Ascorbic acid and adriamycin toxicity. Am J Clin Nutr. 1991;54(Suppl 6):1298S–1301S. doi: 10.1093/ajcn/54.6.1298s. [DOI] [PubMed] [Google Scholar]
- 55.Vollbracht C, Schneider B, Leendert V, Weiss G, Auerbach L, Beuth J. Intravenous vitamin C administration improves quality of life in breast cancer patients during chemo-/radiotherapy and aftercare: Results of a retrospective, multicentre, epidemiological cohort study in Germany. In Vivo. 2011;25:983–990. [PubMed] [Google Scholar]
- 56.L'Allemain G, Paris S, Pouysségur J. Growth factor action and intracellular pH regulation in fibroblasts. Evidence for a major role of the Na+/H+ antiport. J Biol Chem. 1984;259:5809–5815. [PubMed] [Google Scholar]
- 57.Gerson DF, Kiefer H, Eufe W. Intracellular pH of mitogen-stimulated lymphocytes. Science. 1982;216:1009–1010. doi: 10.1126/science.6281887. [DOI] [PubMed] [Google Scholar]
- 58.Bruni L, Babarinde AA, Ortalli I, Croci S. K-D:rib dampens Hs 578T cancer cell chemoinvasion and proliferation. Cancer Cell Int. 2014;14:77. doi: 10.1186/s12935-014-0077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lacroix M, Toillon RA, Leclercq G. p53 and breast cancer, an update. Endocr Relat Cancer. 2006;13:293–325. doi: 10.1677/erc.1.01172. [DOI] [PubMed] [Google Scholar]
- 60.Subik K, Lee JF, Baxter L, Strzepek T, Costello D, Crowley P, Xing L, Hung MC, Bonfiglio T, Hicks DG, Tang P. The expression patterns of ER, PR, HER2, CK5/6, EGFR, Ki-67 and AR by immunohistochemical analysis in breast cancer cell lines. Breast Cancer (Auckl) 2010;4:35–41. [PMC free article] [PubMed] [Google Scholar]
- 61.Sun D, Lopez-Guajardo CC, Quada J, Hurley LH, Von Hoff DD. Regulation of catalytic activity and processivity of human telomerase. Biochemistry. 1999;38:4037–4044. doi: 10.1021/bi982249n. [DOI] [PubMed] [Google Scholar]
- 62.Harley CB, Futcher AB, Greider CW. Telomeres shorten during ageing of human fibroblasts. Nature. 1990;345:458–460. doi: 10.1038/345458a0. [DOI] [PubMed] [Google Scholar]
- 63.Kim NW, Piatyszek MA, Prowse KR, Harley CB, West MD, Ho PL, Coviello GM, Wright WE, Weinrich SL, Shay JW. Specific association of human telomerase activity with immortal cells and cancer. Science. 1994;266:2011–2015. doi: 10.1126/science.7605428. [DOI] [PubMed] [Google Scholar]
- 64.Zahler AM, Williamson JR, Cech TR, Prescott DM. Inhibition of telomerase by G-quartet DNA structures. Nature. 1991;350:718–720. doi: 10.1038/350718a0. [DOI] [PubMed] [Google Scholar]
- 65.Hurley LH. DNA and its associated processes as targets for cancer therapy. Nat Rev Cancer. 2002;2:188–200. doi: 10.1038/nrc749. [DOI] [PubMed] [Google Scholar]
- 66.Neidle S, Parkinson G. Telomere maintenance as a target for anticancer drug discovery. Nat Rev Drug Discov. 2002;1:383–393. doi: 10.1038/nrd793. [DOI] [PubMed] [Google Scholar]
- 67.Hurley LH, Wheelhouse RT, Sun D, Kerwin SM, Salazar M, Fedoroff OY, Han FX, Han H, Izbicka E, Von Hoff DD. G-quadruplexes as targets for drug design. Pharmacol Ther. 2000;85:141–158. doi: 10.1016/S0163-7258(99)00068-6. [DOI] [PubMed] [Google Scholar]
- 68.Redon S, Bombard S, Elizondo-Riojas MA, Chottard JC. Platinum cross-linking of adenines and guanines on the quadruplex structures of the AG3(T2AG3)3 and (T2AG3)4 human telomere sequences in Na+ and K+ solutions. Nucleic Acids Res. 2003;31:1605–1613. doi: 10.1093/nar/gkg259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Phan AT, Patel DJ. Two-repeat human telomeric d(TAGGGTTAGGGT) sequence forms interconverting parallel and antiparallel G-quadruplexes in solution: Distinct topologies, thermodynamic properties, and folding/unfolding kinetics. J Am Chem Soc. 2003;125:15021–15027. doi: 10.1021/ja037616j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li J, Correia JJ, Wang L, Trent JO, Chaires JB. Not so crystal clear: The structure of the human telomere G-quadruplex in solution differs from that present in a crystal. Nucleic Acids Res. 2005;33:4649–4659. doi: 10.1093/nar/gki782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Włodarczyk A, Grzybowski P, Patkowski A, Dobek A. Effect of ions on the polymorphism, effective charge, and stability of human telomeric DNA. Photon correlation spectroscopy and circular dichroism studies. J Phys Chem B. 2005;109:3594–3605. doi: 10.1021/jp045274d. [DOI] [PubMed] [Google Scholar]
- 72.Ambrus A, Chen D, Dai J, Bialis T, Jones RA, Yang D. Human telomeric sequence forms a hybrid-type intramolecular G-quadruplex structure with mixed parallel/antiparallel strands in potassium solution. Nucleic Acids Res. 2006;34:2723–2735. doi: 10.1093/nar/gkl348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dai J, Carver M, Punchihewa C, Jones RA, Yang D. Structure of the Hybrid-2 type intramolecular human telomeric G-quadruplex in K+ solution: Insights into structure polymorphism of the human telomeric sequence. Nucleic Acids Res. 2007;35:4927–4940. doi: 10.1093/nar/gkm522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hadi SM, Ullah MF, Shamim U, Bhatt SH, Azmi AS. Catalytic therapy of cancer by ascorbic acid involves redox cycling of exogenous/endogenous copper ions and generation of reactive oxygen species. Chemotherapy. 2010;56:280–284. doi: 10.1159/000319951. [DOI] [PubMed] [Google Scholar]