Abstract
Objective To examine the effects of Stepping Stones Triple P (SSTP) and Acceptance and Commitment Therapy (ACT) on child functioning, quality of life, and parental adjustment. Method 67 parents (97.0% mothers) of children (64.2% male; mean age 5.3 ± 3.0 years) with cerebral palsy participated in a randomized controlled trial with three groups: wait-list control, SSTP, and SSTP + ACT. This article details the secondary outcomes. Results In comparison with wait-list, the SSTP + ACT group showed increased functional performance and quality of life as well as decreased parental psychological symptoms. No differences were found for parental confidence. No differences were found between SSTP and wait-list or between SSTP and SSTP + ACT. Conclusions ACT-integrated parenting intervention may be an effective way to target child functioning, quality of life, and parental adjustment.
Keywords: cerebral palsy, family therapy, parenting, quality of life
Cerebral palsy (CP) is the most common physical disability in childhood, occurring in 2.0–2.5 of every 1,000 live births (Stanley, Blair, & Alberman, 2000). Although the definition of CP focuses on the disorder of the development of movement and posture (Rosenbaum, Paneth, Leviton, Goldstein, & Bax, 2007), cognitive, sensory, and behavioral impairments are common (Novak, Hines, Goldsmith, & Barclay, 2012). Further, disability is understood as emerging from a complex interplay between individual and context (Colver, 2009), with the importance of family-centered care, everyday functioning, and quality-of-life issues increasingly recognized.
This article reports the secondary outcomes of the first randomized controlled trial (RCT) of a parenting intervention with families of children with CP (removed for blinded review). This study, reported in two papers, is also the first RCT to test the additive benefits of Acceptance and Commitment Therapy (ACT) above and beyond established parenting intervention. The primary outcomes of the three-group RCT were child behavioral problems and parenting styles. It was demonstrated that Stepping Stones Triple P (SSTP) combined with ACT was associated with improvements in child behavior and hyperactivity as well as decreases in dysfunctional parenting styles relative to the wait-list control group (removed for blinded review). SSTP alone was associated with improvements in child behavior and emotional symptoms. Within this article, the secondary outcomes of parental adjustment, parenting confidence, child functioning, and child quality of life will be explored.
Family-centered care involves providing services in partnership with parents and leveraging the understanding, skills, and day-to-day interactions that exist within the family system for the benefit of both child and family (Novak & Cusick, 2006; Novak, Cusick, & Lannin, 2009; Rosenbaum, King, Law, King, & Evans, 1998). To effectively leverage the resources within the family system, the family must be supported and parental adjustment must be considered. Parents of children with CP experience increased stress (Parkes, Caravale, Marcelli, Franco, & Colver, 2011), anxious and depressive symptoms (Barlow, Cullen-Powell, & Cheshire, 2006; Lach et al., 2009), as well as increased burden of care (Sawyer et al., 2011), and an adaptive grieving process termed chronic sorrow (Whittingham, Wee, Sanders, & Boyd, 2013a, 2013b). The links between parental adjustment and child psychological health are well understood (Newland, 2015). Thus, parental adjustment and confidence deserve consideration as outcomes of intervention.
Quality of life is individuals' subjective estimation of their life’s quality within the context of the systems in which they live and their expectations and goals (Colver, 2009; Waters et al., 2007; Zekovic & Renwick, 2003). In a cross-sectional study of 818 children (8–12 years) with CP, decreased impairment was associated with poorer parent-reported quality-of-life outcomes across emotional, self-perception, social acceptance, and school environmental domains (Arnaud et al., 2008). In a study of 743 children (8–12 years) measuring child-reported quality of life, specific impairments were associated with specific aspects of quality of life only, for example, self-mobility predicted physical well-being (Dickinson et al., 2007). Overall, impairment was associated with just 3% of the variance in quality of life. This suggests, consistent with the disability paradox (Albrecht & Devlieger, 1999), that impairment itself has less impact on quality of life than we intuitively estimate and that, if we wish to improve quality of life, we should look beyond impairment to identify appropriate targets. Parental stress is associated with all domains of parent-reported quality of life (Arnaud et al., 2008), and parenting style predicts physical and psychosocial quality of life in children with CP (Aran, Shalev, Biran, & Gross-Tsur, 2007). This suggests that targeting contextual family factors, such as parental adjustment and parenting style, may be an effective means to improve child quality of life.
This article focuses on testing the efficacy of SSTP combined with ACT for targeting child functional performance and quality of life as well as parental adjustment and confidence. SSTP is a variant of the widely disseminated parenting intervention Triple P (Positive Parenting Program) that targets families of children with disabilities (Roberts, Mazzucchelli, Studman, & Sanders, 2006). ACT is a Cognitive Behavioral Therapy that incorporates mindfulness (nonjudgmental psychological contact with present-moment experience), experiential acceptance (psychological contact with emotions, cognitions, and memories), and valued action (engagement in meaningful, values-driven activities), to enhance psychological flexibility (Coyne, McHugh, & Martinez, 2011; Hayes, Strosal, & Wilson, 2003). Psychological flexibility is the ability to persist or to change in your behavior with full awareness of your ongoing context, in the pursuit of valued ends. Whereas SSTP focuses on enhancing parenting skills, ACT focuses on the psychological meaning of parenting for the parent, increasing parental flexibility and boosting parent ability to use parenting skills in a stressful emotional context. ACT, and the combination of ACT with parenting intervention, has been shown to improve psychological adjustment in parents of children with developmental disabilities including autism (Blackledge & Hayes, 2006) and acquired brain injury (ABI) (Brown, Whittingham, Boyd, McKinlay, & Sofronoff, 2015). However, the additive effects of ACT above and beyond parenting intervention on child functioning and quality of life as well as on parental adjustment remain untested. Efficacy was tested in a three-group RCT (SSTP, SSTP + ACT, wait-list control).
The aim of this article was to examine efficacy in terms of the secondary outcomes of child functional performance, child quality of life, parental adjustment, and parenting confidence. It was predicted that both Stepping Stones alone and Stepping Stones combined with ACT would be associated with improvements in child functional performance, parent-reported child quality-of-life parental adjustment, and parental confidence in comparison with the wait-list control (WL) group. It was further predicted that Stepping Stones combined with ACT would be associated with additional benefits in parental adjustment.
Methods
Design
Child behavior and parenting style outcomes are reported elsewhere (removed for blinded review), and the study protocol details the design in full (removed for blinded review). Participants were allocated to three groups (Stepping Stone alone [SSTP]; Stepping Stones with Acceptance and Commitment therapy [SSTP + ACT]; and the wait-list control [WL]) in a two-phase RCT. The primary focus was the first phase, a comparison between SSTP, SSTP + ACT, and WL groups at postintervention. The WL group was offered the SSTP following postintervention for ethical reasons, and wait-list families were asked to complete additional postintervention assessment as well as follow-up assessment after they completed SSTP. The second phase involved testing maintenance at 6-month follow-up and included all families who received an intervention and completed follow-up assessment. The retention of intervention effect from postintervention to 6-month follow-up was tested. In addition, a comparison between families who received SSTP and families who received SSTP + ACT at 6-month follow-up was conducted.
Ethical clearance was obtained from the Children’s Health Queensland Human Research Ethics Committee (HREC/09/QRCH/125), the University of Queensland Behavioral and Social Sciences Ethical Review Committee (2009001871), and the Cerebral Palsy League Research Ethics Committee (CPLQ-2010/11/1033), and all participants provided written consent.
Participants
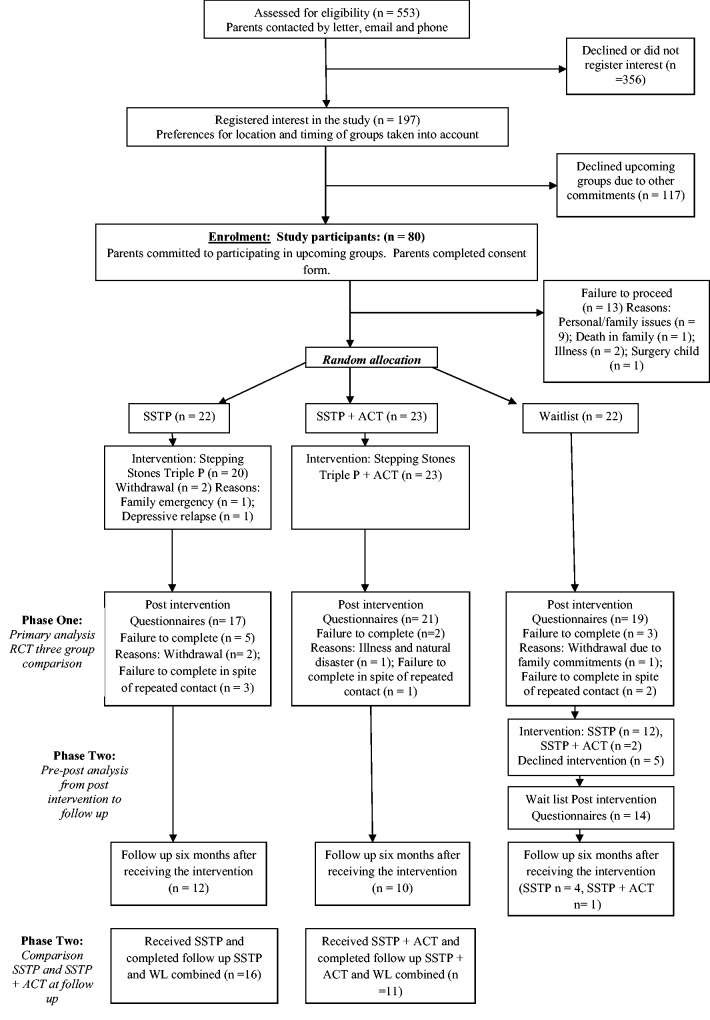
Participation was restricted to parents (including step, adoptive, and long-term foster parents) of children, aged 2–12 years, with a diagnosis of CP (all functional severity levels) who believed they would benefit from participating in a parenting intervention. Participants were recruited from the databases of the Queensland Cerebral Palsy and Rehabilitation Research Centre, the Cerebral Palsy League, and the Queensland Cerebral Palsy Register by mailing families who met inclusion criteria a study flyer. In addition, information on the study was placed in the waiting room of the Queensland Cerebral Palsy Health Service, allowing interested families the opportunity to register their interest with the study coordinator. The study flow is reported in Figure 1 according to Controlled Standards of Reporting Trials guidelines.
Figure 1.
Controlled Standards of Reporting Trials flow diagram.
Sample-Size Calculation
Sample-size calculations were based on the primary outcome, child behavior (removed for blinded review). An effect size of 0.25 was assumed, as it is comparable with the effect size for Stepping Stones (SSTP) obtained with the Autism Spectrum Disorder (ASD) population, η2 = .27 (Whittingham, Sofronoff, Sheffield, & Sanders, 2009), and it is consistent with a clinically important difference of 0.5 SD. A total sample size of 98 families (power 0.8, two-tailed, p = .05) was calculated, with 110 required to account for attrition.
Procedure
A computerized sequence generation with block randomization was used to ensure near-equal allocation of participants to groups. A staff member not involved in the study put allocations into sealed, opaque, and numbered envelopes. When a family enrolled in the study, the coordinator opened the next envelope in sequence. Each study participant was randomized to one of three groups: (1) SSTP; (2) SSTP + ACT; or (3) the WL group.
SSTP was delivered by psychologists with accreditation in SSTP (Sanders, Mazzucchelli, & Studman, 2003), and ACT was delivered by psychologists with training in ACT. SSTP consisted of six (2-hr) group sessions and three (30-min) telephone consultations, and the ACT intervention consisted of two (2-hr) group sessions. The SSTP + ACT group participated in ACT sessions first, before SSTP. A weekend workshop format (all group sessions in a single weekend) was a pragmatic solution to enable delivery as an outreach program in far North Queensland. Participants receiving the intervention in the weekend workshop format were offered phone consultations after the weekend workshop.
Intervention Content
Stepping Stones (SSTP) was delivered in line with the SSTP manual (Sanders et al., 2003) with sessions focussing on building a positive parent–child relationship, encouraging desirable behavior, teaching new skills and behaviors, managing misbehavior, and managing high-risk parenting situations. Parents are introduced to a range of evidence-based parenting strategies including spending quality time with children, descriptive praise, incidental teaching, logical consequences, and time out. Throughout the program, parents are assisted in setting goals for change, in monitoring their child’s behavior, and in using the parenting strategies discussed to achieve their goals. The SSTP DVD A Survival Guide for families with a child who has a disability was shown in group sessions to introduce specific concepts, as suggested in the SSTP manual.
ACT was delivered in line with a manual developed for this project, and consistently with the published literature on ACT (Hayes et al., 2003). The ACT sessions focussed on enhancing psychological flexibility through mindfulness (nonjudgmental psychological contact with present-moment experience), experiential acceptance (psychological contact with emotions, cognitions, and memories), and valuing (engagement in meaningful, values-driven activities). The intervention drew on metaphors commonly used in ACT including the battlefield metaphor, the quicksand metaphor, and the passengers on the bus metaphor. Mindfulness exercises included mindfulness of the breath, mindfulness of thoughts, and mindfulness of emotions. In addition, cognitive defusion techniques (techniques to increase psychological distance from thoughts) were used, for example, prefacing thoughts with “I’m noticing that I’m having the thought that…” The full manual is freely available by contacting the first author.
Assessment
The Family Background Questionnaire was used to gather demographic data (Sanders, Mazzucchelli, & Studman, 2009), and the Gross Motor Function Classification System was used to classify children by gross motor functional ability (Palisano, 1997), as described in the study protocol (removed for blinded review). Child behavior and parenting style outcomes were reported elsewhere (removed for blinded review).
This article focuses on reporting outcomes for child functional performance (Pediatric Evaluation of Disability Inventory; PEDI), child quality of life (Cerebral Palsy Quality of Life Child; CP QOL-child), parental adjustment (Depression Anxiety Stress Scale; DASS), and parental confidence and problems in performing disability-related parenting practices (Cerebral Palsy Daily Parenting Tasks Checklist; CP-DPTC). All measures were parent report.
Pediatric Evaluation of Disability Inventory
The PEDI is a standardized measure of functional performance in children with disabilities with good validity and reliability (Haley, Coster, Ludlow, Haltiwanger, & Andrellos, 1992). Within this study, the capability scales were used, with parents responding to each item whether their child was or was not capable of that task. Responses are scored to obtain subscales with higher scores reflecting better functioning. The PEDI has three subscales: self-care (range: 0–73), mobility (range: 0–54), and social function (range: 0–65). Internal consistency was high in the current study for the self-care (α = .98), mobility (α = .98), and social function (α = .97) subscales.
Cerebral Palsy Quality of Life Child
The CP QOL-child measures parent-reported well-being across several aspects of the child’s life including social well-being and acceptance, feelings about functioning, participation and physical health, emotional well-being and self-esteem, access to services, pain and impact of disability, and family health (range 0–100 for all subscales). As a condition-specific measure, it has good concurrent validity and test–retest reliability (r = .80–.90) (Waters et al., 2007). Internal consistency in this sample was high for the social well-being and acceptance (α = .94), feelings about functioning (α = .91), participation (α = .94), emotional well-being and self-esteem (α = .84), access (α = .77), and family health (α = .81) scales. Internal consistency was poor for the pain and impact scale (α = .51).
Depression Anxiety Stress Scale
The DASS-42 produces three subscales: depression (range: 0–42), anxiety (range: 0–42), and stress (range: 0–42) scales, measuring depressive, anxious, and stress symptoms (Lovibond & Lovibond, 1995). The DASS also has good discriminant and concurrent validity. In this sample, internal consistency was high for the depression (α = .96), anxiety (α = .87), and stress (α = .94) scales.
Cerebral Palsy Daily Parenting Tasks Checklist
The CP-DPTC was developed specifically for this project based on qualitative research (removed for blinded review). It has 20 items detailing parenting tasks commonly performed by parents of children with physical disabilities, for example, “assisting my child with dressing.” Parents rate how problematic each task is and how confident they are at performing the task on Likert scales of 1–5. Responses are summed to produce two scales, the confidence scale (range: 20–100) measures parental confidence in performing specific daily parenting tasks and the problems scale (range: 20–100) measures how problematic those parenting tasks are for the parent. Internal consistency was high in this study for both the confidence (α = .95) and the problems (α = .88) scales.
Statistical Analysis
The first phase of the study, a comparison between groups receiving SSTP and SSTP + ACT and WL at postintervention, was achieved through a series of analyses of covariance (ANCOVAs) with preintervention scores as a covariate. Significant results were followed up to examine group by group differences with linear contrasts (i.e., WL vs. SSTP; WL vs. SSTP +ACT; SSTP vs. SSTP + ACT). A Bonferroni correction was applied to linear contrasts to correct for multiple comparisons resulting in a p value of .0167. A sensitivity analysis was conducted with the last observation carried forward.
The second phase of the study included all families who received an intervention and completed 6-month follow-up assessment (Total, n = 28: including SSTP, n = 12; SSTP + ACT, n = 11; wait-list, n = 5). The retention of the effect from postintervention to 6-month follow-up was tested with a series of paired t tests. A comparison between families who received SSTP (n = 16) and families who received SSTP + ACT (n = 12) at follow-up was conducted via a series of ANCOVAs with preintervention scores as a covariate. All families allocated to the WL group subsequently received SSTP except one family who received SSTP + ACT.
Results
Sample Characteristics
The study flow is reported in Figure 1, and sample characteristics are presented in Table I. Recruitment efforts led to a final sample size of 67. Unfortunately, there were challenges in recruiting. The need to physically attend group sessions was a significant barrier to participation. A series of chi-squares and analyses of variance identified no differences between the groups at baseline.
Table I.
Sample Characteristics of Participating Families (N = 67)
| Variable [mean (SD) / n (%)] | WL (n = 22) | SSTP (n = 22) | SSTP + ACT (n = 23) |
|---|---|---|---|
| Demographics | |||
| Child age in years, mean (SD) | 5.00 (3.24) | 5.31 (2.89) | 5.35 (3.29) |
| Child gender, male | 13 (59.1) | 13 (59.1) | 17 (73.9) |
| Intellectual disability | 5 (22.7) | 3 (13.4) | 5 (21.7) |
| Learning disability | 6 (27.3) | 7 (31.8) | 6 (26.1) |
| Autism spectrum disorder | 2 (9.1) | 1 (5.9) | 1 (4.3) |
| Attention-deficit/hyperactivity disorder | 1 (4.5) | 0 | 0 |
| Vision impairment | 4 (18.2) | 3 (13.6) | 7 (33.4) |
| Hearing impairment | 1 (4.5) | 3 (13.6) | 2 (8.7) |
| Receiving services for emotional/behavioral problems | 2 (9.1) | 2 (9.5) | 4 (17.4) |
| Classification | |||
| GMFCS I | 6 (27.3) | 5 (22.7) | 4 (17.4) |
| GMFCS II | 6 (27.3) | 5 (22.7) | 7 (30.4) |
| GMFCS III | 3 (13.6) | 5 (22.7) | 4 (17.4) |
| GMFCS IV | 6 (27.3) | 5 (22.7) | 7 (30.4) |
| GMFCS V | 1 (4.5) | 2 (9.1) | 1 (4.3) |
| Relationship to child, mother (if not mother, father) | 20 (90.9) | 22 (100) | 23 (100) |
| Parent age in years, mean (SD) | 39.65 (6.09) | 38.67 (5.55) | 37.88 (9.39) |
| Parent marital status | |||
| Married | 18 (81.8) | 19 (86.4) | 14 (60.9) |
| Defacto | 0 | 1 (4.5) | 5 (21.7) |
| Separated | 1 (4.5) | 1 (4.5) | 1 (4.3) |
| Divorced | 2 (9.1) | 0 | 1 (4.3) |
| Never married/defacto | 0 | 1 (4.5) | 2 (8.7) |
| Family type | |||
| Original family | 17 (77.3) | 21 (95.5) | 17 (73.9) |
| Sole parent family | 4 (18.2) | 1 (4.5) | 3 (13.0) |
| Step family | 1 (4.5) | 0 | 3 (13.0) |
| Education level of participating parent | |||
| Less than year 10 | 0 | 0 | 0 |
| Year 10/11 | 1 (4.5) | 2 (9.1) | 3 (13.0) |
| Year 12 | 4 (18.2) | 1 (4.5) | 1 (4.3) |
| Trade/apprenticeship | 2 (9.1) | 1 (4.5) | 0 |
| TAFE/college certificate | 4 (18.2) | 5 (22.7) | 9 (39.1) |
| University degree | 11 (50.0) | 13 (59.1) | 10 (43.5) |
| Employment of participating parent | |||
| Full time | 1 (4.5) | 1 (4.5) | 5 (21.7) |
| Part time | 9 (40.9) | 13 (59.1) | 10 (43.5) |
| Unemployed (seeking work) | 1 (4.5) | 1 (4.5) | 0 |
| Full time parent/home duties | 11 (50.0) | 7 (31.8) | 8 (34.8) |
| Education level of partner (if applicable) | |||
| Less than year 10 | 0 | 0 | 1 (4.3) |
| Year 10/11 | 1 (4.5) | 4 (18.2) | 3 (13.0) |
| Year 12 | 2 (9.1) | 1 (4.5) | 2 (8.7) |
| Trade/apprenticeship | 4 (18.2) | 4 (18.2) | 3 (13.0) |
| TAFE/college certificate | 2 (9.1) | 1 (9.1) | 4 (17.4) |
| University degree | 9 (40.9) | 9 (40.9) | 6 (26.1) |
| Employment of partner (if applicable) | |||
| Full time | 16 (72.7) | 18 (81.8) | 13 (56.5) |
| Part time | 1 (4.5) | 1 (4.5) | 3 (13.0) |
| Unemployed (seeking work) | 0 | 1 (4.5) | 1 (4.3) |
| Full-time parent/home duties | 1 (4.5) | 0 | 2 (8.7) |
| Family income | |||
| <25,000 | 4 (18.2) | 2 (9.1) | 5 (21.7) |
| 25,000–50,000 | 1 (4.5) | 1 (4.5) | 3 (13.0) |
| 50,000–75,000 | 8 (36.4) | 2 (9.1) | 4 (17.4) |
| 75,000+ | 6 (36.4) | 16 (72.7) | 11 (47.8) |
| Professional advice in past 6 months from | |||
| Psychologist | 5 (22.7) | 6 (27.3) | 5 (21.7) |
| Psychiatrist | 1 (4.5) | 1 (4.5) | 3 (13.0) |
| Counselor | 6 (27.3) | 4 (18.2) | 4 (17.4) |
| Social worker | 5 (22.7) | 6 (27.3) | 3 (13.0) |
| Outcome measures at baseline, mean (SD) | |||
| PEDI Self-care | 37.94 (18.48) | 40.82 (18.60) | 35.78 (22.16) |
| PEDI Mobility | 34.00 (17.57) | 30.84 (18.20) | 31.17 (18.56) |
| PEDI Social function | 41.73 (17.08) | 43.82 (18.60) | 39.95 (17.64) |
| CP-QOL Social Well-being and acceptance | 72.66 (21.11) | 78.22 (18.46) | 77.39 (15.23) |
| CP-QOL Feelings about functioning | 60.05 (14.07) | 62.37 (22.67) | 61.09 (14.90) |
| CP-QOL Participation and physical health | 54.17 (20.15) | 56.61 (25.43) | 63.28 (12.89) |
| CP-QOL Emotional well-being and self-esteem | 71.65 (16.07) | 75.02 (18.10) | 78.02 (12.54) |
| CP-QOL Access to services | 54.12 (19.38) | 58.79 (17.63) | 60.97 (17.83) |
| CP-QOL Pain and impact of disability | 31.19 (13.57) | 36.68 (12.42) | 29.87 (11.40) |
| CP-QOL Family health | 58.19 (20.61) | 56.53 (24.34) | 56.79 (21.87) |
| Daily Tasks Checklist Problem Scale | 51.38 (17.30) | 47.31 (15.37) | 42.55 (13.52) |
| Daily Tasks Checklist Confidence Scale | 81.61 (18.57) | 82.32 (20.15) | 80.69 (21.46) |
| DASS Depression | 7.23 (8.81) | 7.77 (9.68) | 5.26 (5.30) |
| DASS Anxiety | 3.41 (3.97) | 3.37 (5.25) | 3.78 (5.03) |
| DASS Stress | 11.95 (8.46) | 11.45 (9.79) | 9.75 (6.86) |
Note. WL = wait-list control; SSTP = Stepping Stones Triple P; SSTP + ACT = Stepping Stones Triple P and Acceptance and Commitment Therapy; GMFCS = Gross Motor Functioning Classification Scale; PEDI = Pediatric Evaluation of Disability Inventory; CP-QOL = Cerebral Palsy Quality of Life (Child); DASS = Depression Anxiety Stress Scale.
Preliminary Analysis and Assumption Testing
The pattern of missing data was random with <10% missing for the primary analysis at postintervention. If <30% of items were missing for a particular participant on a specific scale, then the score was generated from the remaining items. That is, that individual’s mean for items on that scale was imputed as the missing value: a simple, intuitive, and rigorous method for handling missing data (Shrive, Stuart, Quan, & Ghali, 2006). If >30% of items were missing, then the participant was excluded from the analysis because insufficient data were obtained from that participant to estimate their mean for items on that scale. Last observation carried forward was used as a conservative sensitivity analysis to account for drop out according to intention to treat. There was significant attrition from the study at 6-month follow-up, and results of these analyses should be interpreted with caution.
The assumption of homogeneity of regression slopes was violated for the CP-QOL Social Well-being and Acceptance, CP-QOL Feelings about Functioning, CP-QOL Participation and Physical Health, CP-QOL Emotional Well-being and Self-esteem, DASS depression, DASS anxiety, and DASS stress scales. This means that there may be an interaction between the independent variable, group allocation, and the covariate, preintervention score, for these variables. Caution is required in interpretation, as the presented results may be an oversimplification of complex relationships. Original, untransformed data are reported. Sample characteristics appear in Table I.
Intervention Adherence
The interventions were delivered as per protocol in all group sessions, with the exception that in 8.19% of sessions, part of the SSTP DVD was not shown owing to technical difficulties or time management. The content on the SSTP DVD was still delivered verbally. A second therapist rated protocol delivery for 50.81% of sessions, with 100% agreement with the primary therapist. Eleven families in North Queensland received the intervention as an outreach weekend workshop format (four SSTP group, four SSTP + ACT group, three WL group). Participants in the SSTP group attended a mean of 5.31 (SD = 0.79) of the total six group sessions and a mean of 2.87 (SD = 0.34) of three phone consultations. Participants in the SSTP + ACT group attended a mean of 5.25 (SD = 0.97) of six group sessions, a mean of 2.75 (SD = 0.44) of three phone consultations, and a mean of 1.95 ACT group sessions (SD = 0.22). Every effort was attempt to arrange make up sessions when sessions were missed, with SSTP participants receiving a mean of 0.44 (SD = 0.40) SSTP make up sessions and SSTP + ACT participants receiving a mean of 0.55 (SD = 1.0) SSTP make up sessions and a mean of 0.10 (SD = 0.31) ACT make up sessions.
RCT: Comparison of Groups at Postintervention
Child Functioning
Significant differences were found at postintervention for parent-reported child functioning on the PEDI mobility scale, F(2, 53) = 3.59, p = .03. No differences were found for the PEDI self-care or social function scales. The combined parenting intervention (SSTP + ACT) showed improved child functional mobility on the PEDI (MD = −3.34, p = .016) compared with wait-list. Differences between SSTP and the combined SSTP + ACT approached significance for child functional mobility on the PEDI (MD = −2.87, p = .048) with the combined SSTP + ACT group reporting higher functional mobility. No differences were found between the SSTP alone and the WL groups.
Child Quality of Life
Consistent with an intervention effect, the three groups showed significant differences at postintervention on the CP-QOL social well-being and acceptance, F(2, 53) = 3.35, p = .04, CP-QOL feelings about functioning, F(2, 52) = 3.20, p = .05 and CP-QOL family health scales, F(2, 54) = 3.59, p = .03. All other CP-QOL subscales showed no difference. The combined Stepping Stones and ACT group showed improved child quality of life on the CP-QOL social well-being and acceptance (MD = −9.01, p = .012) and feelings about functioning domains of the CP-QOL (MD = −8.72, p = .015) in comparison with WL group. Differences approached significance for the family health domain of the CP-QOL (MD = −9.31, p = .032). Differences between SSTP and the combined SSTP + ACT groups approached significance for the family health domain of the CP-QOL (MD = −10.31, p = .022), with the combined SSTP + ACT group reporting higher quality of life at postintervention. No differences between the SSTP alone and the WL group were found.
Parental Adjustment
Significant differences were found at postintervention for the DASS depression, F(2, 53) = 3.08, p = .05, and DASS stress, F(2, 53) = 3.53, p = .03 scales. No differences were found for the DASS Anxiety scales or for the parental confidence and parental problems scales of the CP-DPTC. The combined intervention (SSTP + ACT) also showed decreased parental depressive (MD = 5.33, p = .017) and stress (MD = 5.50, p = .014) symptoms on the DASS in comparison with WL group. There were no significant differences between SSTP alone and the WL group. All ANCOVAs with linear contrasts are presented in full in Table II.
Table II.
ANCOVAs Comparing Wait-List Control, SSTP, and SSTP + ACT Groups at Postintervention With Preintervention Scores as a Covariate With Linear Contrasts
| Variable | Unadjusted postintervention Mean (SD) |
F | Partial η2 | Linear contrasts mean differences |
||||
|---|---|---|---|---|---|---|---|---|
| WL | SSTP | SSTP + ACT | WL vs. SSTP | WL vs. SSTP + ACT | SSTP vs. SSTP + ACT | |||
| PEDI Self-care | 39.23 (18.45) | 42.67 (18.86) | 39.82 (22.04) | 0.98, p = .38 | .04 | −2.33 (−5.99 to 1.34), p = .209 | −1.99 (−5.47 to 1.48), p = .256 | 0.33 (−3.25 to 3.92), p = .85 |
| PEDI Mobility | 33.27 (17.69) | 28.12 (18.96) | 32.69 (18.60) | 3.59, p = .03* | .12 | −0.56 (−3.49 to 2.37), p = .703 | −3.43 (−6.19 to −0.66), p = .016* | −2.87 (−5.71 to −0.03), p = .048 |
| PEDI Social function | 42.86 (16.94) | 45.83 (16.56) | 43.34 (17.23) | 1.65, p = .20 | .06 | −3.36 (−7.36 to 0.64), p = .098 | −0.43 (−4.16 to 3.31), p = .819 | 2.93 (−0.98 to 6.84), p = .139 |
| CP-QOL Social Well-being and acceptance | 74.49 (20.77) | 83.12 (15.16) | 85.81 (13.80) | 3.35, p = .04* | .11 | −4.79 (−12.18 to 2.60), p = .200 | −9.01 (−15.98 to −2.03), p = .012* | −4.22 (−11.40 to 2.95), p = .24 |
| CP-QOL Feelings about functioning | 63.14 (16.12) | 67.77 (20.10) | 70.91 (13.83) | 3.20, p = .05* | .11 | −5.13 (−12.42 to 2.16), p = .164 | −8.72 (−15.56 to −1.79), p = .015* | −3.59 (−10.63 to 3.44), p = .310 |
| CP-QOL Participation and physical health | 57.05 (24.47) | 63.11 (18.18) | 69.66 (14.09) | 1.88, p = 1.6 | .07 | −6.46 (−15.31 to 2.39), p = .149 | −7.80 (−16.37 to 0.76), p = .073 | −1.34 (−10.06 to 7.37), p = .758 |
| CP-QOL Emotional well-being and self-esteem | 72.24 (18.84) | 77.21 (15.99) | 81.15 (12.82) | 0.51, p = .51 | .60 | −1.98 (−9.17 to 5.21), p = .583 | −3.47 (10.38 to 3.44), p = .318 | −1.49 (−8.50 to 5.52), p = .672 |
| CP-QOL Access to services | 55.35 (17.35) | 61.82 (19.95) | 63.62 (20.77) | 0.40, p = .67 | .01 | −1.08 (−8.79 to 6.62), p = .779 | −3.19 (−10.50 to 4.11), p = .385 | −2.11 (−9.57 to 5.35), p = .572 |
| CP-QOL Pain and impact of disability | 32.63 (11.30) | 35.47 (11.04) | 31.51 (10.48) | 0.01, p = .99 | 0.00 | −0.07 (−5.90 to 5.76), p = .981 | −0.24 (−5.72 to 5.23), p = .929 | −0.18 (−5.97 to 5.62), p = .95 |
| CP-QOL Family health | 56.08 (19.80) | 54.41 (22.18) | 64.43 (19.77) | 3.59, p = .03* | .12 | 1.00 (−7.94 to 9.94), p = .823 | −9.31 (−17.79 to −0.83), p = .032 | −10.31 (−19.04 to −1.58), p = .022 |
| CP-DPTC Problem | 44.52 (14.61) | 39.16 (17.45) | 35.07 (11.31) | 0.63, p = .53 | .02 | 3.91 (−4.85 to 12.67), p = .373 | 4.65 (−4.27 to 13.58), p = .299 | 0.74 (−7.89 to 9.37), p = .863 |
| CP-DPTC Confidence | 86.12 (15.67) | 95.29 (9.82) | 90.97 (22.59) | 1.11, p = .34 | .04 | −8.91 (−20.98 to 3.16), p = .144 | −4.90 (−16.48 to 6.68), p = .399 | 4.01 (−7.58 to 15.60), p = .490 |
| DASS Depression | 7.68 (9.79) | 6.35 (9.76) | 1.95 (4.66) | 3.08, p = .05* | .10 | 2.44 (−2.13 to 7.01), p = .29 | 5.33 (1.01 to 9.65), p = .017* | 2.89 (−1.59 to 7.38), p = .20 |
| DASS Anxiety | 4.89 (7.25) | 3.88 (6.38) | 2.09 (3.79) | 2.58, p = .08 | .09 | 1.39 (−1.77 to 4.55), p = 0.38 | 3.37 (0.37 to 6.37), p = .03 | 1.98 (−1.11 to 5.07), p = .204 |
| DASS Stress | 12.00 (9.52) | 10.53 (9.39) | 5.84 (5.47) | 3.53, p = .03* | .12 | 1.43 (−3.12 to 5.98), p = .53 | 5.50 (1.18 to 9.82), p = .014* | 4.07 (−0.38 to 8.52), p = .07 |
Note. WL = wait-list control; SSTP = Stepping Stones Triple P; SSTP + ACT = Stepping Stones Triple P and Acceptance and Commitment Therapy; PEDI = Pediatric Evaluation of Disability Inventory; CP-QOL = Cerebral Palsy Quality of Life (Child); DASS = Depression Anxiety Stress Scale.
*Significant.
Sensitivity Analysis: Intention to Treat
A conservative sensitivity analysis, repeating ANCOVAs with the last observation carried forward for all families who failed to complete postintervention assessments, was conducted to satisfy the intention-to-treat analysis (N = 67). The interpretation of the results was in all cases consistent with the results above.
Retention of Effect: A Pre–Post Analysis From Postintervention to Follow-Up
Families receiving the combined SSTP + ACT reported significant improvements in functional performance on the PEDI self-care, t(10) = −3.56, p = .005, the PEDI mobility, t(10) = −2.45, p = .034, and the PEDI social functioning scales, t(10) = −1.95, p = .080. All other t tests were nonsignificant, consistent with the maintenance of gains.
Comparison of Families Receiving SSTP and SSTP + ACT at Follow-Up
Families that received the combined SSTP + ACT reported improved quality of life for CP-QOL Functioning Scale, F(2, 23) = 5.92, p = .023. These comparisons should, however, be interpreted with caution owing to lower sample size (SSTP, n = 16; SSTP + ACT, n = 12). The ANCOVAs and follow-up means are presented in full in Table III.
Table III.
Omnibus ANCOVA Comparing Families Receiving SSTP and SSTP + ACT at 6-Month Follow-Up With Preintervention Scores as a Covariate
| Variable | Unadjusted follow-up Mean (SD) |
F | Partial Eta squared | |
|---|---|---|---|---|
| SSTP | SSTP + ACT | |||
| PEDI Self-care | 40.20 (17.95) | 40.74 (22.49) | 0.00, p = .95 | .00 |
| PEDI Mobility | 32.86 (17.16) | 33.47 (18.54) | 0.03, p = .86 | .00 |
| PEDI Social function | 43.74 (16.74) | 45.39 (17.28) | 0.052, p = .82 | .00 |
| CP-QOL Social well-being and acceptance | 83.89 (12.85) | 86.42 (11.72) | 0.37, p = .055 | .02 |
| CP-QOL Feelings about functioning | 68.68 (13.29) | 72.92 (13.18) | 5.92, p = .023* | .20 |
| CP-QOL Participation and physical health | 67.19 (14.86) | 72.26 (17.74) | 3.26, p = .085 | .13 |
| CP-QOL Emotional well-being and self-esteem | 81.94 (12.59) | 86.74 (12.99) | 2.02, p = .169 | .08 |
| CP-QOL Access to services | 66.17 (17.44) | 65.36 (12.00) | 2.75, p = .111 | .11 |
| CP-QOL Pain and impact of disability | 35.58 (10.49) | 30.28 (13.14) | 0.39, p = .538 | .017 |
| CP-QOL Family health | 62.92 (15.97) | 61.08 (15.01) | 0.75, p = .39 | .03 |
| Daily Tasks Checklist Problem Scale | 40.52 (22.22) | 32.82 (13.08) | 0.39, p = .54 | .02 |
| Daily Tasks Checklist Confidence Scale | 97.88 (6.66) | 88.87 (26.68) | 1.81, p = .19 | .08 |
| DASS Depression | 2.73 (3.43) | 2.45 (3.78) | 0.01, p = .904 | .00 |
| DASS Anxiety | 1.47 (2.29) | 1.45 (3.24) | 0.11, p = .741 | .00 |
| DASS Stress | 6.35 (6.08) | 3.54 (3.75) | 2.92, p = .101 | .11 |
Note. WL = wait-list control; SSTP = Stepping Stones Triple P; SSTP + ACT = Stepping Stones Triple P and Acceptance and Commitment Therapy; PEDI = Pediatric Evaluation of Disability Inventory; CP-QOL = Cerebral Palsy Quality of Life (Child); DASS = Depression Anxiety Stress Scale.
*Significant.
Discussion
Parents receiving the combined SSTP and ACT intervention showed reductions in depressive symptoms and stress. There were no effects on parental anxiety or parental confidence or the degree to which parents found parenting tasks problematic. Given the increased risk of parents of children with CP for depressive symptoms (Barlow et al., 2006; Lach et al., 2009) and stress (Parkes et al., 2011), this is an important result. Further, it is consistent with existing research demonstrating benefits of ACT for parental adjustment in families of children with ASD and ABI (Blackledge & Hayes, 2006; Brown et al., 2015).
The combined intervention, SSTP combined with ACT, was associated with improved parent-reported child functional performance, in the mobility domain. There were no effects on self-care or social function. As child functional performance was measured by parent report, it is impossible to know if gains were truly made in child functional performance or if the intervention merely changed parental perceptions. Future research is necessary to confirm. Increased parental flexibility and parenting skills may have promoted child functional performance by increasing adherence to home programs, increasing family participation in physical activities or by improved parental encouragement for child physical exploration. Additional research should investigate whether ACT-based family interventions can be effectively incorporated into family-centered care, supporting existing interventions such as home therapy programs (Novak et al., 2009) and environmental enrichment (Morgan, Novak, & Badawi, 2013).
To our knowledge, this is also the first study to demonstrate an effect of a parenting intervention, SSTP combined with ACT, on quality of life. This result is consistent with the finding that parenting style predicts child quality of life in children with CP (Aran et al., 2007) as with the vast literature demonstrating links between family and child well-being (Newland, 2015). Further, it reinforces the family-centered care philosophy, in demonstrating the impact of a family intervention on child quality of life (Novak & Cusick, 2006; Novak et al., 2009; Rosenbaum et al., 1998). Child quality of life emerges from the complex interplay between child-specific factors and the wider context of the family. Within this study, the parent-report CP-QOL was used owing to child age. Further research should confirm findings for child-reported quality of life. ACT interventions delivered dyadically, to both parent and child, may be an effective means of targeting child and parent quality of life.
Coupled with the primary outcomes data (removed for blinded review), this study demonstrates further support for the combination of SSTP and ACT with families of children with CP. SSTP alone effectively targeted behavioral and emotional problems in children with CP, with the combination of Stepping Stones and ACT effectively targeting behavioral problems, hyperactivity, dysfunctional parenting, child functioning, child quality of life, and parental adjustment. This is the first RCT to demonstrate the efficacy of a parenting intervention for families of children with CP and the first to demonstrate the additive benefits of ACT.
Clinical Implications
This study suggests that parenting intervention should be integrated into routine care for children with CP and their families. Further, clinicians providing parenting intervention should consider the addition of ACT. SSTP is a widely disseminated parenting intervention and training in ACT is also readily available to clinicians worldwide.
Study Limitations and Future Research
The present study has several limitations. It is unknown whether the intervention effect of the combined SSTP and ACT intervention is a result of ACT alone, a result of the combination of SSTP and ACT or simply a result of additional intervention time. All of the assessments in this study were parent report, and hence, it is unclear if the intervention changed child functioning and quality of life or merely altered parental perception of child functioning and quality of life. Further research should confirm the present findings using child-reported quality-of-life measures as well as blinded clinician assessments of functional outcomes. In addition, the small sample size, particularly at 6-month follow-up, should be acknowledged, and the results on the CP-QOL child and the DASS should be interpreted with caution owing to violation of the assumption of homogeneity of regression slopes. The results presented in this study may oversimplify more complex relationships for parental adjustment and child quality of life in the areas of well-being and acceptance and feelings about functioning. The findings regarding child functioning in the domain of mobility and child quality of life in the domain of family health are not affected by this need for caution. Further research is required to confirm the effects found in this article.
Conclusion
This RCT demonstrates the efficacy of a parenting intervention, SSTP combined with ACT, in improving child functional performance and quality of life as well as parental adjustment. In conjunction with the child behavioral and parental style outcomes already reported from this study (removed for blinded review), this article demonstrates an additive benefit of ACT above and beyond established parenting interventions. This clinical trial reinforces the value of an ACT parenting intervention approach in enhancing parent and child outcomes for families of children with CP.
Funding
This work was supported by a National Health and Medical Research Council postdoctoral fellowship (631712 to K.W.), a National Health and Medical Research Council Career Development Fellowship (1037220 to R.B.), and a Smart State Fellowship (R.B.).
Conflict of interest: Stepping Stones Triple P is owned by the University of Queensland and sublicensed to Uniquest the University of Queensland’s Technology Transfer Company. Professor Sanders is a coauthor of the Stepping Stones Triple P program and receives royalty payments from the publisher Triple P International in accordance with the University of Queensland Intellectual Property Policy.
Clinical trial registration: Australian New Zealand Clinical Trials Registry (00336291).
References
- Albrecht G. L., Devlieger P. J. (1999). The disability paradox: High quality of life against all odds. Social Science and Medicine, 48, 977–988. [DOI] [PubMed] [Google Scholar]
- Aran A., Shalev R. S., Biran G., Gross-Tsur V. (2007). Parenting style impacts on quality of life in children with cerebral palsy. The Journal of Pediatrics, 151, 56–60. [DOI] [PubMed] [Google Scholar]
- Arnaud C., White-Koning M., Michelsen S. I., Parkes J., Parkinson K., Thyen U., Beckung E., Dickinson H. O., Fauconnier J., Marcelli M., McManus V., Colver A. (2008). Parent-reported quality of life of children with cerebral palsy in Europe. Pediatrics, 121, 54–64. [DOI] [PubMed] [Google Scholar]
- Barlow J. H., Cullen-Powell L. A., Cheshire A. (2006). Psychological well-being among mothers of children with cerebral palsy. Early Child Development and Care, 176, 421–428. [Google Scholar]
- Blackledge J. T., Hayes S. C. (2006). Using acceptance and commitment training in the support of parents of children diagnosed with autism. Child and Family Behavior Therapy, 28(1), 1–18. [Google Scholar]
- Brown F. L., Whittingham K., Boyd R., McKinlay L., Sofronoff K. (2015). Does Stepping Stones Triple P plus Acceptance and Commitment Therapy improve parent, couple, and family adjustment following pediatric acquired brain injury? A randomised controlled trial. Behaviour Research and Therapy, 73, 58–66. [DOI] [PubMed] [Google Scholar]
- Colver A. (2009). Quality of life and participation. Developmental Medicine and Child Neurology, 51, 656–659. [DOI] [PubMed] [Google Scholar]
- Coyne L. W., McHugh L., Martinez E. R. (2011). Acceptance and Commitment Therapy (ACT): Advances and applications with children, adolescents and families. Child and Adolescent Psychiatric Clinics of North America, 20, 379–399. [DOI] [PubMed] [Google Scholar]
- Dickinson H. O., Parkinson K. N., Ravens-Sieberer U., Schirripa G., Thyen U., Arnaud C., Beckung E., Fauconnier J., McManus V., Michelsen S. I., Parkes J., Colver A. F. (2007). Self-reported quality of life of 8-12 year old children with cerebral palsy: A cross-sectional European study. Lancet, 369, 2171–2178. [DOI] [PubMed] [Google Scholar]
- Haley S. M., Coster W. J., Ludlow L. H., Haltiwanger J. T., Andrellos P. J. (1992).Pediatric Evaluation of Disability Inventory: Standardization and administration manual. Boston, MA: Trustee of Boston University. [Google Scholar]
- Hayes S. C., Strosal K. D., Wilson K. G. (2003). Acceptance and Commitment Therapy: An experiential approach to behavior change. New York, NY: Guilford Press. [Google Scholar]
- Lach L. M., Kohen D. E., Garner R. E., Brehaut J. C., Miller A. R., Klassen A. F., Rosenbaum P. L. (2009). The health and psychosocial functioning of caregivers of children with neurodevelopmental disorders. Disability and Rehabilitation, 31, 607–618. [DOI] [PubMed] [Google Scholar]
- Lovibond P. E., Lovibond S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behavior Research and Therapy, 33, 335–343. [DOI] [PubMed] [Google Scholar]
- Morgan C., Novak I., Badawi N. (2013). Enriched environments and motor outcomes in cerebral palsy: Systematic review and meta-analysis. Pediatrics, 132, e735–e746. [DOI] [PubMed] [Google Scholar]
- Newland L. A. (2015). Family well-being, parenting, and child well-being: Pathways to health adjustment. Clinical Psychologist, 19, 3–14. [Google Scholar]
- Novak I., Cusick A. (2006). Home programs in paediatrics occupational therapy for children with Cerebral Palsy: Where to start? Australian Occupational Therapy Journal, 53, 251–264. [Google Scholar]
- Novak I., Cusick A., Lannin N. (2009). Occupational therapy home programs for Cerebral Palsy: Double-blind, randomised, controlled trial. Pediatrics, 124, 606–614. [DOI] [PubMed] [Google Scholar]
- Novak I., Hines M., Goldsmith S., Barclay R. (2012). Clinical prognostic messages from a systematic review on cerebral palsy. Pediatrics, 130, 1285–1312. doi: 10.1542/peds.2012-0924 [DOI] [PubMed] [Google Scholar]
- Palisano R. (1997). Development & reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine Child Neurology, 39, 214–223. [DOI] [PubMed] [Google Scholar]
- Parkes J., Caravale B., Marcelli M., Franco F., Colver A. (2011). Parenting stress and children with cerebral palsy: A European cross-sectional survey. Developmental Medicine and Child Neurology, 53, 815–821. doi: 10.1111/j.1469-8749.2011.04014.x [DOI] [PubMed] [Google Scholar]
- Roberts C., Mazzucchelli T., Studman L., Sanders M. R. (2006). Behavioural family intervention for children with developmental disabilities and behavioural problems. Journal of Clinical Child and Adolescent Psychology, 35, 180–193. doi: 10.1207/s15374424jccp3502_2 [DOI] [PubMed] [Google Scholar]
- Rosenbaum P., King S., Law M., King G., Evans J. (1998). Family-centred service: A conceptual framework and research review. Physical and Occupational Therapy in Pediatrics, 18 (1), 1–20. [Google Scholar]
- Rosenbaum P., Paneth N., Leviton A., Goldstein M., Bax M. (2007). Definition and classification of cerebral palsy. Developmental Medicine and Child Neurology, 49 (Suppl 109), 8–14. [PubMed] [Google Scholar]
- Sanders M. R., Mazzucchelli T., Studman L. (2003). Practitioner's manual for standard Stepping Stones Triple P. Brisbane: Triple P International. [DOI] [PubMed] [Google Scholar]
- Sanders M. R., Mazzucchelli T. G., Studman L. J. (2009). Facilitator's manual for Group Stepping Stones Triple P for families with a child who has a disability. Brisbane: Triple P International. [DOI] [PubMed] [Google Scholar]
- Sawyer M. G., Bittman M., La Greca A. M., Crettenden A. D., Borojevic N., Raghavendra P., Russo R. (2011). Time demands of caring for children with cerebral palsy: What are the implications for maternal mental health? Developmental Medicine and Child Neurology, 52, 338–343. [DOI] [PubMed] [Google Scholar]
- Shrive F. M., Stuart H., Quan H., Ghali W. A. (2006). Dealing with missing data in a multi-question depression scale: a comparison of imputation methods. BMC Medical Research Methodology 13(6), 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley F., Blair E., Alberman E. (2000). Cerebral palsies: Epidemiology and causal pathways. Clinics in Developmental Medicine No. 151. London: MacKeith Press. [PMC free article] [PubMed] [Google Scholar]
- Waters E., Davies E., Mackinnon A., Boyd R., Graham H. K., Kai Lo S., Wolfe R., Stevenson R., Bjornson K., Blair E., Hoare P., Ravens-Sieberer U., Reddihough D. (2007). Psychometric properties of the quality of life questionnaire for children with Cerebral Palsy. Developmental Medicine and Child Neurology, 49, 49–55 [DOI] [PubMed] [Google Scholar]
- Whittingham K., Sofronoff K., Sheffield J. K., Sanders M. (2009). Stepping Stones Triple P: An RCT of a parenting program with parents of a child diagnosed with an autism spectrum disorder. Journal of Abnormal Child Psychology, 37, 469–480. doi: 10.1007/s10802-008-9285-x [DOI] [PubMed] [Google Scholar]
- Whittingham K., Wee D., Sanders M., Boyd R. N. (2013a). Sorrow, coping and resiliency: Parents of children with cerebral palsy share their experiences. Disability and Rehabilitation , 35, 1447–1452. [DOI] [PubMed] [Google Scholar]
- Whittingham K., Wee D., Sanders M., Boyd R. N. (2013b). Predictors of psychological adjustment, experienced parenting burden and chronic sorrow symptoms in parents of children with cerebral palsy. Child: Care, Health and Development, 39, 366–373. [DOI] [PubMed] [Google Scholar]
- Zekovic B., Renwick R. (2003). Quality of life for children with adolescents with developmental disabilities: Review of conceptual and methodological issues relevant to public policy. Disability and Society, 18, 19–34. [Google Scholar]