Abstract
Objectives This study aimed to examine the applicability of the Social-ecological Model of Adolescent and Young Adult Readiness to Transition (SMART) model for adolescents and young adults (AYA) with sickle-cell disease (SCD). Methods 14 AYA with SCD (14–24 years old) and 10 clinical experts (6–20 years of experience) completed semi-structured interviews. AYA completed brief questionnaires. Interviews were coded for themes, which were reviewed to determine their fit within the SMART model. Results Overall, most themes were consistent with the model (e.g., sociodemographics/culture, neurocognition/IQ, etc.). Factors related to race/culture, pain management, health-care navigation skills, societal stigma, and lack of awareness about SCD were salient for AYA with SCD. Conclusions Findings suggest the SMART model may be appropriate in SCD with the consideration of disease-related stigma. This study is a step toward developing a disease-specific model of transition readiness for SCD. Future directions include the development of a measure of transition readiness for this population.
Keywords: adolescents, qualitative methods, sickle-cell disease
Owing to advances in medical care, a larger proportion of children with chronic illnesses are living past age 18 and must transfer from pediatric to adult care (American Academy of Pediatrics, 2002). Although this transfer from one health-care team to another represents a discrete event, the transition process is dynamic and should involve a planned and purposeful transfer of chronically ill adolescents and young adults (AYA) from pediatric to adult care (Schwartz, Tuchman, Hobbie, & Ginsberg, 2011). It is recommended that the timing of this health care transition be based on AYA’s developmental readiness, knowledge and skills related to illness management, and understanding of the adult health-care system (Reiss, Gibson, & Walker, 2005). Patients’ knowledge and skills regarding illness management are often referred to as transition readiness. However, recent research has led to a broader description of the construct that includes multiple social and ecological systems (Schwartz et al., 2011, 2013). In their description of the Social-ecological Model of Adolescent and Young Adult Readiness to Transition (SMART), which was developed as a conceptual framework for pediatric cancer patients, Schwartz et al. (2013) acknowledge the roles of family, peers, and health-care providers when defining transition readiness. They describe it as “indicators that patients and those in their support system can begin, continue, and finish the transition process from child-centered to adult-oriented health care, through the event of transfer” (p. 940).
The present study seeks to examine the applicability of the SMART model in the sickle-cell disease (SCD) population. The issue of transitioning is particularly salient for AYA with SCD (Hauser & Dorn, 1999), as certain characteristics of SCD are likely to differentially impact transition readiness. SCD is the most commonly inherited blood disorder in the United States and primarily affects individuals of African descent. Approximately 1 in 500 African American children are born with SCD (Kaye et al., 2006), and between 70,000 and 100,000 individuals in the United States currently have the disorder (DeBaun & Telfair, 2012). Within the past 40 years, improvements in care have increased average life expectancy in SCD from 14 to 50 years old (Claster & Vichinsky, 2003). However, survival into adulthood presents numerous health problems including predisposition to infections, lung and cardiac issues, stroke, vaso-occlusive crises (VOC), as well as psychosocial considerations such as self-care, coping, and readiness for autonomy (Telfair, Ehiri, Loosier, & Baskin, 2004).
Unlike other chronic illness populations, a disproportionate number of individuals with SCD are racial minorities (DeBaun & Telfair, 2012). This racial disparity could contribute to discriminatory experiences and health-related stigma associated with SCD (Jenerette & Brewer, 2010). Moreover, pain, due to VOC, is a distinguishing feature of the disorder (Barakat, Patterson, Daniel, & Dampier, 2008). Exposure to pain since childhood often contributes to patient self-knowledge regarding specific pain medications and dosages that are effective (Reiss et al., 2005), which may lead health-care providers unfamiliar with the disease to perceive individuals with SCD as drug-seeking (Elander, Lusher, Bevan, & Telfer, 2003).
Another unique aspect of SCD that might impact transition is the high rate of neurocognitive impairment due to silent or overt strokes (Hulbert et al., 2011). Declines in cognitive functioning appear to increase with age among individuals with SCD (Schatz, Finke, Kellett, & Kramer, 2002) and may be particularly relevant when considering transition readiness in this population. AYA with SCD may also be at an increased risk of poor educational achievement regardless of stroke as a result of frequent school absences related to medical complications (e.g., VOC; DeBaun & Telfair, 2012). Low educational attainment, in addition to cognitive deficits secondary to stroke, may create a discrepancy between patients’ chronological age and cognitive functioning (DeBaun & Telfair, 2012), disputing the use of age as an indicator of transition readiness (Reiss et al., 2005) particularly among this population.
The unique transition experiences of AYA with SCD may warrant consideration to accurately assess transition readiness and improve outcomes in adulthood for this population. Currently, AYA with SCD are at an increased risk of death following transfer owing to various reasons including a disruption in medical care (Jenerette & Brewer, 2010). Although the literature has identified several barriers to a successful transition for AYA with SCD, including deficient information regarding the transition process, fear of leaving familiar health-care providers and being treated as an adult, and concerns about the cost of treatment and adult providers understanding SCD and its treatment (Telfair et al., 2004), factors impacting transition readiness for this population have yet to be specified. Moreover, a universal measure of transition readiness for AYA with SCD has yet to be developed and routinely administered in clinical practice. In fact, the lack of a developmentally appropriate assessment tool to evaluate transition readiness has been cited as one of the reasons that gaps in transition support have persisted (Cooley & Sagerman, 2011; Schwartz et al., 2011). Without such an instrument, pertinent areas that may impede upon these patients’ successful transition cannot be identified readily or addressed accordingly. Although the Sickle-Cell Transfer Questionnaire (SCTQ; Telfair, Myers, & Drezner, 1994; Telfair et al., 2004) was developed to assess transition readiness in AYA with SCD, it was created from several expert opinion checklists rather than empirically derived, it has an open-ended questionnaire format with no available norms, and its psychometric properties have not been reported in the literature.
The Patient-Reported Outcomes Measurement Information System (PROMIS) was developed by the National Institutes of Health to improve the dynamic assessment of patient-reported health outcomes (Cella et al., 2007). PROMIS is a system of highly reliable, precise child- and adult-reported measures of health and well-being. It was not only designed to facilitate treatment planning and improve communication between patients and providers about managing chronic illness, but also to create a set of standards for instrument development and validation (see www.nihpromis.org for more information). These standards consist of a unique mixed-methods approach initially involving a qualitative design to define the target domain and construct an item bank, and then quantitative methods aimed at psychometric evaluation (National Institutes of Health, 2012). The PROMIS standards have been described as an ideal tool for advancing the assessment of child-reported health (Forrest et al., 2012), including transition outcomes (Pierce & Wysocki, 2015), and may be particularly applicable to the development of a transition readiness measure for SCD.
A conceptual model to guide the development of a transition readiness measure for SCD is currently absent from the literature. Schwartz et al. (2011) note that the “lack of theoretical models of transition readiness has hindered efforts to advance research and clinical practice related to transition” (p. 891). Moreover, the first PROMIS standard requires defining the target concept and developing a conceptual model by reviewing the extant literature and incorporating the input of patients, clinicians, content and measurement experts, as well as end-users and stakeholders using sound qualitative methods. Additionally, a conceptual model could assist clinicians and researchers in determining risk and protective factors associated with transition readiness for SCD and facilitate the identification of potential targets for intervention.
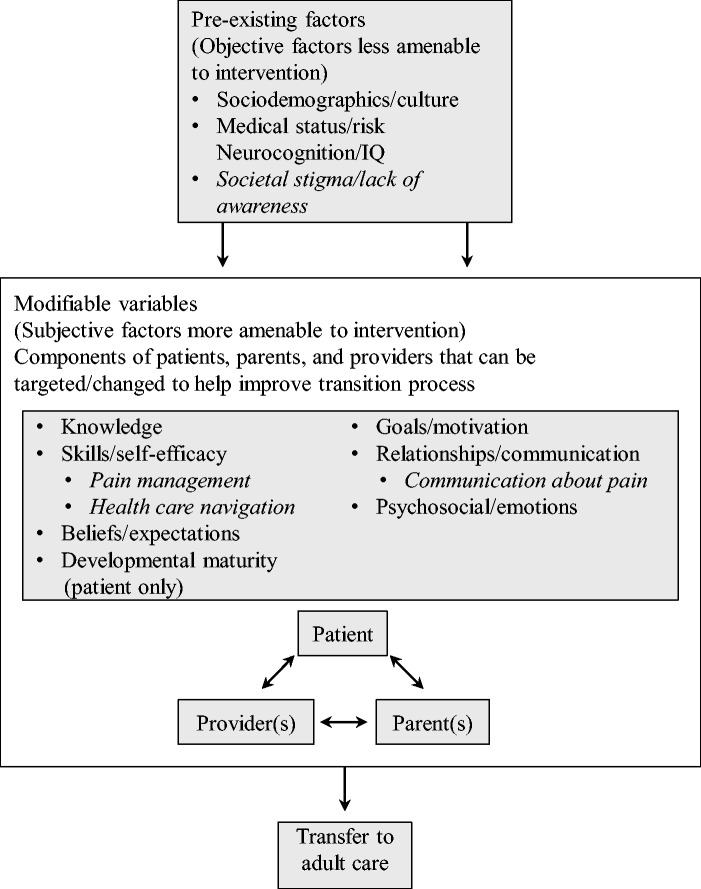
The SMART model (Schwartz et al., 2011, 2013) conceptualizes transition from a social-ecological perspective, including multiple stakeholders (e.g., patients, parents, and providers) with preexisting objective factors less amenable to intervention (e.g., access/insurance, medical status/risk, etc.) and subjective factors (e.g., knowledge, skills/self-efficacy, etc.) that may be modifiable with intervention in a clinic setting. Although factors in this model appear to capture the construct of transition readiness adequately among the pediatric cancer population, the SMART model requires validation in other chronic illness groups (Schwartz et al., 2013).
Consistent with the first PROMIS standard, the objective of the present study is to utilize a qualitative design to identify factors influencing transition readiness among AYA with SCD from the perspectives of multiple stakeholders in the transition process. Findings from interviews with AYA and clinical experts in the present study are considered within the framework of the SMART model to inform the model’s applicability to the SCD population.
Method
Participants
Participants were recruited from two outpatient clinics (a pediatric hematology clinic and an adult SCD clinic) within a large southeastern medical center. Study inclusion criteria for AYA with SCD are described for adolescent participants and young adults participants: (1) confirmed SCD diagnosis (all AYA participants), (2) aged 13–17 (for adolescents) or 18–25 (for young adults), (3) living with at least one caregiver (for adolescents) or transitioned in the past five years (for young adults), and (4) fluent in English (all AYA participants). The sole exclusion criterion for all AYA with SCD was the presence of cognitive or psychological impairment that would affect participation in an individual interview. A total of 19 eligible participants with SCD (10 adolescents, nine young adults) were recruited for participation. One adolescent and two young adults with SCD could not be reached by phone to schedule a meeting time; one adolescent and one adult did not show up for their scheduled interviews.
Inclusion criteria for clinical experts were: (1) a licensed medical professional or member of the Foundation for Sickle-Cell Disease Research (FSCDR) and (2) at least five years of experience caring for individuals with SCD or studying transition in this population. Twelve eligible clinical expert participants from across the United States were identified using purposive, snowball sampling methods. Clinical experts were initially identified based on the authors’ knowledge of their research or clinical work or their participation in the FSCDR. Then, expert participants recommended additional clinical experts who met eligibility criteria to participate. Among these recommendations, authors invited experts with varying areas of expertise (e.g., pediatric vs. adult, clinical care vs. research) and from varying geographic locations (e.g., Northeastern United States, Western United States, etc.). Two clinical experts did not respond to the recruitment email. Thus, analyses were based on a final sample of 14 (74%) AYA with SCD (eight adolescents, six young adults) and 10 (83%) clinical experts.
Procedure
All study procedures were approved by the institutional review boards of the relevant institutions. Invitation letters were distributed by nursing staff to eligible AYA patients in the pediatric and adult clinics. Interested participants returned the letter to nursing staff with contact information, and they were contacted to schedule a meeting where (1) informed consent and assent were obtained, (2) brief questionnaires were administered (a demographic questionnaire to all AYA participants, and a transition-related questionnaire to adolescents; see Measures), and (3) a semi-structured interview (approximately 30 minutes) was conducted. In an effort to increase adolescents’ openness and honesty during the discussion, parents left the room after providing consent. The first author and two research assistants who had no prior relationship with participants conducted the interviews in the pediatric and adult clinics. Although attempts were made to conduct interviews in a private conference room away from exam rooms, the majority of participants (n = 11) were interviewed before or shortly after medical appointments for participant convenience. AYA participants’ medical records were reviewed to obtain the following descriptive information: hemoglobin genotype and complications resulting from SCD (e.g., incidence of stroke, number of hospitalizations in the past six months; see Table I).
Table I.
Adolescent and Young Adult Participants’ Characteristics
| Variable | Adolescents (n = 8) | Adults (n = 6) |
|---|---|---|
| M (SD) or n (%) | M (SD) or n (%) | |
| Age (in years) | 15.86 (1.13) | 20.67 (2.81) |
| Sex – female | 6 (75%) | 5 (83.33%) |
| Race/Ethnicity | ||
| African American (AA) | 5 (62.50%) | 5 (83.33%) |
| Caribbean/Black | 2 (25%) | 1 (16.67%) |
| Hispanic | 1 (12.50%) | – |
| Highest grade completed (in years) | 10.38 (1.30) | 12.83 (0.98) |
| Marital status – single | – | 6 (100%) |
| Caregiver(s) in the home – one | 5 (62.50%) | – |
| Public health insurance | 7 (87.50%) | 5 (83.33%) |
| Receiving SSI/SSDI | 5 (62.50%) | 4 (66.67%) |
| Living below federal poverty level | 3 (37.50%) | 4 (66.67%) |
| Time since transfer (in years) | – | 2.26 (2.02) |
| Genotype | ||
| SS | 4 (50%) | 4 (66.67%) |
| SC | 2 (25%) | 2 (33.33%) |
| S/β Th | 2 (25%) | – |
| Complications from SCD | ||
| Splenectomy | 2 (25%) | 4 (66.67%) |
| Cholecystectomy | 3 (37.50 %) | 2 (33.33%) |
| Bone infarction | 1 (12.50%) | – |
| Silent/overt stroke | – | 1 (16.67%) |
| Number of hospitalizations in past six months | 0.63 (0.74) | 2.50 (1.38) |
Note. SSI = supplemental security income; SSDI = social security disability insurance.
For clinical expert participants, invitation emails were sent with the written informed consent forms attached. Interested clinical experts returned a signed consent form via email and indicated their availability to complete a 30-minute, semi-structured interview either by phone (nine clinical experts) or in-person (one clinical expert). During the interview, participants answered brief demographic questions and were asked to provide recommendations and contact information for additional clinical experts eligible to participate in the study.
Interviews
The first author and two research assistants conducted all interviews. Interview questions were modeled after those described by Hauser and Dorn (1999) and Valenzuela et al. (2011) and were aimed at determining factors impacting transition outcomes specifically for individuals with SCD. All questions were open-ended to avoid bias and to allow participants to describe their views and experiences from their own perspective. Example interview questions include: (1) “What are some things you think would be important to know in order to have a good transition? How would knowing these things be helpful?” (Asked to adolescents); (2) “Do you think your transition was successful or unsuccessful? Why or why not? What would a successful transition be like? What would an unsuccessful transition be like?” (Asked to young adults); and (3) “What do you think are some unique challenges for patients with sickle cell preparing to transition to adult care? What about after they have already transitioned?” (Asked to clinical experts). Follow-up questions were asked to clarify responses. Each interview was audio-recorded with participant consent and transcribed for the purpose of data analysis. Interviewers made field notes and identified transition readiness topics discussed by participants.
Measures
The following measures were administered to obtain descriptive information or to determine the trustworthiness of the data.
Demographic and Health Status Questionnaire
All participants completed this brief questionnaire; adolescents completed it with parental assistance. Items assessed participant age, sex, race, education, employment status, young adults’ marital status or number of caregivers with whom adolescents resided, health complications due to SCD, type of health-care insurance, and receipt of supplemental security income or social security disability insurance. To estimate the number of participants living at or below the federal poverty level (FPL), participants provided the number and ages of individuals living in the home as well as the family’s gross annual income.
Sickle-Cell Transfer Questionnaire
The SCTQ is a self-report measure with nine domains that assesses transition readiness among patients with SCD and their feelings about a transition program (Telfair et al., 1994, 2004). It was developed from several opinion checklists, allows for both closed- and open-ended responses to items, and was initially designed for clinical use. Adolescents completed two domains of the SCTQ for the purpose of triangulating SCTQ responses with interview responses: (1) “concerns about transition” (e.g., Do you any have concerns about what it will be like going from a children and adolescent medical care program to an adult care program? If you have concerns, what are they?); and (2) “feelings about moving to an adult care program” (e.g., What do you think will be some of your feelings when told that you will be transferring to an adult treatment program?). Response options vary from dichotomous “yes” or “no” responses to qualitative responses (e.g., I have concerns about being treated as an adult; I will be nervous, etc.). The psychometric properties of the SCTQ have not been reported in the literature.
Data Analysis
Data were systematically analyzed with ATLAS.ti software (Scientific Software Development GmbH, 2011) using the thematic analysis procedure outlined by Braun and Clark (2006). Units of analysis were subject and predicate clauses in interview transcriptions. Data analysis began with reviewing transcripts, followed by coding for emerging concepts and themes consistent with participant responses and transition readiness as defined in the SMART model (Schwartz et al., 2013). All data were coded independently by the first author and a research assistant. The coding process involved creating a list of codes derived from the data (e.g., “challenging experiences in the ER”) and developing a standard definition for each code. Segments of interview transcriptions determined to be relevant based on the transition literature were reduced to brief phrases or sentences and coded using the ATLAS.ti software (Scientific Software Development GmbH, 2011). Codes were subsequently organized into logical categories (e.g., “patient and provider relationships”) and, finally, broader themes (e.g., “relationships”). Emerging themes from each interview were checked iteratively against all other interviews until the point of saturation (i.e., the final interview in each participant group did not contribute any new codes or themes). Themes were then examined for overall trends, patterns, and relationships and subsequently compared with factors in the SMART model (e.g., “relationships/communication”). Coding disagreements were resolved collaboratively through an iterative process until both coders agreed on all codes assigned. Two instances in which a resolution could not be obtained resulted in those particular phrases being left uncoded owing to the ambiguity of the topic being discussed.
Representative quotations of emerging themes were taken from participants’ transcriptions and are presented in the Results. For the purpose of clarity and to facilitate comprehension, filler words such as “um, uh, and ah,” stock phrases like “you know,” and stuttering or unnecessary repetitions were edited out of the transcription. Otherwise, quotations were kept intact and may have included slang, incorrect grammar, and colloquialisms.
Trustworthiness
Internal validity (i.e., credibility) of qualitative interviews was examined by triangulating (Guion, Diehl, & McDonald, 2011) adolescents’ responses to interview questions with responses to the SCTQ. Adolescents’ responses on the SCTQ were compared with their corresponding interview transcript and subjectively rated on a five-point Likert scale for congruence by the first author, where a numerical rating of 1 indicated that no SCTQ responses were discussed in interview transcripts, a rating of 2 indicated that few (i.e., less than half) SCTQ responses were discussed, a rating of 3 indicated that some (i.e., approximately half) SCTQ responses were discussed, a rating of 4 indicated that most (i.e., more than half) SCTQ responses were discussed, and a rating of 5 indicated that all SCTQ responses were discussed in interview transcripts. Seven adolescents were rated as a 4 on this scale, and one was rated as a 3. Interview responses from adolescents, young adults, and clinical experts were also compared. Similarities and differences in themes discussed by each subset of the sample are reported in the Results.
Results
Participant Characteristics
The mean age for the adolescent group was 15.86 years (range: 14–17 years) and for the young adult group was 20.67 years (range: 18–24 years). Females comprised the majority of the sample. Almost all AYA participants identified as Black or African American, and more than half had the hemoglobin SS genotype. The mean number of years since young adults transferred to adult providers was 2.26 years (range two months to five years). Table I includes additional details regarding AYA participants’ characteristics. Clinical expert participants were primarily female (80%), 50% African American, 50% Caucasian, and consisted of pediatric psychologists (n = 3), physicians (n = 4; 2 pediatric hematologists, 2 adult hematologists), clinical researchers (n = 2), and one registered nurse. Seventy percent were located in the Southeast, 20% in the Northeast, and 10% on West Coast. The sample’s mean years of experience working with the SCD population or in transition were 14.60 years (range: 6–20 years).
Themes
A total of 10 broad themes emerged (see Data Analysis for details on how themes were derived). Themes are reported within the SMART framework of objective and subjective factors (Schwartz et al., 2013) when possible. Figure 1 depicts the adapted SMART model for SCD. Themes specific to SCD that were identified in the present study and resulted in a modification of the original SMART model are italicized (Figure 1). Four themes fit into the preexisting objective factors category: (1) sociodemographics/culture, (2) stigma and lack of awareness, (3) medical status/risk and neurocognition/IQ, and (4) health-care system and policies. Six themes fit into the modifiable subjective factors category: (1) relationships/communication, (2) knowledge, (3) skills/self-efficacy, (4) developmental maturity, (5) psychosocial/emotions and goals/motivation, and (6) beliefs/expectations. Several sub-themes also emerged within each broad theme.
Figure 1.
Social-ecological Model of Adolescent and Young Adult Readiness to Transition (SMART) adapted for sickle-cell disease (SCD). Note. Italicized components are disease-specific considerations for transition readiness in SCD.
Preexisting Objective Factors
Sociodemographics/Culture
Half of the clinical experts (n = 5) stated that developmental milestones such as attending college, obtaining employment, and starting romantic relationships interfered with transition readiness for AYA. One physician explained, “There’s all these other things that are transitioning at the same time so it’s a really uncertain time anyway and I think that background makes it almost impossible for kids to be successful in transitioning [to adult care]” (Pediatric hematologist, nine years of experience with the SCD population). One adolescent and one young adult also discussed the influence of developmental milestones (e.g., attending college, obtaining employment) on the transition process. Nearly half of the clinical experts (n = 4) discussed the potential influence of socioeconomic status and related factors (e.g., adequate housing, financial stability, and transportation) as well as patients’ ethnic minority status (n = 5) on transition readiness. One physician observed, “[SCD is] largely one ethnic group and that ethnic group already deals with inherent biases and attitudes, so that’s one struggle” (Adult hematologist, 20 years of experience with SCD).
Stigma and Lack of Awareness
Clinical experts were more likely than other participants (n = 9; 5 clinical experts, 2 adolescents, 2 adults) to report that stigma and lack of community awareness regarding SCD were unique challenges for building relationships with adult providers and acquiring support during transition. One physician provided this example of SCD stigma:
If an asthma patient comes in and says, “I think I probably need back to back nebs and 10 mg of prednisone,” everyone would be like, “Wow, I’m so impressed. You know your disease so well.” Whereas, if a sickle cell patient comes in and says, “I think I need 2 mg of Dilaudid,” they’re gonna say, “Oh, you’re a drug-seeker” (Pediatric hematologist, eight years of experience with the SCD population).
Clinical experts also noted that AYA’s desire to be “like everybody else” and not discuss their illness contributes to the “invisibility” of the disease and perpetuates a lack of community awareness about SCD. As a result, AYA may experience more difficulty accessing social support to cope with their illness and the transition to adult care.
Medical Status/Risk and Neurocognition/IQ
Several participants (n = 6; 1 adolescent, 2 adults, 3 clinical experts) discussed challenges related to the progression of the disease, including health complications and the variability and unpredictability of symptoms as factors affecting transition in SCD (n = 5; 2 adolescents, 2 adults, 1 expert).
Only clinical experts discussed illness severity (n = 4) and cognitive deficits (n = 8) as necessary considerations for transition readiness. When asked to recall cases with less than optimal transition outcomes, clinical experts (n = 4) described patients with greater illness severity who had the SS hemoglobin genotype, complications related to their illness (e.g., endocrine issues and priapism), and were receiving regular blood transfusions. Half (n = 4) of those who mentioned cognitive functioning indicated that cognitive deficits may go unrecognized and hinder AYA’s ability to develop the skills needed to transition successfully. One pediatric psychologist indicated, “There isn’t any cognitive assessment once [AYA] get on the adult side. Since we know our patients are at risk, we need to do a better job assessing and incorporating these results into the transition plan and after [transfer]” (Pediatric psychologist, six years of experience with SCD). The nurse in our sample discussed the impact of cognitive impairment due to stroke on transition readiness, “We have a couple of kids that [are] gonna be physically transitioned, but I don’t know that they’ll ever be mentally ready to transition” (Registered nurse, 18 years of experience with the SCD population). Only one researcher reported a connection between race and cognitive ability in the transition readiness of patients with SCD, “This is a group of kids [where] there is evidence of impaired cognitive development secondary to anemia, and it probably doesn’t show, because these kids are African American and people might not [have] the best expectations [of] them” (Transition researcher, 15 years of experience).
Health-Care System and Policies
All clinical experts (n = 10) but no AYA discussed how the health-care environment affects transition readiness. Flexibility in scheduling appointments and the transfer of care based on AYA’s needs (n = 5) was reported to improve transition outcomes, whereas public health insurance and reimbursement challenges (n = 6) and policies restricting prescription of narcotic medication (n = 3) were described as hindering transition success. Specifically, one researcher commented on how policies related to “dispensing narcotics,” which are the “best and most acceptable medicine” for patients with SCD, can contribute to the “disparity” in health outcomes.
Modifiable Subjective Factors
Relationships/Communication
Patient–Provider Relationships
Patient–provider relationships were discussed by all participants (N = 24) as relevant to transition but were mentioned more frequently by AYA (i.e., coded M = 12.6 times per AYA interview; coded M = 3.0 times per clinical expert interview). All AYA (n = 14) described a strong attachment to their pediatric team. One adolescent equated transitioning to “moving away from your parents.” Two adolescents (n = 2) expressed that the support from pediatric providers who often reminded them to engage in health behaviors (e.g., take medications, eat healthily, exercise) was helpful, but adults (n = 6) and clinical experts (n = 4) noted that this support fosters reliance on pediatric providers. For example, four young adults recalled feeling “babied” by their pediatric providers.
In contrast to the close relationships with pediatric providers, almost all young adults (n = 5) described challenging relationships with adult providers. More specifically, challenges related to provider empathy and understanding (n = 5), being treated like an individual (n = 4), and feeling heard and respected (n = 5) were reported. One young adult explained, “When we try to tell them what works for [our] body, like, ‘You’re supposed to let my arm hang when [drawing] blood because the veins pop up more,’ I’ll get comments like, ‘Who has the RN, me or you?’” (21-year-old female, three years post-transition). Many adolescents (n = 6) discussed concerns about communicating with adult providers, but only two clinical experts discussed the potential for communication issues between AYA and adult providers.
The majority of young adults (n = 4) and half of the clinical experts (n = 5) described problems during transition due to adult providers’ misperception of pain. For example, young adult participants discussed times when they were perceived as “faking” their pain. Communication with adult emergency room (ER) providers when seeking pain treatment was reported to be particularly challenging (n = 8; 4 young adults, 4 clinical experts). Young adults participants often felt discounted and misunderstood by these providers. In contrast, only two adolescents reported worrying about providers not believing them when they were in pain, and none expressed concerns about seeking treatment in the ER.
Social-Emotional Support
Nearly all participants (n = 23; 8 adolescents, 5 young adults, 10 experts) discussed the importance of social and emotional support in facilitating the transition to adult care. One adolescent shared that support from friends who had already transitioned would provide her “footsteps” to follow during her own transition. Family support was described by clinical experts (n = 10) as providing “everything” needed for transition success. Clinical experts (n = 5) specifically voiced a need for parents to be prepared for “their role” in transition (i.e., how to foster patient autonomy without completely withdrawing support).
Pediatric and Adult Provider Relationships
The majority of clinical experts (n = 9), one adolescent, and one young adult (n = 11) emphasized the importance of facilitating continuity of care through “collaboration” between pediatric and adult care providers. One clinical expert shared, “We need to work [on] providers talking to each other about the patient. [Like,] ‘Ms. X has this problem. This works best for her, this does not work. If you have any questions, here is my number’” (Adult hematologist, 20 years of experience with the SCD population).
Knowledge
Many participants indicated patient knowledge about SCD (n = 16; 4 adolescents, 4 young adults, 8 clinical experts) and their personal medical history (n = 15; 5 adolescents, 3 young adults, 7 clinical experts) were necessary for a successful transition. One adolescent reported that SCD-related knowledge can improve self-management and transition readiness because it “makes you understand [doing] certain things have consequences.” Clinical experts discussed how AYA’s knowledge about SCD complications (e.g., stroke) might increase adherence and “health maintenance” behaviors (e.g., routine magnetic resonance imaging [MRI] scans) resulting in positive health outcomes post-transition.
Skills/Self-Efficacy
Most participants (n = 18; 6 adolescents, 3 young adults, 9 clinical experts) emphasized the need for AYA to assume responsibility for disease management before transition. The importance of managing temperature changes (6 adolescents, 2 clinical experts), maintaining proper nutrition (3 adolescents, 1 young adult, 1 clinical expert), and managing stress (2 adolescents, 1 young adult, 1 clinical expert) to prevent pain crises were predominantly discussed by adolescents. Young adults (n = 2) reported having to improve self-care skills related to preventing infection (e.g., “sanitizing” their hands regularly) post-transition. Clinical experts (n = 7) focused on attendance at appointments and medication adherence when considering self-management skills to facilitate transition.
Pain Management Skills
Most participants reported that managing SCD pain influences the transition process (n = 19; 6 adolescents, 6 adults, 7 clinical experts). AYA (n = 9; 5 adolescents, 4 adults) described utilizing several home pain management strategies (e.g., taking over-the-counter pain relievers, using heating pads, etc.) with limited or variable effectiveness and going to the ER when their pain was unbearable. This pattern can lead to an overutilization of ER services (Yusuf, Atrash, Grosse, Parker, & Grant, 2010), which may impact transition outcomes. In addition, young adults (n = 2) reported feeling that they had “grown a tolerance for pain,” and adolescents (n = 6) discussed minimizing their symptoms when at school or around peers to prevent “drawing attention” to themselves.
Health-Care Navigation Skills
All clinical experts, three adolescents and four young adults (n = 17) discussed the importance of health-care navigation skills in transitioning to adult care. Skills such as obtaining and maintaining health insurance coverage (n = 11; 2 adolescents, 3 adults, 6 clinical experts), scheduling clinic appointments (n = 6; 1 adult, 5 clinical experts), and ordering medications (n = 5; 1 adolescent; 4 clinical experts) were communicated as essential to transition success. One young adult observed, “There’s a lot of people who lost their insurance. They search for physicians, but sometimes they’re not covered anymore and they don’t know where to go or what to do” (18-year-old female, two months post-transition).
Developmental Maturity
The importance of developmental maturity was discussed by several participants (n = 10; 3 adolescents, 2 adults, 5 clinical experts). All adolescents (n = 8) said they believed that they would be ready to transition at age 18, but clinical experts expressed that self-management tasks should be tailored to patients’ developmental level so patients can gradually acquire skills necessary for managing SCD and transition to adult care. Only one young adult and one clinical expert specifically discussed challenges with using chronological age as an indicator of transition readiness.
Psychosocial/Emotions and Goals/Motivation
The majority of clinical experts (n = 8) discussed the relationship between psychosocial factors and transition outcomes. Specifically, patients with attributes such as adaptive emotional functioning (i.e., adequate coping, absence of psychopathology, positive outlook about the future, and motivation; n = 6), who are proactive (n = 6), and have life goals (n = 4) were reported to have better transition outcomes. Intergenerational family functioning was also discussed by clinical experts (n = 4) who indicated that patients from “fractured families” (e.g., single-parent households, those with parental involvement with the law) may have more difficulties transitioning even if their SCD symptoms are less severe.
Beliefs/Expectations
Many AYA (5 adolescents, 5 young adults) and one clinical expert (n = 11) indicated an understanding of the transition process and beliefs/expectations about the adult care system are important factors for transition. Most young adults recalled having an abrupt transition (n = 4), and nearly all (n = 5) reported a mismatch between their beliefs/expectations and the reality of adult care. They described being “thrown into the adult world” where “it’s either sink or swim,” which was far from the supportive environment they had expected. The majority of participants (n = 15; 5 adolescents, 5 young adults, 5 clinical experts) noted that becoming familiar with adult providers would assist AYA in developing appropriate beliefs and expectations about transition. The majority of clinical experts (n = 9), three adolescents, and three young adults (n = 15) discussed that a plan or curriculum could foster appropriate beliefs about transition and clarify adult providers’ expectations.
Discussion
This study utilized qualitative data from AYA with SCD and clinical experts in the field of transition and SCD to examine the applicability of the SMART model of transition readiness (Schwartz et al., 2013) to the SCD population. Themes from interviews were mostly consistent with factors within the SMART theoretical framework. Themes related to relationships/communication, knowledge, developmental maturity, and beliefs/expectations were similar to existing factors in the SMART model, whereas themes surrounding sociodemographics/culture, medical status/risk, neurocognition/IQ, and skills/self-efficacy were described as being particularly salient for SCD and included unique sub-themes such as disease-related stigma, the effects of “silent” strokes, pain management, and health-care navigation skills. Themes related to psychosocial/emotions and goals/motivation were discussed concurrently by participants, and there was no evidence that these themes were considered two separate constructs as in the original SMART model.
All participants agreed that the following factors influenced the transition process for AYA with SCD: (1) aspects of the disease itself (i.e., progression over time, variability and unpredictability of symptoms); (2) the stigma associated with SCD and lack of community awareness about the disease; (3) relationships/communication between patients, providers, parents, and others; (4) disease-related knowledge, (5) self-management skills including pain management and health-care navigation skills; (6) patients’ developmental maturity and psychosocial functioning including their goals/motivation; and (7) patients’ beliefs/expectations about transition. These themes are consistent with the SCD transition literature (Telfair et al., 1994, 2004; Hauser & Dorn, 1999; McPherson, Thaniel, & Minniti, 2009; Treadwell, Telfair, Gibson, Johnson, & Osunkwo, 2011; DeBaun & Telfair, 2012) as well as transition research in other pediatric chronic illness groups (Geenen, Powers, & Sells, 2003; Reiss et al., 2005; Russell, Reinbold, & Maltby, 1996; Valenzuela et al., 2011). Therefore, these factors are potentially useful for pediatric psychologists to consider when assessing transition readiness in AYA with SCD. Modifiable factors (e.g., relationships/communication with providers) can be targeted by pediatric psychologists through interventions aimed at enhancing patients’ skills as well as the health-care and home environment necessary for transition success.
Some differences emerged in AYA and clinical experts’ views of factors influencing transition readiness. Whereas AYA more commonly reported concerns about relationships with adult providers that may be more amenable to intervention, clinical experts tended to focus on less modifiable factors such as patients’ cognitive functioning, sociodemographic variables, and the health-care system and policies. This discrepancy supports the use of multiple informants when assessing transition readiness. AYA may be better able to provide insight into aspects of provider relationships that can affect the transition process including communication, trust, and empathy. Clinical experts, such as pediatric psychologists and other health-care providers, may be more adept at detecting the impact of factors such as medical status and cognitive ability and may be more aware of systems-level factors influencing transition readiness.
Study findings indicate that the SMART model may be applicable to the SCD population and also suggest specific ways to tailor the model’s constructs to patients with SCD, their providers, and support systems. First, as described by study participants, the stigma attached to the disease (e.g., patients being viewed as drug-seeking) and lack of community awareness (i.e., “invisibility” of the disease) appear to be unique challenges influencing transition for the SCD population. Because sociocultural issues such as racial stereotyping and discrimination may exacerbate disease-related stigma (Jenerette & Brewer, 2010), these can be categorized as preexisting objective factors (i.e., less amenable to intervention). Nonetheless, pediatric psychologists can advocate for SCD patients and educate providers about SCD and its treatment, the psychological experience of pain, and signs of substance addiction versus attempts to manage pain (Elander et al., 2003), given their expertise in these areas. Additionally, pediatric psychologists can implement psychological interventions aimed at building AYA’s self-advocacy (Jordan, Swerdlow, & Coates, 2013) and self-efficacy skills (Clay & Telfair, 2007), which, in turn, could increase involvement from patients and their families in promoting community awareness and understanding about SCD. These combined efforts from pediatric psychologists, patients, and families may ultimately change perceptions of the disease and affected individuals in ways that improve patients’ experience transitioning to adult care.
Second, findings suggest that pain management and communication are also unique considerations influencing transition readiness in AYA with SCD. As VOC are a distinguishing feature of SCD (Barakat et al., 2008), skills for adequately managing pain symptoms could facilitate transition success (McPherson et al., 2009). Pediatric psychologists can assist these patients in developing effective behavioral pain management skills through cognitive-behavioral interventions such as relaxation training and modifying pain-related cognitions (Chen, Cole, & Kato, 2004). Assertiveness training may be appropriate for enhancing AYA’s communication skills (Jenerette & Murdaugh, 2008). Nevertheless, owing to the racial disparity among individuals with SCD, this population may be at an increased risk for empathy–race bias in the assessment and treatment of pain (Tait & Chibnall, 2014). They may also be more likely to receive poorer quality pain treatment (Drwecki, Moore, Ward, & Prkachin, 2011), which could exacerbate pain management issues and, consequently, impact self-management and transition readiness. For example, if AYA with SCD have negative experiences with pain relief in the ER owing to bias or other issues, they may actively avoid seeking treatment for pain in the future (Booker, Blethyn, Wright, & Greenfield, 2006). Delaying pain treatment could increase these patients’ risk for serious and possibly fatal complications (Ballas, 2005). Study participants described pain management as a prominent issue affecting transition readiness. However, pain-related concerns are poorly understood and understudied, particularly with respect to their interaction with race (Green et al., 2003). Given the unique combination of pain symptoms and racial minority status in SCD, psychologists working with this population are encouraged to conduct additional research to further examine the interrelation between these constructs. Such endeavors may assist in determining ways of reducing these potential biases and health disparities among individuals with SCD.
Third, while the SMART framework includes a focus on neurocognition, participants in our study indicated that these issues are especially salient for AYA with SCD. Clinical experts in the present study reported that neurocognitive challenges might be left unidentified in patients with SCD and discussed the following reasons: a lack of observable symptoms in silent infarcts, inadequate neuropsychological screening to identify impairment, and limited research on the cognitive impact of SCD. There is evidence that diffuse brain injury undetectable through MRI may occur among this population and is more likely with increasing age (Schatz et al., 2002; Steen et al., 2006). Cognitive impairment in SCD may also result from the indirect effects of social and environmental disadvantage (Schatz et al., 2002), which may be common among patients with SCD. Therefore, it is critical that pediatric psychologists routinely assess these patients’ cognitive abilities to aid in effective transition planning. Causal mechanisms underlying cognitive deficits in SCD remain unclear (Schatz et al., 2002), thus, neurocognition may be less amenable to intervention in this population and categorized as a preexisting objective factor.
Finally, study findings suggest that health-care navigation skills are an essential part of transition readiness for AYA with SCD. Skills for acquiring and retaining adequate insurance coverage and preventative health care could reduce the high frequency of ER visits in patients with SCD (Yusuf et al., 2010) and may improve their health service utilization and transition outcomes. Pediatric psychologists can effectively target health-care navigation skills as part of behavioral and educational interventions at home or in the clinic aimed at improving self-management. More specifically, these clinicians can enhance patient knowledge, problem-solving skills, and feelings of self-efficacy (Sawyer, Drew, Yeo, & Britto, 2007).
Although this study gathered rich information about transition readiness from AYA with SCD and clinical experts working with this understudied population, several limitations should be noted. The study’s small convenience sample of AYA consisted of mostly female participants and individuals without a history of stroke. Therefore, it may not be representative of the larger SCD population. More adults than adolescents lived below the FPL, preventing equal comparisons between these groups. Young adults who were lost to care following transfer had no way of enrolling in the present study, so those who experienced the least successful transition did not provide input for consideration. The majority of clinical experts were physicians and psychologists from southeastern metropolitan areas. Thus, our sample may not be representative of providers from all disciplines who may be involved in transition (e.g., social work), or those working in geographic regions where resources, transition planning, and characteristics of the SCD population (e.g., prevalence, culture) may be different. Finally, the perspectives of parents and caregivers were not included in the present study. Given the importance of family support discussed by study participants, future research should examine the input of parents and caregivers to further assess the applicability of the SMART model for SCD.
This study represents the first step in validating components of the SMART model for AYA with SCD. Future research is needed to continue this work by developing a clinically useful measure of transition readiness for AYA with SCD. The PROMIS framework for measure development was used to guide this study’s design and has been cited as having “the potential [for] enhancing collaborative science in pediatric psychology and facilitating advances in multidimensional measurement of child health” (Drotar, 2012, p. 613). Findings from the present study can be used by pediatric psychologists to develop and refine individual assessment items, which can then be analyzed within the PROMIS framework through item pool analysis techniques and cognitive interviewing. Understanding the applicability of the SMART model in the SCD population also allows clinicians and researchers to develop targets for intervention during this challenging period for AYA with SCD. For example, future research should examine the extent to which resources and support for neurocognitive impairments in SCD improve transition success. More research is also needed to understand caregivers’ and family systems’ influence on transition in this population. Ongoing research using larger, representative samples will be needed to evaluate the clinical utility of the SMART model in conceptualizing transition readiness for AYA with SCD.
Findings from the present study provide data that improve our understanding of factors influencing transition among AYA with SCD and help to establish a conceptual model of transition readiness for this population. Findings also underscore the importance of considering transition readiness in SCD from a social-ecological framework, like the SMART model, given the influence of patients, parents, and clinical experts on factors such as societal stigma and health-care policies, as well as the integral role of family and peers on transition outcomes. While previous transition research has often focused on individual-level skills and behaviors (e.g., adherence), our findings emphasize the need to improve health-care systems and policies (e.g., physician training to reduce biases, adapt ER policies to assist with pain management, administer routine screenings to detect cognitive impairment) as well. Pediatric psychologists can help to address these and other factors impacting SCD patients’ transition readiness through targeted interventions such as behavioral pain management and assertiveness training, neurocognitive and psychosocial assessment, provider education, patient advocacy, and additional research. These efforts may reduce the risk of early mortality following transfer for AYA with SCD (Jenerette & Brewer, 2010) and improve transition outcomes in this population.
Conflicts of interest: None declared.
References
- American Academy of Pediatrics (2002). A consensus statement on health care transitions for young adults with special health care needs. Pediatrics, 110(6Pt. 2), 1304–1306. [PubMed] [Google Scholar]
- Ballas S. K. (2005). Pain management of sickle cell disease. Hematology/Oncology Clinics of North America, 19, 785–802. [DOI] [PubMed] [Google Scholar]
- Barakat L. P., Patterson C. A., Daniel L. C., Dampier C. (2008). Quality of life among adolescents with sickle cell disease: Mediation of pain by internalizing symptoms and parenting stress. Health and Quality of Life Outcomes, 6, 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booker M. J., Blethyn K. L., Wright C. J., Greenfield S. M. (2006). Pain management in sickle cell disease. Chronic Illness, 2, 39–50. [DOI] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. [Google Scholar]
- Cella D., Yount S., Rothrock N., Gershon R., Cook K., Reeve B., Ader D., Fries J. F., Bruce B., Rose M. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Medical Care, 45(Suppl. 1), S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E., Cole S. W., Kato P. M. (2004). A review of empirically supported psychosocial interventions for pain and adherence outcomes in sickle cell disease. Journal of Pediatric Psychology, 29, 197–209. [DOI] [PubMed] [Google Scholar]
- Claster S., Vichinsky E. P. (2003). Managing sickle cell disease. BMJ , 327, 1151–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clay O. J., Telfair J. (2007). Evaluation of a disease-specific self-efficacy instrument in adolescents with sickle cell disease and its relationship to adjustment. Child Neuropsychology, 13, 188–203. [DOI] [PubMed] [Google Scholar]
- Cooley W. C., Sagerman P. J. (2011). Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics, 128, 182–200. [DOI] [PubMed] [Google Scholar]
- DeBaun M. R., Telfair J. (2012). Transition and sickle cell disease. Pediatrics, 130, 926–935. [DOI] [PubMed] [Google Scholar]
- Drotar D. (2012). Introduction to commentary: Exploiting opportunities created by the Patient-reported measurement information system in pediatric psychology. Journal of Pediatric Psychology, 37, 612–613. [DOI] [PubMed] [Google Scholar]
- Drwecki B. B., Moore C. F., Ward S. E., Prkachin K. M. (2011). Reducing racial disparities in pain treatment: The role of empathy and perspective-taking. Pain, 152, 1001–1006. [DOI] [PubMed] [Google Scholar]
- Elander J., Lusher J., Bevan D., Telfer P. (2003). Pain management and symptoms of substance dependence among patients with sickle cell disease. Social Science and Medicine, 57, 1683–1696. [DOI] [PubMed] [Google Scholar]
- Forrest C. B., Bevans K. B., Tucker C., Riley A. W., Ravens-Sieberer U., Gardner W., Pajer K. (2012). Commentary: The patient-reported outcome measurement information system (PROMIS) for children and youth: Application to pediatric psychology. Journal of Pediatric Psychology, 37, 614–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geenen S. J., Powers L. E., Sells W. (2003). Understanding the role of health care providers during the transition of adolescents with disabilities and special health care needs. The Journal of Adolescent Health, 32, 225–233. [DOI] [PubMed] [Google Scholar]
- Green C. R., Anderson K. O., Baker T. A., Campbell L. C., Decker S., Fillingim R. B., Kalauokalani D. A., Lasch K. E., Myers C., Tait R. C., Todd K. H., Vallerand A. H. (2003). The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain Medicine, 4, 277–294. [DOI] [PubMed] [Google Scholar]
- Guion L. A., Diehl D. C., McDonald D. (2011). Triangulation: Establishing the validity of qualitative studies. University of Florida: IFAS Extension. Retrieved from http://edis.ifas.ufl.edu/fy394 [Google Scholar]
- Hauser E. S., Dorn L. (1999). Transitioning adolescents with sickle cell disease to adult-centered care. Pediatric Nursing, 25, 479–488. [PubMed] [Google Scholar]
- Hulbert M. L., McKinstry R. C., Lacey J. L., Moran C. J., Panepinto J. A., Thompson A. A., Sarnaik S. A., Woods G. M., Casella J. F., Inusa B., Howard J., Kirkham F. J., Anie K. A., Mullin J. E., Ichord R., Noetzel M., Yan Y., Rodeghier M., DeBaun M. R. (2011). Silent cerebral infarcts occur despite regular blood transfusion therapy after first strokes in children with sickle cell disease. Blood, 117, 772–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenerette C. M., Brewer C. (2010). Health-related stigma in young adults with sickle cell disease. Journal of the National Medical Association, 102, 1050–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenerette C. M., Murdaugh C. (2008). Testing the theory of self‐care management for sickle cell disease. Research in Nursing & Health, 31, 355–369. [DOI] [PubMed] [Google Scholar]
- Jordan L., Swerdlow P., Coates T. D. (2013). Systematic review of transition from adolescent to adult care in patients with sickle cell disease. Journal of Pediatric Hematology/Oncology, 35, 165–169. [DOI] [PubMed] [Google Scholar]
- Kaye C. I., Committee on Genetics, Accurso F., La Franchi S., Lane P. A., Hope N., Sonya P., Bradley S., Michele A. L. (2006). Newborn screening fact sheets. Pediatrics, 118, 934–963. [DOI] [PubMed] [Google Scholar]
- McPherson M., Thaniel L., Minniti C. P. (2009). Transition of patients with sickle cell disease from pediatric to adult care: Assessing patient readiness. Pediatric Blood & Cancer, 52, 838–841. [DOI] [PubMed] [Google Scholar]
- Pierce J. S., Wysocki T. (2015). Topical review: Advancing research on the transition to adult care for Type 1 Diabetes. Journal of Pediatric Psychology, 40, 1041–1047. [DOI] [PubMed] [Google Scholar]
- PROMIS Validity Standards Committee on behalf of the PROMIS Network of Investigators. National Institutes of Health. (2012). PROMIS instrument development and psychometric evaluation: Scientific standards [PowerPoint slides]. Retrieved from http://www.nihpromis.org/science/methodology [Google Scholar]
- Reiss J. G., Gibson R. W., Walker L. R. (2005). Health care transition: Youth, family, and provider perspectives. Pediatrics, 115, 112–120. [DOI] [PubMed] [Google Scholar]
- Russell M. T., Reinbold J., Maltby H. J. (1996). Transferring to adult health care: Experiences of adolescents with cystic fibrosis. Journal of Pediatric Nursing, 11, 262–268. [DOI] [PubMed] [Google Scholar]
- Sawyer S. M., Drew S., Yeo M. S., Britto M. T. (2007). Adolescents with a chronic condition: Challenges living, challenges treating. The Lancet, 369, 1481–1489. [DOI] [PubMed] [Google Scholar]
- Schatz J., Finke R. L., Kellett J. M., Kramer J. H. (2002). Cognitive functioning in children with sickle cell disease: A meta-analysis. Journal of Pediatric Psychology, 27, 739–748. [DOI] [PubMed] [Google Scholar]
- Schwartz L. A., Brumley L. D., Tuchman L. K., Barakat L. P., Hobbie W. L., Ginsberg J. P., Daniel L. C., Kazak A. E., Bevans K., Deatrick J. A. (2013). Stakeholder validation of a model of readiness for transition to adult care. JAMA Pediatrics, 167, 939–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz L. A., Tuchman L. K., Hobbie W. L., Ginsberg J. P. (2011). A social‐ecological model of readiness for transition to adult‐oriented care for adolescents and young adults with chronic health conditions. Child: Care, Health and Development, 37, 883–895. [DOI] [PubMed] [Google Scholar]
- Scientific Software Development GmbH. (2011). ATLAS.ti (Version 5.2) [Computer Software]. [Google Scholar]
- Steen R. G., Fineberg-Buchner C., Hankins G., Weiss L., Prifitera A., Mulhern R. K. (2005). Cognitive deficits in children with sickle cell disease. Journal of Child Neurology, 20, 102–107. [DOI] [PubMed] [Google Scholar]
- Tait R. C., Chibnall J. T. (2014). Racial/ethnic disparities in the assessment and treatment of pain: Psychosocial perspectives. American Psychologist, 69, 131–141. [DOI] [PubMed] [Google Scholar]
- Telfair J., Ehiri J. Ε., Loosier P. S., Baskin M. L. (2004). Transition to adult care for adolescents with sickle cell disease: Results of a national survey. International Journal of Adolescent Medicine and Health, 16, 47–64. [DOI] [PubMed] [Google Scholar]
- Telfair J., Myers J., Drezner S. (1994). Transfer as a component of the transition of adolescents with sickle cell disease to adult care: Adolescent, adult, and parent perspectives. Journal of Adolescent Health, 15, 558–565. [DOI] [PubMed] [Google Scholar]
- Treadwell M., Telfair J., Gibson R. W., Johnson S., Osunkwo I. (2011). Transition from pediatric to adult care in sickle cell disease: Establishing evidence‐based practice and directions for research. American Journal of Hematology, 86, 116–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenzuela J. M., Buchanan C. L., Radcliffe J., Ambrose C., Hawkins L. A., Tanney M., Rudy B. J. (2011). Transition to adult services among behaviorally infected adolescents with HIV – a qualitative study. Journal of Pediatric Psychology, 36, 134–140. [DOI] [PubMed] [Google Scholar]
- Yusuf H. R., Atrash H. K., Grosse S. D., Parker C. S., Grant A. M. (2010). Emergency department visits made by patients with sickle cell disease: A descriptive study, 1999–2007. American Journal of Preventive Medicine, 38, S536–S541. [DOI] [PMC free article] [PubMed] [Google Scholar]