Abstract
Objectives:
This study sought to assess the effects of length and inclination of implants on stress distribution in an implant and terminal abutment teeth in an implant assisted-removable partial denture (RPD) using three-dimensional (3D) finite element analysis (FEA).
Materials and Methods:
In this in vitro study, a 3D finite element model of a partially dentate mandible with a distal extension RPD (DERPD) and dental implants was designed to analyze stress distribution in bone around terminal abutment teeth (first premolar) and implants with different lengths (7 and 10 mm) and angles (0°, 10° and 15°).
Results:
Stress in the periodontal ligament (PDL) of the first premolar teeth ranged between 0.133 MPa in 10mm implants with 15° angle and 0.248 MPa in 7mm implants with 0° angle. The minimum stress was noted in implants with 10mm length with 0° angle (19.33 MPa) while maximum stress (25.78 MPa) was found in implants with 10mm length and 15° angle. In implants with 7 mm length, with an increase in implant angle, the stress on implants gradually increased. In implants with 10 mm length, increasing the implant angle gradually increased the stress on implants.
Conclusion:
Not only the length of implant but also the angle of implantation are important to minimize stress on implants. The results showed that vertical implant placement results in lower stress on implants and by increasing the angle, distribution of stress gradually increases.
Keywords: Dental Implants, Single-Tooth; Dental Stress Analysis; Finite Element Analysis
INTRODUCTION
Distal extension base removable partial denture has always been associated with several problems including low stability and retention as well as poor esthetics and function [ 1 – 5 ]. The difference in displacement between the mucosa and the PDL of terminal abutment was estimated to be up to 25 times [ 6 – 8 ].
Consequently, when functional pressure is applied to the distal extension base removable partial denture, the resultant forces cause damage to the abutment teeth [ 9 ].
It has been proven that osseointegrated implant-borne removable prostheses are successful in partially edentulous patients with severely resorbed ridges and patients with periodontally compromised remaining teeth. Implant placement can increase tooth longevity by distribution of forces to the implant and decreasing the stresses placed on the remaining teeth using implant-assisted prostheses [ 10 ].
Placement of osseointegrated implants beneath distal extension denture base of prostheses results in stable and durable occlusion and improved function [ 11 ]. In addition, the implant is able to protect the remaining natural teeth from overloading, deterioration and bone loss and restore facial skeletal structure [ 12 ]. Despite the high success rate of DERPDs, their failure rate has also been notable [ 12 ].
The success of a dental implant depends on a variety of factors including the design of the abutment and technique by which the abutment screw is placed into the implant. Providing an insufficient biomechanical bond between the implant and the surrounding jawbone or implant fixtures can cause abutment failure [ 13 ]. Besides, implant might be identified as a foreign body by the surrounding tissues and trigger undesirable biological stress responses in the jawbone, which can also lead to implant failure [ 13 ]. Other important factors affecting the distribution of stresses within the surrounding jawbone include implant length and diameter [ 14 ]. Not all patients have sufficient bone height in the posterior region, either because of bone resorption resulting from tooth loss, or anatomical limitations; in such cases, shorter implants may be efficient [ 15 ]. Some observations have emphasized on the role of determining the optimum length and diameter of implants that would best dissipate stresses [ 16 – 18 ]. However, some others did not find any difference in distribution of stress different implant lengths and bicortical anchorage [ 16 – 18 ]. In this regard, future research directions are recommended with particular emphasis on the stress evaluation and its association with geometric parameters of implants. Some authors have found that load applied to the long axis of implant causes better stress distribution; others found that some degrees of implant inclination might not be very harmful after all [ 19 , 20 ].
In some cases, FEA may serve as a unique method to find answers for biomechanical problems. The usefulness of FEA in designing and analyzing dental restorations has been documented [ 21 – 25 ]. Because of the lack of studies on the effect of length and inclination of implants on stress distribution in implant– assisted RPDs, the present study aimed to assess the effects of length and angle of implants on stress distribution in implant– assisted RPDs using 3D-FEA.
MATERIALS AND METHODS
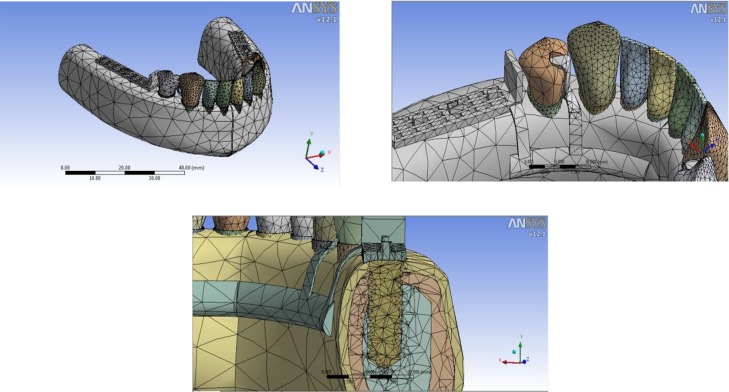
In this in vitro study, 3D-FEA was used. Six models were designed of a partially edentulous mandible with anterior teeth (Fig. 1). Each model contained gingiva, cortical bone (= 1 mm thick), spongy bone and the central incisor to first premolar teeth in both sides of the arch with their PDLs having a uniform thickness of 0.25 mm. The model also included a RPD to replace posterior teeth and an implant inserted in distal extension area. In the models with an implant, a healing abutment compatible with the implant diameter was placed, with a height of 2 mm in all models.
Fig. 1.
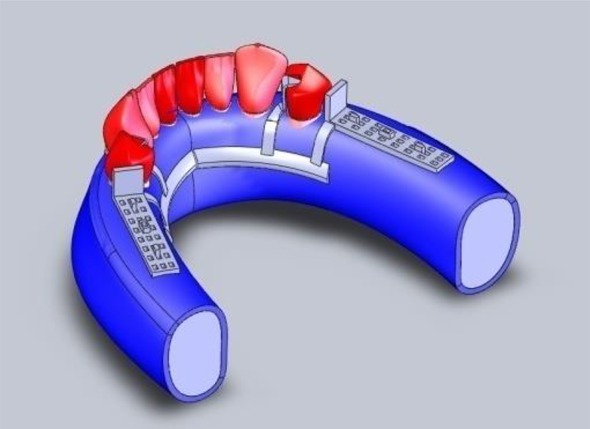
Mandibular model whit implant and RPD.
The models were similar except for the length and inclination of the implant. Diameter of implant was 4 mm in all models and the implant was inserted in the first molar area [ 26 ]. In the models A, B and C, length of implant was 10 mm and angle of implant was 0°, 10° and 15°, respectively. In the models D, E and F, length of implant was 7 mm and angle of implant was 0°, 10°, 15°, respectively (Table 1).
Table 1.
Configuration of the models made for the study. All models representing a mandibular section, with all structures standardized.
| A | Presence of teeth with RPD and associated implant with 10 mm length at 0° angle |
| B | Presence of teeth with RPD and associated implant with 10 mm length at 10° angle |
| C | Presence of teeth with RPD and associated implant with 10 mm length at 15° angle |
| D | Presence of teeth with RPD and associated implant with 7 mm length at 0° angle |
| E | Presence of teeth with RPD and associated implant with 7 mm length at 10° angle |
| F | Presence of teeth with RPD and associated implant with 7 mm length at 15° angle |
The implant inclination was simulated lingually in all models. The partial denture saddle extended to the second molar area with a distal guiding plane in the first premolar and a mesial rest. The major connector was designed as lingual bar [ 27 ] (Fig. 1).
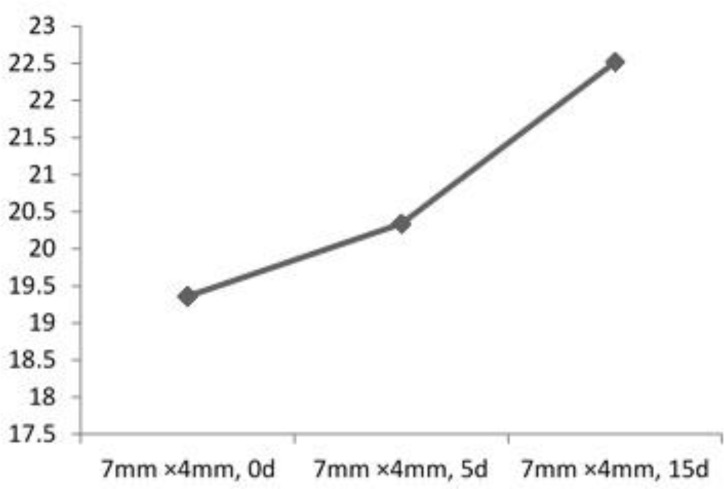
SolidWorks 2006 software (SolidWorks, MA, USA) was selected for the modeling phase. The models were designed in a top-to-bottom manner. The next phase was to transfer the models for calculation to the ANSYS Workbench ver. 11.0 software (ANSYS Inc., PA, USA). All the vital tissues were presumed elastic, homogeneous and isotropic. The corresponding elastic properties such as the Young’s modulus and Poisson’s ratio were determined according to recent researches [ 28 – 31 ] (Table 2). The elastic modulus and Poisson’s ratio of the materials were defined. Models were meshed with 138,895 nodes and 71,866 elements (Fig. 2).
Fig. 2.
Finite element mesh
As boundary condition, all nodes at the distal part of the models and the lower part of the symphysis were restrained so that all rigid body motions were prevented. The models created were exported to the finite element program to generate the finite element meshes. After that, the next step was to incorporate the mechanical properties of each structure and apply loads. This would allow vertical movement of DERPD on the mucosa resulting in reconstruction of changes in the underlying cortical and spongy bone. Load was applied to the cusp tips of natural and artificial teeth in all models.
Load of 50 N was applied, fractioned into five application points of 10N on each cusp point in a strictly vertical direction. Finally, a stress map was designed for each model and stress distribution was evaluated.
RESULTS
The index of stress distribution (Von Mises stress) in the two conditions of premolar PDL and implants in the different models is presented in Table 3. In the PDL of first premolar, the stress ranged between 0.133 MPa in 10mm implant with the angle of 15° and 0.248 MPa in 7mm implant with the angle of 0°. In the implant, the stress ranged between 19.33 MPa in 10mm implant with the angle of 0° and 25.78 MPa in 10mm implant with the angle of 15°.
Table 3.
Increase of stress on implant in line with the increase of implant angle
| Length of implant ( mm) | Angle of implant | Stress on implant (MPa) | Stress on premolar PDL (MPa) |
|---|---|---|---|
| 7 | 0 | 19.36 | 0.2487 |
| 7 | 10 | 20.34 | 0.2444 |
| 7 | 15 | 22.52 | 0.1408 |
| 10 | 0 | 19.33 | 0.1680 |
| 10 | 10 | 22.81 | 0.1776 |
| 10 | 15 | 25.78 | 0.1330 |
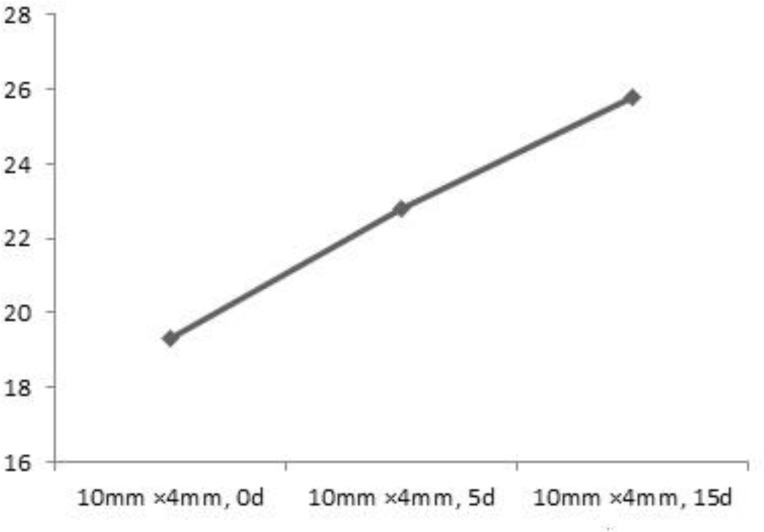
In implants with the fixed length of 7 mm, increase in implant angle gradually increased stress on implants. Similarly, in implants with the fixed length of 10 mm, increasing the implant angle resulted in gradual incerase of stress on implants ( Figs. 3 and 4 ).
Fig. 3.
Gradual increase of stress on implant (7mm×4mm) by increase of angle.
Fig. 4.
Gradual increase of stress on implant (10mm×4mm) by increase of angle.
Increasing implant angulation decreased the stress concentration on the PDL of first premolar. The implants presented higher stress concentration than the PDL, mainly in the implant neck at the implant level (Fig. 5).
Fig. 5.
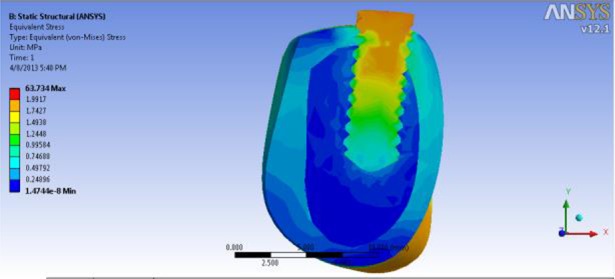
Stress contour
DISCUSSION
This study has two major strengths. First, it used 3D FEA instead of 2D FEA. Second, not only the length of implant, but also the angel of implant were evaluated. Due to these factors, important results were obtained. Fields and Campfield in 1974 for the first time reported using an implant in conjunction with a conventional RPD for treatment of bilateral distal extension in the mandible. They showed no bone loss around the implant, and the tissue around the implants remained healthy [ 32 ]. Watanable et al, in 2003 evaluated the influence of implant inclination (0°, 5° and 15°) on stress distribution in the supporting structures based on two-dimensional FEA.
They placed implant in the first molar edentulous cross-section of the mandible and tested three types of forces. They found that implant inclination was generally worse for stress distribution under vertical load in the center of the crown and an implant placed at 5° inclination displayed slightly lower stress levels than a straight implant [ 33 ].
Himmlova et al, in 2004 used FEA to evaluate stress distribution around implants in all variations in length and diameter of implants. They identified maximum stress area around the implant neck. The maximum decrease in stress (31.5%) was also found for implants with a diameter ranging from 3.6 mm to 4.2 mm. Stress reduction for the 5.0-mm implant was only 16.4%.
The results also showed that an increase in the implant length led to a decrease in the maximum (von Mises) equivalent stress values; the implant length, however, was not as influential as the implant diameter. Note that the length of implants ranged from 8 to 18 mm. Short implants presented higher failure rates [ 34 ].
de Freitas Santos et al, in 2011 evaluated the displacement and stress distribution transmitted by a DERPD associated with an implant placed at different inclinations (0°, 5°, 15° and 30°) in the second molar region of the edentulous mandible ridge based on two-dimensional FEA. The results showed that the introduction of the RPD overloaded the supporting structures and the introduction of the implant helped relieve the stresses of the alveolar mucosa, cortical bone and trabecular bone. The best stress distribution occurred in model with the implant angled at 5°. The use of an implant as a support decreased the displacement of alveolar mucosa for all inclinations simulated. The stress distribution transmitted by the DERPD to the supporting structures improved by the use of straight or slightly inclined implants [ 35 ].
Verri et al, in 2007 evaluated the influence of the length and diameter of the implant incorporated under the saddle of a DERPD based on two-dimensional FEA. It was noted that the presence of the RPD overloaded the supporting tooth. The introduction of the implant reduced stress, mainly at the distal of the edentulous edge. Both the length and diameter tended to reduce stress as their dimensions increased [ 36 ].
According to our study, use of implants with fixed length and diameter may minimize or maximize stress distribution; however, by modifying the angle of implants, stress can be potentially changed. A little information is available about optimized angles for implantation to minimize stress. In this line, we showed that vertical placement of implants resulted in lower level of stress on implants and therefore by increasing this angle, the distribution of stress gradually increased. Numerous investigations have been aimed at determining the optimum geometry of an implant body [ 16 , 17 , 34 , 36 ]. However, the role of implant angle has not been researched adequately and the long-term effects of such stresses in various angles are still unclear and should therefore be investigated and a solution must be sought to minimize undesirable stresses.
CONCLUSION
Within the limitations of this study, we found that:
-
1-
Increasing the length of the implant had little influence on the increase of stress concentration in implant and decrease of stress in the PDL.
-
2-
Increasing the inclination of implant significantly increased stress concentration in the implant and decreased stress in the PDL.
REFERENCES
- 1-. Ohkubo C, Kobayashi M, Suzuki Y, Hosoi T. Effect of implant support on distal-extension removable partial dentures: in vivo assessment. Int J Oral Maxillofac Implants. 2008. Nov-Dec; 23 ( 6): 1095– 101. [PubMed] [Google Scholar]
- 2-. Wilson HJ, Mansfield MA, Heath JR, Spence D. Dental technology and materials for students. 8th ed. London: , Blackwell Scientific Publications; , 1987. : 364 . [Google Scholar]
- 3-. Jepson NJ, Thomason JM, Steele JG. The influence of denture design on patient acceptance of partial dentures. Br Dent J. 1995. April 22 ; 178 ( 8): 296– 300. [DOI] [PubMed] [Google Scholar]
- 4-. Vermeulen AH, Keltjens HM, van't Hof MA, Kayser AF. Ten-year evaluation of removable partial dentures: survival rates based on retreatment, not wearing and replacement. J Prosthet Dent. 1996. September; 76 ( 3): 267– 72. [DOI] [PubMed] [Google Scholar]
- 5-. Wetherell JD, Smales RJ. Partial denture failures: a long-term clinical survey. J Dent. 1980. December; 8 ( 4): 333– 40. [DOI] [PubMed] [Google Scholar]
- 6-. Wills DJ, Mandersone RD. Biomechanical aspects of the support of partial dentures. J Dent. 1977. December; 5 ( 4): 310– 8. [DOI] [PubMed] [Google Scholar]
- 7-. Picton DC, Wills DJ. Viscoelastic properties of the periodontal ligament and mucous membrane. J Prosthet Dent. 1978. September; 40 ( 3): 263– 72. [DOI] [PubMed] [Google Scholar]
- 8-. Monteith BD. Management of loading forces on mandibular distal extension prostheses. Part I: Evaluation of concepts for design. J Prosthet Dent. 1984. November; 52 ( 5): 673– 81. [DOI] [PubMed] [Google Scholar]
- 9-. Aydinlik E, Dayangac B, Celik E. Effect of splinting on abutment tooth movement. J Prosthet Dent. 1983. April; 49 ( 4): 477– 80. [DOI] [PubMed] [Google Scholar]
- 10-. Rasmussen EJ. Alternative prosthodontic technique for tissue integrated prosthesis. J Prosthet Dent. 1987. February; 57 ( 2): 198– 204. [DOI] [PubMed] [Google Scholar]
- 11-. Keltjens HM, Käyser AF, Hertel R, Battistuzzi PG. Distal extension removable partial dentures supported by implants and residual teeth: consideration and case reports. Int J Oral Maxillofac Implants. 1993; 8 ( 2): 208– 13. [PubMed] [Google Scholar]
- 12-. Todescan S, Lavigne S, Kelekis-Cholakis A. Guidance for the maintenance care of dental implants: clinical review. J Can Dent Assoc. 2012; 78: c107. [PubMed] [Google Scholar]
- 13-. Lee JY, Kim HY, Shin SW, Bryant SR. Number of implants for mandibular implant overdentures: a systematic review. J Adv Prosthodont. 2012. November; 4 ( 4): 204– 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14-. Karthikeyan I, Desai SR, Singh R. Short implants: A systematic review. J Indian Soc Periodontol. 2012. July; 16 ( 3): 302– 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15-. Keltjens HM, Kayser AF, Hertel R, Battistuzzi PG. Distal extension removable partial dentures supported by implants and residual teeth: Considerations and case reports. Int J Oral Maxillofac Implants. 1993; 8 ( 2): 208– 13. [PubMed] [Google Scholar]
- 16-. Sohrabi K, Mushantat A, Esfandiari S, Feine J. How successful are small-diameter implants? A literature review. Clin Oral Implants Res. 2012. May; 23 ( 5): 515– 25. [DOI] [PubMed] [Google Scholar]
- 17-. Pommer B, Frantal S, Willer J, Posch M, Watzek G, Tepper G. Impact of dental implant length on early failure rates: A meta-analysis of observational studies. J Clin Periodontol. 2011. September; 38 ( 9): 856– 63. [DOI] [PubMed] [Google Scholar]
- 18-. Romeo E, Bivio A, Mosca D, Scanferla M, Ghisolfi M, Storelli S. The use of short dental implants in clinical practice: literature review. Minerva Stomatol. 2010. Jan-Feb; 59 ( 1–2): 23– 31. [PubMed] [Google Scholar]
- 19-. Watanabe F, Hata Y, Komatsu S, Ramos TC, Fukuda H. Finite element analysis of the influence of implant inclination, loading position, and load direction on stress distribution. Odontology. 2003. September; 91 ( 1): 31– 6. [DOI] [PubMed] [Google Scholar]
- 20-. Cehreli MC, Iplikçioglu H. In vitro strain gauge analysis of axial and off-axial loading on implant supported fixed partial dentures. Implant Dent. 2002; 11 ( 3): 286– 92. [PubMed] [Google Scholar]
- 21-. Geramy A. Alveolar bone resorption and the center of resistance modification (3-D analysis by means of the finite element method). Am J Orthod Dentofacial Orthop. 2000. April; 117 ( 4): 399– 405. [DOI] [PubMed] [Google Scholar]
- 22-. Geramy A, Morgano SM. Finite element analysis of three designs of an implant-supported molar crown. J Prosthet Dent. 2004. November; 92 ( 5): 434– 40. [DOI] [PubMed] [Google Scholar]
- 23-. Geramy A, Sharafodding F. Abfraction: 3D analysis using Finite Element Method. Quintessence Int. 2003. Jul-Aug; 34 ( 7): 526– 33. [PubMed] [Google Scholar]
- 24-. Geramy A, Faghihi S. Secondary trauma from occlusion: 3D analysis using Finite Element method. Quintessence Int. 2004. Nov-Dec; 35 ( 10): 835– 43. [PubMed] [Google Scholar]
- 25-. Lacerda TSP. Comportamento biomecânico das estruturas de suporte e da prótese parcial removível apoiada sobre implante na região distal [dissertação]. São Paulo: : Universidade de São Paulo; Faculdade de Odontologia ; 1999. . [Google Scholar]
- 26-. Birkan TO, Gurcan E, levent C, Volkan K. Insertion of Buccally tilted and placed Implants In edentulous atrophic posterior Mandibular sites. Biotechnol. & Biotechnol. Eq. 2012. January 1 ; 26 ( 4 ): 3163 – 6 . [Google Scholar]
- 27-. Darbar UR, Huggett R, Harrison A, Williams K. Finite element analysis of stress distribution at the tooth-denture base interface of acrylic resin teeth debonding from the denture base. J Prosthet Dent. 1995. December; 74 ( 6): 591– 4. [DOI] [PubMed] [Google Scholar]
- 28-. Farah JW, Craig RG, Meroueh KA. Finite element analysis of a mandibular model. J Oral Rehabil. 1988. November; 15 ( 6): 615– 24. [DOI] [PubMed] [Google Scholar]
- 29-. Ko CC, Chu CS, Chung KH, Lee MC. Effects of posts on dentin stress distribution in pulpless teeth. J Prosthet Dent. 1992. September; 68 ( 3): 421– 7. [DOI] [PubMed] [Google Scholar]
- 30-. Sertgoz A, Gunever S. Finite element analysis of the effect of cantilever and implant length on stress distribution in an implant-supported fixed prosthesis. J Prosthet Dent. 1996. August; 76 ( 2): 165– 9. [DOI] [PubMed] [Google Scholar]
- 31-. Aparicio C, Orozco P. Use of 5-mm-diameter implants: Periotest values related to a clinical and radiographic evaluation. Clin Oral Implants Res. 1998. December; 9 ( 6): 398– 406. [DOI] [PubMed] [Google Scholar]
- 32-. Fields H, Jr, Campfield RW., Jr. Removable partial prosthesis partially supported by an endosseous blade implant. J Prosthet Dent. 1974. March; 31 ( 3): 273– 8. [DOI] [PubMed] [Google Scholar]
- 33-. Watanabe F, Hata Y, Komatsu S, Ramos TC, Fukuda H. Finite element analysis of the influence of implant inclination, loading position, and load direction on stress distribution. Odontology. 2003. September; 91 ( 1): 31– 6. [DOI] [PubMed] [Google Scholar]
- 34-. Himmlova L, Dostalova T, Kacovsky A, Konvickova S. Influence of implant length and diameter on stress distribution: a finite element analysis. J Prosthet Dent. 2004. January; 91 ( 1): 20– 5. [DOI] [PubMed] [Google Scholar]
- 35-. de Freitas Santos CM, Pellizzer EP, Verri FR, de Moraes SL, Falcón-Antenucci RM. Influence of implant inclination associated with mandibular class I removable partial denture. J Craniofac Surg. 2011. March; 22 ( 2): 663– 8. [DOI] [PubMed] [Google Scholar]
- 36-. Verri FR, Pellizzer EP, Rocha EP, Pereira JA. Influence of Length and Diameter of Implants Associated With Distal Extension Removable Partial Dentures. Implant Dent. 2007. September; 16 ( 3): 270– 80. [DOI] [PubMed] [Google Scholar]