Abstract
Objectives:
Accurate localization of the inferior alveolar canal (IAC) is extremely important in some dental treatments. Anatomical variation of the canal means that it can be difficult to locate. The purpose of this study was to assess the relationship of the gonial angle (GA) size and IAC position using cone beam computed tomography (CBCT).
Materials and Methods:
In this in vitro study, 61 dry adult human hemi-mandibles were used. The CBCT scans were taken of all samples and GA was measured on all CBCT scans. The samples were divided into two groups of low angle (≤125°) and high angle (>125°). The canal dimensions, length and course were evaluated. On the sagittal view, the IAC path was classified as type A, B or C. On the axial view, canal course was defined as A1 or A2 according to the mental foramen angle.
Results:
The average GA size was 121.8±7.05° at the right side and 123.8±6.32° at the left side. On the sagittal view, there was a significant correlation between the GA size and the canal course (P=0.04). In the high-angle group, type A was dominant; whereas in the low-angle group, type B was more common. On the axial view of IAC course, type A1 was more common (73.43%).
Conclusion:
The results showed that GA size was associated with IAC course. In cases with a larger GA, the canal runs in a more straightforward path, and at the same level as the mental foramen.
Keywords: Cone Beam Computed Tomography, Mandibular Nerve, Mandible
INTRODUCTION
Precise localization of the IAC is important and successful implant placement or orthognathic surgery depends on the exact determination of the location of the inferior alveolar nerve (IAN). Permanent or temporary IAN damage can cause numbness of the lower lip and chin in orthognathic surgery [ 1 ]. Pressure on this nerve during implant placement is one of the common causes of treatment failure and postoperative pain. On some radiographs, the IAC has a cortical boundary, but in others, the canal may be mistaken for bone marrow especially in osteoporotic patients [ 2 ]. In addition, the anatomical variation of the IAN may be a factor that leads to the failure of block injections [ 3 ]. Recently, by use of CBCT, high anatomical variability of this nerve was discovered [ 4 ]. Although the morphology and the position of the canal vary in different ethnic groups and in different types of jaws, these variations are ignored in many cases and cause problems in dental treatments [ 5 ]. A detailed understanding of the factors affecting the anatomical variations of canal shape and morphology can minimize this problem. Therefore, in this study, we investigated the relationship between the GA size and course of the IAC in human dry mandibles using CBCT. The results may be useful for more accurate localization of the IAC on radiographs before dental treatment.
MATERIALS AND METHODS
In this in vitro study, we obtained dry mandibles from the Anatomy Department of Mashhad University of Medical Sciences. Samples with no anomaly or bone defects were assessed, and those in primary or mixed dentition were excluded [ 3 , 6 – 8 ]. A total of 25 dry adult human mandibles and 6 left and 5 right hemi mandibles (a total of 61 hemi mandibles) of unknown gender or origin were studied.
To increase the accuracy and for easy tracing of the canal, a 0.5 mm diameter orthodontic wire was inserted into the IAC before imaging [ 7 ]. The CBCT scans were obtained (Promax 3D, Planmeca, Helsinki, Finland) with 80×80mm field of view. The exposure parameters were 66 kVp and 5 mA for each sample. As the image field did not cover the entire mandibular bone, the stitch option of CBCT was used, and an oral and maxillofacial radiologist, using Romexis software 2.4.2.R (Planmeca Inc., IL, USA), made the measurements. Intra-observer error was calculated by re-measuring a random sample of 30 images after an interval of two weeks. Both readings were then analysed by paired t-test. In the sagittal view of each ramus, line b was traced tangential to the most prominent point on the posterior border of the ramus and condyle. Line d was also set tangential to the inferior border of the mandible. The angle between lines b and d was measured as GA ( Fig. 1 ) [ 9 – 14 ].
Fig. 1.

Gonial angle measurements
The scans were divided into the following two GA groups: low angle (≤125°) and high angle (>125°) [ 15 ]. To evaluate the shape and position of the canal in coronal views, the distance between the mandibular foramen and the mental foramen was divided into three equal segments and the central cuts (C1, C2, and C3) were measured in each segment [ 16 , 17 ]. In order to evaluate the canal shape, the superior-inferior and buccolingual diameters of the canal were measured in each slice. To evaluate the buccolingual position of the IAC, we measured the distances from the center of the IAC to the tangential lines with buccal and lingual borders and to the lowest point of the inferior border (Fig. 2) [ 17 , 18 ]. In each slice, the distance from the buccal plate to the lingual plate was measured as buccolingual width of the mandibular body [ 16 , 19 ]. Consequently, in order to define the buccolingual position of the canal in each section, the ratio of the distances between the center of the IAC and the buccal and lingual plates to the width of mandible in each section was calculated [ 16 ].
Fig. 2.
Evaluation of the buccolingual position of the IAC by calculating the distance from the center of IAC to buccal, lingual, and inferior borders in C1, C2, and C3 slices
To investigate the total length of IAC, the nerve was traced in coronal views. By using the serial measurements option, the total length of the nerve was exactly measured on the sagittal view (Fig. 3). To investigate the canal course on the sagittal view, the nerve path was classified into three types of A, B, and C [ 7 , 17 ]. In type A, the canal course had a straight path and was positioned at the same level of the mental foramen. In type B, the canal had a curved path, and in type C, the canal had a forward path and then ran superiorly to reach the mental foramen with a sharp ascent (Fig. 4). To evaluate the canal course on the axial view, the nerve path was traced and classified according to the mental foramen angle. If the canal course made an acute angle with mental foramen (≤ 90°), it was defined as type A1; otherwise, it was type A2 ( Fig. 5 ) [ 7 ].
Fig. 3.
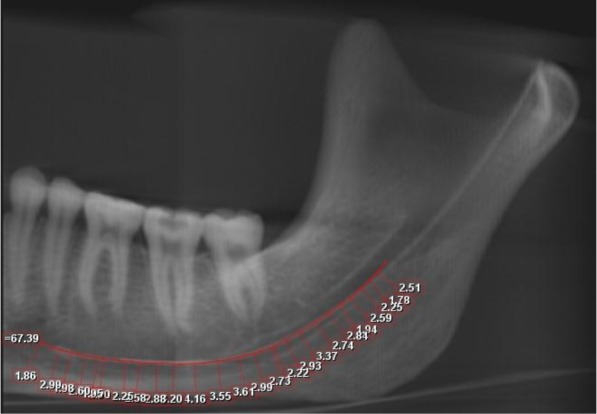
Total length of IAC
Fig. 4.
Different types of canal course on the sagittal view
Type A: The canal course has a straight path at the same level as the mental foramen.
Type B: The canal course has a curve.
Type C: The canal has a forward path and then runs up to reach the mental foramen with a sharp ascent.
Fig. 5.
Different types of canal course on the axial view. The canal course forms an acute angle with the mental foramen on the right side (A1 type) and an obtuse angle on the left side (A2 type)
Statistical analysis was done using PASW® version 18 (SPSS Inc., Chicago, IL, USA). Paired-sample t-test was used for right and left symmetry and calculation of intra-observer agreement between the two readings. Pearson’s correlation coefficient was used to examine the correlation between the right and left GAs. Also, independent-samples t-test was used for quantitative comparison between different canal types on different views. Pearson’s Chi-square test was applied for evaluation of the correlation of canal course in the sagittal plane and GA. A P-value less than 0.05 was defined to be statistically significant.
RESULTS
Intra-observer reproducibility for all variables was calculated by re-examining 30 scans. The differences between measurements in the first and second readings were not significant (P=0.16–0.35).
The mean size of GA was 121.8±7.05° at the right side and 123.8±6.32° at the left side (Table 1). The results showed that there was a statistically significant correlation in the GA size at both sides (P=0.000, r=0.9); however, a significant difference was noted between them (P=0.03). The mean ± standard deviation of canal length at the right and left sides were 63.03±5.48mm and 62.7±5.51mm respectively. There was no significant correlation in the mean total canal length in the right and left sides. No statistically significant difference was found between the two sides in terms of canal lengths (P=0.53).
Table 1.
Descriptive findings for Gas SD: Standard deviation
| Left GA | Right GA | |
|---|---|---|
| Maximum | 141.3° | 138° |
| Minimum | 109.8° | 110.14° |
| Mean±SD | 123.84±7.05° | 121.8±6.32° |
After evaluating different sagittal views of the mandibular canal, it was obvious that the most common type of IAC course on the sagittal view was type B (53.8%), followed by type C (26.2%) and type A (20%). In 70% of the cases, there was no right-left symmetry in the course of the canal on the sagittal view. In addition, it was clear that there was no significant difference between the canal length on the sagittal view, according to canal course (P=0.59).
The samples were grouped according to GA size as high angle (>125°) and low angle (≤125°). The GAs were smaller than 125° and larger than 125° in 60.7% and 39.3% of samples, respectively. As shown in Table 2, there was a significant relationship between different types of canal courses on the sagittal view and the different GA groups (P=0.04). Therefore, in the low GA group, type B was the more common canal course (73.5%), while type A was dominant in the high GA group (66.7%) as shown in Table 2.
Table 2.
Cross tabulation between different canal course types and GA groups on the sagittal view.
| Different angle groups | Total N(%) | |||
|---|---|---|---|---|
|
| ||||
| 125°≥ N(%) | 125°< N(%) | |||
| IAC course on the sagittal view | A | 4(33.3) | 8(66.7) | 12(100) |
| B | 25(73.5) | 9(26.5) | 34(100) | |
| C | 8(53.3) | 7(46.7) | 15(100) | |
|
| ||||
| Total | 37(60.7) | 24(39.3) | 61(100) | |
After evaluating the canal course on the axial view, type A1 was found to be more common (73.43%) than type A2 (26.56%). According to the data in 10.34% of the cases, the canal type was different at both sides of the mandible. There was no statistically significant relationship between the canal course on the axial view and GA group (P>0.05). The total canal length was 63.25±5.4 mm in type A1 and 60.74±4.7 mm in type A2. No significant difference existed in the canal length in different types of canal course on the axial view (P=0.09). Evaluation of the IAC course on the coronal view in segments C1, C2, and C3 showed that on the right side, the canal was closer to the lingual cortex in 86% of the cases in C1, 100% in C2, and 90% in C3; on the left side the corresponding percentages were 77%, 93%, and 93% of the cases, respectively. According to our results, the canal is positioned lingually throughout its path up to the mental foramen, and then reaches the mental foramen with an acute or an obtuse angle.
In addition, these findings can be observed on the axial view. Analysis of the diameters of IAC showed that the greatest mean diameter in the superior-inferior and buccolingual dimensions was in C1 and the smallest was in C2. The most common canal shape on all three cuts was ovoid. A round shape was more frequently observed in C2 and ovoid in C3.
DISCUSSION
In this study, the gender of the individuals from whom the dried human mandibles were obtained was unknown. Many previous studies, including those conducted by de Oliveira-Santos et al, [ 4 ] Ozturk et al, [ 7 ] Kisser et al, [ 8 ] Liu et al, [ 17 ] Apinhasmit et al, [ 20 ] Angel et al, [ 21 ] and Raustia and Salonen [ 22 ] demonstrated that the position of some anatomic landmarks, such as IAC and GA, is not related to gender or age.
The mean size of GA in this study was similar to that found in earlier studies [ 9 – 13 , 23] . The mean GA of the right side was 2° smaller than that in the left side, and this difference was statistically significant. The difference in the mean size of the right and left GA was mentioned in the study by Raustia and Salonen [ 22 ], who stated that the right GA was significantly smaller than the left one. When we analysed the canal shape in the coronal sections, we found that ovoid shape was more common than other shapes. No other study has investigated this issue. Similar to Ozturk et al, [ 7 ] we found that type B was the most common type of canal course on the sagittal view, followed by types C and A. Liu et al. [ 17 ] classified the canal course into four groups (types 1, 2, 3, and 4) using panoramic radiography [ 17 ]. The shape of the canal in type 1 was similar to type A in the current study and the study carried out by Ozturk et al [ 7 ]. Types 2 and 3, which had a catenary like path, were similar to type B, and type 4 was similar to type C. In the study by Liu et al, [ 17 ] the frequency sum of types 2 and 3 was greater than that of type B, but the frequency of types 1 and 4 was lower than that of types A and C [ 17 ]. The difference in the prevalence rate of IAC course shape in the study by Liu et al, [ 17 ] compared to that observed by Ozturk et al, [ 7 ] and in the current study, may be due to the difference in the type of imaging system and methodology of the studies, and may also be because of the difference in GA [ 7 , 17 ].
There was no difference in the total canal length between types A and B; however, there was a high prevalence (66.7%) of type A in the high-angle group, while type B was dominant (73.5%) in the low-angle group. It is analogous to a situation in which you have two identical ropes; if you tie the ends of one of the ropes, its path will be bent, whereas the other rope would have a more direct route. There was no difference in the canal length observed in our study and that found by Liu et al [ 17 ]. Although the method to obtain the total canal length used by Liu et al. was via the tracing cord with a 5 mm arch, while we calculated the length using a specific type of software; the average length found in both studies was very similar [ 17 ].
Ozturk et al. introduced four types of canal course on the axial view, and two of these (types B and C) were introduced for the first time [ 7 ]. Similar to Liu et al, [ 17 ] we did not observe these types in the current study, but type A1 was the most commonly found, which is in accordance with the results of Ozturk et al [ 7 ]. In the current study, the IAC was located near the lingual plate throughout its path, and then travelled to the buccal plate with a sharp ascent near the mental foramen in the majority of samples. Ozturk et al, [ 7 ] Hwang et al, [ 19 ] Som and Curtain [ 24 ], Kim et al, [ 25 ] and Fabian [ 26 ] also found that the IAC is close to the lingual plate, and then runs to the buccal plate near the mental foramen [ 7 , 19 , 24 – 26 ]. Hwang et al. showed that the IAC is close to the lingual plate in the posterior two thirds of the mandible and runs towards the buccal side in the anterior third [ 19 ]. In our study, the entire canal course was of A1 and A2 types on the axial view, which shows that the canal is in the lingual plate, then in front of the mental foramen, it reaches with a sharp turn to the buccal side [ 7 , 19 ]. The canal was located almost 1cm above the inferior border of the mandible in the second premolar and the first molar region, which appears to provide the greatest superior-inferior dimension for implant placement. Ozturk et al. showed that the least distance to the lower border was almost 1cm in the first molar region [ 7 ].
According to the results of the current study, the IAC has the greatest diameter in the ramus region (behind the third molar) and the smallest diameter in the molar region. De Oliveira-Santos et al. studied canal diameter in the first molar region and their conclusion was in accordance with our findings [ 4 ]. No other study has calculated IAC diameter on the coronal view.
In this study we were not able to identify the sex of subjects whose dry mandibles were evaluated; thus further studies on human mandibles are suggested taking into account the sex and age parameters.
CONCLUSION
We concluded that:
-
1-
The GA size has a correlation with the IAC course. In subjects with small GAs, the canal has a curved path. But in cases with large GAs, the canal is more straight and at the same level as the mental foramen.
-
2-
The alveolar crest has the maximum distance from the IAC in the second premolar and first molar region.
Since the IAC is located in the lingual side of the mandible, the safe zone for implant placement and pre-prosthetic surgery is believed to be the buccal side. In addition, the greatest height of bone can be obtained in the second premolar and first molar regions.
REFERENCES
- 1-. Jung YH, Nah KS, Cho BH. The location of the mandibular canal in prognathic patients compared to subjects with normal occlusion . Korean J Oral Maxillofac Radiol 2007; 37: 217– 20. [Google Scholar]
- 2-. Stella JP, Tharanon W. A precise radiographic method to determine the location of the inferior alveolar canal in the posterior edentulous mandible: implications for dental implants. Part 1: Technique. Int J Oral Maxillofac Implants. 1990. Spring; 5 ( 1): 15– 22. [PubMed] [Google Scholar]
- 3-. Prado FB, Groppo FC, Volpato MC, Caria PH. Morphological changes in the position of the mandibular foramen in dentate and edentate Brazilian subjects. Clin Anat. 2010. May; 23 ( 4): 394– 8. [DOI] [PubMed] [Google Scholar]
- 4-. de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, Stinkens L, Moyaert K, Rubira–Bullen IR, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012. April; 16 ( 2): 387– 93. [DOI] [PubMed] [Google Scholar]
- 5-. Levine MH, Goddard AL, Dodson TB. Inferior alveolar nerve canal position: a clinical and radiographic study. J Oral Maxillofac Surg. 2007. March; 65 ( 3): 470– 4. [DOI] [PubMed] [Google Scholar]
- 6-. Kilarkaje N, Nayak SR, Narayan P, Prabhu LV. The location of the mandibular foramen maintains absolute bilateral symmetry in mandibles of different age-groups. Hong Kong Dent J. 2005; 2: 35– 7. [Google Scholar]
- 7-. Ozturk A, Potluri A, Vieira AR. Position and course of the mandibular canal in skulls. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012. April; 113 ( 4): 453– 8. [DOI] [PubMed] [Google Scholar]
- 8-. Kieser J, Kieser D, Hauman T. The Course and Distribution of the Inferior Alveolar Nerve in the Edentulous Mandible. J Craniofac Surg. 2005. January; 16 ( 1): 6– 9. [DOI] [PubMed] [Google Scholar]
- 9-. Heston G, Share J, Frommer J, Kronman JH. Statistical evaluation of the position of the mandibular foramen. Oral Surg Oral Med Oral Pathol. 1988. January; 65 ( 1): 32– 4. [DOI] [PubMed] [Google Scholar]
- 10-. Chrcanovic BR, Abreu MH, Custódio AL. Morphological variation in the dentate and edentulous human mandibles. Surg Radiol Anat. 2011. April; 33 ( 3): 203– 13. [DOI] [PubMed] [Google Scholar]
- 11-. Huumonen S, Sipilä K, Haikola B, Tapio M, Söderholm AL, Remes-Lyly T, et al. Influence of edentulousness on gonial angle, ramus and condylar height. J Oral Rehabil. 2010. January; 37 ( 1): 34– 8. [DOI] [PubMed] [Google Scholar]
- 12-. Xie QF, Ainamo A. Correlation of gonial angle size with cortical thickness, height of the mandibular residual body, and duration of edentulism. J Prosthet Dent. 2004. May; 91 ( 5): 477– 82. [DOI] [PubMed] [Google Scholar]
- 13-. Ohm E, Silness J. Size of the mandibular jaw angle related to age, tooth retention and gender. J Oral Rehabil. 1999. November; 26 ( 11): 883– 91. [DOI] [PubMed] [Google Scholar]
- 14-. Afsar A, Haas DA, Rossouw PE, Wood RE. Radiographic localization of mandibular anaesthesia landmarks. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998. August; 86 ( 2): 234– 41. [DOI] [PubMed] [Google Scholar]
- 15-. Ogawa T, Osato S, Shishido Y, Okada M, Misaki K. Relationships between the gonial angle and mandibular ramus morphology in dentate subjects: a panoramic radiophotometric study. J Oral Implantol. 2012. June; 38 ( 3): 203– 10. [DOI] [PubMed] [Google Scholar]
- 16-. de Oliveira Júnior MR, Saud AL, Fonseca DR, De-Ary-Pires B, Pires-Neto MA, de Ary-Pires R. Morphometrical analysis of the human mandibular canal: a CT investigation. Surg Radiol Anat. 2011. May; 33 ( 4): 345– 52. [DOI] [PubMed] [Google Scholar]
- 17-. Liu T, Xia B, Gu Z. Inferior alveolar canal course: a radiographic study. Clin Oral Implants Res. 2009. November; 20 ( 11): 1212– 8. [DOI] [PubMed] [Google Scholar]
- 18-. Kilic C, Kamburoğlu K, Ozen T, Balcioglu HA, Kurt B, Kutoglu T, et al. The position of the mandibular canal and histologic feature of the inferior alveolar nerve. Clin Anat. 2010. January; 23 ( 1): 34– 42. [DOI] [PubMed] [Google Scholar]
- 19-. Hwang K, Lee WJ, Song YB, Chung IH. Vulnerability of the inferior alveolar nerve and mental nerve during genioplasty: an anatomic study. J Craniofac Surg. 2005. January; 16 ( 1): 10– 4. [DOI] [PubMed] [Google Scholar]
- 20-. Apinhasmit W, Methathrathip D, Chompoopong S, Sangvichien S. Mental foramen in Thais: an anatomical variation related to gender and side. Surg Radiol Anat. 2006. October; 28 ( 5): 529– 33. [DOI] [PubMed] [Google Scholar]
- 21-. Angel JS, Mincer HH, Chaudhry J, Scarbecz M. Cone-beam computed tomography for analyzing variations in inferior alveolar canal location in adults in relation to age and sex. J Forensic Sci. 2011. January; 56 ( 1): 216– 9. [DOI] [PubMed] [Google Scholar]
- 22-. Raustia AM, Salonen MA. Gonial angles and condylar and ramus height of the mandible in complete denture wearers-a panoramic radiograph study. J Oral Rehabil. 1997. July; 24 ( 7): 512– 6. [DOI] [PubMed] [Google Scholar]
- 23-. Oguz O, Bozir MG. Evaluation of location of mandibular and mental foramina in dry, young, adult human male, dentulous mandibles . West Indian Med J . 2002. March; 51 ( 1): 14– 6. [PubMed] [Google Scholar]
- 24-. Som PM, Curtain HD. Embryology and anatomy of the jaw and dentition. In: Head and Neck Imaging. USA: , Mosby; , 2003. : 895 – 8 [Google Scholar]
- 25-. Kim ST, Hu KS, Song WC, Kang MK, Park HD, Kim HJ. Location of the mandibular canal and the topography of its neurovascular structures. J Craniofac Surg. 2009. May; 20 ( 3): 936– 9. [DOI] [PubMed] [Google Scholar]
- 26-. Fabian FM. Position, shape and direction of opening of the mental foramen in dry mandibles of Tanzanian adult black males. Ital J Anat Embryol. 2007. Jul-Sep; 112 ( 3): 169– 77. [PubMed] [Google Scholar]





