Abstract
Background:
Nowadays, restriction on access and optimum use of resources is the main challenge of development in all organizations. Therefore, the aim of this study was to determine the technical efficiency and its factors, influencing hospitals of Tehran.
Methods:
This research was a descriptive-analytical and retrospective study conducted in 2014–2015. Fifty two hospitals with public, private, and social security ownership type were selected for this study. The required data was collected by a researcher-made check list in 3 sections of background data, inputs and outputs. The data was analyzed by DEAP 1.0.2, and STATA-13 technique.
Results:
Seventeen (31/48) of hospitals had the efficiency score of 1 as the highest technical efficiency. The highest average score of efficiency was related to social security hospitals as 84.32, and then the public and private hospitals with the average of 84.29 and 79.64 respectively. Tobit regression results showed that the size, type of practice, and ownership of hospitals were effective on the degree of their technical efficiency. However, there was no significant correlation between teaching / non-teaching hospitals with technical efficiency.
Conclusion:
Establishment of competition system among hospitals, constitution of medium size hospitals and allocation of budget to hospitals based on national accreditation system are recommended.
Keywords: Technical efficiency, Data envelopment analysis, Hospital, Iran
Introduction
Lack of resources for the health care system, is one of the most important reasons for paying attention to efficiency, and appropriate use of existing facilities ( 1 ). Hospitals historically have been among the foremost providers of health care for underserved populations, giving this institutions extensive experience in providing services to diverse patient. Hospitals are the main consumers of resources ( 2 ), and more than 50 percent of health care system costs are allocated to hospitals, therefore these institutions should focus on reduced health care disparities, and improve patient satisfaction ( 3 ). Achievement of technical efficiency of hospitals, produce aggregate health outcomes and relatively efficiency advantages ( 4 ). Technical efficiency, refers to the capability of policymakers’ decision-making to produce the maximum possible output to certain level of input ( 5 ). Estimation of input – oriented technical efficiency is defined as minimizing input, or consumed resources for a specific level of output ( 6 ). Data Envelopment Analysis (DEA) method, presented by Farrell, is a procedure to measure technical efficiency from a single – input, single-out put process to a multiple – input, multiple – output process ( 7 ). “Charnes”, “Cooper”, and “Rhodes” first introduced DEA in 1978, and “Farrells” developed this approach by presumption of Constant Returns to Scale (CRS) as a sensitive model for assessing technical efficiency ( 8 ). Moreover, the second model of DEA was proposed by the presumption of Variable Returns to Scale (VRS), in order to separate pure efficiency from scale efficiency ( 9 ).
There are several factors that can affect hospital efficiency, for example hospital size whose influence can be displayed in two forms of Decreasing Returns to Scale (DRS) and Increasing Returns to Scale (IRS). A hospital- may be too large for its amount of activities, and thus experiences lack of Diseconomies of Scale. On the other hand, it might be too small for giving services, and as a result, experiences Economies of Scale. In addition, because of providing the above situations, DEA method can provide the possibility of determination of multiple-input, and multiple – output process simultaneously. For this reason, it has become the dominant approach for efficiency assessment of health care organizations and the other parts ( 10 , 4 ).
In addition to hospital size as one of the determinant factors, the type of ownership, being special or general, and also the type of hospital practice as teaching or non-teaching, plays an important role in explaining economic performance of a hospital to create different motivations for economical practice ( 11 ). Therefore, these variables have been noteworthy interest of researchers for a long time, and several researches have been studied in this area ( 4 , 10 , 12 – 18 ).
According to WHO reports, the share of health care system monetary of Gross Domestic Product (GDP) has increased from 4.6% to 6.75% from 2000 to 2012 in Iran ( 19 ). In this country, public, private, and social security types of hospitals altogether constitute the set of health care system hospitals. The contribution of each type of hospitals related to provide hospital care in health care system is 65.97%, 14.62% and 6.63% respectively ( 20 , 21 ). Bed occupancy rate (BOR) and patients’ length of stay (LOS) in hospitals affiliated with the Ministry of Health in Iran was 70% and 3.38 days respectively ( 22 , 23 ).
The average of bed occupancy rate in hospitals of Ahvaz belonged to 2011 was about 66.71% ± 13.81 versus the minimum rate for the year 2007 (63.86% ± 11.88). Moreover, the average of length of stay (ALS) was 17.7 days for the year 2007 versus 10.59 days in 2011 ( 24 ). More than 60% of Uremia hospitals had low performance in terms of BOR and BTO ( 25 ). The overall ALSO, BOR and Bed Turn Over (BTO) rates in Qazvin, Iran were 4.1 days, 68.9% and 61.1 respectively. Besides, the studied hospitals need more improvement in managerial decisions in order to enhance their efficiency and productivity ( 26 ).
There are different techniques assessing hospital efficiency indicators, including hospital performance ratios, Data Envelopment Analysis (DEA), Stochastic Frontier Analysis (SFA), Pabon Lasso and so on ( 24 ). Hospitals account for a large share of health care system expenditures. Therefore, use of resources is a significant goal in all health care system, particularly hospitals ( 25 ).
Hospitals in Iran are not in an appropriate condition in terms of technical efficiency, and it is possible to improve Iranian hospitals’ efficiency to attain the international standards. Therefore, the aim of this study was to determine the technical efficiency, and its factors influencing in hospitals of Tehran using DEA method.
Materials and Methods
This research was a descriptive-analytical and retrospective study conducted in 2014. Out of 110 hospitals in Tehran City, 54 hospitals (including 25 governmental hospitals, 19 private hospitals and 10 social security hospitals) entered the study. A self-researcher -made checklist used to collect data in 3 section demography details, and also inputs (number of active beds, number of physicians, number of nurses and other personnel), and outputs (including number of outpatient visits, number of surgery procedures, average length of stay and number of hospitalization days) ( Table 1 ). Data was collected with collaboration of studied hospitals of medical records departments.
Table 1:
Demographic information, inputs, and selective outputs
| Hospital | Ancillary Subgroups | Inputs | Outputs |
|---|---|---|---|
| Ownership type | Governmental, Private, Social security | Active beds number | Outpatients visit number |
| Size | Bed number | Physician number | Surgery number |
| Hospital practice | Teaching, Non-teaching | Nurse number | Average of patient length of stay |
| Type of hospital | General, Special | Other medical staff number | Hospitalized days |
Research Ethics Committee of Tehran University of Medical Sciences approved this research, and the researchers took the needful license from the studied hospitals administrators, and also assure the confidantibility of the data to the mentioned administrators.
Data analysis was induced in two stages. In the first stage, technical efficiency scores were estimated based on input-oriented model with the assumption of Variable Returns to Scale (VRS), using non – parametric methodology, known as the DEA method, and DEAP software 1.0.2.
Deap (Distributed Evolutionary Algorithms in Python) software is an evolutionary computation framework for rapid prototyping and testing of ideas.
On the other hand, “Coell” computer introduced a program written to conduct DEA for the purpose of calculating efficiencies in production. Three principal options are available in the computer program. The first involves the standard CRS and VRS DEA models that involve the calculation of technical and scale efficiencies. The second options consider the extension of this model to account for cost and allocative efficiencies. The third option considers the application of Malmquist DEA methods to panel data to calculate indices of Total Factor Productivity (TFP) change, technical efficiency change and scale efficiency change ( 27 ). Eventually, the hospitals that were technically efficient, gained a score of 1 to 100, and the hospitals that were inefficient gained an efficiency score less than 1 to 100. Therefore:
In the above model, θ shows the technical amount of efficiency of r, and hospital yrj represents the amount of output r in j hospital, and xij shows the amount of input i in j hospital. In this research, j includes the studied hospitals, and i include the amounts of 1, 2, 3, 4 for the number of physicians, nurses, other staffs, and the number of active beds respectively. Also, r includes the amount of 1, 2, 3 and 4 for the variables of the number of outpatient visits, the number of surgeries, the average of patients’ length of stay, and the number of hospitalization days.
In the second stage, the effects of the studied variables on technical efficiency scores were assessed using Tobit regression, because technical efficiency score as the dependent variable has a limited range of variations between 0 and 100%, unlike the typical regression in which the range of scores should not have any special restrictions. The second reason is that due to the limited range of variation of dependent variable (technical efficiency), regression coefficients related to independent variables cannot be assessed by the least squares method. However, in Tobit regression, the assessment of those coefficients is possible. Previous studies also conducted on the efficiency of hospitals, have used Tobit regression model ( 4 , 12 , 15 , 22 ). In this study, the Tobit regression model was used as following:
In this model, yj is the technical efficiency score for hospital j, xjn are independent variables, including hospital ownership, hospital size, type of hospital practice, α is the intercept model (fixed amount), and other α (Alphas) are regression coefficients related to independent variables. Furthermore, εj is the error sentence, which has a normal distribution with mean of μ and standard deviation of σ. To analyze of this stage, STATA-13 software was used.
Results
Table 2 summarizes the descriptive statistics of 54 studied hospitals in Iran. There were variations in the average of input and output based on hospitals’ ownership. For example, the average number of active beds was 153 in social security, and 233 beds in governmental hospitals. Among other variables, such as the number of physicians, the number of outpatients visits, and average of length of stay of patients, there were much difference between governmental hospitals with private and social security hospitals.
Table 2:
Summary of descriptive of inputs and outputs variations
| Inputs variations average and standard deviation | Output variations average and standard deviation | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Ownership | number of hospital | Active beds | Physicians | Nurses | Other medical staff | Surgery | Hospitalized days | Average of patient length of stay | Outpatient visits |
| Governmental | 25 | 233 (152.2) | 67 (52.7) | 206 (126.5) | 373 (258.3) | 8509 (7161.2) | 62562 (47779) | 904 (1.8) | 135746 (106844.7) |
| Private | 19 | 155 (77.6) | 50 (22.8) | 160 (89.4) | 321 (204.2) | 7445 (4479.2) | 51530 (27116) | 3.7 (0.9) | 233136 (147359.7) |
| Social security | 8 | 153 (113.4) | 65 (32.5) | 147 (102.9) | 3.98 (239.1) | 8701 (5063) | 39024 (29934.5) | 3.4 (1.4) | 293769 (102403.9) |
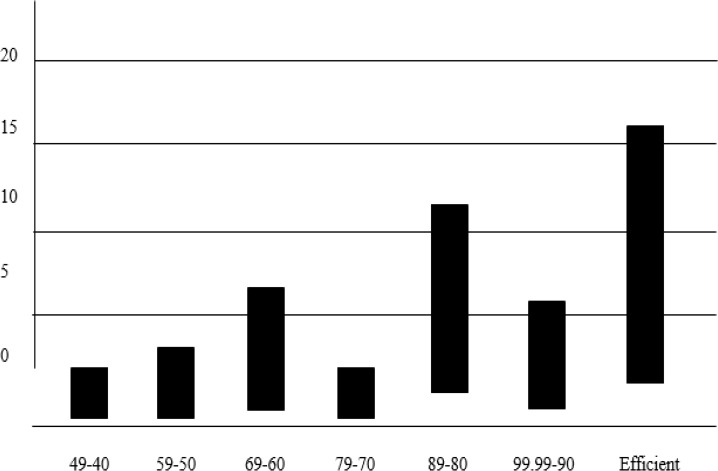
Fig. 1 shows the distribution of technical efficiency scores based on VRS model for the 54 hospitals. Out of 54 hospitals, 17 (31.48%) of hospitals were 100% efficient, 23 (42.6%) with the efficiency score between 70 and 99.99, were relatively efficient, and 16 (29.6%) had an efficiency score below 70. Furthermore, the lowest efficiency scores were in the range of 40 to 49.
Fig. 1:
The distribution of efficiency scores of hospitals based on VRS model
A summary of the average of efficiency scores of hospitals based on their ownership is presented in Table 3 . The average of VRS technical efficiency scores for all hospitals was 81.9 or 0.819. The highest average of efficiency score was related to social security hospitals (84.32), and then private hospitals (84.29), and finally governmental hospitals (79.64) respectively. Out of 54 hospitals, only 17 (31.5%) hospitals were on the efficiency borderline. Out of 17 hospitals that had the best performance, 8 (42%) were private hospitals, 6 (25%) were governmental hospitals, and 3 (30%) were social security hospitals.
Table 3:
Distribution of technical efficiency scores with assumption of VRS based on ownership of hospitals
| Ownership | Hospital number | Average of score (%)VRS | Standard deviation | Minimum | Maximum | Efficient hospital |
|---|---|---|---|---|---|---|
| Governmental | 25 | 79.64 | 18.22 | 43.4 | 100 | 6 (25) |
| Private | 19 | 84.29 | 19.31 | 40.5 | 100 | 8 (42) |
| Social security | 10 | 84.32 | 19.31 | 60 | 100 | 3 (30) |
Table 4 presents the results of Tobit regression analysis. According to regression coefficient, hospitals ownership had an adverse effect on technical efficiency. This means that technical efficiency score reduced from the social security hospitals to governmental hospitals, and the effect of this variable was statistically significant (P=0.05). Hospital type (specialty or general) has a direct impact on technical efficiency.
Table 4:
Estimation of the results of Tobit regression model
| Technical efficiency variation | Regression coefficient | Standard error | t criteria | p value | Interval confidence 95% |
|---|---|---|---|---|---|
| Ownership | −0.0027 | 0.0589 | −0.05 | 0.005 | (0.01212 0.1167) |
| Type of hospital (special/general) | 0.1266 | 0.0525 | 2.41 | 0.02 | (0.02110 0.2321) |
| Hospital size | 0.00037 | 0.00020 | 1.78 | 0.081 | (−0.000047 0.00079) |
| Hospital practice (teaching / non-teaching) | 0.1283 | 0.0903 | 1.42 | 0.162 | (−0.0530 0.3097) |
| Constant amount | 0.1686 | 0.0164 | -- | -- | (0.1353 0.2014) |
In specialty hospitals, technical efficiency was higher, and there was significant correlation between specialty and general hospitals with technical efficiency (P=0.02). Furthermore, hospital size had a significant impact on technical efficiency with 90% confidence, so that by increasing the number of hospital beds, technical efficiency increased (P=0.008). Hospital practice type variable (teaching/non-teaching), was not statistically significant correction with technical efficiency (P=0.162), although in non-teaching hospitals, technical efficiency is higher than teaching hospitals.
Table 5 shows that 36 (67%) of hospitals had technical scale inefficiency, i.e. they were either too small or too large. Out of 54 studied hospitals, 24 (45%) of hospitals had increased output to scale ratio that means these hospitals should increase the amount of inputs to achieve higher efficiency. 18 (33%) of hospitals had constant output to scale ratio, i.e. variation in amount of input had no effect on the efficiency of this group, and eventually 12 (22%) of hospitals had decreased output to scale ratio. Therefore, in order to achieve higher efficiency, the amount of input should be reduced.
Table 5:
Output to scale ratio among the studied hospitals
| Ownership | Increasing (%) | Constant (%) | Decreasing (%) | Hospital number (%) |
|---|---|---|---|---|
| Governmental | 14(56) | 6(24) | 5(2) | 25(100) |
| Private | 8(42.1) | 9(47.37) | 2(10.53) | 19(100) |
| Social security | 2(20) | 3(30) | 5(50) | 10(100) |
| Total | 24(45) | 18(33) | 12(22) | 54(100) |
Discussion
“The establishment of specific and thoroughly researched criteria to evaluate hospitals’ performance is very important, because there is a huge and increasing amount of public resources dedicated to healthcare. Therefore, it is necessary to design a system to evaluate health care performance in order to discover and improve potential inefficiencies” ( 28 ).
A major issue for health care system is accommodation of the needs of people covered by this system. For hospitals, a traditional response to this increased demand might be added resources such as more staff and beds.
Such actions would be unaffordable and unnecessary. Researches has demonstrated that large gains in managed efficiency cause achieve improved bad occupancy rate, without adding beds, through streamlining patient flow and redesigning care process ( 29 ). In Iran, hospitals have experienced reduction in budget, while there is an increasing demand for health services. Such conditions have caused limitations as to the use of financial resources for hospitals ( 5 , 20 ). This necessitates the evaluation of the hospital efficiency and productivity, and the factors affecting them. Moreover, there are changes under way within lending organizations that suggest significant improvements in quality and value can be achieve ( 30 ).
This research is the first study about hospital efficiency that induced after establishment of health care overhaul plan in Iran. Therefore, inefficiency of most hospitals in Tehran, especially in public sector is very important issue for health care policy makers, regardless more allocation of budget to governmental hospitals.
The results of this study showed that approximately 70% of studied hospitals are inefficient; therefore, they do not utilize their resources optimally. In fact, they need to improve their performance. In addition, our study showed that the kind of hospital ownership, hospital type and hospital size influenced technical efficiency, and it was confirmed by significant statistical correlation.
Our results showed that private hospitals are more efficient than governmental and social security hospitals. This finding is compatible with Chang et al. results ( 12 ). One of the main reasons that governmental hospitals are less efficient than other hospitals is that, governmental hospitals are principally assure social benefit, and removed health care problems in the community, while private hospitals can pursue economic goals, besides the above goals as well. The second reason could be related to the provision of health care services with different costs. Governmental hospitals must work with public sector’s tariff which is much lower than the tariff of the private sector ( 12 , 21 ). On the other hand, it should be noted that private hospitals due to their ownership, they work under conditions that enable them to pay more attention to augment more health services by creating changes in hospital inputs due to having more flexibility in work procedures and regulations. For example, in private hospitals, the physicians are more active, and practice as shareholders of the hospitals. This makes physicians practice actively only when necessary. Thus, private hospitals consume their inputs with full flexibility. But governmental and social security hospitals should use physicians as full-time practitioners according to governmental regulations ( 31 , 32 ). Jehu-Appiah et al. in Ghana ( 4 ), reported different results about this claim. In Ghana, the efficiency of governmental hospitals is more than private hospitals. The reason could be related to the payment system in Ghana in which governmental hospitals are supported based on annual fixed budget which trend to reduce extra costs, and as a result, increase efficiency ( 4 ).
Studies that have examined the impact of the kind of ownership on hospital efficiency, have obtained inconsistent, and sometimes contradictory results ( 4 , 12 , 33 ). A study in Germany showed no relationship between these two variables ( 34 ). Private ownership of hospitals had negative impact on their efficiency ( 4 ), while in current study, this impact was positive. Governmental hospitals were potentially more efficient than private hospitals ( 10 , 16 ). However, technical efficiency in governmental hospitals was lower than private hospitals ( 12 ). Although, the current study showed that the highest efficiency was related to private hospitals, but social security and governmental hospitals were in the next rankings respectively. The other results of current study showed the influence of hospital size on technical efficiency, i.e. technical efficiency was increased by increasing the number of beds. This is compatible with other results in Taiwan ( 17 ), in South Korea ( 15 ) and in Iran ( 35 ), which showed that larger hospitals had more efficiency. Furthermore, in Ireland the efficiency of larger hospitals was 8% to 18% more than smaller hospitals similar to our results ( 36 ). In private and governmental hospitals in the US, larger hospitals were more efficient than smaller hospitals in both private and public sectors ( 37 ). A significant positive correlation between the size and efficiency of the hospital is reported ( 16 ). Although, reverse results are reported; for instance, using extra beds in hospital, is one of the factors affecting the decrease of hospitals’ technical efficiency ( 38 ). Perhaps, the one reason for this inconsistency can be attributed to diversity in hospital size.
This question arises if technical efficiency is more in larger hospitals, how far this trend will continue. In response to this question, in developing countries, a number of researchers recommended the size of hospitals up to 190 beds in order to achieve high efficiency, while some suggested 120 beds to achieve greater efficiency, and they believed the average length of stay of patients would be shorter, and technical efficiency index of hospitals would be higher in the ( 17 , 35 ). The reason for this difference may be related to different situations in developed and developing countries.
Specialization of health care system may improve the performance of hospitals. The previous researches confirm this hypothesis. For example, there was a significant relationship between technical efficiency and specialization of hospitals ( 15 ). This means that specialized hospitals are more efficient than general hospitals. This is similar to the results of the current study. According to Tobit model, being specialized or general has a positive impact on hospital efficiency.
The present study also examined the impact of teaching or non-teaching hospitals on technical efficiency. Only few teaching hospitals could effectively compete with non-teaching hospitals based on service delivery to patients ( 13 ). In addition, the efficiency score of teaching hospitals was less than non-teaching hospitals ( 15 ). This is similar to the results of the current study in that based on Tobit regression results; the efficiency of non-teaching hospitals is less than teaching hospitals in Iran, although it was not approved by statistically methods. Finally, in this study, 24(45%) of hospitals made increasing output to scale that corresponds to the results of Jandaghi et al. ( 39 ).
Limitation of the study
One of the main limitations of the present study is, conducted at one specific time. A longitudinal study would be useful, although limited resources make this difficult. Second, many other factors that influence the hospital efficiency has not been included in our research. Therefore, it might not be accurate to state absolute conclusions about hospitals efficiency using the results of this research.
Conclusion
Most of the studied hospitals are inefficient. This inefficiency is more in the public sector. Changes in the efficiency of the studied hospitals are under the influence of ownership, size, type of practice and type of hospitals. Thus, different ownerships, sizes, types of practice and type of teaching and non-teaching hospitals can cause positive, negative, or neutral effects on changes in technical efficiency due to different hospital conditions. Private and social security hospitals have greater efficiency. The effect of size of hospital was positive impact on hospital efficiency in this study, so that efficiency improves by increasing the number of beds. Moreover, teaching hospitals reduce efficiency. These results have important practical implications for health care policy-makers. With increasing competition, health care organizations currently are inevitable to compete more for survival in the health care market. Moreover, hospital administrators also can improve the situation of inefficient hospitals by changing input and output variables besides recognition of the effects of specialization, size and being non-teaching on hospitals’ efficiency.
We suggest the competition system should be established between governmental, private, and social security hospitals by health care policy – makers. Besides, constitution of medium size hospitals according to international standards with special mission, and allocation of budget to hospitals based on national accreditation system one recommended by the authors.
Ethical Considerations
Ethical issues including plagiarism, informed consent, misconduct, data fabrication and / falsification, double publication, redundancy etc. have been completely observed by authors.
Acknowledgments
This research is elicited from MSc. Dissertation supported by Vice-Chancellorship for Research and Technology Affairs and School of Public Health, Tehran University of Medical Sciences. The authors would like to thank hospital administrators, because this survey would not have been possible without their assistance. The authors declare that they have no conflicts of interest.
References
- 1. Hatam N, Moslehi Sh, Askarian A, Shokrpour N, Keshtkaran A, Abbasi M. (2010). The Efficiency of General Public Hospitals in Fars Province, Southern Iran . IRCMJ , 12 ( 2 ): 138 – 144 . [Google Scholar]
- 2. Nayar P, Ozcan YA. (2008). Data Envelopment Analysis Comparison of Hospital Efficiency and Quality. J Med Syst, 32( 3): 193–199. [DOI] [PubMed] [Google Scholar]
- 3. Mohebbifar R, Sokhanvar M, Hasanpoor E, Mosavi H, Ziaiifar H, Kakemam, Mohseni (2014). A survey on the performance of hospitals of Qazvin Province by the Pabon Laso Model. Res J Chem Sie, 3( 12): 5–9. [Google Scholar]
- 4. Jehu – Appiah C, Sekidde S, Adjuik M, Akazili J, Almeida S, Nyonator F, Baltussen Ret, et al. (2014). Ownership and technical efficiency of hospitals: evidence from Ghana using data envelopment analysis. Cost Eff Resour Alloc, 8; 12 ( 1 ): 9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kiadaliri AA1, Jafari M, Gerdtham UG. (2013). Fronitier – based techniques in measuring hospitals efficiency in Iran: a systematic review and meta-regression analysis. BMC Health Serv Res, 15; 13 : 312 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kounetas K, Papathanassopoulos F. (2013). How efficient are Greek hospitals? A care study using a double bootstrap DEA approach. Eur J Health Econ, 14( 6): 979–994. [DOI] [PubMed] [Google Scholar]
- 7. Farrell MJ. (1957). The measurement of productive efficiency. J Royal Statistical Soc, Series A (General): 253 – 290 . [Google Scholar]
- 8. Charnes A, Clark CT, Cooper WW, Golany B. (1984). A developmental study of data envelopment analysis in measuring the efficiency of maintenance units in the US air forces. Ann Oper Res, 2( 1): 95–112. [Google Scholar]
- 9. De Cos PH, Enrique MB. (2014). Determinants of health – system efficiency: evidence from OECD countries. Int J Health Care Finance Econ, 14( 1): 69–93. [DOI] [PubMed] [Google Scholar]
- 10. Hollingsworth B, Wildman J. (2003). The efficiency of health production: re-estimating the WHO panel data using parametric and non-parametric approaches to provide additional information. Health Econ, 12( 6): 493–504. [DOI] [PubMed] [Google Scholar]
- 11. Barbetta GP, Turati G, Zago AM. (2007). Behavioral differences between public and private not-for-profit hospitals in the Italian National Health Service. Health Econ, 16( 1): 75–96. [DOI] [PubMed] [Google Scholar]
- 12. Chang H, Cheng MA, Das S. (2004). Hospital ownership and operating efficiency: evidence from Taiwan. Eur J Oper Res, 159( 2): 513–327. [Google Scholar]
- 13. Grosskopf Sh, Margaritis D, Valdmanis V. Comparing teaching and non-teaching hospitals: a frontier approach (teaching vs. non-teaching hospitals) . Health Care Manag Sci, 4 ( 2 ): 83 – 90 . [DOI] [PubMed] [Google Scholar]
- 14. Lee KH, Yang SB, Choi M. (2009). The association between hospital ownership and technical efficiency in a managed care environment. J Med Syst, 33( 4): 307–315. [DOI] [PubMed] [Google Scholar]
- 15. SooLee KS, Chun KH, Lee JS. (2008). Reforming the hospital service structure to improve efficiency: urban hospital specialization. Health Policy, 87( 1): 41–49. [DOI] [PubMed] [Google Scholar]
- 16. Tiemann O, Schreyogg J. (2009). Effects of ownership on hospital efficiency in Germany. BUR, 2( 2): 115–145. [Google Scholar]
- 17. Watcharasriroj B, Tang J. (2004). The effects of size and information technology on hospital efficiency. J High Tech Manag Res, 15( 1): 1–16. [Google Scholar]
- 18. Herr A. (2008). Cost and technical efficiency of German hospitals: does ownership matter? Health Econ, 17( 9): 1057–1071. [DOI] [PubMed] [Google Scholar]
- 19. WHO EMRO (2013). Strengthening health systems for universal health coverage. Available from: http://www.emro.who.int/annual-report/2013/strengthening-health-systems.html .
- 20. Hajialiafzali H, Moss JR, Mahmood MA. (2007). Efficiency measurement for hospitals owned by the Iranian Social Security Organization. J Med Syst, 31( 3): 166–172. [DOI] [PubMed] [Google Scholar]
- 21. Jafari M, Rashidian A, Abolhasani F, Mohammad K, Yazdani SH, Parkerton P, et al. (2011). Space or no space for managing public hospitals; a qualitative study of hospital autonomy in Iran. Int J Health Plann Manage, 26( 3): e121–137. [DOI] [PubMed] [Google Scholar]
- 22. Gressani D, Larbi H, Fetini H. (2008). Islamic Republic of Iran Health Sector Review: Volume H: Background Sections . Washington, DC: : The World Bank Group; . [Google Scholar]
- 23. Rezapoor A, Morteza HS, Saeed BF. (2014). Studying effects of production factors in hospitals affiliated with Tehran University of Medical Sciences (2008–2011). J Health Policy Sustainable Health, 1( 2): 45–51. [Google Scholar]
- 24. Lotfi F, Kalhor R, Bastani P, Shaarbafchi Zadeh N, Eslamian M, Dehghani MR, Kiaee MZ. ( 2014. ). Various indicators for the assessment of hospitals' performance status: differences and similarities . Iran Red Crescent Med J, 16 ( 4 ): e12950 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bahadori MK, Sadeghifar J, Hamuzadeh P, Hakimzadeh SM, Nejati M. (2011). Combining multi indicators to assess hospital performance in Iran using the Pabon Lasso Model. AMJ, 4( 4): 175–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kalhor R, Salehi N, Keshavarz A, Bastani P, Heidari Orojloo P. ( 2014. ). Assessing hospital performance in Iran using the Pabon Lasso Model . ACHSE, 9 : 77 – 82 . [Google Scholar]
- 27. Monograph on the Internet. Coelli T. (2013). A guide to DEAP Version 2.1: a data envelopment analysis (computer) program . CEPA working Paper 96/08. www.une.edu.au/econometrics/cepa.htm
- 28. Tarazona MC, Clemente IM, Consuelo DV, Martinez IB. (2010). A model to measure the efficiency of hospital performance. Mathematical and Computer Modelling, 52(7): 1095–1102. 10.1016/j.mcm.2010.03.006 . [DOI] [Google Scholar]
- 29. Litvake E, Bisognano M. (2011). More patients, less payment: increasingly hospital efficiency in the aftermath of health reform . Health Aff (Millwood), 30 ( 1 ): 78 – 80 , 10.1377/hlthaff.2010.1114 . [DOI] [PubMed] [Google Scholar]
- 30. Edwards JN, Carroll SS, Lashbook A. (2011). Achieving efficienicey lessons from four top-performing hospitals. Synphesis Reports. The commonwealth Found. http://www.commonwealthfund.org/publications/case-studies/2011/jul/efficiency-series .
- 31. Czypionka T, Kraus M, Mayer S, Rohrling G. (2014). Efficiency, ownership, and financing of hospitals: The Case of Austria. Health Care Manag Sci, 17( 4): 331–347. [DOI] [PubMed] [Google Scholar]
- 32. Santerre RE, Vernon JA. (2005). Hospital ownership mix efficiency in the US: An exploratory study. National Bureau of Economic Research, Technical report, NBER Working Paper 11192.
- 33. Daidone S, Francesco DA. (2009). Technical efficiency, specialization and ownership form: evidences from a pooling of Italian hospitals. J Prod Anal, 32( 3): 203–216. [Google Scholar]
- 34. Staat M. (2006). Efficiency of hospitals in Germany: a DEA-bootstrap approach. JAE, 38( 19): 2255–2263. [Google Scholar]
- 35. Hatam N. (2008). The role of Data Envelopment Analysis (DEA) pattem in the efficiency of social security hospitals in Iran. IRCMJ, 10( 3): 211–217. [Google Scholar]
- 36. Gannon B. (2004). Technical Efficiency of Hospitals in Ireland. ESRI, 18: 1–32. [Google Scholar]
- 37. Coyne JS, Richards MT, Short R, Shultz K, Singh SG. (2009). Hospital cost and efficiency: do hospital size and ownership type really matter? J Healthc Manag, 54( 3): 163–174. [PubMed] [Google Scholar]
- 38. Sherman HD. (1984). Hospital efficiency measurement and evaluation: empirical test of a new technique. Med Care, 22( 10): 922–938. [DOI] [PubMed] [Google Scholar]
- 39. Jandaghi G, Zarei Matin M, Doremami M, Aghaziyarati M. (2010). Efficiency evaluation of Qom public and private hospitals using data envelopment analysis. Eur J Econ Finance Administrative Sci, 22( 2): 83–92. [Google Scholar]