Abstract
Background: Mesenchymal stromal cells (MSCs) may reduce inflammation and promote tissue repair in pulmonary emphysema.
Aim: To study the safety and feasibility of bone marrow-derived autologous (BM-) MSC intravenous administration to patients with severe emphysema.
Design: A phase I, prospective open-label study registered at ClinicalTrials.gov as NCT01306513. Eligible patients had lung volume reduction surgery (LVRS) on two separate occasions. During the first LVRS bone marrow was collected, from which MSCs were isolated and expanded ex vivo. After 8 weeks, patients received two autologous MSC infusions 1 week apart, followed by the second LVRS procedure at 3 weeks after the second BM-MSC infusion.
Methods: Up to 3 weeks after the last MSC infusion adverse events were recorded. Using immunohistochemistry and qPCR for analysis of cell and proliferation markers, emphysematous lung tissue obtained during the first surgery was compared with lung tissue obtained after the second surgical session to assess BM-MSC effects.
Results: From 10 included patients three were excluded: two did not receive MSCs due to insufficient MSC culture expansion, and one had no second surgery. No adverse events related to MSC infusions occurred and lung tissue showed no fibrotic responses. After LVRS and MSC infusions alveolar septa showed a 3-fold increased expression of the endothelial marker CD31 (P = 0.016).
Conclusions: Autologous MSC treatment in severe emphysema is feasible and safe. The increase in CD31 expression after LVRS and MSC treatment suggests responsiveness of microvascular endothelial cells in the most severely affected parts of the lung.
Introduction
Mesenchymal stromal cells (MSCs) are multipotent cells that can differentiate into several cell types, including fibroblasts, osteoblasts, adipocytes and chondrocyte progenitors.1 In addition to their differentiation capacity, it has been shown that bone marrow-derived MSCs (BM-MSCs) release a variety of soluble factors implicated in anti-apoptotic signalling, cell growth and wound healing, potentially facilitating the endogenous regenerative potential.2,3 Moreover, it has become evident that BM-MSCs have potent immunomodulatory effects in vitro and in animal models of chronic inflammation in vivo.2 Importantly, encouraging results have been obtained in patients with severe steroid resistant Graft vs. Host Disease in response to treatment with BM-MSCs as well as in patients with refractory perianal fistulas in Crohn’s disease.4,5
The combination of immunosuppressive, growth-potentiating, angiogenic and anti-apoptotic properties suggests that MSCs might induce lung repair, and this hypothesis is supported by animal models of emphysema.6,7 In a rat model of elastase-induced pulmonary emphysema, placement of biodegradable sheets coated with adipose tissue-derived MSCs on the cut surface of the remaining lung after lung volume reduction surgery (LVRS) resulted in significant regeneration of alveolar and endothelial cells in lung tissue when compared with control animals treated by LVRS and a sheet without MSCs.6 In another study in rats, infusion of BM-MSCs via the tail vein ameliorated papain-induced pulmonary emphysema, which was accompanied by suppression of alveolar cell apoptosis.7 However, in a large phase II study in patients with chronic obstructive pulmonary disease (COPD)/emphysema, allogeneic MSCs showed no effect on forced expiratory volume in one second (FEV1), the primary endpoint.
It remains to be established whether emphysematous tissue is repairable in humans with cigarette smoke-induced emphysema To develop a clinical experimental treatment program using autologous BM-MSC administration for patients with severe emphysema, we started with a phase I study to assess the safety and feasibility of intravenous administration of BM-MSC’s to subjects with severe emphysema. We evaluated standard WHO toxicity criteria for safety analysis as well as lung tissue responses possibly induced by BM-MSC’s.
Methods
Patients
Patient characteristics are shown in Table 1. In- and exclusion criteria for eligible patients are reported in the online supplement. In brief, patients (aged >40 years) had emphysema in both upper lung lobes with an equal distribution pattern in both lungs, as assessed by lung densitometry.8 Additionally, FEV1 was 40% predicted or lower. Patients had stopped smoking more than 6 months prior to screening.
Table 1.
Patient baseline characteristics
| Patient no. | Sex F/M | Age (years) | FEV1 in L (% pred) | Kco (% pred) | Perc15 (HU) | Weight (kg) | Length (m) |
|---|---|---|---|---|---|---|---|
| 1 | F | 48 | 0.62 (22) | 32 | −945 | 77 | 1.68 |
| 2 | F | 43 | 0.82 (35) | 41 | −970 | 51 | 1.52 |
| 3 | F | 49 | 1.21 (38) | 37 | −970 | 59 | 1.67 |
| 4 | M | 65 | 1.21 (40) | 42 | −953 | 85 | 1.71 |
| 5 | M | 58 | 1.20 (38) | 39 | −962 | 62 | 1.70 |
| 6 | F | 56 | 0.94 (30) | 36 | −967 | 75 | 1.62 |
| 7 | F | 61 | 0.45 (20) | — | −987 | 56 | 1.66 |
| 8 | M | 53 | 1.22 (40) | 41 | −973 | 74 | 1.71 |
| 9 | F | 51 | 0.96 (39) | 57 | −933 | 59 | 1.61 |
| 10 | M | 55 | 0.58 (16) | — | −988 | 65 | 1.78 |
Patient 5 was of Asian race, all others were Caucasian. In patient 7 and 10 only multiple breath analysis for gas transfer could be performed; Perc15 is CT-based lung density value of both lungs at the 15th percentile point, expressed in Hounsefield Units (HU). During the screening of patients who volunteered for the study we noticed that the inclusion of subjects who had emphysema equally distributed in the upper lung lobes was rather rare. For the histopathological analysis, we reasoned that equal distribution was of prime importance. This was the reason why the ethical board allowed higher Kco values coinciding with equally distributed emphysema calculated by CT scan-derived lung densitometry.
Study design
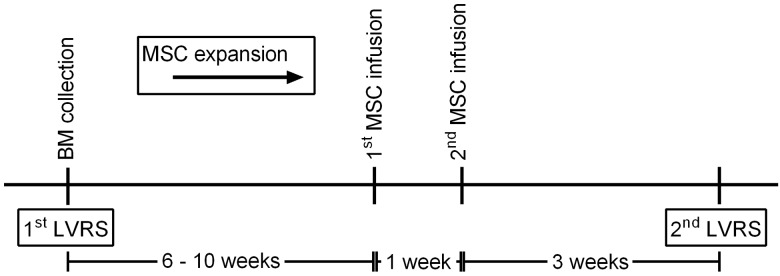
The study is a phase I, open-label prospective study. Eligible patients received two intravenous infusions of BM-MSCs (1–2 × 106 BM-MSCs/kg), 1 week apart. Standard WHO safety parameters were evaluated up to 3 weeks after the last infusion. Since emphysema is defined by histopathological criteria, we also investigated possible deleterious effects of BM-MSC treatment on lung tissue. Patients had bilateral LVRS by video-assisted thoracoscopy in two separate sessions. The side for the first surgical procedure was randomly assigned. During this session bone marrow was aspirated from the posterior iliac crest. The second surgical procedure on the contralateral lung was preceded by two intravenous infusions of BM-MSCs (1–2 × 106 BM-MSCs/kg, at passage 1–3 (see Table 2)), 4 and 3 weeks prior to the second surgery. Time between first and second LVRS was 12 ± 2 weeks (Figure 1). The occurrence of adverse events was monitored during the first 3 weeks after infusion, using WHO toxicity criteria. At baseline and at 12 months follow-up, we measured spirometry, gas transfer, lung volumes and computer tomography (CT)-derived lung densitometry.8
Table 2.
Overview of bone marrow aspirates and number of MSCs for infusions
| Patient no. | Bone marrow volume (ml) | Expansion cycles | No. of BM-MSCs (cells/kg bodyweight) | No. of BM-MSCs (total) |
|---|---|---|---|---|
| 1 | 140 | P2 | 1.7 × 106/kg | 130 × 106 |
| 2 | 183 | P1 | 2.1 × 106/kg | 108 × 106 |
| 3 | 127 | P1 | 1.2 × 106/kg | 70 × 106 |
| 4 | 290 | P2 | 0.9 × 106/kg | 75 × 106 |
| 5 | 85 | None | None | |
| 6 | 225 | P2 | 1.9 × 106/kg | 140 × 106 |
| 7 | 109 | P2 | 1.4 × 106/kg | 80 × 106 |
| 8 | 0 | None | None | |
| 9 | 128 | P2 | 1.0 × 106/kg | 60 × 106 |
| 10 | 139 | P3 | 1.6 × 106/kg | 105 × 106 |
Figure 1.
Schematic overview of the study design. Eligible patients had LVRS on two separate occasions. During the first LVRS bone marrow (BM) was collected, from which MSCs were isolated and expanded ex vivo. After clinical recovery, patients received two autologous MSC infusions, followed by the second LVRS procedure. This study protocol is based on previous clinical trials.4 The expansion of MSCs is described in the supplementary methods.
The study was approved by the Central Committee on Research Involving Human Subjects (CCMO) of The Netherlands and all study participants gave written consent. The study was registered at ClinicalTrials.gov as NCT01306513. The CCMO limited the total number of participants to 10 for safety reasons.
MSC expansion
Bone marrow aspiration, isolation and ex vivo expansion of BM-MSCs was performed as described previously (see online supplementary for details on MSC isolation, expansion and immunophenotyping).9 The number of expansion cycles and expanded BM-MSCs required to reach the target dose was assessed (see Table 2). MSCs were cryopreserved in 10% DMSO. After thawing, the MSC product was diluted with 50% (v/v) 0.9% saline and administered to the patient within 30 min.
Immunohistochemistry
Sections of emphysematous peripheral lung tissue were encoded for blinded analysis and stained with antibodies directed against CD3, CD4, CD8 (T-lymphocytes), CD20 (B-lymphocytes), CD31 (endothelial cells), CD68 (macrophages), Ki67 (cellular proliferation) or Surfactant Protein-C (SP-C, alveolar type II cells). Per section, alveolar septa were analysed in 15 randomly selected fields, summing up to 1000 µm total septum length per field. The number of positive cells was calculated per length of alveolar septa. CD31 and CD20 stainings were quantified calculating the density and area fraction of positively stained area within the alveolar septa. A detailed protocol is provided in the online supplementary.
Following analysis of tissue from the patient cohort, we retrieved archived paraffine-embedded resected lung tissue of three patients who had bilateral LVRS for emphysema in the past (1996–2010), with a similar time interval between the two surgical sessions as in this study.8 This tissue was stained and analysed for CD31 following the protocol as described.
PCR analysis of lung tissue
Peripheral lung tissue (5 × 5 × 5 mm) was frozen in RNA-later. RNA extraction and cDNA synthesis was performed following the protocol described in the online supplementary. Gene expression of markers for proliferation, fibrosis, epithelial and vascular cells, growth factors and immune mediators was assessed by qPCR as described in the online supplement. The relative expression compared to housekeeping genes was calculated.
Statistical analysis
Results are described as mean ± SD unless depicted otherwise; data in graphs are presented as mean with individual data points. Paired data analysis was performed using Wilcoxon signed rank test (GraphPad Prism 6; GraphPad Software Inc., La Jolla, CA). Subjects with missing data are shown in the graphs and tables, but excluded from statistical analysis. Differences at a P values below 0.05 were considered statistically significant.
Results
Feasibility and safety
Seven patients completed the study protocol. Bone marrow could be aspirated from nine patients with a mean volume of 158 ml ( ± 64 ml), and in eight patients the targeted total MSC number was obtained after three expansion cycles (Table 2). No bone marrow could be aspirated from patient number 8 and very poor expansion of MSCs occurred in cultures from patient 5, resulting in withdrawal from the protocol. Patient number 7 could not be evaluated at the histological level. A second surgical procedure was not possible due to persistent air leak after the first LVRS (see below).
In the first 48 h after both BM-MSC infusions vital functions remained stable in all patients and WHO-toxicity criteria showed no change. At 3 weeks after the second BM-MSC infusion, still no toxicity was observed. Patients reported no symptoms that could be related to the infusions at 3 weeks after the second infusion, the day before the second LVRS.
Clinical parameters and follow-up
Post-surgical air leak in days was similar between the initial and the second procedure (8.3 ± 3.4 vs. 8.9 ± 3.1 days). Patient number 7 had persistent air leak and we decided to administer autologous BM-MSCs at Week 5 and 6 after the first LVRS with the opportunity to induce beneficial effects on wound healing. However, air leak persisted and mandated second surgery (pleural rubbing) on the initial side, resulting in withdrawal from the study protocol. At Week 14 the patient was successfully treated with endobronchial valves, followed by hospital discharge at Week 17.
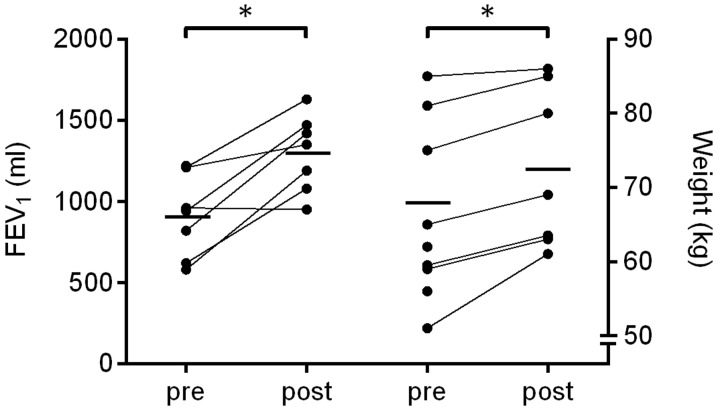
At 12-months follow-up, the FEV1 was increased by 390 ml ± 240 ml (P = 0.03) compared with baseline (Figure 2). Residual volume decreased by 540 ± 145 ml (P = 0.053) and gas transfer was not significantly different. The difference in CT-derived lung density at 15th percentile point (Perc15) obtained from a chest CT-scan prior to the first LVRS and 1-year after the second LVRS was 7.3 ± 4.3 g/l (P = 0.013). These results are comparable to our results reported previously.8 The weight of all patients increased significantly, on average with 4.6 kg (range 1––10 kg; P = 0.016) (Figure 2).
Figure 2.
FEV1 and weight measurements at baseline and follow-up. FEV1 (left) and weight (right) were measured in patients with severe emphysema at baseline prior to the first LVRS procedure (pre), and at 1-year follow-up (post). Individual data points represent individual patients; means are shown as horizontal bars. *P < 0.05.
Immunohistochemical analysis
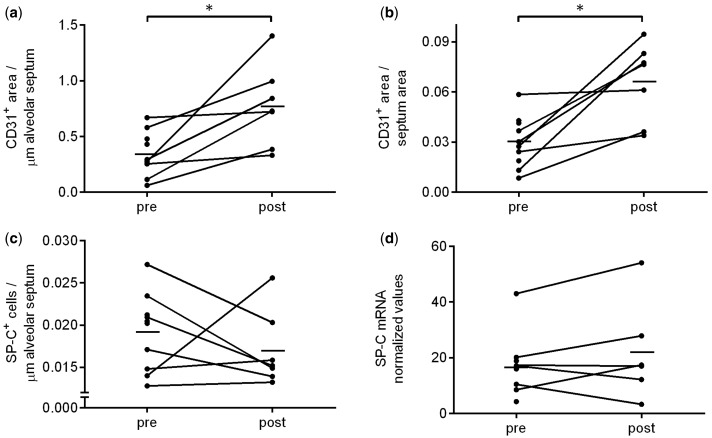
Immunohistochemical (IHC) stainings for cell markers and proliferation markers were analysed in seven paired samples of resected peripheral lung tissue, obtained during initial and second surgery (pre- and post BM-MSC infusion).
The CD31+ (endothelial cells) area within the alveolar septa was 3-fold higher post LVRS + BM-MSC infusion (P = 0.016), corrected for alveolar septum length as well as for total alveolar area (Figure 3a and b and online supplementary Figure S1). CD31 expression was not significantly changed in alveolar septa of the historic controls (online supplementary Figure S2). No changes were observed for SP-C (alveolar type II cells) (Figure 3c).
Figure 3.
CD31 and SP-C expression analysis in lung tissue before and after MSC infusion. Immunohistochemistry and mRNA expression performed on lung tissue obtained during first LVRS (pre) and a second LVRS procedure that was preceded by two MSC infusions (post). Quantification of CD31 IHC staining with (a) CD31 density, normalized by length of alveolar septa; and (b) CD31 area fraction, normalized by area of alveolar septa. (c) Quantification of IHC staining of SP-C (alveolar type II cell marker) normalized by length of alveolar septa. (d) mRNA expression of SP-C. Data in graph represent mean and individual data points. Paired data n = 7 for IHC and n = 6 for mRNA, * P < 0.05.
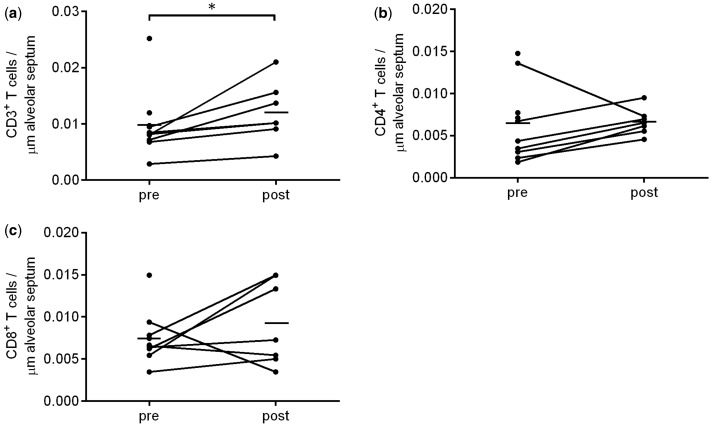
The number of CD3+ T cells in alveolar septa was significantly higher after LVRS + BM-MSC infusion compared to before (P = 0.016) (Figure 4a). This was accompanied by increased numbers of CD4+ T cells in alveolar septa post LVRS + BM-MSC infusion in all patients, except one (P = 0.30; calculated as fold change P = 0.047) (Figure 4b, online supplementary Figure S3). The number of CD8+ T cells did not change (P = 0.22) (Figure 4c). No change was observed in the number CD68+ cells (macrophages) (online supplementary Figure S3).
Figure 4.
IHC analysis of T cell markers pre- and post- MSC infusion. The number of CD3+, CD4+ and CD8+ T cells was assessed in surgical specimen obtained before and after MSC infusion. Quantification of (a) CD3, (b) CD4 and (c) CD8, expressed per length of alveolar septa. Data in graph represent mean (horizontal bar) and individual data points. Paired data n = 7, *P < 0.05.
The number of CD20+ B cell aggregates varied substantially between patients, but there were no significant differences before and after LVRS + MSC infusions. In one patient no aggregates were observed in either of the tissue samples obtained, therefore this patient was excluded from statistical analysis for CD20. The total CD20+ area did not change significantly (P = 0.16; online supplementary Figure S3).
Since only very few Ki67+ cells were observed, this staining was not further quantified.
Gene expression analysis
From six patients mRNA expression data of paired lung tissue samples (pre- and post BM-MSC infusion) were obtained. mRNA isolation from one sample failed because of tissue degradation. Quantitative real time PCR was used to analyse growth factors, immune mediators, proliferation markers and lung cell markers.mRNA expression of SP-C was not altered (Figure 3d) after LVRS + BM-MSC infusion. No changes were observed in the proliferation markers Cyclin D1 (CCDN1) and Cyclin Dependant Kinase Inhibitor 1A (CDKN1A) (online supplementary Figure S4). Genes encoding epithelial cell markers and fibrosis markers (online supplementary Figure S5a), growth factors, including angiogenic growth factors (Figure S5b), and immune mediators (Figure S5c) did not change significantly. Interestingly, a trend towards higher mRNA expression of IL10 and TSG6 in tissue obtained after LVRS + BM-MSC infusion was observed, but this difference did not reach statistical significance (P = 0.06).mRNA expression of Platelet Endothelial Cell Adhesion Molecule 1 (PECAM1, the gene encoding for CD31) was not increased following LVRS + BM-MSCs (Figure S6a). Other vascular markers (i.e. Von Willebrand Factor (VWF) and Vascular Endothelial Growth Factor Receptor 2 (VEGFR2)) were also not significantly changed (online supplementary Figure S6b and c).
Discussion
In this study, we show that infusion of autologous BM-MSCs 3 and 4 weeks prior to LVRS in patients with severe emphysema is feasible and safe. By histological analysis of lung tissue surgically removed from the most severely affected emphysematous areas, we found no evidence of induction of fibrotic responses in the lung by MSCs. There was neither an increase in α-SMA or Connective Tissue Growth Factor mRNA expression, nor in the number of Ki67 positive cells or in mRNA expression of proliferation markers in lung homogenates obtained after LVRS + BM-MSC infusion. We observed no increase in pulmonary fibrosis by CT-derived parenchymal analysis at 1-year follow-up. Treatment by LVRS and MSCs was accompanied by a 3-fold increased expression of the endothelial cell marker CD31 in the alveolar septa of emphysematous lung tissue. This increased tissue expression of CD31 was not accompanied by an increase in mRNA expression of CD31/PECAM1 or other vascular markers. Following LVRS and BM-MSC treatment, CD3+ T cells were increased almost 2-fold in lung tissue sections, but mRNA expression of various immune mediators in lung tissue homogenates were not changed.
The BM-MSC target dosage of 1–2 × 106 cells/kg bodyweight used in this study has been selected on the basis of clinical experience reported in the literature, including our own.2,4 In this study, autologous BM-MSC administration at this dosage to patients with severe to very severe COPD appeared to be safe and well tolerated, which is in line with a prior clinical trial conducted using allogeneic MSC in moderate and severe COPD patients.10 We noted no adverse events and the observed changes in FEV1 and lung densitometry after 1-year follow-up are comparable with a historic cohort of LVRS patients.8 We observed a significant increase in body weight in our patients. Such an increase after BM-MSC treatment has not been reported before, and it is more likely that it resulted from the effects of LVRS than from the BM-MSC infusions.11
The hallmark of pulmonary emphysema is the destruction of alveoli and therefore we focussed our analysis on changes in alveolar septa.12 Three and four weeks after MSC infusion we obtained no clinical, microscopic or molecular evidence for repair of emphysematous lesions. Although no changes were observed in alveolar type II cells as identified by staining for SP-C, we did observe an effect on CD31 in the alveolar septa after BM-MSC infusions, despite the low number of study participants. Our study protocol did not include a control group due to its design as a phase I safety and feasibility study. We cannot exclude a possible carry-over effect by the first LVRS on CD31 responsiveness in the blood vessels around alveoli. Studies addressing this issue in humans are lacking, but a study in rodents analysing stromal cells in emphysema did not reveal surgery-induced effects on vascularization, as expressed by the vascular density.6 Our posthoc analysis using archived tissue specimen of three patients who had bilateral LVRS with no specific treatments in between the two surgical sessions showed no significant change in CD31 expression in alveolar septae. This suggests a role for MSC-induced effects on CD31 expression.
CD31 is widely used as a marker for endothelial cells and endothelial damage is a prominent characteristic of emphysema. This has been demonstrated by the presence of increased levels of circulating endothelial micro-particles reflecting endothelial damage in COPD.13,14 In mice, the contribution of endothelial damage to the development of emphysema has also been established, as impairment of endothelial cell function by inhibition of the VEGF receptor or administration of anti-endothelial antibodies resulted in emphysema development.15 Conversely, whether the increased expression of CD31 in alveolar septa reflects the number of endothelial cells or has functional effects in alveolar septa remains to be investigated.16 Since CD31 (or PECAM1) plays a central role in endothelial cell migration and angiogenesis,17 endothelial cell-cell interaction as well as in downstream anti-apoptotic effects,18 the increased expression of CD31 as seen in our patients may indicate a protective and/or repair response against further tissue destruction. Furthermore, whereas CD31 is generally considered and used as an endothelial cell marker, its expression is not restricted to endothelial cells alone. Therefore, further randomized, placebo-controlled studies in a larger cohort and using additional markers are needed to explore this finding.
In addition to the increase in CD31, we also observed significant increase of CD3 + and CD4 + T cells that was observed in randomly selected parenchymal tissue sections. The role of T-cells in the pathogenesis of emphysema is not fully clear, and in view of the before mentioned limitations of our study design we decided to not further investigate this observation in the historic cohort.
LVRS itself has a substantial effect on e.g. FEV1, which likely could not be further enhanced by the BM-MSC treatment.8 A randomized placebo-controlled clinical trial by Weiss et al.10 showed no statistically significant differences in FEV1 or FEV1% predicted during 2 years follow-up after 4 monthly administrations of allogeneic BM-MSCs, nor did they observe differences between the groups in FVC, FVC% predicted, total lung capacity, or carbon monoxide diffusing capacity from baseline to 1 year or 2 years. The authors questioned the treatment regimen, which was adopted from other clinical trials.
Since we observed an increase in CD31 and CD3 + cells in a relatively short period after MSC infusions, it appears reasonable to further investigate MSCs as a treatment for emphysema, exploring other MSC treatment regimens in a placebo-controlled study.
In conclusion, we demonstrated that infusion of autologous MSCs to patients with severe emphysema is safe and we showed no signs of development of fibrosis in lung tissue 3–4 weeks after MSC infusion, nor in CT-derived parenchymal analysis at 1-year follow-up.
Supplementary material
Supplementary material is available at QJMED online.
Funding
This work was supported by an LUMC institutional grant
Acknowledgements
The authors would like to thank Vera van Rijn for technical assistance with the preparation of tissue sections, Annemarie van Schadewijk for assistance with the IHC stainings, Yvonne de Mooij-Eijk for staining the sections and performing most of the analysis, Jasmijn Schrumpf for technical assistance in tissue mRNA extraction and running qPCRs (all from department of Pulmonology, Leiden University Medical Center, the Netherland), and Ruy Pires-Neto for his advice regarding the IHC analysis (from department of Pathology, São Paulo University Medical School, São Paulo, Brazil).
Conflict of interest: None declared.
References
- 1.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, et al. Multilineage potential of adult human mesenchymal stem cells. Science 1999; 284:143–7. [DOI] [PubMed] [Google Scholar]
- 2.Bernardo ME, Fibbe WE. Mesenchymal stromal cells: sensors and switchers of inflammation. Cell Stem Cell 13:392–402. [DOI] [PubMed] [Google Scholar]
- 3.Petrella F, Acocella F, Barberis M, Bellomi M, Brizzola S, Donghi S, et al. Airway fistula closure after stem-cell infusion. N Engl J Med 2014; 372:96–7. [DOI] [PubMed] [Google Scholar]
- 4.Le Blanc K, Frassoni F, Ball L, Locatelli F, Roelofs H, Lewis I, et al. Mesenchymal stem cells for treatment of steroid-resistant, severe, acute graft-versus-host disease: a phase II study. Lancet 2008; 371:1579–86. [DOI] [PubMed] [Google Scholar]
- 5.Molendijk I, Bonsing BA, Roelofs H, Peeters KC, Wasser MN, Dijkstra G, et al. Allogeneic bone marrow-derived mesenchymal stromal cells promote healing of refractory perianal fistulas in patients with crohn's disease. Gastroenterology 2015; 149:918–27. [DOI] [PubMed] [Google Scholar]
- 6.Shigemura N, Okumura M, Mizuno S, Imanishi Y, Matsuyama A, Shiono H, et al. Lung tissue engineering technique with adipose stromal cells improves surgical outcome for pulmonary emphysema. Am J Respir Crit Care Med 2006; 174:1199–205. [DOI] [PubMed] [Google Scholar]
- 7.Zhen G, Liu H, Gu N, Zhang H, Xu Y, Zhang Z. Mesenchymal stem cells transplantation protects against rat pulmonary emphysema. Front Biosci 2008; 13:3415–22. [DOI] [PubMed] [Google Scholar]
- 8.Stolk J, Versteegh MI, Montenij LJ, Bakker ME, Grebski E, Tutic M, et al. Densitometry for assessment of effect of lung volume reduction surgery for emphysema. Eur Respir J 2007; 29:1138–43. [DOI] [PubMed] [Google Scholar]
- 9.Duijvestein M, Vos AC, Roelofs H, Wildenberg ME, Wendrich BB, Verspaget HW, et al. Autologous bone marrow-derived mesenchymal stromal cell treatment for refractory luminal Crohn's disease: results of a phase I study. Gut 2010; 59:1662–9. [DOI] [PubMed] [Google Scholar]
- 10.Weiss DJ, Casaburi R, Flannery R, LeRoux-Williams M, Tashkin DP. A placebo-controlled, randomized trial of mesenchymal stem cells in COPD. Chest 2013; 143:1590–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim V, Kretschman DM, Sternberg AL, DeCamp MM, Jr, Criner GJ. Weight gain after lung reduction surgery is related to improved lung function and ventilatory efficiency. Am J Respir Crit Care Med 2012; 186:1109–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McDonough JE, Yuan R, Suzuki M, Seyednejad N, Elliott WM, Sanchez PG, et al. Small-airway obstruction and emphysema in chronic obstructive pulmonary disease. N Engl J Med 2011; 365:1567–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomashow MA, Shimbo D, Parikh MA, Hoffman EA, Vogel-Claussen J, Hueper K, et al. Endothelial microparticles in mild chronic obstructive pulmonary disease and emphysema. The multi-ethnic study of atherosclerosis chronic obstructive pulmonary disease study. Am J Respir Crit Care Med 2013; 188:60–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takahashi T, Kobayashi S, Fujino N, Suzuki T, Ota C, He M, et al. Increased circulating endothelial microparticles in COPD patients: a potential biomarker for COPD exacerbation susceptibility. Thorax 2012; 67:1067–74. [DOI] [PubMed] [Google Scholar]
- 15.Tuder RM, Zhen L, Cho CY, Taraseviciene-Stewart L, Kasahara Y, Salvemini D, et al. Oxidative stress and apoptosis interact and cause emphysema due to vascular endothelial growth factor receptor blockade. Am J Respir Cell Mol Biol 2003; 29:88–97. [DOI] [PubMed] [Google Scholar]
- 16.Privratsky J, Newman P. PECAM-1: regulator of endothelial junctional integrity. Cell Tissue Res 2014; 355:607–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gratzinger D, Canosa S, Engelhardt B, Madri JA. Platelet endothelial cell adhesion molecule-1 modulates endothelial cell motility through the small G-protein Rho. Faseb J 2003; 17:1458–69. [DOI] [PubMed] [Google Scholar]
- 18.Kitazume S, Imamaki R, Ogawa K, Komi Y, Futakawa S, Kojima S, et al. Alpha2,6-sialic acid on platelet endothelial cell adhesion molecule (PECAM) regulates its homophilic interactions and downstream antiapoptotic signaling. J Biol Chem 2010; 285:6515–2. [DOI] [PMC free article] [PubMed] [Google Scholar]