Abstract
Even though intravenous thrombolysis with tissue plasminogen activator (IV tPA) is the standard of care in acute ischemic stroke, its use in pregnancy is not clearly defined. Mechanical thrombectomy devices can be an option; however, literature on the use of such mechanical devices in stroke in pregnancy is lacking. Here we describe two cases that developed acute embolic stroke during pregnancy who were successfully treated by mechanical clot retrieval using the Penumbra system 28 (Penumbra Inc., Alameda, California, USA). To the best of our knowledge, these are the only case reports on the use of the Penumbra device in pregnant patients with acute ischemic stroke.
Keywords: Mechanical thrombectomy in pregnancy, penumbra system, stroke in pregnancy
Introduction
Intravenous thrombolysis with tissue plasminogen activator (IV tPA) is the standard of care for eligible patients with ischemic strokes presenting within the 4.5-hour window.[1,2] Though there are several reports of pregnant patients being successfully treated with IV tPA in the setting of acute ischemic stroke,[3,4] in the current guidelines, pregnancy remains a relative exclusion criterion for intravenous tPA.[5] Even though tPA does not cross the placenta, there are many possible potential complications in pregnancy, which can limit its use. Uterine bleeding can occur, leading to premature labor and placental abruption. If there is a need for emergency cesarean section, tPA can increase the risk of bleeding. If the patient goes into labor, there can be increased bleeding during parturition. Hence, tPA should be used in pregnant patients with caution.
A study looking at the risk of hemorrhage with thrombolytics use in pregnancy for various conditions found an overall maternal hemorrhagic complications rate of 8%.[6] In 28 pregnant patients who received thrombolytic therapy with rt-PA for various indications, maternal mortality was 7% and fetal mortality was 23%.[4] In another series where eight pregnant women with AIS was treated with IV thrombolysis with rt-PA or urokinase, 50% of the patients had a bleeding complication and only two babies were delivered healthy.[7] Intra-arterial fibrinolysis and mechanical clot retrieval devices are another option in patients who have risk of intravenous thrombolysis.[8] The Merci, Penumbra System, Solitaire FR, and Trevo thrombectomy devices are the mechanical devices commonly used alone or in combination with local pharmacological fibrinolysis.[9,10,11] However the literature on the use of such mechanical devices in stroke in pregnancy is lacking. Here we describe two cases of stroke in pregnancy that was successfully treated with Penumbra System.
Case Report
Case 1 [Figure 1]
Figure 1.

(a) DWI image showing a well defined infarct involving the right lateral lenticulostriate territory. (b) MRA and (c) DSA showing cut off of the right MCA, M1 segment (white arrows) (d) The Penumbra device deployed in the occluded segment.(e) Post procedure DSA showing partial recanalisation of the MCA with opacification of the inferior branch.(f) Imaging after 24 hours showing mild extension of the infarct to involve the right insula, (g) Evidence of good recanalisation on MRA of the right MCA
A 24-year-old lady who was in the third trimester (first pregnancy) presented to us with acute left hemiplegia. Six years back, she had a mitral valve replacement (3 M Starr Edwards valve) for rheumatic heart disease (indication being severe mitral regurgitation and moderate tricuspid regurgitation). She has been on oral anticoagulation (OAC) since then. One week before the stroke as she was approaching term, the OAC was changed to low molecular weight heparin.
She had left-sided hemi neglect and was in altered sensorium. The National Institutes of Health Stroke Scale (NIHS) was 20. She presented to us within one hour of onset of her symptoms.
A magnetic resonance imaging (MRI) stroke protocol, which included the following sequences ¾ diffusion weighted imaging (DWI), apparent diffusion coefficient (ADC), fluid-attenuated inversion recovery (FLAIR) and magnetic resonance angiography (MRA) was done. The DWI and ADC images showed an infarct involving the right lateral lenticulostriate territory. The MRA showed an abrupt cut-off of the proximal R middle cerebral artery. The patient had features of an evolving malignant middle cerebral artery infarction with hemi neglect and depressed sensorium, suggesting a clinical radiological mismatch. To save the remaining MCA territory, it was decided to take her up for a revascularization.
After obtaining right common femoral arterial access, a diagnostic right common carotid angiogram using a 4F catheter (Vertebral glide catheter, Terumo) was done. The internal carotid artery was patent but there was complete occlusion of M1 segment of right MCA. The vertebral glide catheter was exchanged for a 6F guiding catheter, the tip of which was kept in cervical segment of right internal carotid artery. Penumbra system 28 (Penumbra Inc., Alameda, California, USA) was advanced into the M1 segment of right MCA to the site of occlusion. Mechanical thrombectomy with separator using the Penumbra pump was carried out over a period of 15 minutes. Final check angiogram showed partial recanalization.
Immediately after the procedure, the patient's motor power improved to grade 3, her hemi neglect resolved and sensorium became normal (NIHS improved to 12). Over the next three days, her power improved to grade 4. The NIHS at the time of discharge was 1.
ECHO showed normally functioning mitral valve with no thrombus. Holter was normal. She was advised to continue oral anti-coagulation and INR maintained between 2.5 and 3.5.
The patient subsequently had a normal vaginal delivery. Her oral anticoagulants were continued. At six months follow-up, the Rankin score was 0.
Case 2 [Figure 2]
Figure 2.
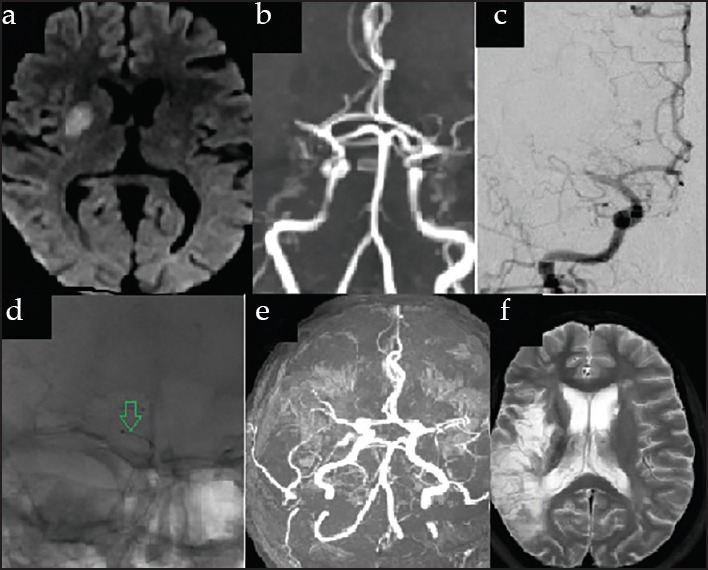
(a) DWI MRI images showing a well defined infarct involving the right putamen, (b) MRA and (C) DSA showing cut off of the right MCA in the proximal M1 segment, (c) The PENUMBRA Catheter (green arrow) deployed in the occluded segment (D) follow MRA showing partial recanalisation of the right MCA (d) T2 axial image after 1 month showing extension of infarct to involve only the territory of the superior branch of the right MCA
A 28-year primigravid at 37 weeks of gestation was admitted to the hospital for an elective lower segment cesarean section (LSCS) with the indications being severe intrauterine growth retardation (IUGR) and unfavorable cervix. She was a case of rheumatic heart disease (mitral stenosis) and a mitral valve replacement (MVR) was done nine years ago. She was on oral anticoagulant, which was changed over to low molecular weight heparin (LMWH) after her admission for the planned LSCS. She developed a sudden dense left hemiplegia and became drowsy (NIHS-21).
MRI was done after 80 minutes of her symptoms showed infarct involving the right putamen on the DWI and ADC. There was cut off of the right MCA in the proximal M1 segment. The FLAIR axial image was showing slow flow within the right MCA branches.
She was taken up for revascularization. The procedure was done similar to case 1. The Penumbra device was used along with the separator for the duration of 30 minutes. Partial recanalization was achieved.
Post procedure the patient became fully conscious and the power improved to grade 3. She was restarted on LMWH. ECHO showed normally functioning mitral valve with no thrombus.
After 10 days, she was taken up for an emergency LSCS under spinal anesthesia and delivered a normal baby girl. She was restarted on oral anticoagulants. At discharge, she had improved to an NIHS of 4. At six months follow-up, her modified Rankin score was 2 (slight disability; unable to carry out all previous activities, but able to look after own affairs without assistance).
Discussion
A number of mechanical thrombectomy devices (e. g., the Merci Retriever, the Penumbra System, the Solitaire Flow Restoration Device, and the Trevo Retriever) are approved in the United States and Europe for clot removal within eight hours of acute stroke symptom onset in selected patients. However the pivotal stroke trials of both the Penumbra and the MERCI devices did not recruit pregnant patients in the trial.[9,10]
Even though the role and advantage of endovascular therapy over systemic thrombolysis for acute ischemic stroke is still being debated,[12] there is a subsection of patients with AIS with contraindications for systemic thrombolysis who may benefit.[13]
In both our cases apart from being pregnant there were other relative contraindications. Both the patients were on LMWH, the NIHS was high (> 20). One patient was admitted for an LSCS. Also both the cases had M1 occlusions where recanalization rates and good outcomes with systemic thrombolysis with tPA is poor.[14]
In both our patients the stroke occurred while they were switched over to LMWH. This was similar to the observation in another study wherein all patients' thrombosis of cardiac valve prostheses occurred after switching from warfarin to heparin.[4]
Conclusion
Endovascular therapy with mechanical thrombectomy devices can be considered as a safe option for the treatment of acute ischemic stroke occurring in pregnancy especially if the patient has other added contraindications/relative contraindications for receiving systemic thrombolytic therapy with IV tPA.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333:1581–7. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 2.Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–29. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 3.Aleu A, Mellado P, Lichy C, Köhrmann M, Schellinger PD. Hemorrhagic complications after off-label thrombolysis for ischemic stroke. Stroke. 2007;38:417–22. doi: 10.1161/01.STR.0000254504.71955.05. [DOI] [PubMed] [Google Scholar]
- 4.Leonhardt G, Gaul C, Nietsch HH, Buerke M, Schleussner E. Thrombolytic therapy in pregnancy. J Thromb Thrombolysis. 2006;21:271–6. doi: 10.1007/s11239-006-5709-z. [DOI] [PubMed] [Google Scholar]
- 5.Jauch EC, Saver JL, Adams HP, Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 6.Turrentine MA, Braems G, Ramirez MM. Use of thrombolytics for the treatment of thromboembolic disease during pregnancy. Obstet Gynecol Surv. 1995;50:534–41. doi: 10.1097/00006254-199507000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Murugappan A, Coplin WM, Al-Sadat AN, McAllen KJ, Schwamm LH, Wechsler LR, et al. Thrombolytic therapy of acute ischemic stroke during pregnancy. Neurology. 2006;66:768–70. doi: 10.1212/01.wnl.0000201272.90216.15. [DOI] [PubMed] [Google Scholar]
- 8.Johnson DM, Kramer DC, Cohen E, Rochon M, Rosner M, Weinberger J. Thrombolytic therapy for acute stroke in late pregnancy with intra-arterial recombinant tissue plasminogen activator. Stroke. 2005;36:e53–5. doi: 10.1161/01.str.0000166203.27135.27. [DOI] [PubMed] [Google Scholar]
- 9.Penumbra Pivotal Stroke Trial Investigators. The penumbra pivotal stroke trial: Safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009;40:2761–8. doi: 10.1161/STROKEAHA.108.544957. [DOI] [PubMed] [Google Scholar]
- 10.Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al. Multi MERCI Investigators. Mechanical thrombectomy for acute ischemicstroke: Final results of the Multi MERCI trial. Stroke. 2008;39:1205–12. doi: 10.1161/STROKEAHA.107.497115. [DOI] [PubMed] [Google Scholar]
- 11.Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. SWIFT Trialists. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): A randomised, parallel-group, non-inferiority trial. Lancet. 2012;380:1241–9. doi: 10.1016/S0140-6736(12)61384-1. [DOI] [PubMed] [Google Scholar]
- 12.Singh B, Parsaik AK, Prokop LJ, Mittal MK. Endovascular therapy for acute ischemic stroke: A systematic review and meta-analysis. Mayo Clin Proc. 2013;88:1056–65. doi: 10.1016/j.mayocp.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Demchuk AM. Yes, intravenous thrombolysis should be administered in pregnancy when other clinical and imaging factors are favorable. Stroke. 2013;44:864–5. doi: 10.1161/STROKEAHA.111.000134. [DOI] [PubMed] [Google Scholar]
- 14.von Kummer R, Holle R, Rosin L, Forsting M, Hacke W. Does arterial recanalization improve clinical outcome in carotid territory stroke? Stroke. 1995;26:581–7. doi: 10.1161/01.str.26.4.581. [DOI] [PubMed] [Google Scholar]


