Abstract
Background
Oral mucositis is one of the irritating side effects of chemotherapy in patients undergoing bone marrow transplantation. However, up until now, the common methods of oral mucositis therapy have failed to show significant effects.
Objectives
The aim of this study was to investigate the effects of local cryotherapy on the intensity of chemotherapy-induced oral mucositis in autologous bone marrow transplantation patients.
Patients and Methods
In this single, blinded, randomized clinical trial, 29 patients undergoing stem cell transplantation in Iran were selected by convenience sampling, and randomly allocated to control (n = 13) and intervention groups (n = 16). In the intervention group, cryotherapy was applied, while the control group received a normal saline mouthwash. The severity of the mucositis and neutrophil rate were investigated in five periods, based on the world health organization (WHO) scales. The data were analyzed using descriptive statistics, the Mann-Whitney test, repeated measures analysis of variance (ANOVA), and linear regression.
Results
In both groups, the mucositis reached its peak intensity on the 7th day, and the least intensity was obtained on the 21st day. The neutrophil rate reached the minimum value on the 7th day, then increased up to the 21st day. The two groups showed no significant differences between the mucositis severity on the 14th and 21st days (P = 0.164), while the severity of the mucositis in the cryotherapy group was significantly less than that in the saline mouthwash group (1.81 < 2.54 and 0.13 < 0.92, respectively) on the 7th and 14th days (P < 0.05). There was no significant difference in the neutrophil rate between the groups.
Conclusions
The results showed that cryotherapy is more effective than the saline mouthwash in reducing the severity of mucositis. This method is recommended for the prevention of mucositis in bone marrow transplantation.
Keywords: Chemotherapy, Mucositis, Stem Cell Transplantation, Autologous, Cryotherapy, Normal Saline
1. Background
Today, cancer is one of the major problems in the healthcare system, especially in developing countries such as Iran. Despite numerous innovative therapeutic techniques, high-dose chemotherapy and bone marrow transplantation remain the best options for patients. Nowadays, bone marrow transplantation is performed using both allogeneic and autologous methods, and nearly fifteen thousand people worldwide have been treated with bone marrow transplantation (1).
Stem cell transplantation is used in cases where the patient is in a remission state, and the disease has recurred after initial treatment. Moreover, it is also used when patient is in a remission state, and there is no large change in the recurrence (2). High dose chemotherapy in autologous stem cell transplantation is one of the standard treatments (3).
The rate and severity of complications after transplantation are influenced by the conditioning regimen before transplantation, which consists of total body irradiation usually combined with chemotherapy, or absolute chemotherapy (4). This treatment affects multiple systems and is followed by side effects such as infection, bleeding, nausea, fatigue, loss of appetite, mouth sores, and skin reactions (5).
Annually, about 40,000 patients in the US experience acute or chronic oral complications during chemotherapy, and about 40% of the patients will develop some degree of oral mucositis (6). Mucositis is the inflammation and ulceration of the superficial membrane overlying the digestive tract from the mouth to the anus. When the inflammation of the mucous involves the mouth and oral oropharyngeal segment, it is called oral mucositis (7). Accordingly, mucositis is a major chemotherapy-induced problem that may cause disturbing pain, the inability to tolerate food, infection, and negative effects on the quality of life. An increased treatment period, increased cost of treatment, and prolonged treatment are among the other side effects. Oral mucositis also causes psychological distress in the patients, and interferes with their physical and mental health status (8).
Thus far, no definite method for the prevention and treatment of oral mucositis has been provided. However, several measures have been recommended, including honey (9), mouthwashes such as allopurinol and saline (10), and sodium bicarbonate (11). In several studies, cryotherapy has been evaluated as one of the proposed methods in the treatment of mucositis. Studies by Heydari et al. (12) (2012) in Iran, Katranci (13) (2011) in Turkey, Svanberg et al. (14) (2007) in Sweden, and other studies have suggested using this method due to better efficacy and fewer side effects. The application of ice or cold water in the mouth is among the conventional methods of cryotherapy; in this case, the patients use ice cubes before, during, and shortly after chemotherapy (15). However, one of the limitations of these studies is the small sample size, and it is always recommended to increase the samples of studies (16, 17).
Overall, there is a knowledge gap with regard to the effects of cryotherapy on chemotherapy-induced oral mucositis in patients undergoing bone marrow transplantation.
2. Objectives
Therefore, the purpose of this study was to evaluate the effects of local oral cryotherapy on the incidence of chemotherapy-induced oral mucositis in patients undergoing autologous transplantation.
3. Patients and Methods
This single, blinded, randomized clinical trial with a control group was conducted in the bone marrow transplant ward of the Namazi specialized teaching and referral hospital, a 750 bed affiliate to Shiraz Medical University in Iran. In order to determine the sample size, the primary data, including the mean and standard deviation of the main variable of the study (mucositis), was gathered based on a pilot study in which five patients in two groups were measured at different times. Consequently, by a confidence level of 95% and power of 80%, the mean scores for the cryotherapy were 0.59 and 1.1 in the two groups. The minimum sample size obtained was 10 using the G*Power software package. By considering a 40% sample attribution, the minimum sample size was raised to 14 patients per group; therefore, considering the low incidence of bone marrow transplant cases, all of the patients meeting the inclusion criteria were included in the study. It should be noted that from April to September of 2013, all of the patients undergoing autologous transplantation in this center were considered as samples (n = 52), among which 33 patients met the criteria for the study.
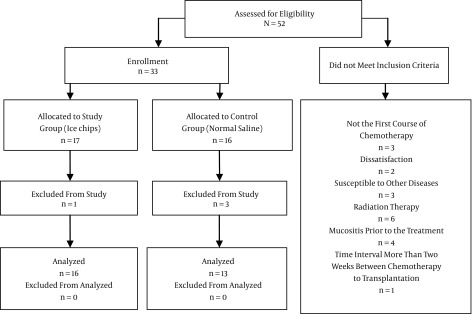
The patients were randomly allocated into control and intervention groups using size-2 random blocks, and based on a 1:1 allocation ratio, random numbers were generated by “Random Allocation Software”. The intervention group contained 17 patients undergoing cryotherapy, and the control group had 16 patients using normal saline mouthwash oral care. Due to fever, four patients were excluded during the study (Figure 1).
Figure 1. Flow Diagram of Trial.
Since the sample size was low, the bootstrap method was used to develop the available data and reduce the bias. In this stage, some of the samples were randomly selected among the available data, with replacement. Using the SPSS software. Melphalan was used in those patients with Hodgkin’s and non-Hodgkin’s transplantations, and in multiple myeloma transplantations, drugs such as melphalan, cytarabine, etoposide, and lomustine were used.
The inclusion criteria were full consciousness, suffering Hodgkin’s or non-Hodgkin’s lymphoma or multiple myeloma, good oral health before treatment, isolation in a separate room, similar basic chemotherapy, being in the first course of chemotherapy, and an autologous treatment protocol. The exclusion criteria were patient dissatisfaction, loss of consciousness, susceptibility to other diseases during treatment which disrupt the continuance of treatment, use of analgesics continuously before the study, combined therapies (such as radiation therapy) at the time of the study, fever, neutropenia and mucositis prior to the treatment, respiratory diseases, oral infections, systemic diseases affecting the oral status (particularly the periodontal tissues), a time interval of more than two weeks between the chemotherapy and transplantation, and finally, changes in the treatment protocol during the study.
First, the demographic and clinical data were collected. Then, the control group received normal saline mouthwash at the first dose of chemotherapy, and the intervention group used ice packs instead of normal saline to improve the oral mucositis. The ice packs were prepared specifically for each patient in the freezer using blocks of disposable nylon and clean mineral water from the fridge. In the cryotherapy group, five minutes before, during, and after each dose of chemotherapy, ice cubes were placed in the patient’s mouth to cool the oral cavity, and kept there as long as the patient could tolerate it. Initially, the ice cubes were used continuously, once, for thirty minutes. Then, with a maximum of a twenty minute break, using the ice began again for the next thirty minutes, and continued up to five minutes after the completion of the chemotherapy. However, the heating sensation in the mouth for less than twenty minutes was considered to be a factor in the reuse of the ice. Ice cubes as an ice mold which measured about three by four centimeters in a sterile container were prepared for the patients.
In the normal saline mouthwash group, based on the therapeutic protocol, 30 - 50 cc of saline mouthwash was used 30 minutes before the start of chemotherapy, and every half-hour until six hours after the completion of the chemotherapy. In both groups, after the bone marrow stem cell transplantation, conventional mouthwash was used for the patients.
In both groups, the severity of the mucositis was tested clinically based on the world health organization (WHO) scale and the neutrophil rate calculated by blood cell counting, based on the laboratory results of a 21-day treatment in five periods (before chemotherapy, and on the third, seventh, fourteenth, and twenty-first days after chemotherapy). The WHO scale is one of the simplest established grading systems that incorporates both subjective and objective criteria, and the validity of the scale has been established in several studies. To determine the severity of the oral mucositis, it was divided into 5 specific degrees of 0 - 4 (Table 1) (18). This scale was applied to evaluate the oral mucosa status, the incidence, and degree before and after the intervention. No equipment was used to determine the mucositis severity, but the hospital’s CBC machine (Sysmex KX21N) was applied to determine the neutrophil rate. This equipment is calibrated daily based on three normal individuals’ CBC data; in addition, the monthly and yearly calibration is done by reference equipment. In order to avoid errors in the observation, only one investigator from the research team observed the results.
Table 1. Severity of Mucositis According to the WHO Scale (18).
| Grade | Diagnostic Criteria |
|---|---|
| 0 | No symptoms |
| 1 | Redness or erythematic |
| 2 | Erythematic-wound; able to eat regular and solid food |
| 3 | Wound; eats only liquids |
| 4 | Oral feeding is not possible |
Abbreviation: WHO, World Health Organization.
This study was approved by the regional research ethics committee of the Tabriz University of Medical Sciences. Informed consent was obtained according to the ethics committee’s guidelines after approval (code 9299 on September 17, 2013). Information about the study and withdrawing from the study was provided to all of the patients, and informed consent was obtained from them.
The data analysis was performed using the statistical package for the social sciences (SPSS) version 13. The effectiveness of each treatment method in the interventional and control groups in the different treatment periods investigated was compared with the prior period via the Mann-Whitney test for independent samples; moreover, the repeated measures analysis of variance was performed to compare the effectiveness of the two methods. In addition, in order to examine the effects of the demographic variables and medical records of the patients undergoing the cryotherapy, the Pearson or Spearman correlation coefficients (depending on the data) were calculated. Finally, a model was provided to predict the severity of mucositis at any of the intervals during treatment, and to determine the approximate time of the full recovery of the oral mucositis using the linear regression variables.
4. Results
There were 29 participants, among which 16 patients in the intervention group were treated with cryotherapy (ice cubes), and 13 patients in the control group were treated with saline mouthwash. There were no differences in terms of the age, sex, educational status, or treatment regimen. The youngest patient was 19 and the oldest one was 66 years old, and the mean age was 41.5 ± 7.3. Among the 29 patients, 17 (56.62%) were male and 12 (41.37%) were female (Table 2).
Table 2. Demographic and Disease Related Characteristics of the Participants.
| Properties | Groups | |
|---|---|---|
| Control | Cryotherapy | |
| Age, y | ||
| Mean | 39.8 | 43.0 |
| (Min-Max) | (21 - 62) | (19 - 66) |
| Gender a | ||
| Male | 8 (40.4) | 9 (41.3) |
| Female | 5 (38.8) | 7 (45.1) |
| Smoking Habit | ||
| Yes | 4 | 2 |
| No | 9 | 14 |
| Chemotherapy Duration, d | ||
| ≥ 21 | 34 | 28 |
| < 21 | 7 | 5 |
| Disease Type, n | ||
| Hodgkin’s | 6 | 5 |
| Non-Hodgkin’s | 3 | 2 |
| Multiple myeloma | 4 | 9 |
avalues are expressed as No. (%).
The results of the oral mucositis during the 21-day period indicated that the mean of the mucositis scores from the first to seventh day increased, and in the first seven days both groups reached their maximum levels (Table 3). Then, from the 7th day on, the mucositis rate was reduced in both groups, and reached zero on the 21st day. Similarly, the changes in the neutrophil rate also showed that immediately after the chemotherapy it was at its highest value, but on the 7th day it was reduced to the minimum possible value, then increased immediately through the 21st day.
Table 3. Comparison of Mucositis in the Two Groups on the 3rd, 7th, 14th, and 21st Days Via the Mann-Whitney U test and Repeated Measures ANOVA.
| Days | Cryotherapya,c | Normal Salineb,c | P Valued | F | Pe |
|---|---|---|---|---|---|
| 3rd | 0.31 (0.17) | 0.77 (0.43) | 0.112 | 0.51 | 0.47 |
| 7th | 1.81 (0.83) | 2.54 (0.87) | 0.031 | 4.28 | 0.04 |
| 14th | 0.13 (0.08) | 0.92 (0.08) | 0.004 | 8.73 | 0.00 |
| 21st | 0.00 | 0.00 | NA | NA | NA |
Abbreviation: NA, not available.
a(n = 16).
cvalues are expressed as mean (SD).
b(n = 13).
dP value found by Mann-Whitney U test, SD = standard deviation.
eP found by repeated measures ANOVA test.
In order to incorporate the oral mucositis severity variables and the number of neutrophils in the treatment process for oral mucositis in those patients undergoing autologous bone marrow transplantation via the cryotherapy and normal saline mouthwash, data from the 7th, 14th, and 21st days after transplantation were compared. The data from the first seven days were not considered, because during this period the effects of the mucositis treatments were negligible, compared to increased side effects. The comparison of the groups showed that the severity of mucositis between the 7th and 14th days in both groups had significantly decreased, while the neutrophil rate significantly increased during this period. Moreover, when assessing the intervals of the 14th and 21st days after transplantation, the severity of mucositis was significantly reduced. This seems to be due to the weakness of this approach in the complete reduction of the severity of mucositis on the 14th day after transplantation (Table 3). The repeated measures ANOVA test validates these results, as shown in Table 3 for the mucositis severity, and Table 4 for the neutrophil rate.
Table 4. Comparison of the Neutrophil Rate in the Two Groups on the 3rd, 7th, 14th, and 21st Days Via the Mann-Whitney U and Repeated Measures ANOVA Tests.
| Days | Cryotherapy (16)a | Normal saline (13)a | P Valueb | Pc | F |
|---|---|---|---|---|---|
| 3rd | 1598.00 (890) | 1625.00 (13.23) | 0.78 | 0.47 | 0.51 |
| 7th | 84.06 (43.82) | 52.31 (49.07) | 0.63 | 0.28 | 0.54 |
| 14th | 2360.13 (1677.97) | 2180.23 (1754.06) | 0.72 | 0.94 | 0.05 |
| 21st | 0.00 | 0.00 | NA | NA | NA |
Abbreviation: NA, not available.
avalues are expressed as mean (SD).
bP value found via the Mann-Whitney U test, SD = standard deviation.
cP found by the repeated measures ANOVA test.
In order to investigate the main objective of the study, a comparison of two treatment methods (cryotherapy and normal saline mouthwash) on oral mucositis in those patients undergoing autologous bone marrow transplantation, in terms of the mucositis severity and neutrophil rates in both studied groups, the Mann-Whitney U test was used for the independent samples on the 3rd, 7th, and 14th intervals after implantation. The results of this comparison showed that there was no significant difference between the severity of mucositis (P = 0.112) and neutrophil rate (P = 0.713) in the two groups. On the seventh day, the severity of the mucositis in the cryotherapy group was significantly less (P = 0.031) than in the normal saline mouthwash group. However, at this point, there was no difference between the two groups with regard to the number of neutrophils (P = 0.634). Similarly, on the fourteenth day, the severity of mucositis in the cryotherapy group was significantly less than that of the normal saline mouthwash group (P = 0.004), and there was no difference between the groups in the neutrophil rate (P = 0.781) (Table 4).
5. Discussion
The purpose of this study was to compare the mean mucositis and neutrophil rates between the two study groups using cryotherapy treatment and a normal saline mouthwash treatment. The results of this study showed that both methods significantly reduced the severity of mucositis from the 7th to the 14th day after transplantation. The comparisons of the two groups indicated that the cryotherapy method was significantly more effective than the normal saline mouthwash procedure to reduce the severity of mucositis. However, there was no significant difference between two groups in the neutrophil rate.
The effects of cryotherapy in controlling side effects in patients treated with chemotherapy have been previously studied (18) For example, Baydar et al. (19) (2005) studied 99 cycles of 5-Fu chemotherapy and ice-therapy with a random pattern of 40 patients suffering from gastrointestinal malignancies. In their study, if the first cycle of chemotherapy was associated with ice treatment, the next cycles were performed on patients with no ice therapy, and vice versa. The results of this study revealed the supportive effect of ice in the incidence of chemotherapy-induced mucositis.
Svanberg et al. (14) (2014) studied 40 patients randomly divided into two case and control groups, and the severity of mucositis was measured on the 22nd day after chemotherapy. In this study, mouth cooling was introduced as an inexpensive and easy way to prevent mucositis. The cancer health association and the international association of oral oncology recommended the use of pieces of ice for 30 minutes before chemotherapy to prevent or reduce the severity of mucositis (20). Lilleby et al. (21) published a paper in 2006 reporting their study on 40 patients with melphalan medicine regimens via case and control groups evaluating the effects of cryotherapy and washing with normal saline. The severity of the mucositis was compared based on the national cancer institute scale (NCI). The patients’ reports about the presence and incidence of mucositis in the case group were significantly lower than in the control group, and the case group reported a better quality of life in comparison with the control group. The cancer health association and the international association of oral oncology recommended the use of pieces of ice for 30 minutes before chemotherapy to prevent or reduce the severity of mucositis (22). The results of this study also showed that cryotherapy is more effective than a normal saline mouthwash in the improvement of oral mucositis, which seems to be consistent with the findings of the previously mentioned studies. According to these studies, cryotherapy can significantly reduce the incidence and severity of stomatitis. Moreover, proponents of ice therapy believe that the process of the prevention of chemotherapy-induced oral mucositis is based on local vascular contraction, which leads to a reduction in the amount of medication reaching the mucosa.
5.1. Conclusions
The quantitative results of this study showed that cryotherapy is more effective than a normal saline mouthwash in the recovery from oral mucositis in those patients undergoing autologous bone marrow transplantation. Therefore, considering the lower costs and greater impact, it is suggested to use cryotherapy in the recovery of oral mucositis in these patients. One of the limitations of this study was that the study was conducted in one center, and interactions between the two groups were possible, because all of the patients were admitted to a single ward. Additionally, one person evaluated the severity of the mucositis in both groups of patients, and was aware of the arrangement in both groups. For this reason, it could be a limitation of the study. Therefore, studies in multiple centers and separate data collection are suggested.
This study also has some strengths and weaknesses from the point of view of the research method and results. This research is a pioneer study of a mucositis treatment substitution method in the bone marrow transplant ward in Iran. Cryotherapy is a cheap treatment method, especially in the availability and implementation aspects, and has less side effects than drug treatment. In addition, the medical staff expressed a desire to implement and continue this method. However, because of the limited number of bone marrow transplant wards in Iran, the statistical population was limited. Furthermore, this method is new and unusual compared to the drug treatments for some patients, which leads to a lack of trust and confidence in this method. However, the patients showed resistance to using the ice chips in cold conditions, so this situation could be investigated as a mental barrier to using cryotherapy. Finally, the success factors of the cryotherapy have not been defined, and could be proposed in future studies.
Acknowledgments
This study is the result of a nursing master’s thesis at the Tabriz University of Medical Sciences. We would like to acknowledge all of the patients participating in the study, and the Namazi hospital officials affiliated with the Shiraz University of Medical Sciences for their help in making this study possible. Furthermore, we would like to thank the Tabriz Medical Science University and its students’ research center for the use of their facilities in this study. It should be noted that this article is part of a research project registered in the Iranian.
Footnotes
Authors’ Contribution:Study concept and design: Marzieh Askarifar; acquisition of data: Marzieh Askarifar; analysis and interpretation of data: Mani Ramzi; critical revision of the manuscript for important intellectual content: Sima Lakdizaji; statistical analysis: Azad Rahmani; Administrative, technical, and material support: Faranak Jabbarzade; study supervision: Sima Lakdizaji.
Financial Disclosure:This research was conducted with the financial support of the Tabriz University of Medical Sciences.
Funding/Support:This research was conducted with the financial support of the research deputy of the Tabriz University of Medical Sciences.
References
- 1.Hingorani SR, Guthrie K, Batchelder A, Schoch G, Aboulhosn N, Manchion J, et al. Acute renal failure after myeloablative hematopoietic cell transplant: incidence and risk factors. Kidney Int. 2005;67(1):272–7. doi: 10.1111/j.1523-1755.2005.00078.x. [DOI] [PubMed] [Google Scholar]
- 2.Phianmongkhol Y, Suwan N. Symptom management in patients with cancer of the female reproductive system receiving chemotherapy. Asian Pac J Cancer Prev. 2008;9(4):741–5. [PubMed] [Google Scholar]
- 3.Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354(17):1813–26. doi: 10.1056/NEJMra052638. [DOI] [PubMed] [Google Scholar]
- 4.Shalet SM, Didi M, Ogilvy-Stuart AL, Schulga J, Donaldson MD. Growth and endocrine function after bone marrow transplantation. Clin Endocrinol (Oxf). 1995;42(4):333–9. doi: 10.1111/j.1365-2265.1995.tb02640.x. [DOI] [PubMed] [Google Scholar]
- 5.Rini C, Manne S, DuHamel KN, Austin J, Ostroff J, Boulad F, et al. Mothers' perceptions of benefit following pediatric stem cell transplantation: a longitudinal investigation of the roles of optimism, medical risk, and sociodemographic resources. Ann Behav Med. 2004;28(2):132–41. doi: 10.1207/s15324796abm2802_9. [DOI] [PubMed] [Google Scholar]
- 6.Sonis ST. A biological approach to mucositis. J Support Oncol. 2004;2(1):21–32. [PubMed] [Google Scholar]
- 7.Sonis ST. The pathobiology of mucositis. Nat Rev Cancer. 2004;4(4):277–84. doi: 10.1038/nrc1318. [DOI] [PubMed] [Google Scholar]
- 8.McGuire DB, Correa ME, Johnson J, Wienandts P. The role of basic oral care and good clinical practice principles in the management of oral mucositis. Support Care Cancer. 2006;14(6):541–7. doi: 10.1007/s00520-006-0051-8. [DOI] [PubMed] [Google Scholar]
- 9.Jayachandran S, Balaji N. Evaluating the effectiveness of topical application of natural honey and benzydamine hydrochloride in the management of radiation mucositis. Indian J Palliat Care. 2012;18(3):190–5. doi: 10.4103/0973-1075.105689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shabanloei R, Ahmadi F, Vaez J, Ansarin K, Hajizadeh E, Javadzadeh Y, et al. Alloporinol, chemomile and normal saline mouthwashes for the prevention of chemotherapy-induced stomatitis. [in Persian]. Tehran Univ. Med. J. . 2009;3(3):1537–42. [Google Scholar]
- 11.Choi SE, Kim HS. Sodium Bicarbonate Solution versus Chlorhexidine Mouthwash in Oral Care of Acute Leukemia Patients Undergoing Induction Chemotherapy: A Randomized Controlled Trial. Asian Nurs Res (Korean Soc Nurs Sci). 2012;6(2):60–6. doi: 10.1016/j.anr.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Heydari A, Sharifi H, Salek R. Effect of oral cryotherapy on combination chemotherapy-induced oral mucositis: A Randomized clinical trial. Middle East J. Cancer. 2012;3(2 & 3):55–64. [Google Scholar]
- 13.Katranci N, Ovayolu N, Ovayolu O, Sevinc A. Evaluation of the effect of cryotherapy in preventing oral mucositis associated with chemotherapy - a randomized controlled trial. Eur J Oncol Nurs. 2012;16(4):339–44. doi: 10.1016/j.ejon.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 14.Svanberg A, Birgegard G, Ohrn K. Oral cryotherapy reduces mucositis and opioid use after myeloablative therapy--a randomized controlled trial. Support Care Cancer. 2007;15(10):1155–61. doi: 10.1007/s00520-007-0245-8. [DOI] [PubMed] [Google Scholar]
- 15.Harris DJ, Eilers J, Harriman A, Cashavelly BJ, Maxwell C. Putting evidence into practice: evidence-based interventions for the management of oral mucositis. Clin J Oncol Nurs. 2008;12(1):141–52. doi: 10.1188/08.CJON.141-152. [DOI] [PubMed] [Google Scholar]
- 16.Mori T, Yamazaki R, Aisa Y, Nakazato T, Kudo M, Yashima T, et al. Brief oral cryotherapy for the prevention of high-dose melphalan-induced stomatitis in allogeneic hematopoietic stem cell transplant recipients. Support Care Cancer. 2006;14(4):392–5. doi: 10.1007/s00520-005-0016-3. [DOI] [PubMed] [Google Scholar]
- 17.Peterson DE, Ohrn K, Bowen J, Fliedner M, Lees J, Loprinzi C, et al. Systematic review of oral cryotherapy for management of oral mucositis caused by cancer therapy. Support Care Cancer. 2013;21(1):327–32. doi: 10.1007/s00520-012-1562-0. [DOI] [PubMed] [Google Scholar]
- 18.Lalla RV, Sonis ST, Peterson DE. Management of oral mucositis in patients who have cancer. Dent Clin North Am. 2008;52(1):61–77. doi: 10.1016/j.cden.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baydar M, Dikilitas M, Sevinc A, Aydogdu I. Prevention of oral mucositis due to 5-fluorouracil treatment with oral cryotherapy. J Natl Med Assoc. 2005;97(8):1161–4. [PMC free article] [PubMed] [Google Scholar]
- 20.Taheri JB, Razavi SM, Hajir S, Vaziri P, Bakhtiari S. Effect of local hypothermia in prevention or reduction of chemotherapy induced mucositis signs. J. Dent. Sch. 2009;27(3) [Google Scholar]
- 21.Lilleby K, Garcia P, Gooley T, McDonnnell P, Taber R, Holmberg L, et al. A prospective, randomized study of cryotherapy during administration of high-dose melphalan to decrease the severity and duration of oral mucositis in patients with multiple myeloma undergoing autologous peripheral blood stem cell transplantation. Bone Marrow Transplant. 2006;37(11):1031–5. doi: 10.1038/sj.bmt.1705384. [DOI] [PubMed] [Google Scholar]
- 22.Rubenstein EB, Peterson DE, Schubert M, Keefe D, McGuire D, Epstein J, et al. Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer. 2004;100(9 Suppl):2026–46. doi: 10.1002/cncr.20163. [DOI] [PubMed] [Google Scholar]