Abstract
Since the beginning of the cholera epidemic in Haiti 5 years ago, the prevalence of this deadly water-borne disease has fallen far below the initial rates registered during its explosive outset. However, cholera continues to cause extensive suffering and needless deaths across the country, particularly among the poor. The urgent need to eliminate transmission of cholera persists: compared to the same period in 2014, the first 4 months of 2015 saw three times the number of cholera cases. Drawing upon epidemiology, clinical work (and clinical knowledge), policy, ecology, and political economy, and informed by ethnographic data collected in a rural area of Haiti called Bocozel, this paper evaluates the progress of the nation’s 10-year Plan for the Elimination of Cholera. Bocozel is a rice-producing region where most people live in extreme poverty. The irrigation network is decrepit, the land is prone to environmental shocks, fertilizer is not affordable, and the government’s capacity to assist farmers is undermined by resource constraints. When peasants do have rice to sell, the price of domestically grown rice is twice that of US-imported rice. Canal water is not only used to irrigate thousands of acres of rice paddies and sustain livestock, but also to bathe, wash, and play, while water from wells, hand pumps, and the river is used for drinking, cooking, and bathing. Only one out of the three government-sponsored water treatment stations in the research area is still functional and utilized by those who can afford it. Latrines are scarce and often shared by up to 30 people; open defecation remains common. Structural vulnerabilities cut across all sectors – not just water, sanitation, health care, and education, but agriculture, environment, (global and local) commerce, transportation, and governance as well. These are among the hidden sicknesses that impede Haiti and its partners’ capacity to eliminate cholera.
Keywords: water, sanitation, WASH, oral cholera vaccination, elimination
Video abstract
Introduction
“Many people here died of cholera during the epidemic”, recalled a peasant farmer in a remote village in the communal section of Bocozel, Haiti. Bocozel lies in the lower Artibonite Valley, where the country’s most significant waterway – the Artibonite River – meets the Caribbean Sea. For the 60,000 people, most of whom are peasant rice farmers, living in this 180 km2 area just north of the coastal city of Saint Marc, the river is the villagers’ main source of water for bathing, washing, cooking, and drinking.
Five years ago, however, thousands began falling ill and hundreds died there as a result of water-borne pathogens carried by that very river. “In the blink of an eye, we went from a few patients to dozens at a time”, recalls the director of the only medical clinic in Bocozel. In a blink of the proverbial eye, cholera would rage across the entire country. Vibrio cholerae, which causes extreme dehydration due to diarrhea and vomiting and is spread by ingesting contaminated food or water, had been introduced into a nation already ranking among the most insecure in the world in terms of safe water, sanitation, and access to food. The estimated death toll as of January 10, 2016 is 9,163.1
Efforts to control the cholera epidemic in Haiti have been many and range widely in scale, coordination, and impact. The Government of Haiti’s National Plan for the Elimination of Cholera in Haiti, 2013–2022, launched in February 2013, is a comprehensive guide to tackling short- and long-term epidemiological, structural, and management issues within the water, sanitation, hygiene, and health sectors. As of 2015, however, only 18% of the plan’s $2.2 billion budget had been financed.2 Beyond the dearth of funding, hidden and unaddressed structural factors – food insecurity and hunger, vagaries of weather and trade – influence not only the ecology of disease but also the ultimate success of the elimination plan.
We undertook a biosocial study to evaluate progress toward the elimination of cholera in Haiti, focusing our efforts on one region of rural Haiti that saw some of the first cholera cases during the outset of the epidemic in October 2010. From June to July 2015, one author (VKK) lived in Bocozel and employed participant observation and interview methods to collect ethnographic data from peyizan (peasant farmers), medical professionals, government officials, and other local community members.3 Verbal informed consent was obtained from all participants. Two focus groups, ten individual semi-structured interviews, and dozens of informal conversations were conducted, transcribed, and coded. Together with primary source literature, these data were analyzed thematically using medical anthropology approaches and drawing on the conceptual rights-based framework advanced by the 2009 report, Wòch nan Soley: The Denial of the Right to Water in Haiti.4 Incorporating these ethnographic data with epidemiology, clinical work (and clinical knowledge), understanding of policies and the challenges of implementing them, ecology, and political economy, we evaluated the progress toward eliminating cholera as well as the factors that impede or promote realization of this goal. The research was approved by the institutional review boards of Partners HealthCare, Boston, USA, and Zanmi Lasante, Cange, Haiti.
During a focus group interview with members of the local grassroots organization of peyizan rice farmers, Oganizasyon d’Ayiti pou Developman (Haitian Organization for Development [OAD]), men and women from Bocozel often invoked the Haitian proverb, maladi kache pa gen remèd (hidden sickness cannot be cured). They meant by this that issues left unexposed or unconsidered will fester and subvert any efforts toward healing or amelioration. These sicknesses, the farmers explained, do not only refer to cases of underlying disease, but also evoke unspoken, malignant challenges that one faces daily – challenges that, if left unaddressed, threaten to undermine progress.
This paper will critically review Haiti’s 10-year National Plan for the Elimination of Cholera as well as its measures that have been implemented and their successes and shortfalls. We will then situate the plan in the realities faced in Bocozel, which will help to elucidate those underlying elements that factor into the feasibility of eradicating cholera from Haiti. As one farmer said, “If you do not hide your problems, you can hope that one day they will change”.
The national cholera elimination plan
In February 2013, the Government of Haiti’s Ministry of Public Health and Population (MSPP) and the National Directorate for Potable Water and Sanitation (DINEPA) officially launched the National Plan for the Elimination of Cholera in Haiti, 2013–2022 in collaboration with the United Nations Children’s Fund (UNICEF), the US Centers for Disease Control (CDC), and the Pan American Health Organization, the regional office in the Americas of the World Health Organization (WHO-PAHO). This 10-year plan targets four major areas for eliminating cholera – water and sanitation, health care services and management, epidemiology and surveillance, and health and hygiene promotion – and comprises three implementation phases.5 The first 2 years are dedicated to short-term objectives, by which annual cholera incidence should fall from 3% to less than 0.5%; 5 years are for medium-term objectives, by which incidence should be reduced to less than 0.1%; and 5 years are for long-term goals and having an incidence rate of less than 0.01%.
To meet these aims, the elimination plan promotes an integrated approach that involves improving access to potable water and sanitation facilities, increasing the collection of solid waste in metropolitan areas, strengthening the health care system, maintaining epidemiological and laboratory surveillance and early detection, ensuring rapid response to outbreaks, intensifying public health education on hygiene and prevention, promoting efforts in researching the social impacts of cholera, and decentralizing the sector through the development of community-based forms of monitoring and implementation. The plan also calls for the coordination of domestic and international actors in the water, sanitation, and hygiene (WASH) sector involved in both emergency and long-term response efforts.
To accomplish these goals, the Government of Haiti and its partners identified $2.2 billion as urgently needed, the majority of which would be dedicated to activities in the WASH sector, reflecting the massive needs in that area. They also recognized that the efforts described above would require extensive capacity building within the Haitian government – strengthening financial management and human resources from national to local level. The successful and lasting realization of the ultimate aim of the plan – to eliminate cholera from Haiti – must overcome long-standing limitations in institutional ability to manage investments and sustain WASH facilities and programs.5
The plan in action
Immediately following the launch of the National Plan for the Elimination of Cholera, MSPP and DINEPA released the Short Term Plan, 2013–2015, which outlined in three phases – emergency, postemergency, and development – a framework for addressing water and sanitation as well as public health.6 The prevention activities outlined in this plan sought to curb the transmission of cholera from one person to another through the use of potable water for consumption, hand washing, and proper food handling.
While the framework contains actions for immediate response, such as supply distribution and health care provision for cholera cases, many of its interventions would help to lay a foundation for long-term cholera prevention. Such measures include improving access to safe and affordable water and water treatment products, disseminating hygiene and health education, coordinating a local network of municipal sanitary technicians and community health agents, carrying out a campaign to mandate families to build latrines (with technical assistance from the government), vaccinating against cholera in high-risk communities, and opening wastewater treatment plants. In those first 2 years of the plan, gains have been made in each of these areas, in part, thanks to initial increased funding from donors across the world and coordinated efforts between the Government of Haiti, non-governmental organizations (NGOs), and the United Nations (UN).
Recognizing that early detection and treatment of cholera are also preventive measures, MSPP, DINEPA, and their partners developed an epidemiological surveillance and alert system. Using rapid diagnostic cholera tests, national epidemiologists and their foreign counterparts attempt to distinguish cholera from other pathological acute diarrheas and isolate pockets of cholera outbreaks. Coordination among WASH and health actors in response to alerts has helped to collect epidemiological data from 90% of geographic departments and communes, although the target, of course, is to cover 100% of the country.7
In addition to surveillance and medical treatment, the plan’s coalition of partners has implemented cholera prevention policies geared toward health promotion at the local level. By 2014, DINEPA had deployed across Haiti 280 commune-level field agents and 266 communal drinking water and sanitation technicians (techniciens eau potable et assainissement communaux [TEPACs]) to contribute to both cholera case management as well as prevention efforts.7 MSPP and other partners also established local rapid response mobile teams and mobilized community health workers to promote and report on water and sanitation in addition to health issues at the geographic departmental level. Since 2012, MSPP, PAHO, and others have drawn upon this local network to carry out a vaccination campaign targeting 375,000 people in 12 communes.8 Last year, the Government of Haiti and UNICEF launched the National Sanitation Campaign, which deploys low-cost WASH technologies and uses a strategy similar to the Community-Led Total Sanitation approach, but are more specific to Haiti’s context, to strive for zero open defecation. The campaign targets 55 communes over 5 years with the aim of encouraging community-level behavior change and leadership, as well as sustained financing strategies and private sector participation, such as regarding the supply and demand for sanitation products.9
Several major infrastructural projects as well as numerous quick-impact ones have also been undertaken over the past 2 years as part of the plan’s measures to improve water and sanitation infrastructure: from building latrines in public spaces and rehabilitating existing latrine blocks to providing desludging services and establishing small-scale water treatment stations. Measurable outcomes of the lasting effects of these projects, however, remain to be assessed. A Cholera Short Term (Phase I) Elimination Plan Evaluation Committee, led by MSPP’s Unite d’Appui a la Decentralisation Sanitaire, accompanied by DINEPA, UNICEF, and WHO-PAHO, is currently conducting site visits in majority of the departments of Haiti, collecting water, sanitation, hygiene, and health data and drafting a report. According to one committee member, the report will assess the progress of the elimination plan over its first 2 years (comparing the results obtained to the plan’s objectives, while recognizing that only a small fraction of the required funds has been received). The committee will give recommendations on how to improve the medium- and long-term components of the remaining phases of the plan through 2022.
Since the launch of the elimination plan, DINEPA and its partners have made advances in sanitation capacity. By 2012, two massive wastewater treatment centers had been constructed – supported by international donors and collaborators – to manage a portion of the sewage from Port-au-Prince with the hope of building more than a dozen others around the country that would receive human waste transported by trucks.10 By August 2015, however, only one of those facilities (Morne a Cabrit) outside of the capital remained open. At the other site, Titanyen, the gates are locked, and the funding necessary for operations is as stagnant as the abandoned pools within the facility. The sewage plants face challenges in establishing supply chains to channel more of the human waste generated in the catchment area toward the facilities rather than following the practice of unregulated dumping of human waste elsewhere (which continues on a large scale), finding a common vision among the partners for specific operating decisions, dealing with significant amounts of rubbish in latrine matter which clog the ponds, generating enough revenue for the plants to remain open, and collaborating with local bayakou (men who nocturnally empty latrines and septic tanks) and the companies with which they work to maintain the bayakou’s economic viability while still having them pay a fee to discharge their collected waste at the facility.
In a July 2015 update, the UN Office for the Coordination of Humanitarian Affairs reported that only 18% of the elimination plan’s $2.2 billion budget had been funded, sharply limiting its realization.2 The Haitian government agencies also have limited staffing resources and management capacity, restricting their ability to coordinate the activities of the diverse WASH sector. Despite these barriers and there have been measurable advancements made by the cholera elimination plan across the domains of epidemiologic surveillance, rapid response and outbreak management, hygiene promotion and sensitization, medical treatment, water supply and sanitation, and coordination among government entities, particularly MSPP and DINEPA, and international organizations.
Each of the target areas mentioned above, however, has also faced significant shortfalls. At the local level, for example, DINEPA has faced challenges in maintaining the continuous employment of TEPACs and DINEPA commune-level field teams, who have been trained, but whose salaries have thus far relied on project-specific funds and, therefore, not guaranteed long term. Beyond direct funding deficits for the elimination plan, the withdrawal of many implementing field partners due to insufficient funds of their own has had serious consequences. By 2014, for instance, the number of cholera treatment facilities dropped from 250 to 159; of the remaining centers providing cholera treatment, only 60% were found to have adequate water supply and sanitation infrastructure, sanitary practices, and infection control measures.7
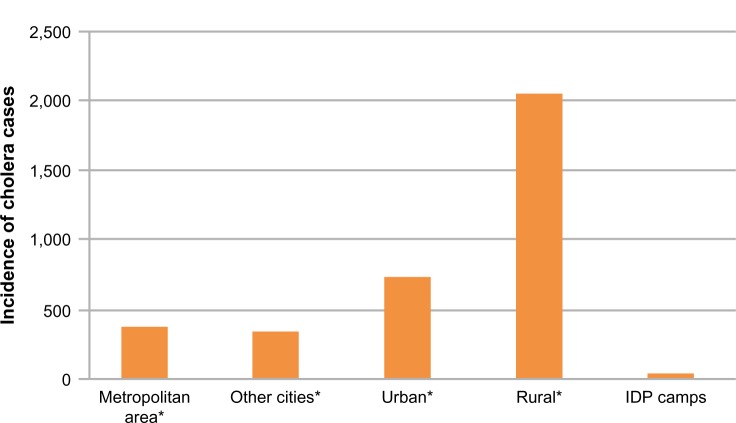
Within such a context, DINEPA and MSPP have had little choice but to focus their efforts in settings where defeating cholera is a first priority, as the present funding cannot be stretched to cover the comprehensive, nationwide efforts laid out in the elimination plan. The poor, and especially those living in rural areas which have historically suffered the greatest neglect in terms of development, continue to face disproportionate limitations when it comes to accessing health care, clean water, and sanitation services (Figures 1 and 2).
Figure 1.
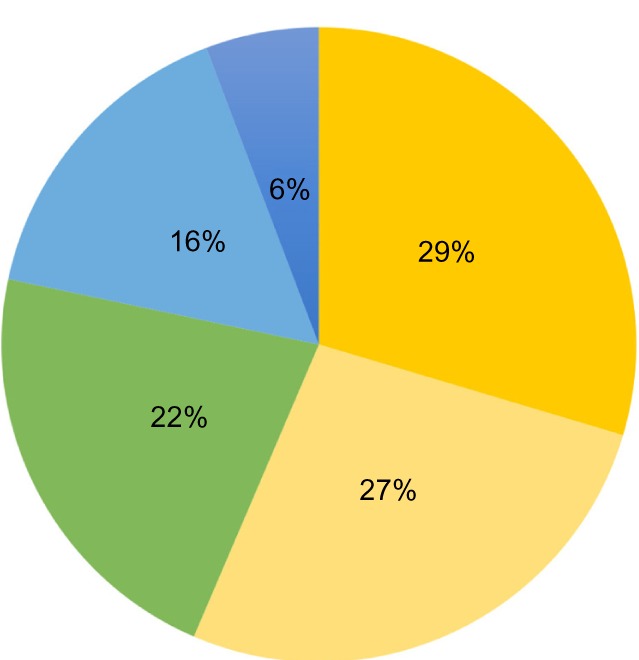
Percentage of cholera cases in Haiti by socioeconomic quintiles, October 2010–2012 (N=2,839).
Note: Reproduced from Ministère de la Santé Publique et de la Population. Enquête Mortalité, Morbidité et Utilisation des Services (EMMUS-V): Haiti 2012 [Survey on Mortality, Morbidity, and Use of Services: Haiti 2012]. Pêtion-Ville, Haiti: Institut Haïtien de l’Enfance; 2013. French. Available from: http://dhsprogram.com/pubs/pdf/FR273/FR273.pdf. Accessed September 23, 2015.23
Figure 2.
Number of cholera cases in Haiti by area of residence among 2,839 patients, October 2010–2012 (*does not include IDP camps).
Note: Reproduced from Ministère de la Santé Publique et de la Population. Enquête Mortalité, Morbidité et Utilisation des Services (EMMUS-V): Haiti 2012 [Survey on Mortality, Morbidity, and Use of Services: Haiti 2012]. Pêtion-Ville, Haiti: Institut Haïtien de l’Enfance; 2013. French. Available from: http://dhsprogram.com/pubs/pdf/FR273/FR273.pdf. Accessed September 23, 2015.23
Abbreviation: IDP, internally displaced persons.
In the 5 years since the beginning of Haiti’s cholera outbreak, incidence rates have dropped substantially, but the number of cases in the first 4 months of 2015 was triple to that of the same period in the previous year.11 In 2014, 27,753 cases of cholera were reported from Haiti, comprising almost 15% of the total global burden of reported cases.12 In the first few weeks of the Haitian epidemic, case fatality reached 6.2%, which was likely a substantial underestimate.13 When launched in 2013, the plan aimed to reduce the global fatality rate of cholera to less than 1% by 2015. Global fatality currently stands at 1.07%,1 and has not substantially changed since November 2011, according to PAHO.14 When asked about the accomplishments of his regional office, one DINEPA official asked, “If something you once called a success is now deficient, is it still a success?”
Successes and shortfalls of the plan: lessons from Bocozel
Bocozel is a 180 km2 area lying in the fertile floodplain between the coastal town of Saint Marc and the Artibonite River (Figure 3). Water flowing through the canals crisscrossing this expansive territory is used to irrigate thousands of acres of rice paddies and sustain livestock; people also use the canals to bathe, wash, and play, while wells, hand pumps, and the river are the main sources of water used for drinking, cooking, and bathing. A 2012 study of water quality in Bocozel showed that the river, canals, and wells contain highly elevated levels of coliform bacteria and Escherichia coli, while most borehole pumps showed undetectable levels (though they are not easily accessible for all residents).15 Only 48% of families in rural areas of Haiti have access to improved drinking water (ie, a source protected from contamination with fecal matter) – a decline from 50% in 1990.16
Figure 3.
Map of Bocozel, Haiti.
Note: Reproduced from Google Maps. Available from: https://commons.wikimedia.org/wiki/File:Haiti_location_map.svg. Accessed September 28, 2015.49
“Go get some water”, Veronica said as she dropped a couple of empty five-gallon buckets in front of two young men sitting below a weathered and knotted tree. The lakou, or sizable open yard, was bustling with activity. That night they would be celebrating a bal, which is just like what it sounds like a ball – a large semiformal dance celebrating the memory of the family’s matriarch who had died 2 years ago. Her husband’s home had been transformed into a Vodou ancestral shrine on the inside, and out in the front a tall poto mitan, or center post, had been placed to hold up a gray-colored USAID tarp. The two young men picked up the buckets and shortly later, returned with them full of slightly murky water from the Artibonite River, which wound its way behind this pocket of homes in the Bocozel locality (or neighborhood) of Duclas.
Immediately, one bucket was taken to the back of Veronica’s house and was reserved for hand washing and other toilet purposes. The other one was placed by a group of women who were busy preparing large amounts of food for the friends, family, Vodou musicians, and neighbors soon to arrive. This water was used to rinse cooking utensils and vegetables and was also boiled to cook rice, plantains, and stew.
If individuals in Bocozel can afford to buy them when they are accessible, most will treat the well, pump, or river water with purification tablets or drops. In another form of treatment, sediment in murky river water can be separated out by mixing in the mucilage, or gummy substance, from a crushed piece of prickly pear cactus. Scientific research shows that these cacti have coagulant properties that can reduce water turbidity by 98% and even remove bacteria.17 Without decent clean water and sanitation infrastructure, people in Bocozel have few other options for meeting their needs.
Meanwhile, the treated water reserved for drinking and ceremonial purposes had run out. Guilanda, Veronica’s sister, and one of Veronica’s daughters hopped on their bicycles with a few empty gallon jugs in hand to purchase water from a treatment station up the road in La Sisyon. Given its location near an important crossroad, La Sisyon was chosen by DINEPA and its partners, including UNICEF and the CDC, as one of the localities in Bocozel that would receive a solar-powered water treatment kiosk; a small Water Point Committee made up of community members was also established to monitor it. The La Sisyon water kiosk serves three surrounding localities, each with an estimated 1,500–2,000 inhabitants. It means that this source alone provides reliably potable water for 4,500–6,000 people – or at least serves those who can afford it or choose to pay for it. For less than 5 cents, people can purchase a couple of gallons of purified water from the station. This price, however, is significant for many Haitian families. An average Haitian family of four would have to spend approximately 12% of its annual income in order to purchase the World Health Organization’s minimum standard of 20 L of water per day.4
Not everyone chooses or has the resources to purchase the water, but the facility is changing the landscape in this rural area of Haiti. “People usually get water from the canal, let it stand, and then drink it”, explained Wilson, a credit union manager in Saint Marc and a close friend of Veronica’s family. He said, “Even though 100% of the population might not take advantage of the treatment stations, you’ll still find a significant number of people who have access to it”. The La Sisyon water kiosk has, thus far, had a beneficial impact on the village and surrounding localities – at least for those who are within walking or biking distance and who are able to afford the treated water. Also, at the end of summer, talks emerged of plans for a new station to be built in Duclas.
Other localities have not had the same success. The water treatment station in the central village of Bocozel was looted of its solar panels and other useful parts and, as of January 2016, was in complete disrepair, with cobwebs spun across its dust-covered machinery. In June 2013, there was a battle between gangs in the neighboring localities of Dubuisson and Bwa Deyo. Many houses were burned and three people were killed; the water station in Dubuisson, which had been widely used, was ransacked; a well, dug years ago by Oxfam in Bwa Deyo was also destroyed.18 As a result, 9,000–12,000 people no longer have reliable access to safe water from the kiosks in Bocozel and Dubuisson, which remain unrepaired.
The rival gangs had targeted water as a way to cut communities off from an essential human need. Their actions, however, were enmeshed in an everyday violence fueled by ecological and social fragility in the context of resource scarcity.19 In other words, the attacks were intimately linked and in response to broader forms of violence structured and perpetuated over long years and situated in certain systems of social and material order.20 These gang members, themselves victims of a continuum of structural violence (eg, chronic water insecurity), had become the victimizers, and the community as a whole suffers.21,22
Resource scarcity is not confined to difficulties accessing safe drinking water. Latrines in Haiti range from raised cement block structures to a mud-and-stick mound built over a deep hole, or to no latrine at all, and other iterations in between. In Bocozel, household latrines have, in many ways, become public facilities. Unless a family keeps it locked, a latrine can be used by 20–30 people or more: “Not only the ten or twelve people living in a home”, explained a Zanmi Lasante community health agent who works in the area, “but people passing by will come use it, too”. A farmer in the remote settlement of Bwa Deyo painted an even starker picture:
We have no toilets around here. We maybe have four toilets in the area […] but now they are all full. People, especially if it’s urgent, go to the bathroom outside in a corner of the land.
Peasant farmers in Bwa Deyo explained that open defecation is common in rural Haiti: “People are used to doing that here. We’ve been going to the bathroom outside since we were children”. In an announcement made last year, the UN Deputy Secretary-General Jan Eliasson lamented the fact that a child dies every 2.5 minutes from diseases linked to open defecation. “Those are silent deaths – not reported in the media, not the subject of public debate. Let’s not remain silent any longer”, he said.24 In the context of resource scarcity, where few latrines or other infrastructure exist, behaviors like open defecation easily become the norm. In order to end these silent deaths, steps must be taken to address the hidden barriers for making improved sanitation (which ensures that human excreta are hygienically separated from human contact) accessible to all.
According to UNICEF, less than 30% of all Haitians have access to improved sanitation; this figure drops to 19% in rural areas.16 One of the major roadblocks is that even if Haitian law requires it, and even if a family wants it, many people in Haiti lack the resources to build a long-lasting latrine with proper materials. A formative study conducted by a team from Quisqueya University’s Laboratory of Water Quality and Environment in Port-au-Prince used field survey data collected from 3,000 adults from across the country to assess sanitation in Haiti. While 97% of the respondents recognized that human waste is a source of disease, almost 85% cited money as the main reason why they are not able to build a toilet in their house.25 Strengthening the sanitation systems in Haiti would have gains not only in the realm of public health, but economically as well: one study showed that US $1 invested in sanitation in the Latin America and Caribbean region produced US $7.20 in return, as well as direct health care savings and productive days gained.26
The hidden sicknesses behind cholera
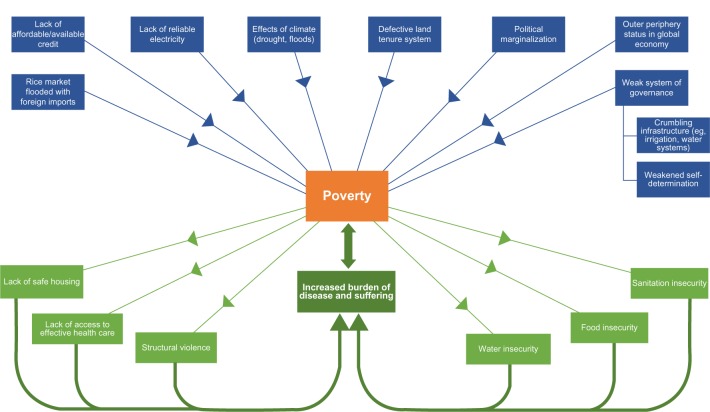
The plan formulated to end the transmission of cholera in Haiti has had some quantifiable impact: government, multilateral, and NGO agencies are able to report on the number of latrines built, wells dug, community health workers trained, and bars of soap distributed. Case fatality has decreased, and vaccination efforts, where they have occurred, have been demonstrably successful in reducing caseload.27–30 Overall, however, the elimination plan has been mired by limitations. We have reviewed how funding and management constraints have curtailed much of its scope. But the plan’s most glaring omissions are the lack of built-in measures to eliminate the hidden sicknesses that have and will sustain cholera in Haiti, unless addressed. These underlying factors contribute to the milieu of poverty, which in turn creates a vicious cycle of increased burden of disease and suffering, mediated by elements such as water insecurity, sanitation insecurity, food insecurity, structural violence, unsafe housing, and lack of access to effective health care. Summarized in Figure 4, some of these factors include unaffordable fertilizer, lack of reliable electricity, political marginalization, weak institutional governance, crumbling infrastructure, the effects of climate, and a rice market flooded by foreign imports.
Figure 4.
How poverty may impede the realization of Haiti’s plan to eliminate cholera.
What was evident during conversations with farmers in Bocozel was a collective awareness of these overlapping problems, despite a frequent reluctance to voice them openly – doing so, people said, can be emotionally draining or embarrassing. No adult, they said, likes to admit that they have not eaten more than some crackers or a cup of rice in 4 days, or that they cannot afford to access clean water, or that they do not have enough money to pay for their prescriptions or to build a toilet at their home. It is only by exposing those hidden problems, however, that “you can hope that one day they will change”. In this section, we will explore several of the hidden sicknesses of cholera, all ultimately linked to poverty.
Development efforts in the context of extreme poverty
Following the earthquake in January 2010 and the beginning of the cholera epidemic in October of same year, hundreds of multilateral organizations and NGOs of all sizes poured into Haiti. A report by the CDC notes that many of these efforts by various organizations focused on disaster response, rather than on longer-term development of WASH infrastructure and programs.31 Some present efforts, though, are geared toward systems-strengthening and community-based accompaniment and are contributing to signs of progress.
With financial support from UNICEF and in partnership with DINEPA, the Ministry of Finance, MSPP, and others, the Ministry of Education is coordinating a Healthy Schools Campaign, which aims to improve sanitation and hygiene in 100 schools. Dr Florence Guillaume, the Minister of Health at the time of the development of the plan, recently announced the results of a nationwide survey which showed that 25% of school children suffer from some form of intestinal parasites.32 In Haiti, only 26% of schools have access to water;33 79% of health facilities have access to an improved water source, and less than half have sanitation facilities.34 The campaign, in many ways, is correcting for past projects that failed to guarantee access to safe water and sanitation in public facilities.
Shortly after the outbreak of cholera began, several international humanitarian organizations arrived in Bocozel. One group’s efforts focused primarily on emergency response and the construction of latrines and what they termed hygiene awareness. “From what I know, [that NGO] is not around anymore”, said the local health clinic’s medical director. He also commented,
People still use the bathroom everywhere [outside] […] and they don’t have the means to wash their hands. Some people, because of lack of money, are compelled to not follow the principles of hygiene. It’s deadly.
A peasant farmer and member of the Haitian OAD also recalled efforts by outside WASH-promoting organizations. “We had people who came to teach us [about proper hygiene]”, he said, “but we don’t even have toilets to use”.
Common throughout two focus groups, ten semistructured interviews, and dozens of informal conversations was the issue of mwayen, or economic means. One middle-aged female peasant farmer in OAD explained, “If we have a little money left, we can go to the market to buy a few small things to eat, or buy a few raw things to try to resell”. Before it was destroyed, she had served on the committee responsible for the local oversight of the Dubuisson water treatment station. “If you don’t have money,” she said, “you will suffer, you will struggle to live.”
The members of OAD spoke about having to choose between buying food or paying for a child’s education because their rice crop had not brought in enough money, being ashamed of having to defecate outside because their latrine was in disrepair, having to go 4 or 5 days in a week without a good meal, being unable to afford the exorbitant price of fertilizer, dealing with nonfunctional canals and weeks of drought, and being unable to access electricity since a transformer blew out a year ago. The rice farmer at the beginning of this article mentioned the deadly hidden sickness of infrastructural inadequacy: “One reason [why so many people died during the cholera outbreak] was because people were drinking untreated water”, he went on.
But there’s also no access to a good road to get to the hospital, so some people died on the way there. […] We had to carry people on our backs until we could find transportation to arrive at the clinic. And sometimes as we were carrying people out, they died on our backs because we didn’t have anything to rehydrate them.
OAD is among those advocating to make the plight of the rural Haitian population known to those in power – from Haitian government officials and elected representatives to leaders and members of NGOs and international funding entities. It is also working to help local farmers identify and articulate the factors that structure the poverty, vulnerability, and violence of their circumstances by creating a space for inspection and discussion of these issues. In other words, it is working toward unmasking the hidden violence of the farmers’ political, economic, and ecological realities. “This is what we are trying to do: to train and educate the people”, explained Rafael, the OAD Coordinator.
We no longer want to wash our hands and wipe them on the ground. It should be an ongoing training to try to help the people become aware of their situation. Otherwise, we will continue going around the cycle that keeps things worse off for the peyizan. [rice farmer]
Challenges of limited institutional governance
From farmers in Bocozel to DINEPA officials to the director of the government agency dedicated to the development of the Artibonite Valley, financial resources were cited as the primary barrier to accessing health care, education, safe water, a well-constructed toilet, food, fertilizer, seeds, equipment, and basically everything else. Poverty is the source of much suffering and conflict. “We have lots of battles over land”, said Marcel, a Bocozel peasant who has been part of the leadership of the government’s local chapter of the National Institute of Reform of Agriculture of the Artibonite for the past 2 decades. Marcel continued, “People are fighting and killing one another; cutting each other’s legs and arms. Anpil moun mouri, lots of people die” – including in Marcel’s own family (his brother-in-law was accused of murdering one of Marcel’s sons using a maleficent powder).
As both a farmer and a member of the National Institute of Reform of Agriculture of the Artibonite – living downstream of and dealing with the internal inadequacies of the governance system – Marcel is well placed to recognize the consequences of poverty compounded by institutional weakness. “The government doesn’t take responsibility. The things that cause this fighting and killing over a piece of land are the responsibility of the government”. Lack of a more responsive system of governance has engendered a state of chronic vulnerability to the structural violence of poverty.
Conflicts arising from resource constraints and inadequate governance are not confined to outright violence. When it comes to water and sanitation, DINEPA is limited in not only its coffers, but also its capacity to sovereignly manage investments and sustain WASH facilities and programs. “We don’t have the freedom to self-direct our projects”, explained a DINEPA official who works in the Artibonite. The official added further, “We’re obliged to develop a project that can fit within a different program, otherwise we cannot do anything”. Top-down direction, rather than accompaniment, from international funding partners overlooks not only the vital knowledge of local institutions but also the crucial role their strengthening plays in long-term sustainability.
The Organization for the Development of the Artibonite Valley (ODVA) – an autonomous body that was established under the Ministry of Agriculture, Natural Resources and Rural Development in 1949 and relies entirely on outside funding – is the government entity tasked with providing technical, administrative, and financial infrastructure for Haiti’s canal system. According to an official report of the Ministry of Agriculture, Natural Resources and Rural Develop ment released in 2012, the irrigation network upon which hundreds of thousands of farmers rely has barely changed in the past 20 years, besides the occasional rehabilitation project supported by international funding institutions.35 Like DINEPA, some of ODVA’s principal deficiencies include weaknesses in management, inadequate training, lack of financial support, and lack of coordination of internal actors as well as international NGOs working in the field of agriculture. Projects that are implemented are significantly limited in scope and sustainability.
“Kanal la te kase”, the local Catholic priest observed solemnly on the morning of June 18, 2015. The situation was dire and the weight of his words hung in the air: a broken canal would put the 60,000 living in Bocozel at increased risk of losing this season’s rice crop, the consequences of which could be a death sentence. Years’ worth of trash and sediment had accumulated in the underground pipe bringing water from the Artibonite River to the canal before it streams through the irrigation network nourishing Haiti’s breadbasket. After a few recent heavy rains, the pipe had become completely clogged. There was barely a trickle in the concrete canal (constructed in the early 2000s) that reaches into Bocozel from the crossroads town of Pont Sondé.
Sediment washed down from bare mountains, plastic bags discarded in the open, empty soda bottles littering the sidewalks, and all kinds of rubbish gradually accumulated in the pipe. Unmitigated deforestation – a consequence of reliance on charcoal as the chief cooking fuel and weak governmental conservation policy, among a host of other factors – has precipitated environmental degradation and erosion. Inadequate municipal services means little to no regular trash collection in poor areas. Poor maintenance of irrigation systems and a failure to collect refuse, when linked to runaway deforestation, prevent farmers from irrigating their fields, which means that many lose their crop and fall deeper into poverty, crippling their access to highly privatized education, food, water, and health care. These issues lead to strong feelings by some community members. “We don’t have a government”, said an OAD farmer. He further added, “They’re like leeches, eating us and drinking our blood. The government considers us like trash they are just going to throw away”. For some, the trash that clogged the pipe in Pont Sondé brought into relief a metaphor for their own lives. The paucity of effective public systems that allows for infrastructural disasters, like the broken canal, perpetuates material insecurities and social-political ones as well.
Two weeks later, ODVA personnel were finally able to borrow an excavator machine from a nearby UN base. Although the major canal was functional again, many secondary networks – especially further downstream – remained stagnant and overgrown with water weeds. Without adequate irrigation, the farmland supplied by these networks was extremely vulnerable to the draught that struck the region soon thereafter. No water means no rice paddies. And no rice means, among many other consequences, no money to buy safe drinking water, reinforcing the vicious cycle of poverty and illness: for example, according to one national study on the impact that the cholera epidemic had on food insecurity in 2011, the supply of labor in the Artibonite Valley and irrigated districts in the Central Plateau area fell nearly 30%, resulting in loss of 10%–15% of rice harvests.36
Consequences of flooded rice market
Even if farmers are able to produce a healthy crop, they face a market dominated by imported US rice to the point where 92% of rice consumed in Haiti is from the USA.37 In 2013, the Artibonite Valley produced more than 70% of domestic rice. Yet, this production represented only 12% of rice consumed in the country.37 Decades of flooding the Haitian rice market with cheap (and highly subsidized) US rice have undermined domestic production, which has had devastating downstream effects on local health, thus perpetuating a vicious cycle of subsistence and poverty in an already vulnerable environment.
The history of the US domination of the Haitian rice market is a fairly brief one, as shown by interviews in Haiti. “The level of rice production that we used to have is much less now”, said the ODVA director. His statement is not only informed by his public position, but also by his personal experience. He also said,
My dad was a rice farmer, growing rice all the time, and my mom was the one selling the rice. My father, my grandfather, and great grandfather – they all planted rice.
Much has changed over the past generation.
In 1986, following the fall of the Duvalier regime, the US government began implementing structural adjustment policies that promoted privatization (private companies often meaning US-based ones), restricted Haitian government involvement,38 and reduced tariffs in imports, allowing US rice to flood the Haitian market. Rather than helping resolve Haiti’s rapidly accumulating debt and economic woes, this period of neoliberal restructuring devastated the domestic market, worsened the nation’s debt problems and trade deficit,39 and crippled local rice production. By 1995, the World Food Program calculated Haiti’s food self-sufficiency ratio to be 50%, which is a decrease from 85% in 1980.40
Sacrificing self-sufficiency for food-security-through-trade has adversely affected most Haitians: President Bill Clinton, who was appointed as UN Special Envoy to Haiti in 2009, publicly apologized in March 2010 for championing policies like drastic tariff reductions that destroyed Haiti’s rice production during the mid-1990s: “It may have been good for some of my farmers in Arkansas, but it has not worked. It was a mistake”, he told the Senate Foreign Relations Committee.41
Since 1986, Haiti’s rural poor have been bearing the brunt of wave upon wave of structural adjustment and liberalization at the hands of national leaders, foreign investors and organizations, and the private sector elite. “There’s no investment in the people in the Artibonite: there’s no water, fertilizer, seeds, or other things needed to grow rice”, Rafael, the coordinator of the Haitian OAD, explained. “So farmers can’t produce enough to feed the whole country. The worse thing is that now US rice is being sold in the Artibonite, too!” As of 2012, three of seven main national importers controlled 70% of the rice market; all of them sourced their rice from the USA.37 While peasant farmers in Bocozel struggle to produce enough rice to survive, these businesses profit off of a lucrative importation system that has exacerbated food insecurity in the nation.
In 2014, Haiti’s Global Health Index score (which combines indicators of undernourishment, underweight children, and child mortality) placed it 67th out of 120 countries included in the study.42 Also, the prospects for the year ahead are, under current circumstances, bleak. According to the Haiti National Coordination for Food Security (Coordination Nationale de Sécurité Alimentaire [CNSA]), agricultural production from July to December 2015 was projected to be below 50% compared to a normal year due to considerable crop losses caused by drought and seed scarcity and compounded by inadequate irrigation infrastructure, rising food and fertilizer prices, and increasing inflation.43 A recent CNSA bulletin reports that 30% of the Haitian population is living in food insecurity, with limited access to enough affordable and nutritious food.43
The consequences of a flooded market, combined with ecological factors and institutional weaknesses, feed into the cycle of poverty and disease. “Everything that we’re able to do – paying for education, food, health care, or building latrines – depends on a person’s crop”, observed a woman in Dubuisson. According to data collected by a national survey in 2012, education level was inversely related to cholera incidence: the majority of cholera patients (86% out of 2,478) had only a primary education or less.23 Lacking resources for education increases one’s risk for cholera, which in turn undermines one’s productivity and income and perpetuates the cycle.
Poor farmers, like OAD members, in Bocozel and elsewhere in the Artibonite are advocating for a paradigm shift: donor policies, trade rules, and external involvement need to better respect national and community sovereignty, strengthen agricultural and water systems, and support small-scale farmers who produce for local markets.44 Shifting the paradigm toward alleviating poverty and its effects among the destitute poor, in part by protecting and prioritizing domestic agricultural production, must be fundamental to a strategy targeting the elimination of cholera.
Existing at the margin of Haitian society – and almost entirely invisible and unheard in the global economy45 – peasant rice farmers are made vulnerable to structural and environmental forces and exploitation. Without viable economic opportunities, social safety nets, food security, or municipal infrastructure, poor Haitians lack the means to access basic human rights like adequate nutrition, water, or sanitation.
What it might take to achieve elimination
The likelihood of Haiti achieving its elimination goals under the current status quo of economic and political disenfranchisement of the poor and peasant classes (urban and rural) is scant. While domestic production for both export and local consumption remains undermined by a market flooded with imports and a closed network of powerful merchants, the long-term impact of investments in WASH is compromised. Sustained investment in health and sanitation – and thus disease eradication – is difficult to imagine without a strategy that addresses the fact that almost 60% of Haitians live on less than $2.44 a day.46
The hidden sickness of this poverty must also be brought into the open if the elimination plan is to succeed. New water supply and sanitation technology is a precarious investment if rice farmers do not have water or fertilizer to grow and earn a living from their small fields and paddies; the cost of education keeps families from affording other basic needs; imported US rice sells for half the price as local rice; the effects of climate change continue to disproportionately burden the poor;47 unsound roads make access to markets and health care a struggle; a defective land tenure system results in extortion and violence; only a quarter of the population has access to electricity;48 and government agencies like DINEPA and ODVA remain grotesquely underfunded and unaccompanied, struggling to maintain vital staff on the job. Without integrating these and other crucial factors into a plan, millions of dollars risk being squandered, attempts at short- and long-term interventions will fade into artifacts of development, and, most importantly, those most vulnerable will suffer the consequences.
As the World Bank highlighted in its 2013 report, the pressure on water resources, given the projected climate change, is expected to increase significantly in the coming years.47 “DINEPA is trying to attract people’s attention, especially among the country’s leadership, to think about the future of water in Haiti”, said a regional staff member. “Let’s take erosion for example”, the official continued.
When it rains, the water washes away the soil and doesn’t absorb into the earth where it can replenish springs. A lot of the time it’s because people cut down trees to make charcoal. And now DINEPA is finding that many springs are going dry because there are not enough trees. This means that the leaders in the Ministry of the Environment should also get involved. The public government should have certain laws to prevent people from cutting down trees, to have an alternative form of energy so that people don’t cut down the trees. This will help protect our soil and our water. [regional staff member]
Just as with water, the protection of health – and similarly, the elimination of cholera – must involve a multisectoral approach.
There remains some debate over whether it would be possible to eradicate cholera from Haiti, with most experts agreeing that elimination of infection is the goal, at least initially. Inherent in the definition of eradication in public health terms is the emphasis that continued measures to prevent infection would no longer be needed if eradication was achieved. However, eradication will not occur if transmission is still occurring. In some ways, an argument calling for eradication of cholera in Haiti (rather than “just” elimination of infection) is valuable, such that it calls on public health experts to raise their expectations of what is possible to accomplish.
Conclusion
Progress has been made in Haiti to reduce cholera morbidity and mortality, but cholera transmission, illness, and death continue to occur on a daily basis. Haiti’s National Plan for the Elimination of Cholera has proposed policies and interventions that incorporate short- and long-term strategies for the improvement of the health and WASH sectors – from distributing water filters and water purification tablets to vaccinating vulnerable communities, and from building public latrines and water systems to strengthening institutions like DINEPA. The success of the plan has and will continue to be limited not only by funding and other resource challenges, but also, intrinsically, by the unaddressed intersecting factors that, though hidden to many in positions of power within and outside of Haiti (particularly those with the means of effecting and implementing policy change), are vital components of the realities that many Haitians face.
Structural vulnerabilities cut across all sectors – not just WASH, health care, and education, but agriculture, environment, (global and local) commerce, transportation, and governance as well. These are among the hidden sicknesses that impede Haiti and its partners’ capacity to eliminate cho lera from the country –they are likely to be neither unique to Haiti nor to the disease of cholera. These hidden sicknesses, along with the perspectives of the rural poor, must be laid bare and incorporated into systems-based and ecologically aware approaches to development in Haiti, and beyond. Over the coming years, the success and sustainability of Haiti’s plan to eliminate cholera will depend as much on adequate funding as it will on partnerships that use innovative strategies to tackle the accompanying etiologies and manifestations of poverty.
Acknowledgments
This paper is dedicated to the memory of the more than 9,100 people who have lost their lives to cholera in Haiti. We deeply thank all of those in and around Bocozel who participated in and contributed their stories, knowledge, and time to this research. We would also like to acknowledge Elio Dortilus for his accompaniment, Rhoda Beutler for sharing her insight into agriculture in Haiti, Professor Elisha Renne and Dr Joseph Kolars for reviewing this manuscript, Jessica Teng for her assistance, and the Medical Scientist Training Program at the University of Michigan Medical School for providing funding. This work was also supported in part by National Institutes of Health (NIAID R01 AI099243 to LCI).
As per the Institutional Review Board-approved methods of this project, all informants were male or female adults. Verbal consent was obtained from all participants. To respect and protect the identity of participants, all names used in this article are pseudonyms.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ministère de la Santé Publique et de la Population Rapport de Cas [Case Report] Jan 10, 2016. [Accessed February 2, 2016]. French. Available from: http://mspp.gouv.ht/site/downloads/Rapport%20cholera%2010%20janvier%202016.pdf.
- 2.Office for the Coordination of Humanitarian Affairs Haiti Cholera Figures: as of July 2015. Aug 12, 2015. [Accessed September 23, 2015]. Available from: http://reliefweb.int/sites/reliefweb.int/files/resources/hti_cholera_figures_july_2015_eng.pdf.
- 3.Orlove B, Caton S. Water sustainability: anthropological approaches and prospects. Annu Rev Anthropol. 2010;39:401–415. [Google Scholar]
- 4.Varma M, Satterhwaite M, Klasing A, et al. for NYU School of Law Center for Human Rights and Global Justice, Partners In Health, RFK Memorial Center for Human Rights, Zanmi Lasante Wòch nan Soley: The Denial of the Right to Water in Haiti. 2009. [Accessed August 1, 2015]. Available from: http://parthealth.3cdn.net/0badc680352663967e_v6m6b1ayx.pdf. [PubMed]
- 5.Ministère de la Santé Publique et de la Population, Direction Nationale de l’Eau Potable et de l’Assainissement . National Plan for the Elimination of Cholera in Haiti, 2013–2022. Port-au-Prince, Haiti: 2013. [Accessed September 23, 2015]. Available from: http://new.paho.org/hq/index.php?option=com_docman&task=doc_download&gid=20326&Itemid=270&lang=eng/ [Google Scholar]
- 6.Ministère de la Santé Publique et de la Population, Direction Nationale de l’Eau Potable et de l’Assainissement . National Plan for the Elimination of Cholera in Haiti, 2013–2011: ShortTerm Plan, 2013–2015. Port-au-Prince, Haiti: Dec, 2012. [Accessed August 1, 2015]. Available from: http://www.onu-haiti.org/wp-content/uploads/2014/12/short-term-plan-2013-to-2015.pdf. [Google Scholar]
- 7.United Nations in Haiti Haiti Cholera Response. Sep, 2014. [Accessed August 1, 2015]. Available from: http://www.un.org/News/dh/infocus/haiti/Cholera_UN_Factsheet_September_2014.pdf.
- 8.Poncelet JL. Cholera in Haiti: successes and challenges in a low income country. [Accessed October 6, 2015];World Health Organization: Wkly Epidemiol Rec. 2015 Oct 5;90(40):542–544. Available from: http://www.who.int/wer/2015/wer9040.pdf?ua=1. [PubMed] [Google Scholar]
- 9.UNICEF Press Release: New sanitation campaign aims to end cholera in Haiti. Jul 16, 2014. [Accessed August 1, 2015]. Available from: http://www.unicef.org/media/media_74287.html.
- 10.Haiti Grassroots Watch . Cholera Tightens Grip on Haiti as Sanitation Funding Slows to a Trickle. 2. Vol. 7. Haiti Libre; Jul 30, 2013. [Accessed September 23, 2015]. Available from: http://haiti-liberte.com/archives/volume7-2/Cholera%20Tightens.asp. [Google Scholar]
- 11.Haiti Libre . Increase of 306% of cholera cases. Haiti Libre; May 29, 2015. [Accessed August 1, 2015]. Available from: http://www.haitilibre.com/en/news-14030-haiti-health-increase-of-306-of-cholera-cases.html. [Google Scholar]
- 12.World Health Organization Cholera, 2014. [Accessed October 6, 2015];World Health Organization: Weekly Epidemiological Record. 2015 Oct 5;90(40):517–528. Available from: http://www.who.int/wer/2015/wer9040.pdf?ua=1. [Google Scholar]
- 13.Centers for Disease Control and Prevention Update: cholera outbreak – Haiti, 2010. [Accessed August 1, 2015];MMWR Morb Mortal Wkly Rep. 2010 Nov 19;59(45):1473–1479. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5945a1.htm. [PubMed] [Google Scholar]
- 14.Pan American Health Organization Epidemiological Update: Cholera. Aug 14, 2013. [Accessed September 23, 2015]. Available from: http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=22575&Itemid.
- 15.Matias WR, Hilaire IJ, Thomson DR, Lasher J, Ivers L. Assessing bacterial water quality as part of comprehensive cholera control efforts in rural Haiti [poster] Consortium of Universities for Global Health; 2012. [Accessed August 1, 2015]. Available from: http://cugh.conferencespot.org/ENV_SOCEC.09/1. [Google Scholar]
- 16.UNICEF, World Health Organization Progress on Drinking Water and Sanitation: 2015 Update. 2015. [Accessed September 23, 2015]. Available from: http://www.unicef.org/publications/files/Progress_on_Sanitation_and_Drinking_Water_2015_Update_pdf.
- 17.Miller SM, Fugate EJ, Craver VO, et al. Toward understanding the efficacy and mechanism of Opuntia spp. as a natural coagulant for potential application in water treatment. Environ Sci Technol. 2008;42(12):4274–4279. doi: 10.1021/es7025054. [DOI] [PubMed] [Google Scholar]
- 18.Artibonite Info . Saint-Marc/Violences: trois morts et plusiers blessés dans des affrontements à Bocozelle [Saint-Marc/Violence: three dead and several wounded in clashes in Bocozelle] Artibonite Info; Jul 1, 2013. [Accessed January 3, 2015]. French. Available from: http://artiboniteinfo.com/violences-trois-morts-et-plusieurs-blesses-dans-des-affrontements-a-bocozelle/#more-243. [Google Scholar]
- 19.Scheper-Hughes N. Small wars and invisible genocides. Soc Sci Med. 1996;43:889–900. doi: 10.1016/0277-9536(96)00152-9. [DOI] [PubMed] [Google Scholar]
- 20.Farmer PE. An anthropology of structural violence. Curr Anthropol. 2004;45(3):305–325. [Google Scholar]
- 21.Bourgois P. In Search of Respect: Selling Crack in El Barrio. 2nd ed. Cambridge and New York: Cambridge University Press; 2003. [Google Scholar]
- 22.Kleinman A, Das V, Lock MM. Social Suffering. Berkeley: University of California Press; 1997. [Google Scholar]
- 23.Ministère de la Santé Publique et de la Population . Enquête Mortalité, Morbidité et Utilisation des Services (EMMUS-V): Haiti 2012 [Survey on Mortality, Morbidity, and Use of Services: Haiti 2012] Pêtion-Ville, Haiti: Institut Haïtien de l’Enfance; 2013. [Accessed September 23, 2015]. French. Available from: http://dhsprogram.com/pubs/pdf/FR273/FR273.pdf. [Google Scholar]
- 24.United Nations End Open Defecation: Breaking the silence on open defecation. 2014. [Accessed September 23, 2015]. Available from: http://www.un.org/millenniumgoals/endopendefecation.shtml.
- 25.Gilles A. Étude Formative en assainissement, design technique de système d’assainissement et plan de communication pour la promotion de l’assainissement en Haïti [Formative Study on sanitation, technical design of sanitation systems, and communication plan for the promotion of sanitation in Haiti] Port-au-Prince, Haiti: Laboratory of Water Quality and Environment, Quisqueya University; 2015. French. [Google Scholar]
- 26.Government of Haiti, World Bank Group, United Nations . Haiti Conference on: Clean Water, Improved Sanitation and Better Health. Washington, DC: World Bank Group; 2014. [Accessed January 4, 2016]. Working Paper. Available from: http://www.lessonsfromhaiti.org/download/Report_Center/haiticonference.pdf. [Google Scholar]
- 27.Ivers LC, Hilaire IJ, Teng JE, et al. Effectiveness of reactive oral cholera vaccination in rural Haiti: a case-control study and bias-indicator analysis. Lancet Glob Health. 2015;3(3):e162–e168. doi: 10.1016/S2214-109X(14)70368-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aibana O, Franke MF, Teng JE, Hilaire J, Raymond M, Ivers LC. Cholera vaccination campaign contributes to improved knowledge regarding cholera and improved practice relevant to waterborne disease in rural Haiti. PLoS Negl Trop Dis. 2013;7(11):e2576. doi: 10.1371/journal.pntd.0002576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ivers LC, Teng JE, Lascher J, et al. Use of oral cholera vaccine in Haiti: a rural demonstration project. Am J Trop Med Hyg. 2013;89(4):617–624. doi: 10.4269/ajtmh.13-0183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rouzier V, Severe K, Juste MA, et al. Cholera vaccination in urban Haiti. Am J Trop Med Hyg. 2013;89(4):671–681. doi: 10.4269/ajtmh.13-0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention Elimination of Cholera Transmission in Haiti and the Dominican Republic. Jan 11, 2011. [Accessed September 23, 2015]. Available from: http://www.cdc.gov/globalhealth/features/cholera.htm.
- 32.Haiti Libre . Alarming situation, 25% of Haitian children infected by intestinal parasites. Haiti Libre; Aug 31, 2015. [Accessed September 23, 2015]. Available from: http://www.haitilibre.com/en/news-14995-haiti-health-alarming-situation-25-of-haitens-children-infected-by-intestinal-parasites.html. [Google Scholar]
- 33.Ministère de l’Education Nationale et de la Formation Professionnelle: Direction de Santé, Nutrition et Education Programme Certification Ecole Amie de l’Hygiène [Certification Program for Schools Friendly of Hygiene] 2013 French. [Google Scholar]
- 34.Ministère de la Santé Publique et de la Population, Institut Haïtien de l’Enfance, USAID, World Bank Haiti: Evaluation de Prestation de Services de Soins de Santé2013 [Haiti: Evaluation of Health Care Service Delivery] 2013. [Accessed September 23, 2015]. French. Available from: http://www.mspp.gouv.ht/site/downloads/Rapport%20de%20synthese%20EPSSS.pdf.
- 35.Ministere de l’Agriculture des Ressources Naturelles et du Development Rural Politique d’Irrigation du MARNDR: 2012–2016 [MARNDR Irrigation Policy: 2012–2016] 2012. [Accessed August 1, 2015]. French. Available from: http://www.agriculture.gouv.ht/view/01/IMG/doc/politique_irrigation_2012_2016_VF.doc.
- 36.USAID, MARNDR/CNSA, FEWS Net Haiti Food Security Outlook: January through June 2011. 2011. [Accessed August 1, 2015]. Available from: http://pdf.usaid.gov/pdf_docs/PNADU881.pdf.
- 37.USAID Office of Food for Peace . Haiti USAID-BEST Analysis. Washington, DC: Fintrac Inc; 2013. [Accessed August 1, 2015]. Available from: http://pdf.usaid.gov/pdf_docs/pnaec206.pdf. [Google Scholar]
- 38.Industry Council for Development Advisory Mission Report . The Development of a National Seed System in Haiti. New York: Industry Council for Development; 1986. [Accessed August 1, 2015]. Available from: http://pdf.usaid.gov/pdf_docs/PDAAU417.pdf. [Google Scholar]
- 39.Farmer PE. The Uses of Haiti. Monroe, ME: Common Courage Press; 2003. [Google Scholar]
- 40.Déralciné VJ, Jackson P. Rocks in the Water, Rocks in the Sun: A Memoir from the Heart of Haiti. Edmonton, AB: AU Press; 2015. [Google Scholar]
- 41.Katz JM. The Associated Press: With Cheap Food Imports, Haiti Can’t Feed Itself. The Denver Post. Mar 20, 2010. [Accessed August 1, 2015]. Available from: http://www.denverpost.com/spencer/ci_14719800.
- 42.International Food Policy Research Institute, Concern Worldwide, Welthungerhilfe 2014 Global Hunger Index: The Challenge of Hidden Hunger. 2014. [Accessed August 1, 2015]. Available from: http://www.ifpri.org/cdmref/p15738coll2/id/128360/filename/128571.pdf.
- 43.Haiti Libre . Drought, alarming situation in the country. Haiti Libre; Sep 11, 2015. [Accessed September 23, 2015]. Available from: http://www.haitilibre.com/en/news-15108-haiti-agriculture-drought-alarming-situation-in-the-country.html. [Google Scholar]
- 44.Steckley ME. Electronic Thesis and Dissertation Repository. London, ON: University of Western Ontario; 2015. Agrarian change and peasant prospects in Haiti [dissertation] [Google Scholar]
- 45.Fatton R. Haiti: Trapped in the Outer Periphery. Boulder, CO: Lynne Rienner Publishers; 2014. [Google Scholar]
- 46.The World Bank Haiti: Overview. 2015. [Accessed July 16, 2015]. Available from: http://www.worldbank.org/en/country/haiti/overview.
- 47.The World Bank . Turn Down the Heat: Climate Extremes, Regional Impacts, and the Case for Resilience. Washington, DC: International Bank for Reconstruction and Development/The World Bank; 2013. [Accessed September 15, 2015]. Available from: http://www.worldbank.org/content/dam/Worldbank/document/Full_Report_Vol_2_Turn_Down_The_Heat_%20Climate_Extremes_Regional_Impacts_Case_for_Resilience_Print%20version_FINAL.pdf. [Google Scholar]
- 48.USAID Haiti: Overview – Energy. Aug 26, 2015. [Accessed September 8, 2015]. Available from: https://www.usaid.gov/haiti/energy.
- 49.Google Maps. [Accessed September 28, 2015]. Available from: https://commons.wikimedia.org/wiki/File:Haiti_location_map.svg.