Vaccines to protect against HIV-1, the causative agent of AIDS, are not approved for use. Antibodies that neutralize genetically diverse strains of HIV-1 bind to discrete regions of the envelope glycoproteins, including the gp41 MPER. We engineered recombinant reoviruses that displayed MPER epitopes in attachment protein σ1 (REO-MPER vectors). The REO-MPER vectors replicated with wild-type efficiency, were genetically stable, and retained native antigenicity. However, we did not detect HIV-1-specific immune responses following inoculation of the REO-MPER vectors into small animals. This work provides proof of principle for engineering reovirus to express antigenic epitopes and illustrates the difficulty in eliciting MPER-specific immune responses.
KEYWORDS: human immunodeficiency virus, immunization, live vector vaccines, neutralizing antibodies, reovirus
ABSTRACT
The gp41 membrane-proximal external region (MPER) is a target for broadly neutralizing antibody responses against human immunodeficiency virus type 1 (HIV-1). However, replication-defective virus vaccines currently under evaluation in clinical trials do not efficiently elicit MPER-specific antibodies. Structural modeling suggests that the MPER forms an α-helical coiled coil that is required for function and immunogenicity. To maintain the native MPER conformation, we used reverse genetics to engineer replication-competent reovirus vectors that displayed MPER sequences in the α-helical coiled-coil tail domain of viral attachment protein σ1. Sequences in reovirus strain type 1 Lang (T1L) σ1 were exchanged with sequences encoding HIV-1 strain Ba-L MPER epitope 2F5 or the entire MPER. Individual 2F5 or MPER substitutions were introduced at virion-proximal or virion-distal sites in the σ1 tail. Recombinant reoviruses containing heterologous HIV-1 sequences were viable and produced progeny yields comparable to those with wild-type virus. HIV-1 sequences were retained following 10 serial passages in cell culture, indicating that the substitutions were genetically stable. Recombinant viruses engineered to display the 2F5 epitope or full-length MPER in σ1 were recognized by purified 2F5 antibody. Inoculation of mice with 2F5-containing vectors or rabbits with 2F5- or MPER-containing vectors elicited anti-reovirus antibodies, but HIV-1-specific antibodies were not detected. Together, these findings indicate that heterologous sequences that form α-helices can functionally replace native sequences in the α-helical tail domain of reovirus attachment protein σ1. However, although these vectors retain native antigenicity, they were not immunogenic, illustrating the difficulty of experimentally inducing immune responses to this essential region of HIV-1.
IMPORTANCE Vaccines to protect against HIV-1, the causative agent of AIDS, are not approved for use. Antibodies that neutralize genetically diverse strains of HIV-1 bind to discrete regions of the envelope glycoproteins, including the gp41 MPER. We engineered recombinant reoviruses that displayed MPER epitopes in attachment protein σ1 (REO-MPER vectors). The REO-MPER vectors replicated with wild-type efficiency, were genetically stable, and retained native antigenicity. However, we did not detect HIV-1-specific immune responses following inoculation of the REO-MPER vectors into small animals. This work provides proof of principle for engineering reovirus to express antigenic epitopes and illustrates the difficulty in eliciting MPER-specific immune responses.
INTRODUCTION
Despite tremendous strides in understanding human immunodeficiency virus type 1 (HIV-1) pathobiology since its discovery in 1983, an efficacious HIV-1 vaccine remains elusive. With an estimated 7,000 to 8,000 new infections occurring each day, an HIV-1 vaccine is our best hope for significantly reducing the global health burden attributable to HIV-1 (http://www.unaids.org). However, FDA-approved vaccines for HIV-1 are not available.
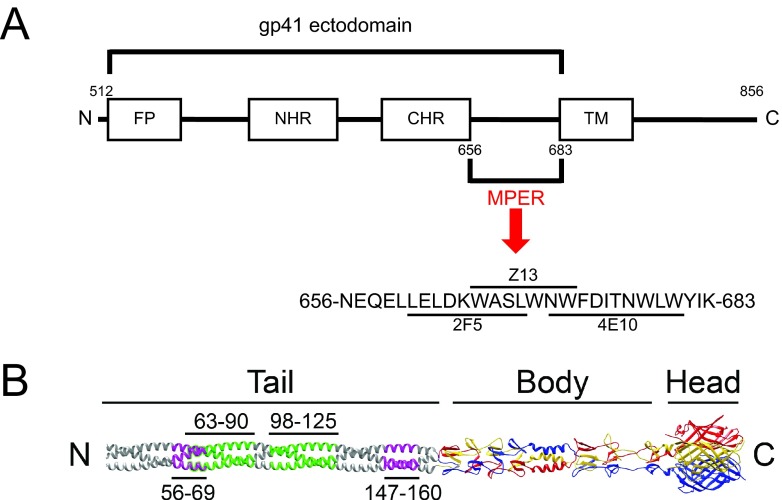
Some HIV-1-infected persons produce monoclonal antibodies (MAbs) that neutralize diverse strains of HIV-1 (i.e., broadly neutralizing). These MAbs bind epitopes in the gp120 surface glycoprotein or gp41 transmembrane glycoprotein (1–6). Those that bind the gp41 membrane-proximal external region (MPER) can potently neutralize a wide spectrum of HIV-1 primary isolates, including strains in clades B and C (2, 7–9). Of three such MPER-specific MAbs, 2F5 and 4E10 bind to adjacent MPER epitopes and Z13 binds to an epitope overlapping the 2F5 and 4E10 binding sites (Fig. 1A) (8).
FIG 1 .
Structure of reovirus attachment protein σ1. (A) Schematic of the HIV-1 gp41 ectodomain. The gp41 ectodomain is comprised of a fusion peptide (FP), N-terminal heptad repeat (NHR), C-terminal heptad repeat (CHR), and membrane-proximal external region (MPER) (8). The transmembrane region also is indicated. MPER-specific 2F5, 4E10, and Z13 MAb epitopes are indicated. N- and C-terminal boundaries are shown. Numbers represent amino acid positions. (B) A full-length depiction of σ1, generated by appending a predicted trimeric α-helical coiled coil to the amino terminus of the largest available crystallized σ1 fragment (30). The three monomers of the crystallized region are shown in red, blue, and yellow; the model is shown in gray. Tail, body, and head regions are indicated. N and C termini are shown. Insertion sites for 2F5 sequences are indicated in purple. Insertion sites for whole MPER sequences are indicated in green.
MPER sequences are conserved across HIV-1 subtypes (7, 8) and mediate an essential function in HIV-1 cell entry (8, 10). Following the sequential binding of gp120 to CD4 and a chemokine coreceptor, gp41 undergoes a series of conformational changes that result in fusion of the viral envelope and cell membrane (8). The ectodomain of gp41 is composed of a fusion peptide, an N-terminal heptad repeat (NHR), a C-terminal heptad repeat (CHR), and the MPER. Structural modeling suggests that the NHR, CHR, and MPER form α-helical coiled-coils that are required for function and immunogenicity (Fig. 1A) (8).
Three lines of evidence support a role for MPER-specific antibody responses in defense against HIV-1 infection. First, rates of mother-to-child transmission correlate inversely with reactivity of maternal sera against peptides corresponding to the MPER and C-terminal heptad repeat of gp41 (11–13). Second, MPER 2F5 epitope-specific IgA derived from colostral and cervico-vaginal secretions of HIV-infected women prevents transcytosis of HIV-1 across epithelial barriers in vitro (14). Third, passive immunization of nonhuman primates with MPER-specific MAbs isolated from HIV-1 subtype B-infected individuals, including 2F5 and 4E10, protects against infection or disease progression following simian-human immunodeficiency virus challenge (15–17). Despite these findings, a vaccine that induces protective MPER-specific antibody responses in experimental animals has not been developed.
Mammalian orthoreovirus (reovirus) forms nonenveloped icosahedral particles composed of two protein shells (18) that enclose 10 segments of double-stranded RNA (dsRNA) (19). The outer capsid contains four structural proteins, σ1, σ3, μ1, and λ2. The σ1 protein is anchored into pentameric λ2 turrets at the capsid vertices (18) and mediates reovirus attachment to target cells (20, 21). Virtually all mammals, including humans, can be infected with reovirus, but disease is restricted to the very young (22). Infection with reovirus is common, as the majority of adults have detectable reovirus-specific immune responses (23–25).
Reovirus attachment protein σ1 is a filamentous trimer that is ~480 Å in length (Fig. 1B) (26–28). It has a modular organization with three tandemly arranged structural regions: an N-terminal amphipathic α-helical coiled-coil tail (residues 1 to ~170), a triple β-spiral body interrupted by a short α-helix region (residues ~170 to 309), and a C-terminal globular head (residues 310 to 455) (28–30). Like other amphipathic α-helices, the α-helical coiled coil in the σ1 tail is formed by recurring sets of 7 amino acids, called heptad repeats (31). There are 25 heptad repeats in the α-helical coiled-coil region of strain type 1 Lang (T1L) σ1, spanning amino acid residues 7 to 181 (29). The MPER assumes an α-helical secondary structure (8) similar to that predicted for the σ1 tail (27–29).
Viable reovirus can be recovered from cells expressing T7 polymerase following transfection of plasmid cDNA copies of the viral gene segments under transcriptional control of the T7 promoter (32, 33). Neither helper virus nor coexpression of viral replication proteins is required. Plasmid-derived virus recapitulates properties of native virus in all cell culture and in vivo models of reovirus infection studied to date. We have used a reverse genetics system to introduce changes into viral capsid and replication proteins to define roles of individual amino acids, functional domains, and structural motifs in receptor utilization (30, 34–36), virion disassembly (32, 37, 38), membrane penetration (39, 40), interferon induction (41–43), dsRNA synthesis (44–46), viral replication and spread in vivo (32, 47–50), and neurovirulence (39, 40, 51). Thus, the technology exists to use reovirus as a replication-competent vaccine vector.
In this study, we recovered reovirus vectors in which α-helical regions in the σ1 tail were replaced with antigenic α-helical regions of the HIV-1 MPER (REO-MPER vectors). REO-MPER vectors replicated comparably to wild-type virus, were genetically stable following 10 cell culture passages, and retained the native MPER-specific MAb epitope. However, the REO-MPER vectors did not elicit HIV-1-specific immune responses in mice or rabbits. These findings indicate that reovirus can be engineered to serve as a vaccine vector, and they provide another example of the challenge in raising MPER-specific immune responses.
RESULTS
Generation of recombinant reoviruses displaying the 2F5 epitope in viral attachment protein σ1.
Reovirus attachment protein σ1 is partitioned into tail, body, and head domains (28–30) (Fig. 1B). To test the hypothesis that α-helical coiled-coil sequences derived from other viruses can be inserted into structurally homologous regions of the σ1 tail and retain native immunogenicity, we replaced two heptad repeats in σ1 with two heptad repeats from the HIV-1 gp41 MPER (Fig. 1B). The MPER sequences chosen for insertion contain the 2F5 epitope, which in the context of HIV-1 elicits broadly neutralizing antibody responses against HIV-1 (52–54). We replaced nucleotides encoding amino acids 56 to 69 or 147 to 160 of strain T1L σ1 with sequences encoding residues 656 to 669 of gp160 (the precursor of gp41) from HIV-1 strain Ba-L (656-NEQELLELDKWASL-669) in a σ1-encoding S1 gene plasmid vector. This region spans the entire 2F5 core epitope (662-ELDKWASL-669). Resultant plasmids were used to generate recombinant strain (rs) reoviruses via reverse genetics (32, 33). 2F5-expressing reoviruses rsT1L/σ1 2F5-56 and rsT1L/σ1 2F5-147 and wild-type rsT1L were isolated from cell lysates by plaque purification using murine L cells and purified using CsCl gradients. Insertion of the 2F5-encoding sequence into the viral genome was confirmed by sequence analysis of viral dsRNA.
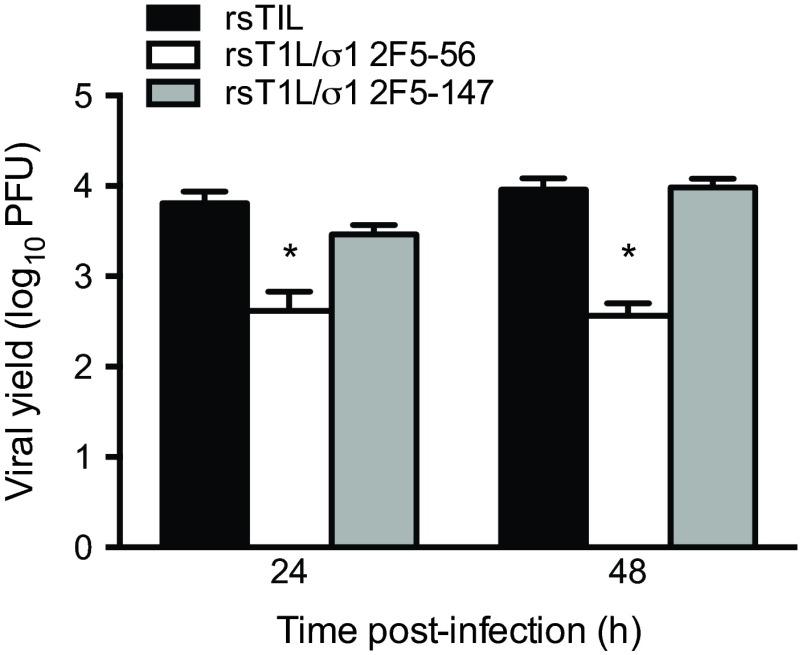
To determine whether the substituted 2F5 sequences affect replication of the recombinant reoviruses, we quantified viral yields following infection of L cells (Fig. 2). Progeny yields of rsT1L/σ1 2F5-147 were comparable to those obtained for wild-type rsT1L at 24 and 48 h postinfection. However, yields of rsT1L/σ1 2F5-56 were markedly reduced relative to rsT1L. Sequence alterations were not detected in the S1 gene of either 2F5-containing virus following 10 serial passages in culture (data not shown). Together, these data indicate that α-helical sequences in σ1 can be replaced with heterologous sequences that contain a similar secondary structure and that the substitutions are genetically stable.
FIG 2 .
Reoviruses that display the HIV-1 2F5 epitope in attachment protein σ1 replicate efficiently in cell culture. L cells were adsorbed with rsT1L, rsT1L σ1/2F5-56, or rsT1L σ1/2F5-147 at an MOI of 1 PFU/cell. Viral titers in cell lysates were determined by plaque assay at 0, 24, and 48 h postadsorption. Results are expressed as the mean viral yield for triplicate samples. Error bars indicate standard deviations. *, P < 0.05 compared with rsT1L (Student’s t test).
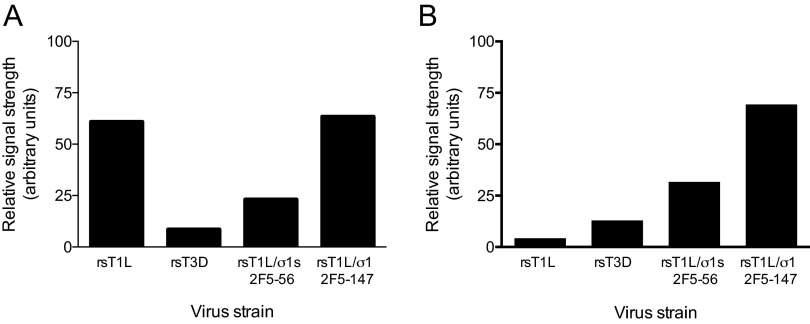
To determine whether the 2F5 epitope is exposed on the surface of recombinant reovirus particles, we used a fluorophore-linked immunosorbent assay (FLISA) to detect the binding of MAb 2F5 to immobilized reovirus virions (Fig. 3). In these experiments, MAb 2F5 bound to viruses with insertions at either site in the σ1 α-helical coiled-coil domain but not to rsT1L. Both 2F5-expressing viruses also were detected by FLISA using a T1L σ1 head-specific antiserum (Fig. 3). These data indicate that the HIV-1 2F5 epitope retains the native conformation in the context of the reovirus σ1 protein.
FIG 3 .
The 2F5 epitope is displayed by reovirus vectors encoding single 2F5 substitutions. Wells of FLISA plates were coated with 1011 particles of rsT1L, rsT3D, rsT1L σ1/2F5-56, or rsT1L σ1/2F5-147 and incubated with a T1L σ1 head-specific polyclonal antiserum (A) or MAb 2F5 (B) at 37°C for 1 h. Antibody binding to the immobilized virus was detected following incubation with fluorophore-conjugated donkey anti-human IgG. FLISA signals were quantified using a LI-COR Odyssey infrared imaging system.
Immunogenicity of REO-2F5 vectors.
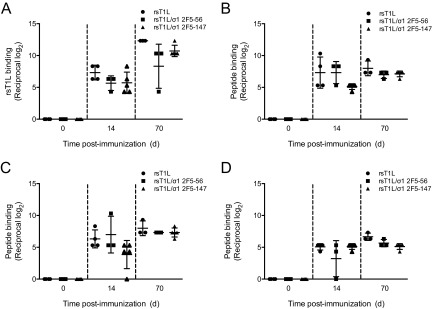
To determine whether the REO-2F5 vectors elicit 2F5-specific humoral immune responses, we inoculated BALB/c mice perorally with 107 PFU of rsT1L, rsT1L/σ1 2F5-56, or rsT1L/σ1 2F5-147. Booster doses were administered 21 and 42 days following the initial immunization. Blood was collected on the day of inoculation (day 0) and on days 14 and 70 postinoculation. Pre- and postimmunization serum samples were tested for the presence of reovirus-specific and 2F5 peptide-specific antibodies by FLISA (Fig. 4). As anticipated, we detected significant increases in reovirus-specific antibody titers from day 14 to day 70 in sera from mice inoculated with wild-type virus and each REO-2F5 vector (Fig. 4A). Although sera from mice inoculated with rsT1L/σ1 2F5-56 or rsT1L/σ1 2F5-147 displayed detectable binding to two 2F5-containing peptides (Fig. 4B and C), the levels were comparable to those detected in sera from mice inoculated with rsT1L. Moreover, the 2F5 peptide binding activity in sera of mice inoculated with rsT1L, rsT1L/σ1 2F5-56, or rsT1L/σ1 2F5-147 did not exceed the levels of binding detected with the negative-control peptide (Fig. 4D).
FIG 4 .
Induction of humoral immune responses in mice by REO-2F5 vectors. Six-week-old, reovirus-seronegative BALB/c mice were inoculated perorally with 107 PFU of rsT1L, rsT1L/σ1 2F5-56, or rsT1L/σ1 2F5-147 (n = 3 to 5 mice per group). Blood was collected on day 0 (preinoculation) and on days 14 and 70 (postinoculation). Serial 4-fold dilutions of sera were tested for reovirus-specific antibodies using wells coated with rsT1L (A) or 2F5-specific antibodies using wells coated with three different 2F5-containing peptides (8926, 8927, or 8888) (B, C, and D) by FLISA. FLISA signals were quantified using a LI-COR Odyssey infrared imaging system and are expressed as the log2 mean reciprocal antibody titers relative to day 0 results. Error bars indicate standard deviations.
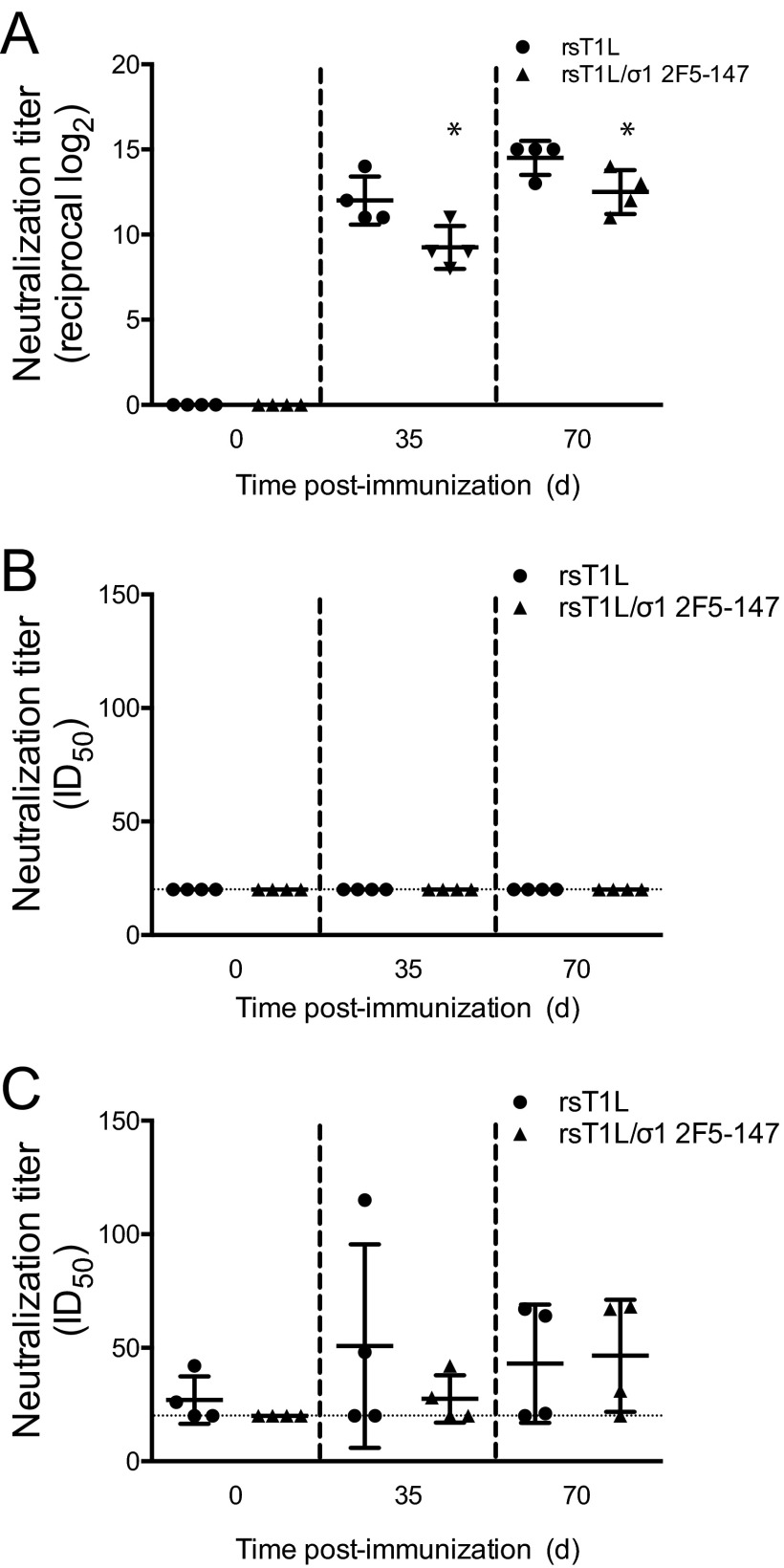
We next tested whether the REO-2F5 vectors were capable of inducing 2F5-specific humoral immune responses in rabbits, which represent a preferred small-animal model for studies to evaluate induction of HIV-1-specific humoral immune responses (55). Rabbits were inoculated perorally with 109 PFU of rsT1L or rsT1L/σ1 2F5-147. Booster doses were administered 21 and 42 days following the initial immunization. Blood was collected on the day of inoculation (day 0) and on days 35 and 56 postinoculation. Due to high levels of background binding of rabbit sera to 2F5 and control peptides, we tested pre- and postimmunization serum samples for the capacity to neutralize reovirus and HIV-1 (Fig. 5). Preimmunization samples were negative for reovirus-neutralizing antibodies. However, at day 35 postimmunization, all rabbits had detectable reovirus-specific antibodies, with 60% plaque reduction neutralization (PRNT60) antibody titers ranging from 8 to 14 (the log2 reciprocal titer) (Fig. 5A). Anti-reovirus neutralizing antibody titers increased slightly at day 70. A modest, but statistically significant, higher anti-reovirus antibody titer was detected in mice inoculated with rsT1L than in those inocluated with rsT1L/σ1 2F5-147. We used tier 1 and tier 2 Env-pseudotyped reporter retroviruses (56, 57) to assess the HIV-1 neutralization capacity in serum from reovirus-inoculated rabbits. No neutralization of tier 1 Env-containing pseudoviruses was detected in any of the samples tested. Neutralization activity against tier 2 Env-containing pseudotyped viruses was comparable between sera collected from rabbits inoculated with rsT1L or rsT1L/σ1 2F5-147 (Fig. 5B). Together, these findings indicate that REO-2F5 vectors elicit vector-specific antibodies but fail to stimulate production of HIV-1 2F5 epitope-specific humoral immune responses.
FIG 5 .
Induction of humoral immune responses in rabbits by REO-2F5 vectors. Six-week-old, reovirus-seronegative New Zealand White rabbits were inoculated perorally with 109 PFU of rsT1L or rsT1L/σ1 2F5-147 (n = 4 rabbits per group). Blood was collected on day 0 (preinoculation) and on days 35 and 70 (postinoculation). Serial 4-fold dilutions of sera were tested for reovirus-specific antibodies by determining the PRNT60 (A) and HIV-specific antibodies by determining the capacity to neutralize infection of TZM-bl cells by tier 1 HIV-1 Env-pseudotyped viruses (B) or A3R5 cells by tier 2 HIV-1 Env-pseudotyped viruses (C). Results are expressed as the 50% infectious dose (ID50) for pseudotyped viruses. Error bars indicate standard deviations. *, P < 0.05 compared with rsT1L (Student’s t test).
Second-generation reovirus vectors encode the entire MPER.
We thought it possible that the minimal 2F5 epitope inserted into σ1 was of insufficient size to elicit a detectable response. To assess this possibility, we engineered second-generation reovirus vectors in which a sequence containing four heptad repeats corresponding to the entire MPER motif from HIV-1 strain Ba-L (656-NEQELLELDKWASLWNWFDITKWLWYIK-683) was substituted for four heptad repeats in the T1L σ1 protein. This region contains epitopes for three MPER-specific antibodies, 2F5 (662-ELDKWASL-669), 4E10 (669-LWNWFDITKWLWYIK-683), and Z13 (666-WASLWNWFDITK-677) (Fig. 1A). MPER-specific sequences were introduced into σ1 at residues 63 to 90, 98 to 125, or 147 to 174, and recombinant viruses (REO-MPER vectors) were recovered using reverse genetics (Fig. 1B). Viruses with MPER sequences inserted at residues 63 (rsT1L/σ1 MPER-63) and 98 (rsT1L/σ1 MPER-98) were viable. However, we were not able to recover virus containing the insertion at amino acid 147 (rsT1L/σ1 MPER-147). Insertion of the MPER-encoding sequence into the S1 gene segment of viable virus was confirmed by sequence analysis of viral dsRNA.
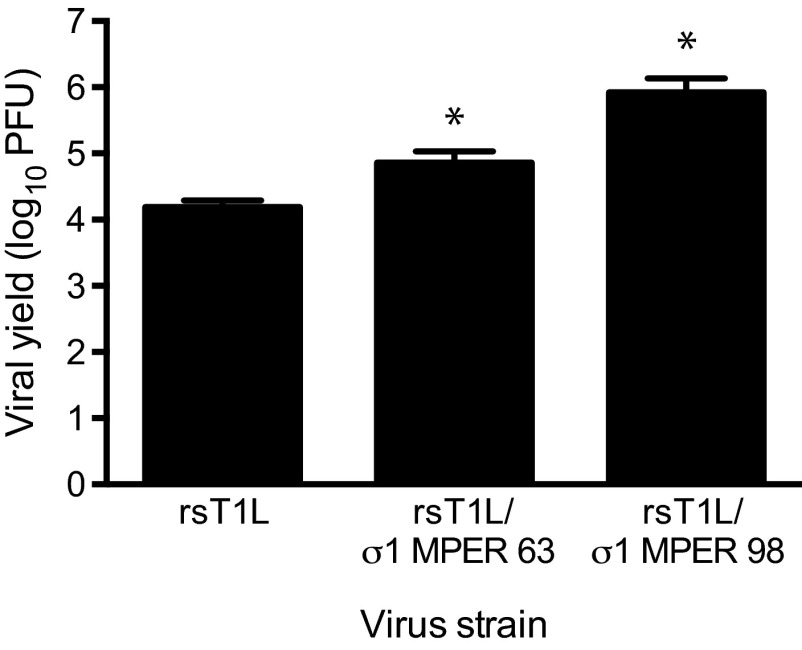
To determine whether insertion of the entire MPER sequence into the σ1 protein affects viral replication in cultured cells, we quantified viral titers 48 h after infection of L cells (Fig. 6). Both rsT1L/σ1 MPER-63 and rsT1L/σ1 MPER-98 produced yields equivalent to, or greater than, those of wild-type rsT1L. No sequence alterations were detected in the recombinant reovirus S1 gene sequences following 10 serial passages in cell culture. Together, these data indicate that the entire MPER of HIV-1 gp41 can be substituted for α-helical regions of σ1. However, the C-terminal portion of the σ1 tail is less amenable to genetic manipulation, suggesting that key determinants of σ1 protein stability or function reside in this region of the protein.
FIG 6 .
Reoviruses that display the HIV-1 MPER in attachment protein σ1 replicate efficiently in cell culture. L cells were adsorbed with rsT1L, rsT1L σ1/MPER-63, or rsT1L σ1/MPER-98 at an MOI of 1 PFU/cell. Viral titers in cell lysates were determined by plaque assay at 0 and 48 h postadsorption. Results are expressed as the mean viral yield for triplicate samples. Error bars indicate standard deviations. *, P < 0.05 compared with rsT1L (Student’s t test).
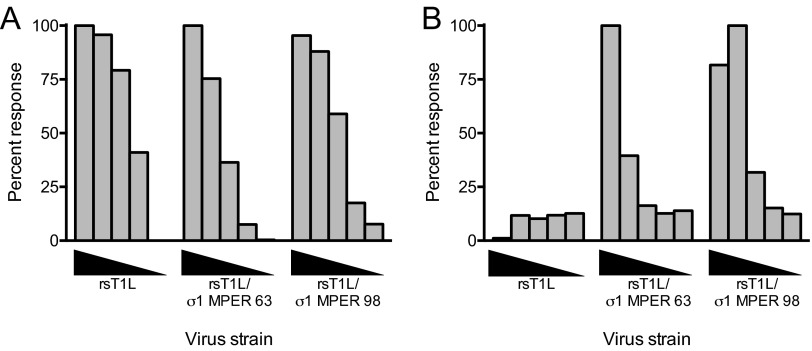
To determine whether the MPER epitope in the REO-MPER vectors retains its native conformation, we stained L cells infected with rsT1L, rsT1L/σ1 MPER-63, or rsT1L/σ1 MPER-98 with a 2F5 epitope-specific monoclonal antibody (Fig. 7A). Cells infected with rsT1L/σ1 MPER-63 or rsT1L/σ1 MPER-98 were stained with the 2F5 antibody, but no 2F5 staining was observed in cells infected with rsT1L. As a positive control, cells infected with each virus displayed staining with polyclonal reovirus-specific antiserum (Fig. 7B). These data indicate that the HIV-1 MPER epitope retains its native conformation in the context of the reovirus σ1 protein.
FIG 7 .
Second-generation reovirus vectors display the MPER epitope. L cells plated in 96-well plates were adsorbed with 10-fold serial dilutions of rsT1L, rsT1L/σ1 MPER-63, or rsT1L/σ1 MPER-98 over a range of MOIs (0.01 to 100 PFU/cell). At 24 h postadsorption, cells were fixed and stained with 2F5 epitope-specific monoclonal antibody (A) or polyclonal reovirus-specific antiserum (B) followed by secondary antibodies conjugated to AlexaFluor 488. The results were quantified using an Odyssey infrared imaging system and normalized to the maximum response achieved for each antibody. The data are presented as percentages of the normalized response.
Immunogenicity of REO-MPER vectors displaying the entire MPER motif.
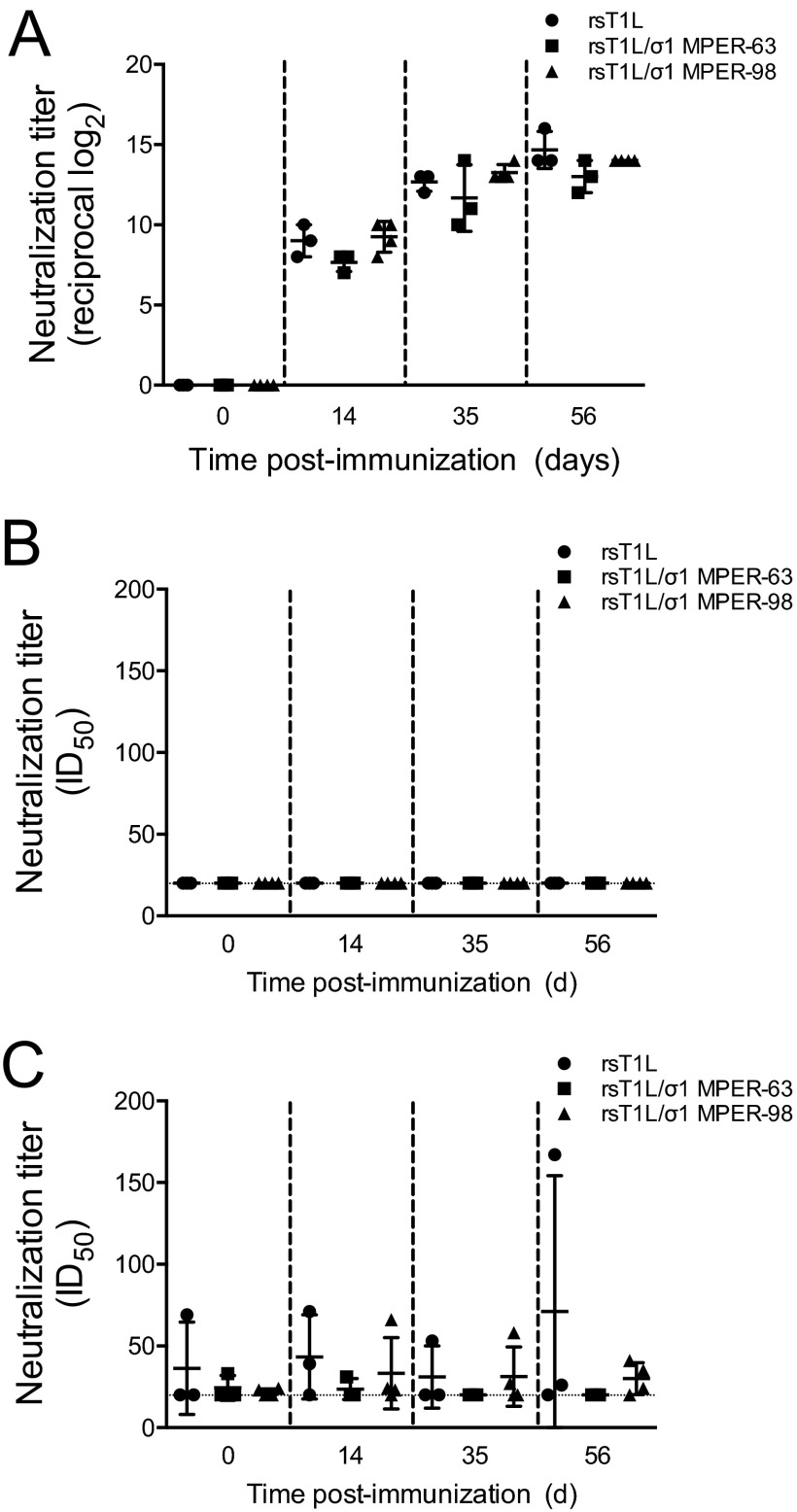
To determine whether REO-MPER vectors elicit MPER-specific humoral immune responses, we inoculated rabbits perorally with 109 PFU of rsT1L, rsT1L/σ1 MPER-63, or rsT1L/σ1 MPER-98. Booster doses were administered 21 and 42 days following the initial immunization. Blood was collected on the day of inoculation (day 0) and on days 14, 35, and 56 postinoculation. Pre- and postimmunization serum samples were tested for the presence of reovirus-specific and MPER peptide-specific antibodies by FLISA (Fig. 8). As with the previous experiments, preimmunization samples were negative for both types of antibodies. At day 14 postimmunization, all rabbits had detectable reovirus-specific antibodies, with antibody titers ranging from 7 to 10 (reciprocal log2 titer) (Fig. 8A). By day 56, anti-reovirus antibody titers increased to a range of 12 to 16 (reciprocal log2 titer) per animal. However, we did not detect neutralization activity in serum from rabbits inoculated with MPER-containing vectors when we used tier 1 or tier 2 Env-pseudotyped viruses (Fig. 8B and C). Together, these findings indicate that REO-MPER vectors elicit reovirus-specific antibody responses but not responses specific for the HIV-1 MPER.
FIG 8 .
Immunogenicity of REO-MPER vectors. Six-week-old, reovirus-seronegative New Zealand White rabbits were inoculated perorally with 109 PFU of T1L, rsT1L/σ1 MPER-63, or rsT1L/σ1 MPER-98 (n = 3 or 4 rabbits per group). Blood was collected on day 0 (preinoculation) and on days 14, 35, and 56 (postinoculation). Serial 4-fold dilutions of sera were tested for reovirus-specific antibodies by determining the PRNT60 (A) and HIV-specific antibodies by determining the capacity to neutralize infection of TZM-bl cells by tier 1 HIV-1 Env-pseudotyped viruses (B) or A3R5 cells by tier 2 HIV-1 Env-pseudotyped viruses (C). Results are expressed as the 50% infectious dose (ID50) for pseudotyped viruses. Error bars indicate standard deviations.
DISCUSSION
Most current HIV-1 vaccine candidates are replication defective, administered intramuscularly, and unlikely to induce immune responses at mucosal surfaces. The goal of this study was to develop an orally administered replication-competent reovirus-based HIV-1 vaccine that stimulates mucosal and systemic humoral immune responses against broadly neutralizing epitopes of HIV-1. Reovirus infects intestinal mucosa to stimulate potent immune responses (58, 59), is naturally attenuated in humans (25, 60, 61), and can be manipulated to express vaccine antigens (32, 33). These features make reovirus an ideal HIV-1 vaccine vector.
In mice, reovirus initiates infection by traversing M cells overlying Peyer’s patches (PPs) in the small intestine (62, 63) and undergoes primary replication in adjacent epithelial cells and PP mononuclear cells (64–66). The reovirus-specific humoral immune response is characterized by mucosal IgA production through priming of B lymphocytes and development of plasma cells in PPs, mesenteric lymph nodes, and the spleen (67). IgA and IgG responses are directed against reovirus outer capsid proteins σ1, σ3, and μ1 (67–70), and reovirus-specific IgA and IgG antibodies prevent viral intestinal infection and systemic dissemination (68), respectively. Disease associated with reovirus infection is rare and limited to the very young, who recover without sequelae (22, 71–73). Preexisting immunity to reovirus is not a barrier to induction of immune responses, as demonstrated during clinical trials in which reovirus was used as an oncolytic adjunct to cancer chemotherapy (24).
We engineered reovirus vectors to display epitopes derived from the HIV-1 gp41 MPER that elicit broadly neutralizing antibodies. The resulting REO-MPER vectors replicated comparably to wild-type virus in cell culture, retained the inserted sequences following 10 serial cell culture passages, and were recognized by an MPER-specific MAb that neutralizes HIV-1 infection in cultured cells and protects against HIV-1 challenge in animal models. REO-MPER vectors elicit high-titer reovirus-specific antibody responses in mice and rabbits but fail to induce MPER-specific antibody responses or HIV-1 neutralization activity. Collectively, these data indicate that reovirus can be manipulated to display antigenic epitopes. However, the REO-MPER vectors used in this study did not yield detectable HIV-1-specific immune responses.
Several vector systems have been designed to display HIV-1 MPER sequences. These include adenovirus (74), hepatitis A virus (75), hepatitis B virus (76), influenza A virus (77), papillomavirus (78), potato virus X (79), and rhinovirus (80). However, these MPER-expressing vectors failed to elicit neutralizing antibody responses in animal models. In this regard, the MPER epitopes in each vector were displayed as monomeric units within surface-exposed loops of vector capsid components, whereas these epitopes form α-helical coiled-coil trimers in native gp41 (8). The strategy used here yielded vectors that displayed MPER sequences in the native trimeric conformation. Nonetheless, these vectors did not elicit MPER-specific immune responses.
What accounts for the failure of REO-MPER vectors to stimulate production of MPER-specific antibodies in mice and rabbits? It is possible that the epitope inserted into σ1 is not fully native. Although the σ1 tail domain may be sufficient to allow MPER epitopes to form trimers, additional structural constraints provided by the native gp41 framework could be required for the epitopes to be displayed in an immunogenic manner. We think this possibility is less likely, as MAb 2F5 is capable of binding REO-MPER vectors that display amino acid sequences that constitute the 2F5 epitope. It also is possible that generation of MPER-specific antibodies requires association with lipid. The MPER is immediately adjacent to the viral membrane (81), and some antibodies that recognize MPER epitopes, including 2F5 and 4E10, require interaction with lipid along with engagement of gp41 (82, 83). To our knowledge, σ1 does not associate with membranes and, therefore, it may be difficult to engineer MPER-containing σ1 molecules with the capacity to elicit MPER-specific antibodies if lipid engagement is required for immunogenicity. Alternatively, mice and rabbits may be incapable of producing an MPER-specific antibody response, even following three immunizations with a vector that appropriately displays the target epitope. MPER-specific antibodies in humans are characterized by substantial somatic hypermutation (84), which likely takes a prolonged interval (on the order of months to years) of chronic infection to develop (85, 86). The immunization protocols used in our study would not likely recapitulate the exposure of the MPER epitope required to generate an effective antibody response. Moreover, the CDR3 region of MPER-specific MAbs is much longer than the corresponding region of mouse or rabbit antibodies, which may preclude development of MPER-specific antibody responses in these animals (52, 87).
Our findings indicate that reovirus can be engineered to display foreign epitopes. The α-helical coiled-coil σ1 tail domain appears to tolerate insertion of heterologous sequences as long as the heptad repeat register is maintained. A common theme among enveloped viruses is utilization of viral proteins that contain α-helical motifs to mediate fusion of the viral envelope with the cell membrane during virus entry (31). For many human-pathogenic viruses, including Ebola virus (88) and influenza virus (89), broadly neutralizing antibodies have been isolated that bind to these α-helical coiled-coil regions and prevent infection. It is possible that reovirus vectors constructed to display these sequences will elicit protective immune responses.
MATERIALS AND METHODS
Cell lines.
L929 (L) cells were maintained in Joklik’s minimal essential medium (Lonza) supplemented to contain 5% fetal bovine serum (FBS), 2 mM l-glutamine, 100 U/ml penicillin, 100 µg/ml streptomycin, and 25 ng/ml amphotericin B. HeLa cells were maintained in Dulbecco’s modified Eagle medium (DMEM; Gibco) supplemented to contain 10% FBS, 2 mM l-glutamine, 100 U/ml penicillin, 100 µg/ml streptomycin, and 25 ng/ml amphotericin B (Invitrogen). BHK-T7 cells were maintained in DMEM supplemented to contain 5% FBS, 2 mM l-glutamine, 2% minimal essential medium amino acid solution (Invitrogen), and 1 mg/ml Geneticin (Invitrogen).
Viruses.
Recombinant reoviruses were recovered by using plasmid-based reverse genetics (32, 33). Monolayers of BHK-T7 cells at approximately 90% confluence (3 × 106 cells) in 60-mm dishes (Corning) were cotransfected with nine plasmid constructs representing cloned gene segments from strain T1L: pT7-L1T1L (2 µg), pT7-L2T1L (2 µg), pT7-L3T1L (2 µg), pT7-M1T1L (1.75 µg), pT7-M2T1L (1.75 µg), pT7-M3T1L (1.75 µg), pT7-S2T1L (1.5 µg), pT7-S3T1L (1.5 µg), and pT7-S4T1L (1.5 µg), in combination with 2 µg of pBacT7-S1T1L or S1-MPER constructs. For each transfection mixture, 3 µl of TransIT-LT1 transfection reagent (Mirus) was used per microgram of plasmid DNA. Following 2 days of incubation, recombinant virus was isolated from transfected cells by plaque purification using monolayers of L cells (90). To engineer recombinant viruses displaying MPER sequences in σ1, pBacT7-S1T1L was altered via QuikChange (Stratagene) site-directed mutagenesis. Nucleotides encoding amino acids 56 to 69 and 147 to 160 of T1L σ1 were exchanged with sequences encoding residues 656 to 669 of gp160 (the precursor of gp41) from HIV-1 strain Ba-L (656-NEQELLELDKWASL-669) spanning the entire 2F5 epitope. Nucleotides encoding amino acids 63 to 90, 98 to 125, and 147 to 174 (four heptad repeats) of T1L σ1 were exchanged with sequences encoding the entire MPER motif from HIV-1 strain Ba-L (656-NEQELLELDKWASLWNWFDITKWLWYIK-683). Sequences encoding whole MPER insertions of four heptad repeats were synthesized by GenScript, introduced into the PstI site of pUC57, and subcloned into pBacT7-S1 by using a TaKaRa DNA ligation kit (Clontech). Sequences of mutant viruses were confirmed using S1 gene cDNAs prepared from viral RNA extracted from purified virions subjected to OneStep reverse transcription-PCR (RT-PCR; Qiagen) with S1-specific primers. Primer sequences are available from the corresponding authors upon request. PCR products were analyzed following electrophoresis in Tris-borate-EDTA agarose gels or purified and subjected directly to sequence analysis.
Purified reovirus virions were prepared using second- or third-passage L cell lysate stocks of twice-plaque-purified reovirus, as described elsewhere (26). Viral particles were freon extracted from infected cell lysates, layered onto 1.2- to 1.4-g/cm3 CsCl gradients, and centrifuged at 62,000 × g for 18 h. Bands corresponding to virions (1.36 g/cm3) (91) were collected and dialyzed in virion storage buffer (150 mM NaCl, 15 mM MgCl2, 10 mM Tris-HCl [pH 7.4]). The concentration of reovirus virions in purified preparations was determined from the equivalence of one optical density (OD) unit at 260 nm to 2.1 × 1012 virions (91). Viral titers were determined by plaque assay using L cells (90).
Virus replication assays.
For assays of viral yield, L cells (5 × 104 cells/well) seeded in 24-well plates (Costar) were adsorbed in triplicate with reovirus strains at a multiplicity of infection (MOI) of 1 PFU/cell at room temperature for 1 h in serum-free medium, washed once with Dulbecco’s phosphate-buffered saline without calcium or magnesium (PBS; Invitrogen), and incubated in serum-containing medium for various intervals. Cells were frozen and thawed twice prior to determination of viral titer by plaque assay using L cells (90). Viral yield was calculated using the following formula: log10 yield at tx = log10(PFU/ml)tx − log10(PFU/ml)t0, where t is the time postadsorption.
Serial passage of reovirus vectors in cell culture.
Recombinant viruses were consecutively passaged 8 to 10 times in confluent monolayers of L cells cultivated in T-25 tissue culture flasks (Costar) by inoculating cells with 1 ml of virus stock diluted to provide a low MOI. Cells were lysed by freezing and thawing twice, and viral RNA from each passage was purified from culture lysates by using an RNA isolation kit (Roche). RNA was converted to cDNA via OneStep RT-PCR (Qiagen) using S1-specific primers, and cDNAs were sequenced.
Detection of MPER epitopes by FLISA.
Black, clear-bottom, 96-well plates (Costar) were coated with 1010 or 1011 particles of either rsT1L or recombinant reovirus strains and incubated with 2.5 µg/ml of MAb 2F5 (92) and rabbit σ1 head-specific antiserum (47) at 37°C for 1 h. Antibody binding to the 2F5 epitope displayed by immobilized virus was detected following incubation with fluorophore-conjugated donkey anti-human IgG (Rockland). Antibody binding to the σ1 head was detected following incubation with goat anti-rabbit antiserum (LI-COR). FLISA signals were quantified using a LI-COR Odyssey infrared imaging system and are expressed as the relative signal strength, proportional to the quantity of dye-labeled antibody bound per well. Background fluorophore-conjugated antibody binding to empty wells was subtracted from that in particle-coated wells to determine the final integrated intensity values.
Infection of mice and rabbits.
Reovirus-seronegative BALB/c mice were obtained from Jackson Laboratory. Fifteen 6-week-old mice were inoculated with wild-type rsT1L, rsT1L/σ1 2F5-56, or rsT1L/σ1 2F5-147 diluted in PBS on day 0 and were boosted on days 21 and 42. Blood samples were obtained by tail vein puncture on day 0 (prior to inoculation) and on days 14 and 70. The dose of reovirus used for all mouse inoculations ranged from 106 to 107 PFU/ml.
Reovirus-seronegative New Zealand White rabbits were obtained from Covance, Inc. Purified recombinant reovirus was emulsified in TiterMax gold adjuvant (Sigma-Aldrich) for the first experiment and PBS for the subsequent experiment. For the first experiment, eight 14-week-old rabbits were inoculated intramuscularly in the hind limb with rsT1L or rsT1L/σ1 2F5-147 on day 0 and boosted on days 21 and 42. Blood samples were obtained by ear central artery puncture on days 0 (prior to immunization), 14, 35, 56, and 70. For the second experiment, 10 14-week-old rabbits were inoculated intramuscularly in the hind limb with rsT1L, rsT1L/σ1 MPER-63, or rsT1L/σ1 MPER-98 on day 0 and boosted on days 21 and 42. Blood samples were collected on days 0 (prior to immunization), 14, 35, and 56. The dose of reovirus used for all rabbit inoculations ranged from 108 to 109 PFU/ml.
Animal husbandry and experimental procedures were performed in accordance with Public Health Service policy and approved by the Vanderbilt University School of Medicine Institutional Animal Care and Use Committee.
Quantification of reovirus-specific antibody responses.
Reovirus-specific antibody responses were determined in PRNT60 assays with rsT1L and L cells. Serum samples were heat inactivated at 56°C for 30 min, serially diluted 4-fold beginning with a dilution of 1:20, and incubated with an equal volume of a virus stock containing 100 PFU. After incubation for 1 h, the serum-virus mixtures were inoculated in duplicate onto confluent L-cell monolayers in 6-well tissue culture plates (Costar). Cells were stained with neutral red on day 7, and plaques were enumerated (90). Serum reciprocal geometric mean titers capable of reducing plaque counts by 60% were calculated via regression analysis. Seroconversion was defined as a ≥4-fold increase in serum neutralizing antibody titer to rsT1L at study days 14, 35, 56, and 70 compared with the prevaccination PRNT60.
Detection of 2F5 epitope-specific antibodies by immunofluorescence.
Pre- and postimmunization serum samples from vaccine recipient and control animals were evaluated for MPER-specific antibodies by FLISA and kinetic enzyme-linked immunosorbent assay (ELISA) (93) using a reference panel of HIV-1 MPER-specific peptides (15-mers; NIH AIDS Research and Reference Reagent Program). Duplicate wells were coated with 2F5 epitope-containing peptides 8926 (EQELLELDKWASLWN), 8927 (LELDKWASLWNWFDI), or negative-control peptide 8888 (VVQREKRAVGIGAMF). An uncoated well was included with each test sample to determine the background level of binding, which was subtracted from the test sample result. A standard curve prepared using a positive rabbit antiserum (provided by G. Ofek, NIH) was included in each assay as a positive control. The kinetic ELISA was developed by addition of biotinylated goat anti-rabbit IgG conjugated with streptavidin-horseradish peroxidase, followed by addition of the substrate 2,2′-azino-bis(3-ethylbenzothiazoline-6-sulfonic acid) diammonium salt (ABTS). Binding was quantified using a Molecular Devices microplate reader and Molecular Devices Softmax software.
Quantification of HIV-1-neutralizing antibody responses.
Serum samples from rabbits were evaluated for the capacity to neutralize a tier 1 HIV-1-Env-containing pseudovirus (W61D TCLA.71) in a TZM-bl assay (56) or a tier 2 HIV-1-Env-containing Renilla luciferase-encoding infectious molecular clone (WITO.LucR.T2A.ecto) using A3R5 cells (57, 94). Reagents were obtained from the NIH AIDS Research and Reference Reagent Program. These assays were performed in a biosafety level 3 laboratory.
Statistical analysis.
Means of triplicate samples were compared by using an unpaired Student’s t test or one-way analysis of variance (ANOVA). Statistical analyses were performed using Prism 6.0 software (GraphPad Software, Inc.). P values of <0.05 were considered statistically significant.
Preparation of the σ1 schematic.
The full-length schematic of σ1 (Fig. 1B) was prepared using the Chimera program from the University of California, San Francisco (http://www.rbvi.ucsf.edu/chimera).
ACKNOWLEDGMENTS
We thank members of the Dermody lab for essential discussions during the course of this research, Richard D’Aquila, Spyros Kalams, and Herman Staats for assistance with the design of the immunization protocols, and Thilo Stehle for advice about placement of the MPER epitopes into σ1. We thank Danica Sutherland for generating the reovirus σ1 schematic. We are grateful to the Vanderbilt University Medical Center Division of Animal Care for expert husbandry of the animals used in this study.
This work was supported by Public Health Service awards R21 AI091537 (T.S.D.) and U01 AI78407 (J.E.C., Jr.) from the National Institute of Allergy and Infectious Disease and the Elizabeth B. Lamb Center for Pediatric Research. Additional support was provided by Public Health Service awards P30 CA68485 for the Vanderbilt-Ingram Cancer Center and P30 DK20593 for the Vanderbilt Diabetes Research and Training Center.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
REFERENCES
- 1.Mehandru S, Wrin T, Galovich J, Stiegler G, Vcelar B, Hurley A, Hogan C, Vasan S, Katinger H, Petropoulos CJ, Markowitz M. 2004. Neutralization profiles of newly transmitted human immunodeficiency virus type 1 by monoclonal antibodies 2G12, 2F5, and 4E10. J Virol 78:14039–14042. doi: 10.1128/JVI.78.24.14039-14042.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Binley JM, Wrin T, Korber B, Zwick MB, Wang M, Chappey C, Stiegler G, Kunert R, Zolla-Pazner S, Katinger H, Petropoulos CJ, Burton DR. 2004. Comprehensive cross-clade neutralization analysis of a panel of anti-human immunodeficiency virus type 1 monoclonal antibodies. J Virol 78:13232–13252. doi: 10.1128/JVI.78.23.13232-13252.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hager-Braun C, Katinger H, Tomer KB. 2006. The HIV-neutralizing monoclonal antibody 4E10 recognizes N-terminal sequences on the native antigen. J Immunol 176:7471–7481. doi: 10.4049/jimmunol.176.12.7471. [DOI] [PubMed] [Google Scholar]
- 4.Scheid JF, Mouquet H, Feldhahn N, Seaman MS, Velinzon K, Pietzsch J, Ott RG, Anthony RM, Zebroski H, Hurley A, Phogat A, Chakrabarti B, Li Y, Connors M, Pereyra F, Walker BD, Wardemann H, Ho D, Wyatt RT, Mascola JR, Ravetch JV, Nussenzweig MC. 2009. Broad diversity of neutralizing antibodies isolated from memory B cells in HIV-infected individuals. Nature 458:636–640. doi: 10.1038/nature07930. [DOI] [PubMed] [Google Scholar]
- 5.Walker LM, Phogat SK, Chan-Hui PY, Wagner D, Phung P, Goss JL, Wrin T, Simek MD, Fling S, Mitcham JL, Lehrman JK, Priddy FH, Olsen OA, Frey SM, Hammond PW, Protocol G Principal Investigators, Kaminsky S, Zamb T, Moyle M, Koff WC, Poignard P, Burton DR. 2009. Broad and potent neutralizing antibodies from an African donor reveal a new HIV-1 vaccine target. Science 326:285–289. doi: 10.1126/science.1178746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang J, Ofek G, Laub L, Louder MK, Doria-Rose NA, Longo NS, Imamichi H, Bailer RT, Chakrabarti B, Sharma SK, Alam SM, Wang T, Yang Y, Zhang B, Migueles SA, Wyatt R, Haynes BF, Kwong PD, Mascola JR, Connors M. 2012. Broad and potent neutralization of HIV-1 by a gp41-specific human antibody. Nature 491:406–412. doi: 10.1038/nature11544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zwick MB, Jensen R, Church S, Wang M, Stiegler G, Kunert R, Katinger H, Burton DR. 2005. Anti-human immunodeficiency virus type 1 (HIV-1) antibodies 2F5 and 4E10 require surprisingly few crucial residues in the membrane-proximal external region of glycoprotein gp41 to neutralize HIV-1. J Virol 79:1252–1261. doi: 10.1128/JVI.79.2.1252-1261.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montero M, van Houten NE, Wang X, Scott JK. 2008. The membrane-proximal external region of the human immunodeficiency virus type 1 envelope: dominant site of antibody neutralization and target for vaccine design. Microbiol Mol Biol Rev 72:54–84. doi: 10.1128/MMBR.00020-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Landais E, Huang X, Havenar-Daughton C, Murrell B, Price MA, Wickramasinghe L, Ramos A, Bian CB, Simek M, Allen S, Karita E, Kilembe W, Lakhi S, Inambao M, Kamali A, Sanders EJ, Anzala O, Edward V, Bekker LG, Tang J, Gilmour J, Kosakovsky-Pond SL, Phung P, Wrin T, Crotty S, Godzik A, Poignard P. 2016. Broadly neutralizing antibody responses in a large longitudinal sub-Saharan HIV primary infection cohort. PLoS Pathog 12:e00086-16. doi: 10.1371/journal.ppat.1005369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frey G, Peng H, Rits-Volloch S, Morelli M, Cheng Y, Chen B. 2008. A fusion-intermediate state of HIV-1 gp41 targeted by broadly neutralizing antibodies. Proc Natl Acad Sci U S A 105:3739–3744. doi: 10.1073/pnas.0800255105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devash Y, Calvelli TA, Wood DG, Reagan KJ, Rubinstein A. 1990. Vertical transmission of human immunodeficiency virus is correlated with the absence of high-affinity/avidity maternal antibodies to the gp120 principal neutralizing domain. Proc Natl Acad Sci U S A 87:3445–3449. doi: 10.1073/pnas.87.9.3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robertson CA, Mok JYQ, Froebel KS, Simmonds P, Burns SM, Marsden HS, Graham S. 1992. Maternal antibodies to gp120 V3 sequence do not correlate with protection against vertical transmission of human immunodeficiency virus. J Infect Dis 166:704–709. doi: 10.1093/infdis/166.4.704. [DOI] [PubMed] [Google Scholar]
- 13.Ugen KE, Goedert JJ, Boyer J, Refaeli Y, Frank I, Williams WV, Willoughby A, Landesman S, Mendez H, Rubinstein A. 1992. Vertical transmission of human immunodeficiency virus (HIV) infection. Reactivity of maternal sera with glycoprotein 120 and 41 peptides from HIV type 1. J Clin Invest 89:1923–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alfsen A, Iniguez P, Bouguyon E, Bomsel M. 2001. Secretory IgA specific for a conserved epitope on gp41 envelope glycoprotein inhibits epithelial transcytosis of HIV-1. J Immunol 166:6257–6265. doi: 10.4049/jimmunol.166.10.6257. [DOI] [PubMed] [Google Scholar]
- 15.Conley AJ, Kessler JA II, Boots LJ, McKenna PM, Schleif WA, Emini EA, Mark GE III, Katinger H, Cobb EK, Lunceford SM, Rouse SR, Murthy KK. 1996. The consequence of passive administration of an anti-human immunodeficiency virus type 1 neutralizing monoclonal antibody before challenge of chimpanzees with a primary virus isolate. J Virol 70:6751–6758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hessell AJ, Rakasz EG, Tehrani DM, Huber M, Weisgrau KL, Landucci G, Forthal DN, Koff WC, Poignard P, Watkins DI, Burton DR. 2010. Broadly neutralizing monoclonal antibodies 2F5 and 4E10, directed against the human immunodeficiency virus type 1 gp41 membrane proximal external region protect against mucosal challenge by simian-human immunodeficiency virus SHIVBa-L. J Virol 84:1302–1313. doi: 10.1128/JVI.01272-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moog C, Dereuddre-Bosquet N, Teillaud J, Biedma ME, Holl V, Van Ham G, Heyndrickx L, Van Dorsselaer A, Katinger D, Vcelar B, Zolla-Pazner S, Mangeot I, Kelly C, Shattock RJ, Le Grand R. 2014. Protective effect of vaginal application of neutralizing and nonneutralizing inhibitory antibodies against vaginal SHIV challenge in macaques. Mucosal Immunol 7:46–56. doi: 10.1038/mi.2013.23. [DOI] [PubMed] [Google Scholar]
- 18.Dryden KA, Wang G, Yeager M, Nibert ML, Coombs KM, Furlong DB, Fields BN, Baker TS. 1993. Early steps in reovirus infection are associated with dramatic changes in supramolecular structure and protein conformation: analysis of virions and subviral particles by cryoelectron microscopy and image reconstruction. J Cell Biol 122:1023–1041. doi: 10.1083/jcb.122.5.1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gomatos PJ, Tamm I. 1963. The secondary structure of reovirus RNA. Proc Natl Acad Sci U S A 49:707–714. doi: 10.1073/pnas.49.5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee PWK, Hayes EC, Joklik WK. 1981. Protein σ1 is the reovirus cell attachment protein. Virology 108:156–163. doi: 10.1016/0042-6822(81)90535-3. [DOI] [PubMed] [Google Scholar]
- 21.Weiner HL, Powers ML, Fields BN. 1980. Absolute linkage of virulence and central nervous system cell tropism of reoviruses to viral hemagglutinin. J Infect Dis 141:609–616. doi: 10.1093/infdis/141.5.609. [DOI] [PubMed] [Google Scholar]
- 22.Dermody TS, Parker JS, Sherry B. 2013. Orthoreoviruses, p 1304–1346. In Knipe DM, Howley PM (ed), Fields virology, 6th ed. Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 23.Tai JH, Williams JV, Edwards KM, Wright PF, Crowe JE, Dermody TS. 2005. Prevalence of reovirus-specific antibodies in young children in Nashville, Tennessee. J Infect Dis 191:1221–1224. doi: 10.1086/428911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.White CL, Twigger KR, Vidal L, De Bono JS, Coffey M, Heinemann L, Morgan R, Merrick A, Errington F, Vile RG, Melcher AA, Pandha HS, Harrington KJ. 2008. Characterization of the adaptive and innate immune response to intravenous oncolytic reovirus (Dearing type 3) during a phase I clinical trial. Gene Ther 15:911–920. doi: 10.1038/gt.2008.21. [DOI] [PubMed] [Google Scholar]
- 25.Galanis E, Markovic SN, Suman VJ, Nuovo GJ, Vile RG, Kottke TJ, Nevala WK, Thompson MA, Lewis JE, Rumilla KM, Roulstone V, Harrington K, Linette GP, Maples WJ, Coffey M, Zwiebel J, Kendra K. 2012. Phase II trial of intravenous administration of Reolysin (reovirus serotype-3-Dearing strain) in patients with metastatic melanoma. Mol Ther 20:1998–2003. doi: 10.1038/mt.2012.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Furlong DB, Nibert ML, Fields BN. 1988. Sigma 1 protein of mammalian reoviruses extends from the surfaces of viral particles. J Virol 62:246–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fraser RD, Furlong DB, Trus BL, Nibert ML, Fields BN, Steven AC. 1990. Molecular structure of the cell-attachment protein of reovirus: correlation of computer-processed electron micrographs with sequence-based predictions. J Virol 64:2990–3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chappell JD, Prota AE, Dermody TS, Stehle T. 2002. Crystal structure of reovirus attachment protein sigma 1 reveals evolutionary relationship to adenovirus fiber. EMBO J 21:1–11. doi: 10.1093/emboj/21.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nibert ML, Dermody TS, Fields BN. 1990. Structure of the reovirus cell-attachment protein: a model for the domain organization of σ1. J Virol 64:2976–2989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reiter DM, Frierson JM, Halvorson EE, Kobayashi T, Dermody TS, Stehle T. 2011. Crystal structure of reovirus attachment protein σ1 in complex with sialylated oligosaccharides. PLoS Pathog 7:e00086-16. doi: 10.1371/journal.ppat.1002166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dutch RE, Jardetzky TS, Lamb RA. 2000. Virus membrane fusion proteins: biological machines that undergo a metamorphosis. Biosci Rep 20:597–612. doi: 10.1023/A:1010467106305. [DOI] [PubMed] [Google Scholar]
- 32.Kobayashi T, Antar AA, Boehme KW, Danthi P, Eby EA, Guglielmi KM, Holm GH, Johnson EM, Maginnis MS, Naik S, Skelton WB, Wetzel JD, Wilson GJ, Chappell JD, Dermody TS. 2007. A plasmid-based reverse genetics system for animal double-stranded RNA viruses. Cell Host Microbe 1:147–157. doi: 10.1016/j.chom.2007.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kobayashi T, Ooms LS, Ikizler M, Chappell JD, Dermody TS. 2010. An improved reverse genetics system for mammalian orthoreoviruses. Virology 398:194–200. doi: 10.1016/j.virol.2009.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kirchner E, Guglielmi KM, Strauss HM, Dermody TS, Stehle T. 2008. Structure of reovirus sigma 1 in complex with its receptor junctional adhesion molecule-A. PLoS Pathog 4:e00086-16. doi: 10.1371/journal.ppat.1000235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reiss K, Stencel JE, Liu Y, Blaum BS, Reiter DM, Feizi T, Dermody TS, Stehle T. 2012. The GM2 glycan serves as a functional coreceptor for serotype 1 reovirus. PLoS Pathog 8:e00086-16. doi: 10.1371/journal.ppat.1003078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bokiej M, Ogden KM, Ikizler M, Reiter DM, Stehle T, Dermody TS. 2012. Optimum length and flexibility of reovirus attachment protein σ1 are required for efficient viral infection. J Virol 86:10270–10280. doi: 10.1128/JVI.01338-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Doyle JD, Danthi P, Kendall EA, Ooms LS, Wetzel JD, Dermody TS. 2012. Molecular determinants of proteolytic disassembly of the reovirus outer capsid. J Biol Chem 287:8029–8038. doi: 10.1074/jbc.M111.334854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Doyle JD, Stencel-Baerenwald JE, Copeland CA, Rhoads JP, Brown JJ, Boyd KL, Atkinson JB, Dermody TS. 2015. Diminished reovirus capsid stability alters disease pathogenesis and littermate transmission. PLoS Pathog 11:e00086-16. doi: 10.1371/journal.ppat.1004693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Danthi P, Coffey CM, Parker JS, Abel TW, Dermody TS. 2008. Independent regulation of reovirus membrane penetration and apoptosis by the μ1 φ domain. PLoS Pathog 4:e00086-16. doi: 10.1391/journal.ppat.1000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Danthi P, Kobayashi T, Holm GH, Hansberger MW, Abel TW, Dermody TS. 2008. Reovirus apoptosis and virulence are regulated by host cell membrane penetration efficiency. J Virol 82:161–172. doi: 10.1128/JVI.01739-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zurney J, Kobayashi T, Holm GH, Dermody TS, Sherry B. 2009. The reovirus μ2 protein inhibits interferon signaling through a novel mechanism involving nuclear accumulation of interferon regulatory factor 9. J Virol 83:2178–2187. doi: 10.1128/JVI.01787-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Irvin SC, Zurney J, Ooms LS, Chappell JD, Dermody TS, Sherry B. 2012. A single amino acid polymorphism in reovirus protein μ2 determines repression of interferon signaling and modulates myocarditis. J Virol 86:2302–2311. doi: 10.1128/JVI.06236-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stebbing RE, Irvin SC, Rivera-Serrano EE, Boehme KW, Ikizler M, Yoder JA, Dermody TS, Sherry B. 2014. An ITAM in a nonenveloped virus regulates activation of NF-κB, induction of beta interferon, and viral spread. J Virol 88:2572–2583. doi: 10.1128/JVI.02573-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kobayashi T, Ooms LS, Chappell JD, Dermody TS. 2009. Identification of functional domains in reovirus replication proteins μNS and μ2. J Virol 83:2892–2906. doi: 10.1128/JVI.01495-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ooms LS, Kobayashi T, Dermody TS, Chappell JD. 2010. A post-entry step in the mammalian orthoreovirus replication cycle is a determinant of cell tropism. J Biol Chem 285:41604–41613. doi: 10.1074/jbc.M110.176255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ooms LS, Jerome WG, Dermody TS, Chappell JD. 2012. Reovirus replication protein 2 influences cell tropism by promoting particle assembly within viral inclusions. J Virol 86:10979–10987. doi: 10.1128/JVI.01172-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boehme KW, Guglielmi KM, Dermody TS. 2009. Reovirus nonstructural protein sigma1s is required for establishment of viremia and systemic dissemination. Proc Natl Acad Sci U S A 106:19986–19991. doi: 10.1073/pnas.0907412106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Frierson JM, Pruijssers AJ, Konopka JL, Reiter DM, Abel TW, Stehle T, Dermody TS. 2012. Utilization of sialylated glycans as coreceptors enhances the neurovirulence of serotype 3 reovirus. J Virol 86:13164–13173. doi: 10.1128/JVI.01822-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nygaard RM, Lahti L, Boehme KW, Ikizler M, Doyle JD, Dermody TS, Schiff LA. 2013. Genetic determinants of reovirus pathogenesis in a murine model of respiratory infection. J Virol 87:9279–9289. doi: 10.1128/JVI.00182-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stencel-Baerenwald J, Reiss K, Blaum BS, Colvin D, Li X, Abel T, Boyd K, Stehle T, Dermody TS. 2015. Glycan engagement dictates hydrocephalus induction by serotype 1 reovirus. mBio 6(2):e00086-16. doi: 10.1128/mBio.02356-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pruijssers AJ, Hengel H, Abel TW, Dermody TS. 2013. Apoptosis induction influences reovirus replication and virulence in newborn mice. J Virol 87:12980–12989. doi: 10.1128/JVI.01931-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zwick MB, Labrijn AF, Wang M, Spenlehauer C, Saphire EO, Binley JM, Moore JP, Stiegler G, Katinger H, Burton DR, Parren PW. 2001. Broadly neutralizing antibodies targeted to the membrane-proximal external region of human immunodeficiency virus type 1 glycoprotein gp41. J Virol 75:10892–10905. doi: 10.1128/JVI.75.22.10892-10905.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Parker CE, Deterding LJ, Hager-Braun C, Binley JM, Schulke N, Katinger H, Moore JP, Tomer KB. 2001. Fine definition of the epitope on the gp41 glycoprotein of human immunodeficiency virus type 1 for the neutralizing monoclonal antibody 2F5. J Virol 75:10906–10911. doi: 10.1128/JVI.75.22.10906-10911.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shen X, Parks RJ, Montefiori DC, Kirchherr JL, Keele BF, Decker JM, Blattner WA, Gao F, Weinhold KJ, Hicks CB, Greenberg ML, Hahn BH, Shaw GM, Haynes BF, Tomaras GD. 2009. In vivo gp41 antibodies targeting the 2F5 monoclonal antibody epitope mediate human immunodeficiency virus type 1 neutralization breadth. J Virol 83:3617–3625. doi: 10.1128/JVI.02631-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Haigwood NL. 2009. Update on animal models for HIV research. Eur J Immunol 39:1994–1999. doi: 10.1002/eji.200939576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Montefiori DC. 2009. Measuring HIV neutralization in a luciferase reporter gene assay. Methods Mol Biol 485:395–405. doi: 10.1007/978-1-59745-170-3_26. [DOI] [PubMed] [Google Scholar]
- 57.Sarzotti-Kelsoe M, Daniell X, Todd CA, Bilska M, Martelli A, LaBranche C, Perez LG, Ochsenbauer C, Kappes JC, Rountree W, Denny TN, Montefiori DC. 2014. Optimization and validation of a neutralizing antibody assay for HIV-1 in A3R5 cells. J Immunol Methods 409:147–160. doi: 10.1016/j.jim.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Silvey KJ, Hutchings AB, Vajdy M, Petzke MM, Neutra MR. 2001. Role of immunoglobulin A in protection against reovirus entry into murine Peyer’s patches. J Virol 75:10870–10879. doi: 10.1128/JVI.75.22.10870-10879.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hutchings AB, Helander A, Silvey KJ, Chandran K, Lucas WT, Nibert ML, Neutra MR. 2004. Secretory immunoglobulin A antibodies against the sigma1 outer capsid protein of reovirus type 1 Lang prevent infection of mouse Peyer’s patches. J Virol 78:947–957. doi: 10.1128/JVI.78.2.947-957.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kasel JA, Rosen L, Evans HE. 1963. Infection of human volunteers with a reovirus of bovine origin. Proc Soc Exp Biol Med 112:979–981. doi: 10.3181/00379727-112-28226. [DOI] [PubMed] [Google Scholar]
- 61.Vidal L, Pandha HS, Yap TA, White CL, Twigger K, Vile RG, Melcher A, Coffey M, Harrington KJ, DeBono JS. 2008. A phase I study of intravenous oncolytic reovirus type 3 Dearing in patients with advanced cancer. Clin Cancer Res 14:7127–7137. doi: 10.1158/1078-0432.CCR-08-0524. [DOI] [PubMed] [Google Scholar]
- 62.Wolf J, Rubin D, Finberg R, Kauffman R, Sharpe A, Trier J, Fields B. 1981. Intestinal M cells: a pathway for entry of reovirus into the host. Science 212:471–472. doi: 10.1126/science.6259737. [DOI] [PubMed] [Google Scholar]
- 63.Gonzalez-Hernandez MB, Liu T, Payne HC, Stencel-Baerenwald JE, Ikizler M, Yagita H, Dermody TS, Williams IR, Wobus CE. 2014. Efficient norovirus and reovirus replication in the mouse intestine requires microfold (M) cells. J Virol 88:6934–6943. doi: 10.1128/JVI.00204-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fleeton MN, Fleeton MN, Contractor N, Leon F, Wetzel JD, Dermody TS, Kelsall BL. 2004. Peyer’s patch dendritic cells process viral antigen from apoptotic epithelial cells in the intestine of reovirus-infected mice. J Exp Med 200:235–245. doi: 10.1084/jem.20041132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Johansson C, Wetzel JD, He JP, Mikacenic C, Dermody TS, Kelsall BL. 2007. Type I interferons produced by hematopoietic cells protect mice against lethal infection by mammalian reovirus. J Exp Med 204:1349–1358. doi: 10.1084/jem.20061587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Antar AAR, Konopka JL, Campbell JA, Henry RA, Perdigoto AL, Carter BD, Pozzi A, Abel TW, Dermody TS. 2009. Junctional adhesion molecule-A is required for hematogenous dissemination of reovirus. Cell Host Microbe 5:59–71. doi: 10.1016/j.chom.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.London SD, Rubin DH, Cebra JJ. 1987. Gut mucosal immunization with reovirus serotype 1-L stimulates virus-specific cytotoxic T cell precursors as well as IgA memory cells in Peyer’s patches. J Exp Med 165:830–847. doi: 10.1084/jem.165.3.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Major AS, Cuff CF. 1996. Effects of the route of infection on immunoglobulin G subclasses and specificity of the reovirus-specific humoral immune response. J Virol 70:5968–5974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Virgin HW IV, Mann MA, Fields BN, Tyler KL. 1991. Monoclonal antibodies to reovirus reveal structure/function relationships between capsid proteins and genetics of susceptibility to antibody action. J Virol 65:6772–6781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tyler KL, Mann MA, Fields BN, Virgin HW IV. 1993. Protective anti-reovirus monoclonal antibodies and their effects on viral pathogenesis. J Virol 67:3446–3453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Giordano MO, Martínez LC, Isa MB, Ferreyra LJ, Canna F, Paván JV, Paez M, Notario R, Nates SV, Nates SV. 2002. Twenty year study of the occurrence of reovirus infection in hospitalized children with acute gastroenteritis in Argentina. Pediatr Infect Dis J 21:880–882. doi: 10.1097/00006454-200209000-00021. [DOI] [PubMed] [Google Scholar]
- 72.Hermann L, Embree J, Hazelton P, Wells B, Coombs RTK. 2004. Reovirus type 2 isolated from cerebrospinal fluid. Pediatr Infect Dis J 23:373–375. doi: 10.1097/00006454-200404000-00026. [DOI] [PubMed] [Google Scholar]
- 73.Tyler K, Barton E, Ibach M, Robinson C, Valyi-Nagy T, Campbell JA, Clarke P, O’Donnell SM, Wetzel J, Dermody T. 2004. Isolation and molecular characterization of a novel type 3 reovirus from a child with meningitis. J Infect Dis 189:1664–1675. doi: 10.1086/383129. [DOI] [PubMed] [Google Scholar]
- 74.Ura T, Yoshida A, Xin K, Yoshizaki S, Yashima S, Abe S, Mizuguchi H, Okuda K. 2009. Designed recombinant adenovirus type 5 vector induced envelope-specific CD8(+) cytotoxic T lymphocytes and cross-reactive neutralizing antibodies against human immunodeficiency virus type 1. J Gene Med 11:139–149. doi: 10.1002/jgm.1277. [DOI] [PubMed] [Google Scholar]
- 75.Beneduce F, Kusov Y, Klinger M, Gauss-Müller V, Morace G. 2002. Chimeric hepatitis A virus particles presenting a foreign epitope (HIV gp41) at their surface. Antiviral Res 55:369–377. doi: 10.1016/S0166-3542(02)00073-6. [DOI] [PubMed] [Google Scholar]
- 76.Eckhart L, Raffelsberger W, Ferko B, Klima A, Purtscher M, Katinger H, Rüker F. 1996. Immunogenic presentation of a conserved gp41 epitope of human immunodeficiency virus type 1 on recombinant surface antigen of hepatitis B virus. J Gen Virol 77:2001–2008. doi: 10.1099/0022-1317-77-9-2001. [DOI] [PubMed] [Google Scholar]
- 77.Muster T, Ferko B, Klima A, Purtscher M, Trkola A, Schulz P, Grassauer A, Engelhardt OG, García-Sástre A, Palese P, Katinger H. 1995. Mucosal model of immunization against human immunodeficiency virus type 1 with a chimeric influenza virus. J Virol 69:6678–6686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang H, Huang Y, Fayad R, Spear GT, Qiao L. 2004. Induction of mucosal and systemic neutralizing antibodies against human immunodeficiency virus type 1 (HIV-1) by oral immunization with bovine papillomavirus-HIV-1 gp41 chimeric virus-like particles. J Virol 78:8342–8348. doi: 10.1128/JVI.78.15.8342-8348.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Marusic C, Rizza P, Lattanzi L, Mancini C, Spada M, Belardelli F, Benvenuto E, Capone I. 2001. Chimeric plant virus particles as immunogens for inducing murine and human immune responses against human immunodeficiency virus type 1. J Virol 75:8434–8439. doi: 10.1128/JVI.75.18.8434-8439.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Arnold GF, Velasco PK, Holmes AK, Wrin T, Geisler SC, Phung P, Tian Y, Resnick DA, Ma X, Mariano TM, Petropoulos CJ, Taylor JW, Katinger H, Arnold E. 2009. Broad neutralization of human immunodeficiency virus type 1 (HIV-1) elicited from human rhinoviruses that display the HIV-1 gp41 ELDKWA epitope. J Virol 83:5087–5100. doi: 10.1128/JVI.00184-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tran EEH, Borgnia MJ, Kuybeda O, Schauder DM, Bartesaghi A, Frank GA, Sapiro G, Milne JLS, Subramaniam S. 2012. Structural mechanism of trimeric HIV-1 envelope glycoprotein activation. PLoS Pathog 8:e00086-16. doi: 10.1371/journal.ppat.1002797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Alam SM, McAdams M, Boren D, Rak M, Scearce RM, Gao F, Camacho ZT, Gewirth D, Kelsoe G, Chen P, Haynes BF. 2007. The role of antibody polyspecificity and lipid reactivity in binding of broadly neutralizing anti-HIV-1 envelope human monoclonal antibodies 2F5 and 4E10 to glycoprotein 41 membrane proximal envelope epitopes. J Immunol 178:4424–4435. doi: 10.4049/jimmunol.178.7.4424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Matyas GR, Wieczorek L, Beck Z, Ochsenbauer-Jambor C, Kappes JC, Michael NL, Polonis VR, Alving CR. 2009. Neutralizing antibodies induced by liposomal HIV-1 glycoprotein 41 peptide simultaneously bind to both the 2F5 or 4E10 epitope and lipid epitopes. AIDS 23:2069–2077. doi: 10.1097/QAD.0b013e32832faea5. [DOI] [PubMed] [Google Scholar]
- 84.Klein F, Diskin R, Scheid J, Gaebler C, Mouquet H, Georgiev IS, Pancera M, Zhou T, Incesu R, Fu B, Gnanapragasam PP, Oliveira T, Seaman M, Kwong P, Bjorkman P, Nussenzweig M. 2013. Somatic mutations of the immunoglobulin framework are generally required for broad and potent HIV-1 neutralization. Cell 153:126–138. doi: 10.1016/j.cell.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gray ES, Madiga MC, Hermanus T, Moore PL, Wibmer CK, Tumba NL, Werner L, Mlisana K, Sibeko S, Williamson C, Abdool Karim SS, Morris L, CAPRISA002 Study Team . 2011. The neutralization breadth of HIV-1 develops incrementally over four years and is associated with CD4+ T cell decline and high viral load during acute infection. J Virol 85:4828–4840. doi: 10.1128/JVI.00198-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mikell I, Sather DN, Kalams SA, Altfeld M, Alter G, Stamatatos L. 2011. Characteristics of the earliest cross-neutralizing antibody response to HIV-1. PLoS Pathog 7:e00086-16. doi: 10.1371/journal.ppat.1001251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cardoso RMF, Zwick MB, Stanfield RL, Kunert R, Binley JM, Katinger H, Burton DR, Wilson IA. 2005. Broadly neutralizing anti-HIV antibody 4E10 recognizes a helical conformation of a highly conserved fusion-associated motif in gp41. Immunity 22:163–173. doi: 10.1016/j.immuni.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 88.Flyak A, Ilinykh P, Murin C, Garron T, Shen X, Fusco M, Hashiguchi T, Bornholdt Z, Slaughter J, Sapparapu G, Klages C, Ksiazek T, Ward A, Saphire E, Bukreyev A, Crowe J Jr.. 2015. Mechanism of human antibody-mediated neutralization of Marburg virus. Cell 160:893–903. doi: 10.1016/j.cell.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Throsby M, van den Brink E, Jongeneelen M, Poon LLM, Alard P, Cornelissen L, Bakker A, Cox F, van Deventer E, Guan Y, Cinatl J, ter Meulen JT, Lasters I, Carsetti R, Peiris M, de Kruif J, Goudsmit J. 2008. Heterosubtypic neutralizing monoclonal antibodies cross-protective against H5N1 and H1N1 recovered from human IgM+ memory B cells. PLoS One 3:e00086-16. doi: 10.1371/journal.pone.0003942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Virgin HW IV, Bassel-Duby R, Fields BN, Tyler KL. 1988. Antibody protects against lethal infection with the neurally spreading reovirus type 3 (Dearing). J Virol 62:4594–4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Smith RE, Zweerink HJ, Joklik WK. 1969. Polypeptide components of virions, top component and cores of reovirus type 3. Virology 39:791–810. doi: 10.1016/0042-6822(69)90017-8. [DOI] [PubMed] [Google Scholar]
- 92.Purtscher M, Trkola A, Gruber G, Buchacher A, Predl R, Steindl F, Tauer C, Berger R, Barrett N, Jungbauer A, Katinger H. 1994. A broadly neutralizing human monoclonal antibody against gp41 of human immunodeficiency virus type 1. AIDS Res Hum Retroviruses 10:1651–1658. doi: 10.1089/aid.1994.10.1651. [DOI] [PubMed] [Google Scholar]
- 93.Boyce TG, Gruber WC, Coleman-Dockery SD, Sannella EC, Reed GW, Wolff M, Wright PF. 1999. Mucosal immune response to trivalent live attenuated intranasal influenza vaccine in children. Vaccine 18:82–88. doi: 10.1016/S0264-410x(99)00183-8. [DOI] [PubMed] [Google Scholar]
- 94.Seaman MS, Janes H, Hawkins N, Grandpre LE, Devoy C, Giri A, Coffey RT, Harris L, Wood B, Daniels MG, Bhattacharya T, Lapedes A, Polonis VR, McCutchan FE, Gilbert PB, Self SG, Korber BT, Montefiori DC, Mascola JR. 2010. Tiered categorization of a diverse panel of HIV-1 Env pseudoviruses for assessment of neutralizing antibodies. J Virol 84:1439–1452. doi: 10.1128/JVI.02108-09. [DOI] [PMC free article] [PubMed] [Google Scholar]