Abstract
Purpose of review
The review describes the European epidemic and the challenges in moving from clinical trials of preexposure prophylaxis (PrEP) to routine practice.
Recent findings
Two European trials conducted in gay and other MSM and transgender women reported a high and consistent reduction in HIV incidence using oral PrEP with tenofovir/emtricitabine (TDF/FTC). The incidence of HIV infection in the control group was much higher than anticipated, based on routine surveillance data in MSM, in spite of the highest standard of HIV prevention available.
Summary
Recent results have highlighted the urgent need to make PrEP available to key populations in Europe as an additional prevention tool. Gilead has not yet submitted an application to use TDF/FTC as PrEP in Europe. Although regulatory approval would accelerate implementation, countries are already dispensing TDF/FTC as postexposure prophylaxis without this. Services for prevention are diverse across countries ranging from free, walk-in services for the diagnosis and treatment of HIV and other sexually transmitted infections, to insurance-dependent reimbursement of private clinical services. Momentum is gathering in Europe with PrEP demonstration projects in MSM and a growing demand from community organizations. Each Member State urgently needs to identify their key populations and determine the service best placed to provide this new prevention strategy within a comprehensive prevention package.
Keywords: Europe, health services, key populations, MSM, preexposure prophylaxis
INTRODUCTION
Europe did not participate in the early trials of preexposure prophylaxis (PrEP), but this was not the only reason for the delay in accepting the potential of this intervention to impact on the HIV epidemic in our setting. The benefit appeared to be modest, the costs to largely centrally funded health systems were substantial, and the model for delivery that would ensure adequate access was not clear. In this review, we describe the European epidemic, the reasons that further clinical trials were deemed necessary, and the momentum that has been generated following the results of two trials.
Key populations in the European HIV epidemic
More than 29 000 persons were diagnosed with HIV in the 30 countries of the European Union and European Economic Area (EU/EEA) in 2013 [1]. The majority of these infections were because of sexual transmission, 12 000 (42%) of the new diagnoses were among MSM, and nearly 10 000 (32%) were among heterosexuals, many from countries with high HIV prevalence. About 1500 (5%) of the new HIV diagnoses were because of injecting drug use. The transmission route was not reported for 5741 (20%) of new diagnoses, and mother-to-child, nosocomial, and transfusion-related transmission were uncommon, accounting for less than 1% of new diagnoses.
HIV surveillance data do not include data on sex work as a risk factor. However, of the 14 EU/EEA countries that reported HIV estimates among female sex workers, prevalence was above 5% in three countries (Estonia, Latvia, and Portugal). Higher rates were reported among male sex workers, for example, 16.9% in Spain, 13.5% in Portugal, and 9.1% in Belgium. In Portugal, HIV prevalence was estimated at over 10% in both men and transgender sex workers and at 47.6% in sex workers who inject drugs [2].
Although Europe-wide data on HIV risk among transgender individuals are not available, a systematic review by Baral et al.[3▪▪] found that transgender women were 45–80 times more likely to have acquired HIV than nontransgender adults in Spain, Italy, and The Netherlands.
During the past decade, despite relatively high HIV treatment coverage and well established multicomponent prevention programmes existing in most EU/EEA countries, the number of new HIV diagnoses in the EU/EEA has not decreased. Since 2004, more than one-quarter of a million individuals were diagnosed with HIV in the EU/EEA. Despite the stable overall trend, the number of new HIV diagnoses among people who inject drugs and among migrants from high-prevalence countries has decreased markedly by 36 and 61%, respectively. Today, the only group in the EU/EEA in which new HIV diagnoses are increasing is MSM, where there have been year-on-year increases in all age groups, with the largest increases among men under 30 years of age and among men over 50 years [4]. Reasons for this increase are likely multifactorial, and may include high numbers of sexual partners among some MSM, and the increased use of alcohol and recreational drugs during sexual encounters with one or more individuals [5], and a reduction in condom use [6▪].
Box 1.
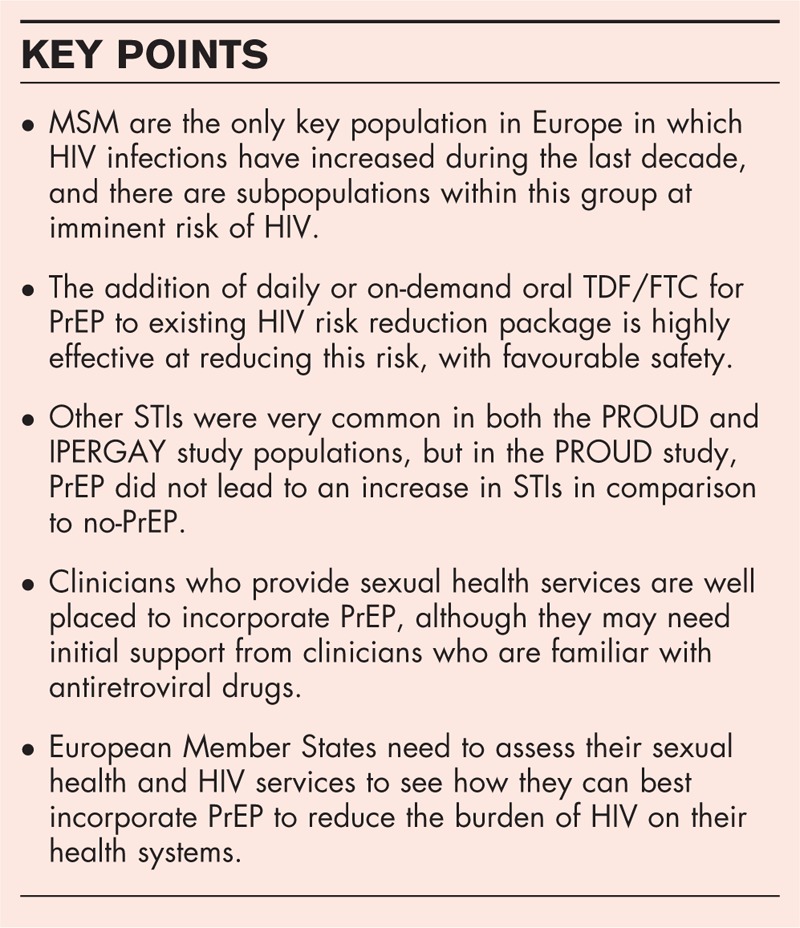
no caption available
Why were European preexposure prophylaxis trials needed?
Previous randomized controlled trials of tenofovir/emtricitabine (TDF/FTC) or TDF alone as PrEP had demonstrated excellent efficacy with full adherence in planned case–control subgroup analyses using plasma drug levels as a measure of adherence [7–10]. However, actual effectiveness as measured by an intent-to-treat analysis varied considerably, with two trials in women, FEM-PREP and VOICE, finding no evidence of benefit [11,12▪▪]. The variation in the intent-to-treat analyses mirrored the level of adherence in the trial populations. The evidence available in July 2012 was enough to satisfy the US Food and Drug Agency leading to the approval of TDF/FTC as PrEP. However, uptake of PrEP in the USA was initially slow and accompanied by considerable controversy in general and specifically within the gay community [13].
The competent authority for approval of medicines in Europe, the European Medicines Agency (EMA), issued a draft reflection paper [14] on PrEP highlighting outstanding research questions, with similar reservations to those expressed in the British HIV Association Position Statement [15], and summarized in a previous review [16▪]. The European Centre for Disease Control was similarly cautious [17]. The two largest areas of concern centred on, firstly, whether PrEP would have an overall negative impact on sexual health, condom use levels, and, in particular, other sexually transmitted infections (STIs), and, secondly, on its cost and cost–effectiveness. There was already considerable concern, especially within the gay community, that rates of condom use had been declining or at best had remained static ever since the introduction of combination antiretroviral therapy (ART) in 1997. The debate hinged on whether PrEP would further weaken gay men's adherence to condoms and whether the recommended behaviour change interventions had reached the limit of what they could do. The concern around whether PrEP would lead to risk compensation was not merely about whether that compensation would be so great as to abrogate the biological efficacy of PrEP, but also whether it would lead to a large increase in the already considerable burden of STIs among gay men. The 2012 EMA reflection paper noted that ‘an important caveat of a placebo-controlled study is that risk compensation – i.e. the potential adjustment of people's behaviour in response to the perceived reduction in risk – will not be detectable’, because trial participants will not know whether they are actually taking PrEP. To respond to this, the UK PROUD study was developed to assess risk compensation in an open-label controlled design.
Regarding cost and cost–effectiveness, TDF/FTC is expensive and has to offer considerable advantages to standard-of-care HIV prevention methods in terms of effectiveness if it is to demonstrate cost–effectiveness. A 2013 meta-analysis of cost–effectiveness studies [18] found that individual adherence and PrEP programme coverage significantly influenced cost–effectiveness, but that the most crucial factors were the cost of the drug and whether it was prioritized to high-incidence populations or not. Background incidence was the strongest determining factor of PrEP cost–effectiveness, and accurate targeting to high-incidence populations improved the cost–effectiveness of otherwise unaffordable programmes. The IPERGAY study was developed primarily to assess whether an intermittent, on-demand PrEP regimen (described below) would be effective, as there were clear potential advantages from the use of less drug in terms of lower toxicity, increased adherence, and reduced cost [19].
Two European trials
Two randomized, controlled trials of TDF/FTC were launched in Europe in 2012 recruiting MSM at risk of acquiring HIV infection. PROUD was designed to assess the net effect of biological efficacy, adherence to daily Truvada, and any impact on risk behaviour that could undermine biological efficacy [20▪▪]. The control group needed to be ‘no-PrEP’, and this comparison was created for the first year of follow-up as half of the participants were randomized to delayed access. IPERGAY was designed to assess an on-demand regimen (at the time of sexual intercourse): two tablets 2–24 h before sex, followed by one tablet 24 h later and a second tablet 48 h later, to be continued daily if risk was ongoing until 2 days after the last exposure [21▪▪].
Both trials started in the pilot phase. PROUD recruited MSM who were attending one of 13 sexual health clinics in England, where there is a network of over 200 clinics following the same clinical guidelines, and offering free services for HIV and other STIs. IPERGAY recruited initially through community peers in France and Canada, drawn from the organizations that were part of the consultation process, then using advertisements on social media and websites. Participants were enrolled in hospital clinics where staff had expertise in treating HIV. Although the eligibility criteria were broad, both studies attracted populations whose baseline characteristics suggested that they were at greater risk of acquiring HIV than the overall MSM population. In PROUD, these characteristics were the proportion who reported rectal gonorrhoea (26%), rectal chlamydia (21%), syphilis (10%), or the use of postexposure prophylaxis (PEP) in the preceding year (34%), the number of partners with whom they reported anal sex without a condom, and the proportion who had recently used one of the drugs recognized to increase sexual disinhibition (γ-hydroxybutyrate, 4-methylmethcathinone or methamphetamine). Context for the PROUD population is provided by the annual reports from the sexual health clinics in England to Public Health England [22]. In 2013, 92 607 HIV-negative MSM attended the clinics; rectal gonorrhoea was diagnosed in 2244 (2%), rectal chlamydia in 2454 (3%), and primary syphilis in 585 (<1%). There were a total of 4133 (4.5%) PEP prescriptions. These annual datasets, together with the avidity assay testing for recent infection, inform the HIV incidence estimates for the overall population of MSM attending sexual health clinics in England [23▪]. Compared with the current estimate of 1.34/100 person-years, the observed incidence in those not on PrEP in PROUD was approximately seven-fold higher at 9/100 person-years. The HIV incidence in IPERGAY was similarly much higher than expected in the placebo group (the sample size calculation assumed an incidence of 3/100 person-years and the observed incidence was 6.75/100 person-years) [21▪▪]. This implies that those that joined the studies appropriately assessed their risk through their own behaviour or their regular partners’ behaviours.
In both trials, TDF/FTC PrEP was remarkably effective, exceeding expectations as the reduction in HIV incidence observed in the modified intent-to-treat analyses was greater than any previously reported PrEP trial. Preceding trials used detectable drug to assess adherence and determine biological efficacy, but in IPERGAY and PROUD the circumstances for the five seroconversions that occurred in participants assigned to active drug strongly suggest that they were not taking PrEP at the time of HIV acquisition. As with previous PrEP trials, the self-reported adherence to PrEP was high. In contrast to some of the previous PrEP trials, this correlated with the detection of drug in the plasma [20▪▪,24▪]. Self-report suggested that the IPERGAY population were using 16 pills a month which is approximately half the amount of drug required to support a daily regimen. In both PROUD and IPERGAY, the safety of PrEP was good, consistent with previous PrEP reports with more drug-related gastrointestinal adverse events in those receiving TDF/FTC compared with those receiving placebo and with only one participant among the 400 enrolled in the IPERGAY trial who discontinued PrEP because of a suspected drug-related adverse event. The combination of PrEP effectiveness and high incidence in those not on PrEP led the Independent Data Monitoring Committee for PROUD to recommend a change in protocol to offer all participants PrEP. Following the PROUD press release, the Data and Safety Monitoring Board of the IPERGAY trial asked for an interim analysis of the data and recommended that all placebo participants be offered on-demand PrEP for the same reasons.
Gathering momentum
The European Centre for Disease Control updated their statement in April 2015 [25], stating that ‘on the basis of the new evidence, EU Member States should give consideration to integrating PrEP into their existing HIV prevention package for those most at-risk of HIV infection, starting with MSM. Issues related to larger-scale PrEP implementation, such as cost–effectiveness, appropriate models of care and access points, provider training, routine monitoring of patients, including adherence to treatment and regular testing for HIV and other STIs, will need to be assessed and carefully addressed in the context of each Member State's health system.’ The results from IPERGAY and PROUD have accelerated the development of two implementation projects – AMPrEP in Amsterdam which started on 22 June 2015, and Be-PrEP-ared which will launch in Antwerp in the autumn of 2015. Both projects will offer on-demand or daily PrEP to MSM, in line with the European AIDS Clinical Society recommendations which will be released later in October 2015. Other projects are expected to follow in 2016 in Ireland, Italy, Germany, Greece, Spain, and Slovenia. Although screening for HIV is freely and widely available in Europe, services beyond that are rarely free and invariably depend on insurance schemes. For example, women in the Netherlands pay for their contraception, and although the drugs for PEP are free in Ireland, there is a €25 fee for attendance at the Accident and Emergency department where these drugs are accessed. Large cities in Europe may have one or more facilities for the diagnosis and treatment of STIs, but these conditions are more typically managed in primary care where screening is motivated by symptoms rather than risk. Where drugs to treat HIV are commissioned centrally, it makes sense to use the same systems for the procurement of drugs to prevent HIV. Provided there are national guidelines, purchase through this mechanism is unlikely to require specific regulatory approval as it has not been necessary for PEP. Practitioners are willing to prescribe [26▪,27▪], but it is not yet clear in most European settings where PrEP would be dispensed from. In the absence of a national service for HIV and sexual health, countries will require a reconfiguration of existing services to bring together HIV testing, sexual healthcare, and antiretroviral prescribing expertise, and the demonstration projects are necessary to show this is feasible.
Gilead Sciences is now in dialogue with the EMA, although an application had not been submitted at the time of writing. EMA licensing is important as regulatory approval for the indication may be required by Member States that rely on reimbursement through insurance schemes. The French Ministry of Health has asked ANRS (French AIDS Research Agency) and the French National AIDS Council to provide a recommendation on PrEP by the end of 2015; the National Health Service England will decide in June 2016.
Awareness of and interest in PrEP in the community remained at a relatively low level in Europe till 2014, though when told about PrEP, many MSM expressed an interest in it [28]. PROUD and IPERGAY were both developed through a process of consultation with the community, starting with informed HIV treatment and prevention advocates who recruited other HIV and lesbian, gay, bisexual, and transgender sector advocates. Community organizations were responsible for the counselling and support aspects of IPERGAY, community representatives were on the steering committees of both studies, and both had community engagement strategies. This generated some interest, and in the case of IPERGAY, some controversy as its placebo-controlled design was criticized by some. This had a net positive effect; it generated more interest in the trial and also spurred an initiative of the French HIV community organisation AIDES, who, in answer to demands that there should be open-label access to PrEP outside the trial, asked that TDF/FTC be granted a Temporary Recommendation for Use for PrEP, a kind of expanded access programme for drugs used in a new indication, pending EMA approval. Gilead submitted an application to the French National Agency for Medicines Security where it is under review.
European interest was mainly restricted to HIV-sector activists until October 2014 when within a 2-week period, the PROUD and IPERGAY studies announced that all those not on TDF/FTC would be offered it. There was considerable press coverage of these decisions and the increased level of interest may be gauged by the fact that a rapidly written sign-on statement in support of PrEP in the United Kingdom attracted 2000 signatories within a week of appearing online [29]. The announcement in February 2015 of the actual effectiveness figures for both trials created a second wave of interest, including a pan-European statement of support, and the beginning of European social media groups for PrEP users and supporters such as the Nous Sommes PrEP group in France. The media and community response to PrEP in Europe since the trial results has been less polarized than in the United States: most commentary has been positive or neutral [30], and occasional hostile comments – such as one in the United Kingdom written by a former conservative party press officer [31] – have failed to gain much traction. The media and community interest in PrEP in most European countries continues to grow and activities range from expert discussions to community seminars, films, and even street demonstrations. So far there has not been a concerted pan-European support and advocacy campaign for PrEP but this is anticipated.
The cost–effectiveness data derived from the two European studies are promising. A 2015 study from Quebec in Canada used demographic and cost inputs from the IPERGAY study from the IPERGAY study participants in Quebec, and showed that PrEP was cost saving under most scenarios, despite using the 44% effectiveness observed in iPrEx instead of the observed 86% effectiveness of IPERGAY. Unlike many cost–effectiveness models, it added in the economic cost to society of HIV infection, such as loss of individuals to employment [32▪].
The first cost–effectiveness study using the 86% reduction in HIV incidence observed in PROUD was presented at a UK conference in June 2015 [33▪]. It looked at five different populations of MSM from a very restricted highest-risk group (five or more condomless sex partners in any one 3-month period in the last year) to larger groups such as that based on the PROUD eligibility criterion of one or more condomless sex partners in the last 3 months. It came to the conclusion that PrEP in the United Kingdom would be cost-effective or even cost saving if targeted at those reporting condomless anal sex with five or more partners, or presenting with a bacterial STI, providing HIV testing rates remain stable. However, they also demonstrated cost–effectiveness without targeting if the drug cost was half the list price.
A second cost–effectiveness study presented in September 2015 used a very different model, but came to similar conclusions [34▪]. It found that a small PrEP programme targeted to people at very high risk, with background incidence at 5% or higher per year (similar to incidence in people diagnosed with rectal STIs in the previous year), would be cost saving at current drug prices, but a larger programme, envisaged as offering PrEP to 5000 at-risk gay men per year, would require a 50–75% cut in drug price to be cost-effective.
The overall clinical trial evidence, which includes European populations, cost–effectiveness, and gathering advocacy, will inform policy decisions whether or not to commission PrEP throughout Europe. It will be interesting to see which country is the first European Member State to truly implement PrEP.
CONCLUSION
The strength of evidence provided by PROUD and IPERGAY among European MSM has served as a catalyst for demonstration projects in other European countries, not least of all because of the very high rate of HIV seen in both studies in the control group. These projects are helpful to show that existing services can incorporate PrEP appropriately into national HIV prevention and risk reduction strategies. This is important if PrEP is to have a sustained impact on the epidemic; however, the earliest PrEP is likely to be available outside such projects in mid-2016, 4 years behind the United States – a far greater gap than occurred in the rollout of antiretroviral therapy. European Member States need to act now to identify those most at risk in key population groups, and determine the appropriate health services to deliver PrEP. HIV testing services are widespread throughout Europe, but they need to develop referral pathways for PrEP as well as early treatment for those already infected to take advantage of the opportunity antiretroviral drugs provide to truly contain the HIV epidemic in Europe.
Acknowledgements
The authors wish to acknowledge the very helpful contribution of Dr Anastasia Pharris for her assistance with the paragraphs on the European Epidemic and supporting references as well as her comments on the overall draft.
Financial support and sponsorship
This work was supported by the institutions that employed the authors.
Conflicts of interest
S.Mc.C. is currently receiving a grant and support through provision of free drug from Gilead Sciences for the PROUD study. J.M.M. has received honoraria for attendance at an advisory board from Gilead Sciences, Bristol Myers Squibb, Merck, ViiV, Tobira Pharm., and Janssen. G.C. works for NAM and EATG, both of which receive grant income from Gilead Sciences, but has received no personal remuneration.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.HIV/AIDS Surveillance in Europe 2013. European Centre for Disease Prevention and Control (ECDC)/World Health Organisation Regional Office for Europe, 2014. [Google Scholar]
- 2.Control ECfDPa. Sex workers. Monitoring implementation of the Dublin Declaration on Partnership to Fight HIV/AIDS in Europe and Central Asia: 2014 progress report. 2015. [Google Scholar]
- 3▪▪.Baral SD, Poteat T, Stromdahl S, et al. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis 2013; 13:214–222. [DOI] [PubMed] [Google Scholar]; The study describes the 10-year trends of HIV cases diagnosed among key populations in theEU/EEA, showing that MSM are the only key population in Europe in which HIV diagnoses continue to increase.
- 4.Pharris A, Spiteri G, Noori T, Amato-Gauci AJ. Ten years after Dublin: principal trends in HIV surveillance in the EU/EEA, 2004 to 2013. Euro Surveill 2014; 19:20968. [DOI] [PubMed] [Google Scholar]
- 5.Men who have sex with men. Monitoring implementation of the Dublin Declaration on Partnership to Fight HIV/AIDS in Europe and Central Asia: 2014 progress report. 2015. [Google Scholar]
- 6▪.Aghaizu A, Nardone A, Copas A, et al. Understanding continuing high HIV incidence: sexual behavioural trends among MSM in London, 2000–2013. Abstract 05. BASHH Spring Conference 2015; 1–3 June 2015; Glasgow, Scotland. [Google Scholar]; Data from 10 annual cross-sectional self-completed surveys conducted in 2000–2013 in gay venues and linked to HIV testing. Results suggest an increasing trend in numbers of condomless anal sex partners combined with serosorting. One in 20 is estimated to be at risk of transmitting HIV, and within this group, there is a subgroup with a very high number of partners.
- 7.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med 2010; 363:2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med 2012; 367:399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med 2012; 367:423–434. [DOI] [PubMed] [Google Scholar]
- 10.Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet 2013; 381:2083–2090. [DOI] [PubMed] [Google Scholar]
- 11.Van Damme L, Corneli A, Ahmed K, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med 2012; 367:411–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12▪▪.Marrazzo JM, Ramjee G, Richardson BA, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med 2015; 372:509–518. [DOI] [PMC free article] [PubMed] [Google Scholar]; Randomized placebo controlled design evaluating daily oral tenofovir, daily vaginal tenofovir, and daily oral Truvada. No benefit was observed overall compared with placebo, but the majority of participants did not use product. When the women in the vaginal gel group with detectable TFV at the first visit were compared with those without there was a significant reduction in HIV.
- 13.New York Times Opinion Page Is PrEP a Good Way to Fight H.I.V. Infections? New York Times. 2014 June 17, 2014. [Google Scholar]
- 14.European Medicines Agency. Reflection paper on the nonclinical and clinical development for oral and topical HIV preexposure prophylaxis (PrEP). EMA/171264/2012. 2012. [Google Scholar]
- 15.McCormack S, Fidler S, Fisher M. The British HIV Association/British Association for Sexual Health and HIV Position Statement on preexposure prophylaxis in the UK. Int J STD AIDS 2012; 23:1–4. [DOI] [PubMed] [Google Scholar]
- 16▪.Molina JM, Pintado C, Gatey C, et al. Challenges and opportunities for oral preexposure prophylaxis in the prevention of HIV infection: where are we in Europe? BMC Med 2013; 11:186. [DOI] [PMC free article] [PubMed] [Google Scholar]; The review focuses on the challenges and opportunities of oral PrEP with TDF/FTC in Europe to curb the rising incidence of HIV infection in high-risk groups and explains why in Europe more research was needed in 2013 before PrEP could be implemented.
- 17.Evaluating HIV treatment as prevention in the European context. 2012. [Google Scholar]
- 18.Gomez GB, Borquez A, Case KK, et al. The cost and impact of scaling up preexposure prophylaxis for HIV prevention: a systematic review of cost-effectiveness modelling studies. PLoS Med 2013; 10:e1001401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lorente N, Fugon L, Carrieri MP, et al. Acceptability of an ‘on-demand’ preexposure HIV prophylaxis trial among men who have sex with men living in France. AIDS Care 2012; 24:468–477. [DOI] [PubMed] [Google Scholar]
- 20▪▪.McCormack S, Dunn D, Desai M. Preexposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]; Effectiveness emerged in the pilot phase of this randomized design, in which PrEP could be compared with no-PrEP, because HIV incidence was much higher than anticipated in the no-PrEP group, as was effectiveness.
- 21▪▪.Molina J-M, Capitant C, Charreau I. On Demand PrEP With Oral TDF-FTC in MSM: Results of the ANRS Ipergay Trial. Abstract 23LB. Conference on Retroviruses and Opportunistic Infections; 23–26 February 2015; Seattle, Washington; 2015. [Google Scholar]; The abstract presented the results of the ANRS IPERGAY trial demonstrating the high effectiveness (86% relative reduction of HIV incidence with TDF/FTC vs. placebo) and good tolerability of on-demand PrEP in France and Canada.
- 22.Public Health England. Genitourinary medicine clinic activity dataset (GUMCADv2). 2014. [Google Scholar]
- 23▪.Aghaizu A, Murphy G, Tosswill J, DeAngelis D, Charlett A, Gill N, et al. HIV incidence among people who attend sexual health clinics in England in 2012: estimates using a biomarker for recent infection. Abstract O4. BASHH Spring Conference 2015; 1–3 June 2015; Glasgow, Scotland: 2015. [Google Scholar]; Incidence estimates overall and for key populations in the UK (MSM, Black Africans) using clinic data and an avidity assay to detect recent infection. Results suggest that only 47% of incident infections are diagnosed within a year.
- 24▪.J F, Capitant C, Spire B. High adherence rate to intermittent oral PrEP with TDF/FTC among high risk MSM (ANRS IPERGAY). International AIDS Society; 20–25 July 2014; Melbourne, Australia: 2014. [Google Scholar]; The study provides important information about early adherence in the trial, as assessed by detection of drugs in plasma and hair samples. More than 80% of enrolled participants had drug levels detectable.
- 25.Preexposure prophylaxis to prevent HIV among MSM in Europe. 2015 30 April 2015. Report No. [Google Scholar]
- 26▪.Puro V, Palummieri A, De Carli G, et al. Attitude towards antiretroviral Pre-Exposure Prophylaxis (PrEP) prescription among HIV specialists. BMC Infect Dis 2013; 13:217. [DOI] [PMC free article] [PubMed] [Google Scholar]; Survey of Italian physicians who care for patients with HIV to determine attitudes to PrEP and willingness to prescribe.
- 27▪.Desai M, Gafos M, Dolling D, et al. Healthcare providers’ knowledge of, attitudes to and practice of preexposure prophylaxis for HIV infection. HIV Med 2015; Epub 2015/07/15. doi: 10.1111/hiv.12285. [DOI] [PubMed] [Google Scholar]; Survey of UK healthcare providers working in sexual health and/or HIV medicine to determine attitudes toward PrEP and support for a national programme.
- 28.Sigma Research. Prospective attitudes to HIV Preexposure prophylaxis (PrEP). 2011. [Google Scholar]
- 29.Statement on PrEP. 2014. http://www.prepaccess.org.uk/ [Accessed 7 September 2015]. [Google Scholar]
- 30.Boseley S. Daily pill Truvada cuts spread of HIV by 86%, study shows. The Guardian 2015. [Google Scholar]
- 31.Platell A. Why should WE pay for gays to have unsafe sex? Daily Mail. 2015. [Google Scholar]
- 32▪.Ouellet E, Durand M, Guertin JR, et al. Cost effectiveness of ‘on demand’ HIV preexposure prophylaxis for noninjection drug-using men who have sex with men in Canada. Can J Infect Dis Med Microbiol 2015; 26:23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this economic evaluation of the potential cost-effectiveness of on-demand PrEP in Canada, the authors use the PrEP effectiveness reported in the iPrEx trial (42%) and the design of the IPERGAY trial, and showed that the on-demand PrEP strategy ranged from cost saving to largely cost-effective.
- 33▪.Cambiano V, Miners A, Dunn D, et al. Is preexposure prophylaxis for HIV prevention cost-effective in men who have sex with men who engage in condomless sex in the UK? Abstract O1. BASHH Spring Conference 2015; 1–3 June 2015; Glasgow, Scotland: 2015. [Google Scholar]; In this cost-effectiveness study based on UK data, PrEP offered at current prices was found to be cost saving if offered to people with five or more condomless sex partners in the past year, or an STI diagnosis in the last 3 months. Price cuts of 50–80% would be necessary to make PrEP cost-effective for larger groups.
- 34▪.Ong K-J, Desai S, Desai M, et al. Will HIV PrEP given to high-risk MSM in England be cost-effective? Preliminary results of a static decision analytical model. Public Health England Conference, Coventry. September 2015. [Google Scholar]; The cost–effectiveness study based on UK data, but using a different model, in which PrEP was offered sequentially to the most high-risk gay men in any 1 year, found that PrEP (at the effectiveness seen in the PROUD study) would be cost saving if the background annual HIV incidence (i.e. without PrEP) of those men was more than about 5%, but would require price cuts of 50–75% to be cost-effective to larger groups with lower incidence.


