Abstract
This study examines the impact of the Family Check-Up, a school-based prevention program, as delivered in public secondary schools on suicide risk across adolescence. Students were randomly assigned to a family-centered intervention (N = 998) in sixth grade, and offered a multilevel intervention that included (a) a universal classroom-based intervention, (b) the Family Check-Up (selected; Dishion, Stormshak, & Kavanagh, 2011), and (c) family management treatment (indicated). Engagement with the FCU predicted significant reductions in suicide risk across adolescence and early adulthood.
Keywords: Family intervention, compliance, prevention, suicide risk, early adolescence
The development of prevention programs that reduce risk of suicide is a critical public health goal, as suicide represents one of the leading causes of death among youth aged 13 – 18 (Bridge, Goldstein, & Brent, 2006). Indeed, prevention programs targeting suicide risk in adolescence have been identified, with common components of successful programs including treatment aimed at both family and youth functioning (see Brent et al., 2013). Suicidal behavior is often related to a range of risk factors that overlap with broader emotion and behavior problems in youth, including harsh, critical parenting, elevated family conflict, peer relational difficulties, depression, conduct problems, and substance use in adolescence (see Bridge, Goldstein, & Brent, 2006). Given that many prevention programs for conduct-problems target similar risk factors, there may be crossover effects to the reduction of risk of suicide. Indeed, such crossover effects have been found in several such prevention programs (Hawkins, Kosterman, Catalano, Hill, & Abbot, 2005; Kerr, DeGarmo, & Leve, 2014; Lynn et al., 2014). For example, Wilcox and colleagues (2008) found that the classroom-based Good Behavior Game delivered in early elementary school predicted reductions in suicide risk at age 19 – 21 years.
The current analyses examined the effects of the Family Check-Up (FCU; Dishion, Stormshak, & Kavanagh, 2011) on suicide risk (an index of ideation and/or attempts) across adolescence and early adulthood. The FCU is a school-based prevention program initiated in sixth grade, and designed to reduce adolescent substance use and behavior problems through improving parenting skills and family functioning (see Dishion et al., 2011). The FCU program follows an adaptive intervention framework (Collins, Murphy and Bierman, 2004), in which intervention targets and doses are tailored to the individual needs of families. Advantages of adaptive designs include more efficient use of resources, increased intervention engagement, and greater resemblance to real-world clinical practice where treatment decisions are assessment-based (Collins, et al., 2004).
At the core of the intervention model is the FCU, which incorporates motivational interviewing techniques to enhance family engagement and trigger the behavior change process (Miller & Rollnick, 1991). The FCU is a three-session intervention designed to identify potential targets for intervention, support parent's motivation to engage in effective family management practices, and provide more intensive support for families in need. The outcome of the FCU is the identification of specific targets for subsequent family management support (see Dishion, et al., 2011), tailored to the individual strengths and goals of the parent. Given that the FCU targets aspects of family functioning that overlap with suicide prevention efforts (e.g. family conflict, coercive parenting, communication skills) and has demonstrated effects not only on the original targets (conduct problems, substance use, and family conflict; e.g., Connell, Dishion, Yasui, & Kavanagh, 2007; Van Ryzin & Dishion, 2012), but also on secondary outcomes such as depression (Connell et al., 2008; in press), we predict that the FCU program may have crossover effects on reducing suicide-risk as well.
Methods
Participants
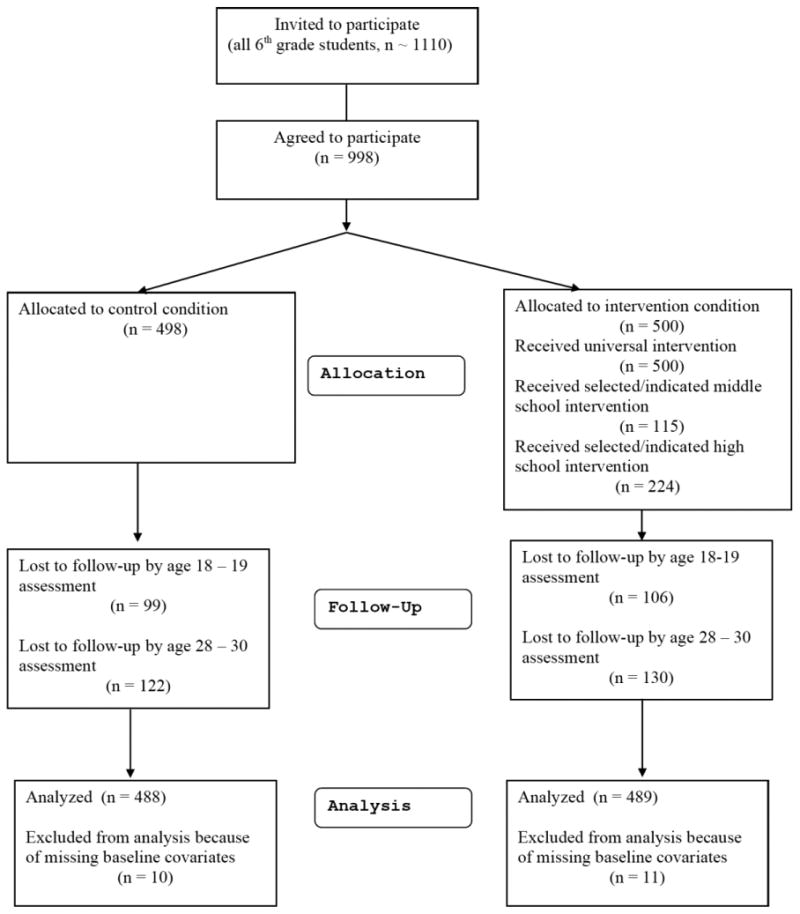
Participants included 998 adolescents and their families, recruited in sixth grade from three middle schools within a metropolitan community in the northwestern United States. Parents of all sixth grade students in two cohorts were approached for participation, and 90% consented to participate (see Figure 1). The sample included 526 males (52.7%) and 472 females (47.3%). There were 423 Caucasians (42.3%), 291 African Americans (29.1%), 68 Latinos (6.8%), 52 Asian American families (5.2%), and 164 (16.4%) youth of other ethnicities (including biracial). Biological fathers were present in 585 families (58.6%). Youth were randomly assigned at the individual level to either control (498 youth) or intervention classrooms (500 youth) in the spring of sixth grade.
Figure 1. Flow of participants through study.
Intervention Protocol
The FCU was designed for delivery in public schools, with a model that links universal, selected, and indicated family interventions, titrating intervention intensity to the needs and motivation of the family. (For more complete descriptions of the program, see Dishion, et al., 2011). The universal intervention involves universal screening, and the establishment of a family resource center in schools, which provided parent-centered services, including brief parent consultations and access to videotapes and books. The goal of these services was to support positive parenting practices and to engage parents of high-risk youth for the selected intervention with a multistage screening procedure. Students identified through this screening were referred to the selected level of intervention, the FCU, which is a brief assessment-driven intervention designed to motivate parenting change when it is needed, as determined by comprehensive assessment, including direct observations and parent and youth reports. Although all families in the intervention condition could receive the FCU, families of high-risk youth (as determined by teacher ratings) were specifically offered the FCU in seventh and eighth grades. An outcome of the FCU is the development of a menu of intervention options, including family-management training targets adapted from empirically supported parenting interventions, which represent the indicated level of intervention (Dishion, et al., 2011).
In the intervention condition, 115 families (23%) received the FCU in grades 7 - 9, and 88 families received further intervention services after the FCU. For Cohort 1, 46% of FCUs were completed following the seventh grade family assessment, 53% following the eighth grade assessment, and 1% following the ninth grade assessment. For Cohort 2, 93% of FCUs were completed following the seventh grade family assessment, and 7% following the eighth grade family assessment. These families had an average of 8.9 hours of direct contact with the intervention staff during the course of the study (SD = 9.42 hours). FCUs were also offered in high school (in Grades 10–11) for those families remaining in the school district, and 170 families (34%) received the FCU, 109 of whom had not received it during middle school. Therefore, 224 families (45%) received the FCU in middle school, high school, or both. Additionally, when youths were aged 16–17, they were offered the Teen Check-Up (TCU), that included the same three sessions as those in the FCU (initial interview, assessment, and feedback session), and directly involved the adolescent. In the intervention group, 174 youths (35%) participated in the TCU, including 58 whose families had not previously received the FCU.
Assessment Procedures
In the spring semester of sixth grade, student surveys were conducted in schools using an instrument developed by Metzler, Biglan, Rusby, & Sprague (2001). Students who moved out of their original schools were followed at their new location. Youth were paid $20 for completing each assessment.
Measures
Suicide Risk
Diagnostic interviews were administered to youth twice, at ages 18 – 19, and ages 28 - 30, using the Composite International Diagnostic Interview (CIDI; World Health Organization, 1997), administered by trained research staff unaware of the participant's intervention status. Due to study attrition, interviews were not available at age 18 for 206 youth (20.6%), and at age 28-30 for 244 youth (24.4%). Little's (1988) MCAR test indicated that the data was consistent with MCAR assumptions (age 18-19; χ2[71] = 73.70, n.s.; age 28-39, χ2[71] = 77.67, n.s.), supporting the use of FIML estimation. The Major Depressive Disorder (MDD) section of the CIDI includes four items reflecting thoughts of death (n = 107, age 18-19; n = 103, age 28-30), suicidal ideation (n = 56, age 18-19; n = 61, age 28-30), ideation with a plan (n = 21, age 18-19; n = 16, age 28-30), and attempts (n = 15, age 18-19; n = 11, age 28-30). A Suicide Risk Index was created by counting the number of items endorsed at each interview point, with potential scores ranging from 0 to 4. Only respondents endorsing screening items were administered the entire depression module including suicide items (n = 320, age 18-19; n = 200, age 28-30; n = 410 responded at least once).
Covariates
Baseline demographic factors (youth gender, ethnic minority status, and the presence of the biological father in the youth's primary residence), youth reports of substance use, antisocial behavior, positive family relationships, deviant peer affiliation, and parental monitoring, and teacher reports of behavioral risk were included as covariates. (For complete scale descriptions, and reliability and validity evidence, see Dishion, et al., 2011).
Engagement Status
Engagement status was coded to reflect family participation in the FCU (and further services as warranted). Families in the intervention condition who elected to receive the FCU were coded 1 (n = 115), and those who did not receive the FCU were coded 0 (n = 385). In the control condition, engagement status was coded as missing data.
Analytic plan
Because the FCU protocol follows an adaptive intervention design, with levels of intervention engagement self-selected by families randomly assigned to the intervention, Complier Average Causal Effect (CACE; see Jo, 2002) analysis was used to examine intervention effects on suicide risk. CACE analysis permits the examination of intervention effects specifically among families who engaged with treatment, using a finite mixture modeling approach to identify latent “engager” and “non-engager” classes in the full sample, with observed engagement in the intervention class used to estimate most-likely engagement status in the control condition.
CACE estimates are unbiased, if five assumptions are met (see Jo, 2002), including that: (1) treatment assignment is random, (2) the rate of compliance with treatment is not zero, (3) outcomes for individuals are independent of one another, and (4) there are no “defiers,” (e.g., members of the control group who receive the active intervention). The most challenging assumption, known as the exclusion restriction, states that random assignment to treatment does not affect the outcomes of individuals who do not comply with treatment. The inclusion of covariates predicting class membership can, however, ameliorate potential bias in model results if the exclusion restriction assumption is violated (see Jo, 2002). Prior work suggests that these assumptions are reasonable for the current trial (see Connell et al., 2007).
The model is depicted graphically in Figure 2. As shown, latent class membership and within-class variation in suicide risk were regressed on baseline demographic and risk variables. Intervention was allowed to predict within-class variation in suicide risk scores only within-the engager class (consistent with the exclusion restriction assumption). Finally, age 28-30 suicide risk was regressed on age 18-19 suicide risk.
Figure 2. CACE model examining suicide risk.
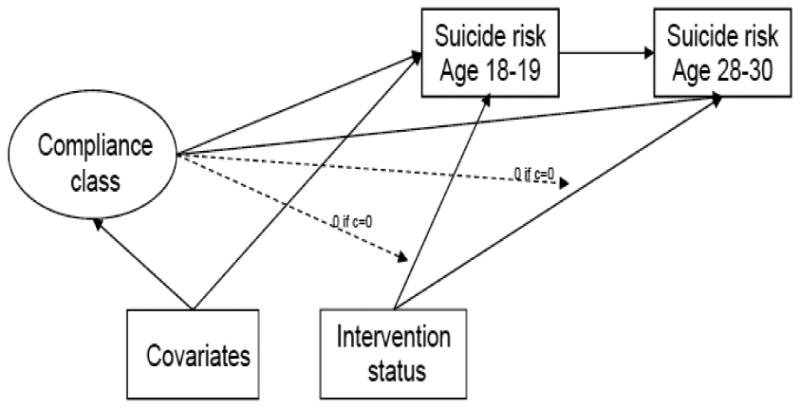
Note: The following covariates were included in the model: youth gender, ethnicity, the presence of biological fathers in the youth's primary residence at baseline, as well as baseline peer deviance, substance use, antisocial behavior, positive family relations, parental monitoring, and teacher reports of youth engagement in risky behavior.
Results
Descriptive statistics and correlations are available upon request. Suicide risk was stable across assessments (r = .35, p < .05), and related to female gender (r = .11 to .08, p < .05), biological father absence from the home (age 28-30; r = .09, p < .05), sixth grade substance use (age 18-19; r = .08, p < .05), parental monitoring (r = -.11 to -.08, p < .05) and positive family relations (age 18-19; r = -.12, p < .05).
CACE Analysis
Typical estimates of model fit are not available for mixture models. However, the quality of classification of the engagement groups within the model is represented by entropy, a summary measure of the probability of membership in the most-likely class for each individual (i.e., in the engager or non-engager class). Possible entropy values range from 0 to 1.0, and values closer to 1.0 represent better classification (Muthén & Muthén, 1998–2012). High entropy was observed in the current analyses (entropy = .97), indicating good class discrimination.
Results for predictors of engagement followed a logistic regression framework, examining the extent to which variables discriminate membership in the engager versus non-engager classes. FCU engagement was predicted by the absence of biological fathers from the home, and teacher reports of youth risk at baseline (see Table 1). Within the engager class, intervention status was significantly related to suicide risk at both ages 18-19 and age 28-30, with youth in the intervention condition reporting significantly lower levels of suicide risk in late adolescence and (controlling for earlier suicide risk) in early adulthood. Within the engager class, greater suicide risk at age 18-19 was also predicted by higher levels of substance use, and at age 18-30 by biological father absence from the home at baseline.
Table 1. CACE model results predicting suicide risk.
| Class membership | Within-class variability | ||||
|---|---|---|---|---|---|
| Engager vs. non-engager | Non-engager Class | Engager Class | |||
| Age 18-19 | Age 28-30 | Age 18-19 | Age 28-30 | ||
| Logit (SE) | Est (SE) | Est (SE) | Est (SE) | Est (SE) | |
|
| |||||
| Intervention status | Fixed at 0 | Fixed at 0 | Fixed at 0 | -.84 (.18) * | -1.95 (.18) * |
| Female Gender | .39 (.21) | .09 (.05) | .01 (.04) | .26 (.17) | .06 (.11) |
| Ethnic minority | -.16 (.21) | .02 (.04) | -.01 (.04) | .01 (.18) | -.02 (.13) |
| Biological dad present (6th grade) | -.56 (.20) * | -.08 (.05) | -.03 (.04) | .16 (.20) | -.36 (.14) * |
| Deviant peers (6th grade) | .14 (.12) | -.01 (.03) | .00 (.02) | -.08 (.07) | .06 (.07) |
| Teacher report of risk (6th grade) | .33 (.12) * | -.07 (.03) * | -.03 (.03) | -.12 (.10) | -.04 (.08) |
| Substance Use (6th grade) | .03 (.03) | .00 (.01) | .00 (.01) | .06 (.03) * | .03 (.04) |
| Antisocial (6th grade) | -.19 (.25) | .03 (.04) | .03 (.06) | -.06 (.22) | -.17 (.20) |
| Positive Family Relations (6th grade) | -.17 (.11) | -.06 (.03) | -.03 (.02) | -.06 (.10) | .06 (.08) |
| Parental Monitoring (6th grade) | .03 (.13) | -.02 (.03) | .03 (.02) | -.20 (.12) | -.10 (.09) |
| Age 18-19 suicide risk | / | / | .17 (.06) * | / | .24 (.09) * |
|
| |||||
| Parameter intercept | -1.49 (.75) * | .64 (.21) * | .12 (.11) | 2.28 (.72) * | 2.68 (.69) * |
| Parameter residual variance | N/A | .43 (.06) * | .25 (.04) * | .43 (.06) * | .25 (.04) * |
p < .05
Discussion
Receipt of the FCU was associated with reductions in suicide risk across adolescence and early adulthood. These results are consistent with prior work documenting FCU effects on depressive symptoms (Connell et al., 2008; in press), with other family-focused prevention and intervention programs for suicidal adolescents (e.g. Pineda & Dadds, 2013), and with other prevention programs targeting youth behavior problems yielding crossover effects on suicide risk (e.g. Kerr et al., 2014, Wilcox et al., 2008). It is worth highlighting that the effects of intervention on suicide risk persisted into early adulthood, controlling for prior intervention effects in late adolescence, suggesting that the effects of the FCU on suicide risk are fairly durable. Of note, broad-based prevention programs may be particularly worth investigating in the context of suicide prevention. Suicide risk is associated with a range of risk factors, including family functioning (e.g., harsh/critical parenting), adolescent mental health (depression, conduct problems and substance use), peer relational problems, and academic difficulties (Hawton, Saunders, & O'Connor, 2012). Broad-based prevention programs may ultimately provide a cost-effective way to address the complex risk-pathways leading to suicidal ideation and behavior.
Several limitations to the current study are worth noting. First, the suicide risk measure, derived from the CIDI, was completed only by respondents endorsing depression screening items, therefore possibly underrepresenting the overall number of participants experiencing suicide risk. Second, the cumulative score we used means that an individual who denied ideation or planning and reported an attempt, may have the same score (=1) as an individual who endorsed ideation only (=1). It is possible that the intervention had a differential impact depending on the type of suicide risk. As a result, future work should include more robust measures of suicide risk. Additionally, the CIDI was only available at later waves of the study. In addition to attrition, we cannot rule out baseline differences in suicide risk across intervention and control groups, although prior work with outcomes assessed at baseline (e.g., conduct problems and depression) suggested intervention and control groups are generally equivalent at baseline.
Despite such limitations, this study extends the literature showing that broad-based family-focused preventive interventions delivered in adolescence can significantly reduce suicide risk across adolescence, and is consistent with the growing body of work suggesting improvements in depression and related outcomes as a function of the FCU intervention (Connell et al, 2008, in press). Future randomized trials of the FCU specifically targeting adolescent depression (and closely-related outcomes such as suicide risk) are needed to enhance these effects and examine potential mechanisms of FCU effects on these important outcomes, including family functioning and co-occurring problem domains (e.g., depression, conduct problems, and substance use).
Acknowledgments
This project was supported by grants DA07031 and DA13773 from the National Institute on Drug Abuse, and AA12702 from the National Institute on Alcohol Abuse and Alcoholism, to Thomas Dishion. The authors gratefully acknowledge the clinical leadership of Dr. Kate Kavanagh on this project, and the contribution of the Project Alliance staff, Portland Public Schools, and the participating youth and families.
Contributor Information
Arin M. Connell, Case Western Reserve University.
Hannah N. McKillop, Case Western Reserve University.
Thomas J. Dishion, Arizona State University, REACH Institute & Oregon Research Institute.
References
- Brent D, McMakin D, Kennard B, Goldstein T, Mayes T, Douaihy A. Protecting adolescents from self-harm: a critical review of intervention studies. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52:1260–1271. doi: 10.1016/j.jaac.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridge J, Goldstein T, Brent D. Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Collins L, Murphy S, Bierman K. A Conceptual Framework for Adaptive Preventive Interventions. Prevention Science. 2004;5:185–196. doi: 10.1023/b:prev.0000037641.26017.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell A, Dishion T. Reducing depression among at-risk early adolescents: three-year effects of a family-centered intervention embedded within schools. Journal of Family Psychology. 2008;22:574. doi: 10.1037/0893-3200.22.3.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell A, Dishion T, Yasui M, Kavanagh K. An ecological approach to family intervention: Linking parent compliance with treatment to long-term prevention of adolescent problem behavior. Journal of Consulting & Clinical Psychology. 2007;75:568–579. doi: 10.1037/0022-006X.75.4.568. [DOI] [PubMed] [Google Scholar]
- Connell A, Stormshak E, Dishion T, Fosco G, Van Ryzin M. (in press). The Family Check-Up and adolescent depression: An examination of treatment responders and non-responders. Prevention Science. doi: 10.1007/s11121-015-0586-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion T, Stormshak E, Kavanagh K. Everyday parenting: A professional's guide to building family management skills. Champaign, IL: Research Press; 2011. [Google Scholar]
- Hawton K, Saunders K, O'Connor R. Self-harm and suicide in adolescents. The Lancet. 2012;379:2373–2382. doi: 10.1016/S0140-6736(12)60322-5. [DOI] [PubMed] [Google Scholar]
- Jo B. Estimation of intervention effects with noncompliance: Alternative model specifications. Journal of Educational and Behavioral Statistics. 2002;27:385–409. [Google Scholar]
- Little R. A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association. 1988;83:1198–1202. [Google Scholar]
- Metzler C, Biglan A, Rusby J, Sprague J. Evaluation of a comprehensive behavior management program to improve school-wide positive behavior support. Education & Treatment of Children. 2001;24:448–479. [Google Scholar]
- Miller W, Rollnick S. Motivational interviewing: Preparing people for change. New York: Guilford press; 2002. [Google Scholar]
- Muthén L, Muthén B. MPlus users' guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998-2012. [Google Scholar]
- Pineda J, Dadds M. Family intervention for adolescents with suicidal behavior: a randomized controlled trial and mediation analysis. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52:851–862. doi: 10.1016/j.jaac.2013.05.015. [DOI] [PubMed] [Google Scholar]
- Van Ryzin M, Dishion T. The impact of a family-centered intervention on the ecology of adolescent antisocial behavior: Modeling developmental sequelae and trajectories during adolescence. Development and Psychopathology. 2012;24:1139–1155. doi: 10.1017/S0954579412000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox H, Kellam S, Brown C, Poduska J, Ialongo N, Wang W, Anthony J. The impact of two universal randomized first-and second-grade classroom interventions on young adult suicide ideation and attempts. Drug and Alcohol Dependence. 2008;95:S60–S73. doi: 10.1016/j.drugalcdep.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Composite International Diagnostic Interview — Version 2.1. World Health Organization; Geneva: World Health Organization; 1997. [Google Scholar]


