Abstract
Background
The Stroke Impact Scale (SIS) is a stroke‐specific, quality of life measure recommended for research and clinical practice. Completion rates are suboptimal and could relate to test burden. We derived and validated a short form SIS (SF‐SIS).
Methods and Results
We examined data from the Virtual International Stroke Trial Archive, generating derivation and validation populations. We derived an SF‐SIS by selecting 1 item per domain of SIS, choosing items most highly correlated with total domain score. Our validation described agreement of SF‐SIS with original SIS and the SIS‐16 and correlation with Barthel Index, modified Rankin Scale, National Institutes of Health Stroke Scale, and Euro‐QoL 5 dimensions visual analog scales. We assessed discriminative validity (associations between SF‐SIS and factors known to influence outcome [age, physiological parameters, and comorbidity]). We assessed face validity and acceptability by sharing the SF‐SIS with a focus group of stroke survivors and multidisciplinary stroke healthcare staff. From 5549 acute study patients (mean age 68.5 [SD 13] years, mean SIS 64 [SD 32]) and 332 rehabilitation patients (mean age 65.7 [SD 11] years, mean SIS 61 [SD 11]), we derived an 8‐item SF‐SIS that demonstrated good agreement with original SIS and good correlation with our chosen functional and quality of life measures (all ρ>0.70, P<0.0001). Significant associations were seen with our chosen predictors of stroke outcome in the acute group (P<0.0001). The focus group agreed with the choice of items for SF‐SIS across 7 of 8 domains.
Conclusions
Using multiple, complementary methods, we have derived an SF‐SIS and demonstrated content, convergent, and discriminant validity. This shortened SIS should allow collection of robust quality of life data with less associated test burden.
Keywords: Patient‐reported outcome measures, quality of life, stroke, Stroke Impact Scale, stroke scales
Introduction
Many outcome assessments are available to measure stroke recovery, often with compromise between test burden and richness of data captured.1 Traditionally clinicians and researchers have favored impairment or activity assessments.2 From the stroke survivor perspective, these scales may be overly reductionist.3 Patient‐reported outcome measures (PROMs) are self‐report questionnaires designed to capture the impact of ill health on a broad range of areas that influence quality of life (QOL). PROMs have been found to provide unique insights into the clinical status of stroke survivors.4 There is no single PROM that has become universally accepted in stroke. In a recent structured review of PROMs for use in stroke, the Stroke Impact Scale (SIS)5 was selected as having a well‐documented and thorough development history, together with good psychometric properties.6
This SIS is a stroke‐specific, health‐related QOL measure (HR‐QOL). SIS assesses 60 items across 8 domains. The multidomain testing inherent in SIS results in a tool that can take considerable time to complete. This may limit the scale's use in practice, particularly in time‐pressured environments or for stroke survivors with persisting physical and cognitive impairments. In a multidisciplinary, expert consensus statement, time required for SIS assessment was noted as a major limitation for stroke survivors.6 A proxy SIS form has been described; however, proxy responses may not correlate with patient QOL perceptions.7 The ideal would be a brief assessment that maintains the psychometrics strengths of SIS.
Internal consistency of SIS is high, suggesting a degree of redundancy in scale items.8 This finding would support removing some items to create a shorter form. A modified version of SIS, limited to physical domains, has been described (SIS‐16),9 but there is no accepted short form of the complete SIS. Using data from 73 stroke survivors, it was shown that an 8‐item short form is possible with favorable properties.10 These pilot data are encouraging but require robust, independent assessment and validation. In particular, it is important that validation work is carried out using populations independent of the derivation cohort and that there is opportunity for key stakeholders, both medical and lay persons, to comment on the short form scale.
We used the patient‐level data held in the Virtual International Stroke Trials Archive (VISTA) to derive and validate a short form of the SIS (SF‐SIS).
Methods
We used the VISTA resource for our derivation and validation. VISTA is a not‐for‐profit repository for stroke trial data, containing study‐quality data on thousands of participants.11 All studies contained within VISTA and associated work have been approved by an institutional review committee and included participants, or their proxies, provided informed consent. The VISTA data sets have been used to investigate various novel hypotheses including analyses of stroke assessment scale properties.12
Data Set
VISTA data sets predominantly used version 3.0 of the SIS scale with domains of strength (4 items), hand function (5 items), mobility (9 items), activities of daily living (ADLs) (10 items), memory (7 items), communication (7 items), emotion (9 items), and societal participation (8 items). Some acute data sets used the modified SF‐16; this version of the scale had fewer items for domains of strength (0 items), hand function (1 item), mobility (8 items), and ADLs (7 items). Domains are scored on a metric of 0 to 100, with higher scores indicating better self‐reported health. Some of the available SIS data sets also contained a visual analog scale (VAS) describing global QOL. Where certain domain items of SF‐SIS were unavailable, as original data had used SIS‐16, we substituted with the best‐fit available item (hand function: “carry heavy objects”) or did not include that item in analysis (strength domain).
We selected all patient‐level, anonymized data that contained SIS along with any other outcome measures of interest. Our chosen comparator outcomes were other PROMs (EuroQOL EQ‐5D, EQ‐5D‐VAS, and SIS‐VAS) or functional outcome measures (Barthel Index [BI], modified Rankin Scale [mRS], and National Institutes of Health Stroke Scale [NIHSS]). A priori, we decided to treat data from acute stroke trials and from rehabilitation studies separately. We divided the data set using a randomized 60:40 split to create cohorts for independent derivation and validation analyses.
Descriptive Analyses
We described clinical and demographic features of the main data set. We described the distribution of scores on SIS globally and for each domain. We assessed internal consistency, using Cronbach's α, for the complete SIS and for each domain. Where data were collected at >1 time‐point, we used the time‐point that gave the largest data set. For acute studies, “baseline” assessments were generally within first 24 hours; for rehabilitation studies, “baseline” assessments were predominantly at 4 weeks post ictus.
Derivation Analyses
We described correlation, by using Spearman's ρ, for each domain item relative to the domain total score and selected the single item per domain with the greatest correlation. All analyses were performed in the acute and rehabilitation data sets and compared. We compared the resulting, 8‐item VISTA‐derived short form (ie, SF‐SIS) with the short form from our previous pilot work (herein referred to as SF‐SIS [pilot]).
Validation Analyses
We assessed convergent validity by describing the agreement of SF‐SIS with the original SIS or SIS‐16 and by describing correlation of SF‐SIS with other functional (BI, mRS, and NIHSS) and QOL (EQ‐5D, EQ‐VAS, and SIS‐VAS) outcomes where available. EQ‐5D data were transformed into a single index using the Europe‐VAS data set.13 As a check of discriminant validity, we performed linear univariate regressions to assess association of SF‐SIS with, where data were available, clinical and demographic features known to influence outcome (age, baseline stroke severity, physiologic variables, cardiac disease, prior stroke, and use of thrombolytic therapy) and described odds of a point change in SF‐SIS associated with unit change in other outcomes. All analyses were performed in the acute and rehabilitation data sets and compared. All analyses were performed with the use of SAS version 9.3 (SAS Institute) software.
Focus Group
We conducted a focus group to assess the opinions of key stakeholders on the original and short forms of SIS and other QOL scales. We invited multidisciplinary staff involved in stroke care, focusing on those who regularly use PROMS in clinical practice. We also invited stroke survivors and their carers, asking for volunteers through a Stroke Research Network managed database. We presented the full SIS, SIS‐16, SF‐SIS, as well as EQ‐5D and the Short Form‐36 (SF‐12). Participants were asked to compare and comment on the various scales in terms of content, perceived ease of completion, and relevance to stroke. Participants were then asked to rate items from each domain of the full SIS and to comment on preferred items. The group was led by one of the authors (M.P.), and all participants were encouraged to contribute. Responses were transcribed in real time and reviewed by a researcher independent of the main study group who described and collated common themes in participant responses (PM, see Acknowledgments).
The final decision on content of the SF‐SIS was based on results from the pilot data10; the derivation and validation analyses presented here and the opinions of the focus group. We selected those items that were favored in ≥2 of these 3 data sources (Figure).
Figure 1.
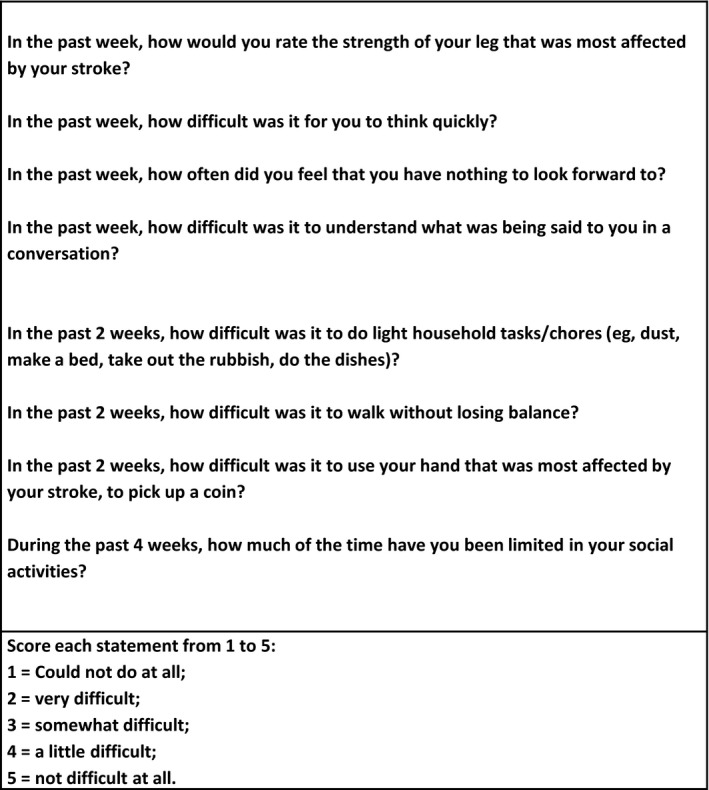
Short‐form Stroke Impact Scale.
Results
The VISTA database had SIS data on 5549 acute trial participants and 332 rehabilitation study participants. The rehabilitation data set had data at various time‐points (baseline, 1 month, 3 month, 1 year). We used the baseline data set for analyses because this was the largest data set. The included patients consisted of 2445 (44%) female patients in the acute data set (mean age 68.5 [SD 13] years) and 107 (32%) female patients in the rehabilitation data set (65.7 [SD 11.0] years; Tables 1 and 2).
Table 1.
Clinical and Demographic Features of the VISTA Data Set—Acute Stroke Trial Data Set
| Age, y | 68.5 (13) |
| Baseline NIHSS, median (IQR) | 12 (9) |
| Systolic blood pressure, mm Hg | 156.5 (27) |
| Glucose at baseline, mmol/L | 7.6 (3.06) |
| Female | 2445 (44%) |
| Use of thrombolysis | 1915 (35%) |
| Intracerebral hemorrhage | 603 (11%) |
| Diabetes mellitus | 1247 (23%) |
| Hypertension | 4157 (75%) |
| Atrial fibrillation | 1325 (24%) |
| Previous stroke | 1046 (19%) |
| Transient ischemic attack | 439 (8%) |
| Ischemic heart disease | 1710 (31%) |
| Myocardial infarction | 661 (12%) |
| Congestive heart failure | 485 (9%) |
Data are given as n (%) for nominal data and as mean (SD) for other data unless otherwise stated. NIHSS indicates National Institutes of Health Stroke Scale; VISTA, Virtual International Stroke Trials Archive.
Table 2.
Clinical and Demographic Features of the VISTA Data Set—Rehabilitation Study Data Set
| Variable | All Stroke Types |
|---|---|
| Age, y, mean (SD) | 65.73 (10) |
| Baseline BI, median (IQR) | 15 (7) |
| Female | 107 (32%) |
| LACS | 59 (18%) |
| PACS | 118 (36%) |
| TACS | 143 (43%) |
| Atrial fibrillation | 45 (13%) |
| Hypertension | 243 (73%) |
| Diabetes mellitus | 44 (13%) |
| Ischemic heart disease | 67 (20%) |
| Heart failure | 8 (2%) |
| Previous stroke | 57 (17%) |
| Intracerebral hemorrhage | 46 (14%) |
Data are given as n (%) for nominal data and as mean (SD) for other data unless otherwise stated. BI indicates Barthel Index; LACS, lacunar stroke; NIHSS, National Institutes of Health Stroke Scale; PACS, partial anterior circulation stroke; TACS, total anterior circulation stoke; VISTA, Virtual International Stroke Trials Archive.
There was a spread of SIS scores across both data sets: for acute data, mean SIS 64.5 (SD 32.4), and for rehabilitation data, mean SIS 61.2 (SD 11.0). Internal consistency for complete SIS was high, with α=0.98 (acute) and α=0.93 (rehabilitation). Across both data sets, for individual domains the internal consistency was generally high (>0.85) for all domains other than “emotion” with α=0.60 (acute) and strength α=0.77 and emotion α=0.63 (rehabilitation).
In both data sets, we described individual items that correlated best with the corresponding domain. The best‐performing rehabilitation items agreed with the acute data for all domains that had a full data set and agreed with the original SF‐SIS (pilot) for 5 of 8 items (Table 3).
Table 3.
Correlation (Spearman's ρ) of Individual Items With Total Domain Score Across Various Stroke Impact Scale Data Sets
| Domain/Item Within Domain | Acute | Rehabilitation | SF Pilot | Focus Group |
|---|---|---|---|---|
| 1. Strength dimension | ||||
| a) Strength of arm | NA | 0.708 | ||
| b) Grip of hand | NA | 0.704 | ||
| c) Strength of leg* | NA | 0.809 | Y | Y |
| d) Strength of foot | NA | 0.791 | ||
| 2. Memory dimension | ||||
| a) Remember things that people just told you | 0.880 | 0.794 | ||
| b) Remember things that happened the day before | 0.906 | 0.790 | ||
| c) Remember to do things | 0.906 | 0.767 | ||
| d) Remember the day of the week | 0.880 | 0.685 | ||
| e) Concentrate | 0.907 | 0.851 | N | |
| f) Think quickly* | 0.916 | 0.866 | Y | |
| g) Solve everyday problems | 0.901 | 0.819 | ||
| 3. Emotion dimension | ||||
| a) Feel sad | 0.681 | 0.673 | ||
| b) Feel that there is nobody you are close to | 0.640 | 0.520 | ||
| c) Feel that you are a burden to others | 0.704 | 0.674 | ||
| d) Feel that you have nothing to look forward to* | 0.747 | 0.722 | Y | Y |
| e) Blame yourself for mistakes that you made | 0.608 | 0.603 | ||
| f) Enjoy things as much as ever | −0.539 | −0.438 | ||
| g) Feel quite nervous | 0.573 | 0.535 | ||
| h) Feel that life is worth living | −0.609 | −0.657 | ||
| i) Smile and laugh at least once a day | −0.613 | −0.581 | ||
| 4. Communication dimension | ||||
| a) Say the name of someone | 0.864 | 0.770 | ||
| b) Understand what was being said | 0.804 | 0.627 | N | |
| c) Reply to questions | 0.914 | 0.816 | ||
| d) Correctly name objects | 0.894 | 0.736 | ||
| e) Participate in a conversation* | 0.921 | 0.854 | Y | |
| f) Have a conversation on phone | 0.921 | 0.881 | ||
| g) Call another person on the phone | 0.856 | 0.798 | ||
| 5. ADL dimension | ||||
| a) Cut your food with a knife and fork? | NA | 0.475 | ||
| b) Dress top half of your body? | 0.877 | 0.705 | ||
| c) Bathe yourself? | 0.896 | 0.755 | ||
| d) Clip your toenails? | NA | 0.549 | ||
| e) Get to the toilet on time? | 0.905 | 0.699 | N | |
| f) Control your bladder? | 0.741 | 0.545 | ||
| g) Control your bowels? | 0.702 | 0.398 | ||
| h) Do light household tasks?* | NA | 0.793 | N | Y |
| i) Go shopping? | 0.871 | 0.705 | ||
| j) Do heavy household chores? | 0.839 | 0.676 | ||
| 6. Mobility dimension | ||||
| a) Sit without losing your balance? | 0.690 | 0.485 | ||
| b) Stand without losing your balance* | 0.892 | 0.823 | ||
| c) Walk without losing your balance | 0.922 | 0.851 | Y | |
| d) Move from bed to chair? | 0.895 | 0.817 | ||
| e) Walk down one street? | 0.913 | 0.862 | ||
| f) Walk fast? | 0.888 | 0.662 | N | |
| g) Climb one flight of stairs? | 0.910 | 0.846 | ||
| h) Climb several flights of stairs | 0.741 | |||
| i) Get in and out of a car? | 0.915 | 0.783 | ||
| 7. Hand function dimension | NA | |||
| a) Carry heavy objects? | 0.815 | 0.708 | ||
| b) Turn a door knob | NA | 0.836 | ||
| c) Open a can or a jar? | NA | 0.781 | ||
| d) Tie a shoelace? | NA | 0.658 | ||
| e) Pick up a coin?* | NA | 0.841 | Y | Y |
| 8. Social participation dimension | ||||
| a) Your work | 0.834 | 0.735 | ||
| b) Your social activities* | 0.900 | 0.766 | Y | Y |
| c) Quiet recreation | 0.839 | 0.704 | ||
| d) Active recreation | 0.856 | 0.722 | ||
| e) Your role as a family member/friend | 0.828 | 0.541 | ||
| f) Your participation in spiritual activities | 0.810 | 0.692 | ||
| g) Your ability to control your life | 0.891 | 0.783 | ||
| h) Your ability to help others | 0.894 | 0.782 | ||
Data are correlation of individual items scores with total domain score. In the acute data set, certain items were not available (NA). Data are presented for our acute trial and rehabilitation study data sets. We compare best‐performing items (highlighted with *) with those reported in our initial short‐form pilot work (SF pilot) and our focus group, labeling “Y” where there was agreement with our derived SF‐SIS and “N” where preferred items differ. Final choice of questions for the SF‐SIS was based on those items those that were favored in ≥2 of the 3 data sets: pilot work, main analysis, and focus group.
We validated our SF‐SIS in our acute data set. Agreement of SF‐SIS with SIS‐16 was excellent, α=0.92. SF‐SIS showed strong correlations with all our chosen outcome measures: mRS (−0.83), BI (0.82), NIHSS (−0.77), EQ‐5D (0.82), and EQ‐VAS (0.72); correlations were equivalent to those seen for full SIS (−0.87, 0.89, −0.77, 0.88, and 0.73, respectively) (Table 4). On linear univariate analyses, age, stroke severity (NIHSS), baseline blood pressure (systolic), baseline glucose, previous stroke, cardiac disease (atrial fibrillation), and use of thrombolysis were all associated (P<0.0001) with SF‐SIS (Table 5).
Table 4.
Correlation (Spearman's ρ) of SIS and Short‐Form SIS With Other Quality of Life and Functional Outcome Measures
| SIS | SF‐SIS | |
|---|---|---|
| Acute trial data | ||
| SIS | 1.00 | |
| SF‐SIS | 0.94 | 1.00 |
| mRS | −0.87 | −0.80 |
| BI | 0.89 | 0.80 |
| NIHSS | −0.77 | −0.73 |
| EQ‐5D | 0.88 | 0.82 |
| EQ‐5D VAS | 0.73 | 0.72 |
| Rehabilitation study data | ||
| SIS | 1.00 | |
| SF‐SIS | 0.96 | 1.00 |
| SIS‐VAS | 0.56 | 0.57 |
| BI | 0.72 | 0.65 |
| EQ‐5D | 0.69 | 0.69 |
| EQ‐5D VAS | 0.46 | 0.40 |
BI indicates Barthel Index; EQ‐5D, EuroQOl; mRS, modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale; SIS, Stroke Impact Scale; SF‐SIS, Short‐Form SIS; VAS, visual analog scale. All P<0.001.
Table 5.
Associations of SF‐SIS With Clinical and Demographic Outcome Predictors—Acute Trial Data Set
| Variable | Coefficient (95% CI) | ||
|---|---|---|---|
| SIS‐16 | SF‐SIS | SF‐SIS (Pilot) | |
| Age | −0.777 (−0.851 to −0.702) | −0.454 (−0.523 to −0.386) | −0.456 (−0.521 to −0.392) |
| Baseline NIHSS | −2.619 (−2.79 to −2.45) | −1.924 (−2.082 to −1.766) | −1.655 (−1.807 to −1.504) |
| SBP | −0.105 (−0.14 to −0.069) | −0.056 (−0.090 to −0.023) | −0.052 (−0.083 to −0.021) |
| Glucose | −1.223 (−1.56 to 0.88) | −0.619 (−0.930 to −0.308) | −0.596 (−0.890 to −0.301) |
| Sex (female=1) | −8.85 (−10.78 to −6.92) | −5.398 (−7.149 to −3.647) | −5.346 (−6.992 to −3.698) |
| Use of tPA (yes=1) | 4.287 (2.26 to 6.32) | 2.163 (0.333 to 3.993) | 2.140 (0.418 to 3.862) |
| AF (yes=1) | −11.17 (−13.5 to −8.84) | −6.814 (−8.922 to −4.706) | −6.663 (−8.647 to −4.678) |
| Prior stroke (yes=1) | −4.16 (−6.65 to −1.67) | −4.427 (−6.628 to −2.225) | −4.952 (−7.022 to −2.883) |
AF indicates atrial fibrillation; NIHSS, National Institutes of Health Stroke Scale; SBP, systolic blood pressure; SF‐SIS (pilot), short form of Stroke Impact Scale derived in initial pilot work; SF‐SIS, short form of Stroke Impact Scale derived from VISTA resource; tPA, tissue plasminogen activator (thrombolysis).
Using the rehabilitation data set, agreement of SF‐SIS with SIS was excellent, α=0.96. SF‐SIS showed significant (P<0.0001) correlation with BI (ρ=0.65), EQ‐5D (ρ=0.69), EQ‐VAS (ρ=0.45), and SIS‐VAS (ρ=0.57). Correlations were roughly equivalent to those seen for full SIS (0.72, 0.69, 0.46, and 0.58, respectively) (Table 4). SF‐SIS was significantly (P<0.0001) associated with certain predictors of stroke severity, age, and baseline stroke severity (BI) but not with previous stroke or cardiac disease (heart failure) (Table 6).
Table 6.
Associations of SF‐SIS With Clinical and Demographic Outcome Predictors—Rehabilitation Study Data Set
| Variable | Coefficient (95% CI) | ||
|---|---|---|---|
| SIS Full | SF‐SIS | SF‐SIS (Pilot) | |
| Age | −0.313 (−0.449 to −0.178) | −0.315 (−0.469 to −0.161) | −0.367 (−0.527 to −0.206) |
| Sex | 0.732 (−2.541 to 4.005) | 0.3646 (−3.325 to 4.054) | 1.094 (−2.769 to 4.958) |
| Baseline BI | 1.583 (1.303 to 1.863) | 1.677 (1.352 to 2.003) | 1.800 (1.462 to 2.137) |
| TIA | −4.476 (−8.31 to −0.637) | −5.561 (−9.851 to −1.271) | −6.412 (−10.927 to −1.897) |
| Previous Stroke | −3.687 (−7.847 to 0.472) | −3.502 (−8.199 to 1.195) | −5.813 (−10.696 to −0.930) |
| Heart failure | −10.891 (−20.17 to −1.61) | −9.988 (−20.44 to 0.47) | −10.52 (−21.55 to 0.51) |
| IHD | −1.064 (−4.731 to 2.604) | −2.009 (−6.125 to 2.108) | −2.419 (−6.755 to 1.917) |
| AF | −4.028 (−8.521 to 0.464) | −4.985 (−10.007 to 0.037) | −3.669 (−8.972 to 1.633) |
AF indicates atrial fibrillation; BI, Barthel Index; IHD, ischemic heart disease; SF‐SIS (pilot), short form of Stroke Impact Scale derived in initial pilot work; SF‐SIS, short form of Stroke Impact Scale derived from VISTA resource; SIS full, complete Stroke Impact Scale; TIA, transient ischaemic attack.
Focus Group
Thirteen people attended the focus group: 3 research nurses, 2o ward nurses (acute and rehabilitation settings), 1 occupational therapist, 1 physiotherapist, 1e stroke physician, 1 clinical psychologist, 3 stroke survivors, and 1 caregiver. On analysis of free‐form responses, themes were that wording of certain SIS items was confusing in places; that the original SIS was too long, albeit provided more detail than the short scales; and that certain important aspects of recovery were not adequately captured. On direct questioning, the group preferred the SF‐SIS to the other scales presented but had concerns that in shortening the scale, some important details would be lost (Data S1). Preferred domain items from SIS were those included in SF‐SIS for 7 of the 8 domains (Table 3). For the 2 domains (communication and activities of daily living) where SF‐SIS did not agree with the original SF‐SIS (pilot), the focus group preferred the SF‐SIS wording.
Discussion
We have suggested a shortened form of the SIS and validated the measure by using a multimodal approach. The resulting SF‐SIS is robust and broadly acceptable to stroke survivors and clinical/research staff. We believe our SF‐SIS could have use as an outcome measure in stroke research, as quality metric in audit (using a short QOL measure to benchmark and compare services) and as a tool for assessing patient recovery in clinical practice.
Capturing stroke specific QOL data by using PROMs can be challenging. The SIS has been suggested as the optimal PROM for this purpose as it has been shown to be reliable, valid, and sensitive to change.14 However, there are examples of clinical studies where SIS was used as an end‐point measure and, as a result of perceived burden, questionnaire return rates were so poor as to invalidate the study.15 In the pilot that informed earlier work on short forms of SIS, >40% of the questionnaire returns had missing items.10 The problem of lengthy completion time limiting the use of an otherwise good stroke outcome measure is not unique to SIS. Even relatively short assessments such as BI have shown poor completion because of perceived test burden.16 Because there is evidence of redundancy in the full SIS, a short form approach is attractive. Where short forms of lengthy questionnaires are available, they can often replace the original as the test of choice; for example, the short form (16 items) of the Informant Questionnaire for Cognitive Decline in the Elderly is now the preferred version,17 and the recently described short form of the Parkinson's Disease Questionnaire18 is now commonly used.19 Short forms may have particular use in situations where time available for testing is limited or when used as a component of an outcomes battery in a large clinical trial. A measure of success of a short form is that it takes less time to complete than the original instrument. Reviews of SIS describe time to complete as 20 minutes20 although administration may be longer still in stroke survivors with more complex impairments. Within the development group, we tested SF‐SIS and found time to complete of <1 minute. Further work, testing our SF‐SIS in an unselected, “real‐world” population of stroke survivors, is now needed.
There is no perfect assessment scale for stroke survivors. The choice of instrument will depend on the properties of that scale and purpose of testing. A primary limitation of SIS concerns feasibility and acceptability. Other commonly used scales in stroke are limited by imperfect reliability (mRS), floor and ceiling effects (BI), and poor validity for certain stroke syndromes (NIHSS).21, 22, 23 The context of testing is also important. We tested SIS by using data from “acute” and “rehabilitation” settings and found reasonable validity for both. Our short form may have use early in stroke recovery at a time when detailed testing may not be feasible. Future work should examine all psychometric properties of SF‐SIS across various settings where PROMs may be used.
The work presented is an extension of our original description of an SF‐SIS using UK primary care data. The SF‐SIS derived from the VISTA data agreed with the original short form for most domains, suggesting reasonable validity of these items. Where there was disagreement between SF‐SIS items selected for inclusion here and previous work, we chose to use the items preferred by our focus group. Thus, the SF‐SIS described here may be preferable as it has been tested in a larger sample, has robust properties, and has been reviewed by stakeholders.
The use of the VISTA data set allowed access to patient‐level data on thousands of trial participants. This size of data set is considerably larger than that for most previous work concerning derivation and validation of novel stroke outcomes.10, 24 As well as deriving the SF‐SIS, VISTA data allowed us to explore properties of the original SIS with an unprecedented precision. We note the high internal consistency of SIS, suggesting that certain items in SIS may be noncontributory and supporting our work to create a condensed scale. We note also that the emotional domain of SIS is problematic, a feature worthy of further exploration. Previous work on modifying existing assessment tools have tended to restrict analyses to a single data set.25 We created independent data sets for derivation and validation.
There are potential limitations of using VISTA. The data were all from clinical studies and patients were younger and had less severe stroke than unselected populations. While this potentially limits external validity, we are reassured that our SF‐SIS broadly agreed with previous work on SIS using a more representative cohort.10 There was differential availability of clinical and outcome data across the studies included in VISTA. Based on initial scoping, we formulated an analysis plan that made best use of the data; we did not pool acute and rehabilitation data sets as available data differed and intuitively these populations may give differing scores on SIS. The rehabilitation data set had fewer participants than the acute data set. The smaller data set may limit power and external validity, although our sample size is still much larger than that of most psychometric studies of stroke scales.10, 24
The use of a modified version of SIS (the SIS‐16) in certain acute studies limited the SIS data available and we had to modify our analyses accordingly. Again, we are reassured that this limitation has not systemically biased our results as there was broad agreement with those data sets that had full SIS. The focus group contained various clinical disciplines: stroke survivors and their caregivers. For a more robust assessment of acceptability, the tool should be assessed with more stroke survivors and caregivers in the settings for which it is designed. We would encourage further work of this nature. In moving to a shorter version of an assessment scale, there is a tradeoff between richness of data captured and the time and effort required for completion. In our SF‐SIS, certain items are not explicitly measured. To ensure breadth of assessment, we have kept 1 question from each functional domain. Loss of certain items was an issue raised in our focus group, although the group agreed on the final set of items as an acceptable compromise.
We believe our SF‐SIS has robust properties is acceptable to patients and provides an alternative to original SIS. The final step of validation of any assessment scale concerns implementation. If the scale is adopted, we hope to collect prospective data on feasibility, acceptability, and test properties. We would welcome feedback from those using the scale.
Sources of Funding
This work was supported by a research grant from Chest Heart and Stroke Scotland. Dr Quinn is supported by a Joint Stroke Association/Chief Scientist Office Senior Clinical Lectureship. Dr Peters is a senior research scientist of the Department of Health–funded Policy Research Unit on Quality and Outcomes of Person‐Centred Care (QORU), a collaboration between the London School of Economics and Political Science, the University of Kent, and the University of Oxford.
Disclosures
VISTA and VICCTA are not‐for‐profit collaborations of researchers from academia and commercial organizations. The VISTA and VICCTA Steering Committee members have each contributed to the organization of contributing trials, and where these have involved industry support, they have acknowledged that within the original publications.
Supporting information
Data S1. Comments generated in the focus group.
Appendix S1. Steering Group members of the Virtual International Stroke Trials Archive (VISTA).
Acknowledgments
We thank all those who contributed to our focus group, and we are grateful to the Scottish Stroke Research Network for assistance in contacting volunteers for our stroke group. We thank Peter Moffit for transcribing and collating the discussions from our focus groups. We thank NHS Greater Glasgow and Clyde Patient and Carer Forum for organizing stroke survivor input to the focus group.
(J Am Heart Assoc. 2016;5:e003108 doi: 10.1161/JAHA.115.003108)
References
- 1. Lees KR, Bath PM, Schellinger PD, Kerr DM, Fulton R, Hacke W, Matchar D, Sehra R, Toni D; for the European Stroke Organisation Outcomes Working Group . Contemporary outcome measures in acute stroke research: choice of primary outcome measure. Stroke. 2012;43:1163–1170. [DOI] [PubMed] [Google Scholar]
- 2. Quinn TJ, Dawson J, Walters MR, Lees KR. Functional outcome measures in contemporary stroke trials. Int J Stroke. 2009;3:200–205. [DOI] [PubMed] [Google Scholar]
- 3. Quinn TJ, McArthur KS, Ellis G, Stott DJ. Functional assessment in older people. BMJ. 2011;343:d4681. [DOI] [PubMed] [Google Scholar]
- 4. Stewart JC, Cramer SC. Patient‐reported measures provide unique insights into motor function after stroke. Stroke. 2013;4:1111–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Duncan PW, Bode RK, Min Lai S, Perera S. Rasch analysis of a new stroke specific outcome scale: the Stroke Impact Scale. Arch Phys Med Rehabil. 2003;84:950–963. [DOI] [PubMed] [Google Scholar]
- 6. Jenkinson C, Gibbons E, Fitzpatrick R. A Structured Review of Patient‐Reported Outcome Measures (PROMs) for Stroke (Report to Department of Health). Oxford: University of Oxford; 2009. [Google Scholar]
- 7. Duncan PW, Lai SM, Tyler DA, Perera S, Reker DM, Studenski S. Evaluation of proxy responses to the Stroke Impact Scale. Stroke. 2002;33:2593–2599. [DOI] [PubMed] [Google Scholar]
- 8. Edwards B, O'Connell B. Internal consistency and validity of the Stroke Impact Scale 2.0 (SIS 2.0) and SIS‐16 in an Australian sample. Qual Life Res. 2003;12:1127–1135. [DOI] [PubMed] [Google Scholar]
- 9. Duncan PW, Lai SM, Bode RK, Perea S, DeRosa JT; GAIN Americas Investigators . Stroke Impact Scale‐16: a brief assessment of physical function. Neurology. 2003;60:291–296. [DOI] [PubMed] [Google Scholar]
- 10. Jenkinson C, Fitzpatrick R, Crocker H, Peters M. The Stroke Impact Scale, validation in a UK setting and development of a SIS Short Form and SIS Index. Stroke. 2013;44:2532–2535. [DOI] [PubMed] [Google Scholar]
- 11. Ali M, Bath PMW, Brady M, Davis S, Diener HC, Donnan G, Fisher M, Hacke W, Hanley DF, Luby M, Tsivgoulis G, Wahlgren N, Warach S, Lees KR; for the VISTA Steering Committees . Development, expansion and use of a stroke clinical trials resource. Int J Stroke. 2012;7:133–138. [DOI] [PubMed] [Google Scholar]
- 12. Ali M, Fulton R, Quinn TJ, Brady M; on behalf of VISTA . How well do standard stroke outcome measures reflect quality of life. Stroke. 2013;44:3161–3165. [DOI] [PubMed] [Google Scholar]
- 13. EURO‐QOL . Available at: www.euroqol.org/about-eq-5d/valuation-of-eq-5d/eq-5d-3l-value-sets.html. Accessed April 26, 2016.
- 14. Duncan PW, Wallace D, Lai SM, Johnson D, Embretson S, Laster LJ. The stroke impact scale version 2.0. Evaluation of reliability, validity, and sensitivity to change. Stroke. 1999;30:2131–2140. [DOI] [PubMed] [Google Scholar]
- 15. Murray J, Forster A, Young J. Response and completion rates for postal outcomes booklets in stroke rehabilitation. Int J Ther Rehabil. 2007;14:440–445. [Google Scholar]
- 16. McAvoy E. The use of ADL indices by occupational therapists. Br J Occup Ther. 1991;54:383–385. [Google Scholar]
- 17. Harrison JK, Fearon P, Noel‐Storr AH, McShane R, Stott DJ, Quinn TJ. IQCODE for the diagnosis of dementia within a secondary care setting. Cochrane Database Syst Rev. 2015;3:CD010772. [DOI] [PubMed] [Google Scholar]
- 18. Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N. The PDQ‐8: development and validation of a short‐form Parkinson's disease questionnaire. Psychol Health. 1997;12:805–814. [Google Scholar]
- 19. Jenkinson C, Fitzpatrick R, Peto V, Morley D, Dummett S, Saunders P. The PDQ Questionnaires User Manual. Oxford: Health Services Research Unit; 2012. [Google Scholar]
- 20. Rehab measures: Stroke Impact Scale. Available at: rehabmeasures.org/Lists/RehabMeasures/DispForm.aspx?ID=934RehabilitationMeasuresdatabase. Accessed April 26, 2016.
- 21. Quinn TJ, Dawson J, Walters MR, Lees KR. Reliability of the modified Rankin Scale systematic review. Stroke. 2009;40:3393–3395. [DOI] [PubMed] [Google Scholar]
- 22. Duffy L, Gajree S, Langhorne P, Stott DJ, Quinn TJ. Reliability (inter‐rater agreement) of the Barthel Index for assessment of stroke survivors: systematic review and meta‐analysis. Stroke. 2013;44:462–468. [DOI] [PubMed] [Google Scholar]
- 23. Harrison JK, McArthur KS, Quinn TJ. Assessment scales in stroke, clinimetric and clinical considerations. Clin Interv Aging. 2013;8:201–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Quinn TJ, Langhorne P, Stott DJ. Barthel Index for stroke trials: development, properties, and application. Stroke. 2011;42:1146–1151. [DOI] [PubMed] [Google Scholar]
- 25. Goetz C, Coste J, Lematayer F, Rat AC, Montel S, Recchia S, Debouverie M, Pouchot J, Spitz E, Guillemin F. Item reduction based on rigorous methodological guidelines is necessary to maintain validity when shortening composite measurement scales. J Clin Epidemiol. 2013;66:710–718. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Comments generated in the focus group.
Appendix S1. Steering Group members of the Virtual International Stroke Trials Archive (VISTA).


