Abstract
Management of obesity in the context of the primary care physician visit is of limited efficacy in part because of limited ability to engage participants in sustained behavior change between physician visits. Therefore, healthcare systems must find methods to address obesity that reach beyond the walls of clinics and hospitals and address the issues of lifestyle modification in a cost-conscious way. The dramatic increase in technology and online social networks may present healthcare providers with innovative ways to deliver weight management programs that could have an impact on health care at the population level. A randomized study will be conducted on 70 obese adults (BMI 30.0–45.0 kg/m2) to determine if weight loss (6 months) is equivalent between weight management interventions utilizing behavioral strategies by either a conference call or social media approach. The primary outcome, body weight, will be assessed at baseline and 6 months. Secondary outcomes including waist circumference, energy and macronutrient intake, and physical activity will be assessed on the same schedule. In addition, a cost analysis and process evaluation will be completed.
Keywords: Social media, Obesity, Methods, Distance learning
1. Introduction
Approximately 69% of U.S. adults are classified as overweight or obese (BMI > 25) [1]. Obesity is associated with significant comorbidity; it is estimated that for every one-point increase in body mass index (BMI), health care costs increase by 8% [2] and the estimated cost of obesity in the U.S. was $147 billion in 2008 [3]. Current clinical guidelines recommend behavioral based programs, which include energy restriction and physical activity to produce clinically relevant weight loss of 5% or more of total body weight [4–10]. Management of obesity in the context of the primary care physician visit is of limited efficacy (1.4–2.5 kg weight loss at 6 months [11], in part because of limited ability to engage participants in sustained behavior change between physician visits. Furthermore, numerous barriers prevent individuals from participating in weight management programs, including cost, transportation, time, family and job commitments, and others. These same barriers are frequently cited as reasons why individuals who do participate subsequently drop out of treatment. Therefore, healthcare systems must find methods to address obesity that reach beyond the walls of clinics and hospitals and address the issues of lifestyle modification in a cost-conscious way.
Alternative strategies to deliver weight management programs have produced promising results. Delivery of weight management services through over-the-phone group visits with a health educator following a social cognitive theory-based curriculum on diet, exercise, and healthy lifestyle across 18 months has been shown to produce equivalent weight loss with significantly lower costs compared to traditional face to face delivery. [12]. However, over the past decade the use of internet-delivered health care/health behavior change interventions, including weight management, has greatly expanded. With the dramatic increase in technology and online social networks (OSN), individuals have started to pursue information, share experiences, ask questions and provide support to peers about health online [13–15]. OSN may present health care providers innovative ways to deliver weight management programs that could have an impact on health care at the population level by minimizing barriers such as cost, time to deliver materials, and access to hard-to-reach populations as 70% of all house-holds in the United States report internet use and this will only increase in the future [16]. Several short-term studies have shown that incorporating social media into weight loss interventions led to favorable weight loss outcomes [17–19]. Using OSN to produce health behavior change is in its early stages of development and, while several studies show promise, more research is needed to acquire information about optimizing these interventions to increase their efficacy.
2. Materials and methods
2.1. Overview of study design
The purpose of this feasibility study is to compare weight loss between an established cost effective weight management delivery system (group conference call) and OSN (Facebook) delivered weight management intervention. Seventy obese men and women have been randomly assigned to a 6-monthweight loss program that will be delivered by group conference call (n = 34) or Facebook (n = 36). The behaviorally-based conference call group is considered the reference treatment in this study because this method has been shown to produce clinically significant weight loss while reducing barriers and cost [12]. Behavioral group meetings for both the conference call and OSN groups will be conducted weekly. Outcomes were assessed at baseline and will be assessed at 6 months. We expect equivalent and clinically significant (≥5%) weight loss in both groups. Change in weight was selected as the primary outcome. Secondary outcomes include waist circumference as an indication of reduction in chronic disease risk, and measures of dietary intake and physical activity to help explain both group and individual differences in weight change. A cost analysis and extensive process evaluation will also be completed. We expect similar participant and provider costs in the OSN group. Approval for this study was obtained from the Human Subjects Committee at the University of Kansas Medical Center. Recruitment, randomization and baseline testing have been completed thus far for the study.
2.2. Participant eligibility
To improve the generalizability of the results, individuals with chronic medical conditions were allowed to participate because they represent the population of individuals typically seeking weight management. For instance, individuals with hypertension or type 2 diabetes were not automatically excluded if their condition was controlled by medication. Medical conditions and medication use may be considered potential confounders; however, randomization should ensure that health status will be similar across both study groups. Inclusion criteria: 1) Age 21 to 70 years. This age range was chosen as weight management for young or older individuals typically employs different behavioral strategies. 2) Body mass index (BMI) of 30 to 45 kg/m2. The sample is restricted to this BMI range because individuals with a BMI greater than 30 kg/m2 are at a higher risk and weight loss would have the greatest cost savings [7,9,20], and individuals with a BMI > 45 kg/m2 require more aggressive weight loss interventions than we propose (e.g., surgery, medication, etc.) [7]. And 3) Have access to a computer, smart phone, or tablet with access to wireless internet or cell data. The Fitbit activity tracker and wireless scale, which was provided to participants, require wireless internet or cell data for real time data transferring. Exclusion criteria: 1) Unable to participate in moderate intensity PA (i.e., walking). 2) Participation in a weight loss or physical activity program in the previous 6 months as these proximal experiences may impact the results of this study. 3) Greater than 3, 30-min bouts of planned exercise/week. 4) Not weight stable (±4.6 kg) for 3 months prior to intake. 5) Unwilling to be randomized to 1 of the 2 study groups. 6) Report being pregnant during the previous 6 months, currently lactating, or planned pregnancy in the following 6months. 7) Serious medical risk such as cancer, recent cardiac event (i.e. heart attack, stroke, angioplasty) in the previous 6 months as determined by the study's medical director to participate in the investigation. 8) Current use of antipsychotics or untreated depression. Care of individuals with complex psychiatric illness can be challenging due to balancing medication side effects and is outside the scope of this study. 9) Adherence to specialized diet regimens, e.g., multiple food allergies, vegan, macrobiotic. 10) Binge eating disorder as assessed by the Binge Eating Scale [21] and Eating Attitudes Test [22]. 11) Lack of access to a grocery store. These individuals would not have the ability to make food choices on their own thus would not be able to follow the diet protocol and the results would not have been generalizable to them.
2.3. Recruitment/randomization
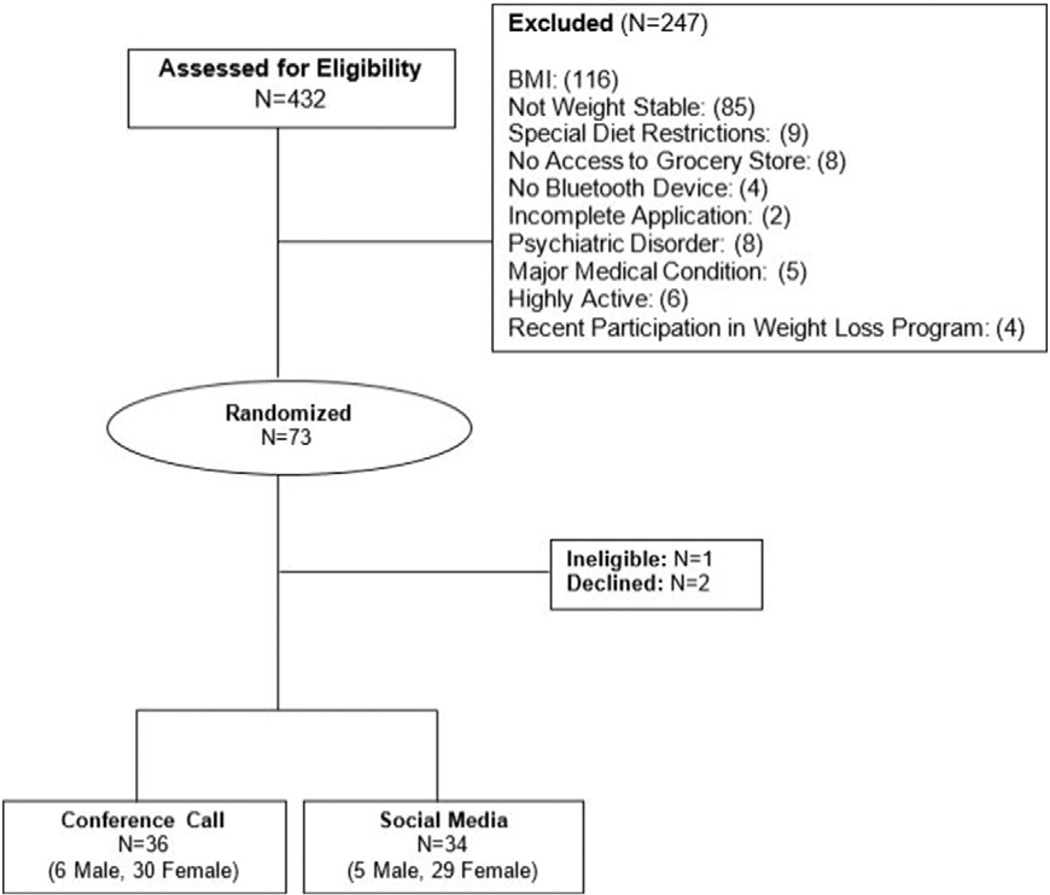
Participants were recruited using university broadcast emails, flyers, the General Medicine Clinic at the University of Kansas Medical Center and the wait list for participation in the Center for Physical Activity and Weight Management'sWeight Control Research Projects. Potential participants were asked to contact study staff via phone or email. Interested individuals were directed to complete an initial eligibility questionnaire through Research Electronic Data Capture (REDCap) version 6.4.4 hosted at The University of Kansas Medical Center [23]. Participants provided self-reported height and weight (BMI), medication use, previous attempts at weight loss, presence of chronic disease, current physical activity level, and special diet restrictions. Those satisfying the initial eligibility criteria were invited to an orientation session where the procedures were explained, the risks and benefits outlined, the commitments of the participants and investigators explained, and all questions answered prior to obtaining written informed consent. Those who chose to participate were directed to fill out all the remaining screening surveys including a brief health history, eating attitudes [22], binge eating scale [21], Global Physical Activity Questionnaire [24], and the Revised Center for Epidemiologic Studies Depression Scale [25] on REDCap. Eligible participants were enrolled in the study by the project coordinator and randomized in 1:1 ratio to the phone or OSN group stratified by sex. After randomization participants were scheduled to attend a separate 45-minute testing appointment for collection of baseline measures by research assistants. Fig. 1 presents a modified Consolidated Standards of Reporting Trials. The (CONSORT) diagram [26] describes the number of potential participants assessed for eligibility, the number of participants excluded or screened out, reason for screening failure, and the number randomized to the conference call or OSN groups. The baseline characteristics of the conference call and OSN clinic groups are presented in Table 1.
Fig. 1.
CONSORT diagram.
Table 1.
Baseline characteristics.
| Variable | Conference Call | Social media | p-Value | ||||
|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | ||
| Age | 36 | 47.6 | 11.7 | 34 | 46.8 | 13.2 | 0.815 |
| Weight | 36 | 220.0 | 33.5 | 34 | 217.3 | 30.2 | 0.953 |
| Height | 36 | 65.8 | 2.9 | 34 | 64.5 | 2.9 | 0.062 |
| BMI | 36 | 35.5 | 3.7 | 34 | 36.7 | 4.2 | 0.249 |
| Waist circumference | 36 | 101.8 | 10.9 | 34 | 102.9 | 11.7 | 0.622 |
| Female (%) | 83 | 85 | 0.822 | ||||
| Minorities (%) | 22 | 26 | 0.679 | ||||
2.4. Intervention conceptual framework
This feasibility study will compare two approaches for the delivery of a behavioral weight management intervention (conference call and OSN) for weight loss. Similar to many current weight management programs, the interventions is grounded in social cognitive theory, problem-solving theory, and the relapse prevention model [27–31]. Key elements incorporated in both the phone and OSN interventions include: goal-setting, self-monitoring, direct reinforcement, interaction with health educators, and social support.
2.5. Standardized materials
To ensure that similar content is presented in both the conference call and OSN groups, all participants will receive identical lessons that will provide a basic outline for the intervention. Therefore, the diets and PA protocols, behavioral lesson topics, experiential learning assignments and attention (i.e. meeting and assessment schedules), will be identical for both groups. The lessons include detailed instructions for the weight loss phase including behavioral strategies, diet instructions, recipes, and guidelines for PA. The lessons are organized by clinic session and contain handouts, worksheets, and assignments specific to each topic. The lessons also provide general information and guidelines for conduct and participation in the program. An outline of topics discussed by week can be found in Table 2.
Table 2.
Outline of weekly intervention topics.
| Week | Topic |
|---|---|
| 1 | Orientation to program. Introduction to diet |
| 2 | Picking healthy food items |
| 3 | Diet review & benefits of exercise |
| 4 | Goals and values |
| 5 | Food labels — your tools to healthy eating |
| 6 | Exercise 101 |
| 7 | Portion distortion |
| 8 | Fruits and vegetables |
| 9 | Healthy cooking tips and techniques |
| 10 | Meal planning |
| 11 | Surviving social situations |
| 12 | Warm ups/cooldowns & injury prevention |
| 13 | Eating out & snacking on the go! |
| 14 | Antecedents, behaviors, & consequences |
| 15 | Frequency, intensity, time and type of exercise |
| 16 | Metabolism & energy expenditure |
| 17 | Energy density |
| 18 | Mental traps & mindful thinking |
| 19 | Fad diets |
| 20 | Making exercise a habit |
| 21 | Knowing your health numbers |
| 22 | Exercise: the biggest predictor of weight management |
| 23 | Maintaining motivation |
| 24 | Relapse prevention |
2.6. Diet — weight loss (months 0–6)
For participants in both the phone and OSN groups, total daily energy expenditure will be estimated using the equation of Mifflin–St. Jeor [32] with an activity factor for sedentary/low active individuals of 1.15. Energy intake will be reduced 500–700 kcal/d below the calculated estimated total daily energy expenditure. Participants will be asked to consume a nutritionally balanced, reduced energy, high volume, lower fat (fat = 20% energy) diet as recommended by the Academy of Nutrition and Dietetics [33] and the USDA's MyPlate approach [34]. Participants will be provided examples of meal plans consisting of suggested servings of grains, proteins, fruits, vegetables, dairy, and fats based on their energy needs and will be counseled on appropriate portion sizes.
2.7. Physical activity (months 0–6)
Participants in both the phone and OSN groups were prescribed a progressive moderate intensity PA program (walking, jogging, biking, etc.) as recommended in the “2009 ACSM Position Stand on Physical Activity Interventions for Weight Loss and Prevention of Weight Regain in Adults,” [10]. PA will progress from 45 min/wk in month 1 to 300 min/wk at month 4, and remain at 300 min/wk for the duration of the study (Table 3). Fitbit wireless activity monitors will be provided as a motivational tool, track steps over the 6 months and as incentive to participation in the intervention.
Table 3.
Exercise progression.
| Week | Days per week | Minutes per day | Total for week |
|---|---|---|---|
| 1 | 3 | 15 | 45 |
| 2 | 3 | 20 | 60 |
| 3 | 4 | 20 | 80 |
| 4 | 4 | 25 | 100 |
| 5 | 4 | 30 | 120 |
| 6 | 5 | 25 | 125 |
| 7 | 5 | 30 | 150 |
| 8 | 5 | 40 | 200 |
| 9 | 5 | 45 | 225 |
| 10 | 5 | 50 | 250 |
| 11 and on | 5 | 60 | 300 |
2.8. Health educators
The potential for health educator bias will be minimized by randomly assigning health educators to administer one conference call and one OSN group congruently to eliminate potential between-group differences due to the health educator. Health educators will have backgrounds in nutrition, exercise physiology or behavioral counseling. The content of 20% of the recorded sessions will be compared with a checklist of required content. Health educators failing to deliver ≥80% of the required content will receive additional training to assure standardized delivery of the two interventions.
2.9. Self-monitoring
Self-monitoring is an important predictor of adherence and treatment outcomes in weight management [35]. Therefore, participants in both the phone and OSN groups will be asked to monitor body weight, diet/food consumed, minutes of exercise, steps, and completion of homework assignments. Diet: Patients will log all food and beverages consumed (meals/snacks) using the MyFitnessPal™ application. We will create a MyFitnessPal™ account for each participant, with customized energy intake goals (see Diet above). Patients will log all food and beverages consumed by entering the food name and selecting the portion size or by scanning the bar code of the food item using a smart phone. As a food is entered a bar showing the recommended dietary intake goal for each participant is displayed, providing immediate feedback of how much food patients have consumed during the day and how much more or less they should consume. PA: Patients will be asked to wear a Fitbit Flex (Model: Flex tracker, Fitbit Inc. San Francisco, CA, size 35.5×28 mm) wireless activity tracker on their wrist. The Fitbit records time spent in moderate or vigorous PA that is automatically transferred to the MyFitnessPal™application via Bluetooth connectivity when the device is near the smart phone or computer, thus eliminating the need for manual data recording. The MyFitnessPal™ application provides immediate feedback on a participants accumulated PA relative to their goal via a graphic display. If a participant engages in PA that cannot be recorded by the Fitbit (e.g. biking), they log the activity in the MyFitnessPal™ application and record the information. Reminders: The MyFitnessPal™ application allows reminders to be programed to prompt participants to record their self-monitoring PA/diet data. Reminders will be sent only if no information is reported for a given meal (e.g., breakfast, lunch, dinner) or goal (i.e., exercise time, steps, weight). Weight. Participants' body weight will be obtained weekly to provide feedback regarding weight loss/gain over the course of the trial. Participants will self-weigh prior to each behavioral session using a calibrated wireless digital scale (Model: Withings Wireless Scale, WITHINGS, Inc. Cambridge, MA), which automatically syncs with the MyFitnessPal™ application and updates a visual display of weight change.
2.10. Phone conference intervention
During baseline assessments participants randomized to the phone group will be provided with written information explaining the basic logistics of the conference calls, which will be conducted using the Maestro conferencing system (Oakland, CA). During the 6 month weight loss intervention conference calls well be held once a week lasting approximately 60 min. Participants will be asked to dial a toll-free number 5 min prior to the scheduled meeting time and then enter a unique identifying code number that allows them to “enter” the meeting. In the interest of safety, participants were asked to not call in situations where their attention is compromised, such as while driving, operating machinery, etc. Specific procedures relative to the conduct of the conference call, such as how to request to speak, courtesy to group members, reporting, confidentiality, etc. will be discussed during the first phone session. Each session will include a check-in question to generate discussion regarding diet and PA, a review of compliance with the diet and PA protocols, a lesson on a weight management topic, and an experiential learning assignment that requires problem solving or the practice of behavioral weight management strategies to be completed prior to the next meeting. For example, assignments may include grocery shopping/meal planning to meet specific caloric or nutritional guidelines, eating in social situations or during holidays, food label reading, trying a new form of PA, etc. Assignments will be discussed at the subsequent meeting, and the health educator will provide feedback.
2.11. OSN behavioral clinic
Participants randomized to the OSN group for weight loss will be asked to join a private Facebook group using their personal OSN accounts. The weight loss program will be structured into online modules presented through the private OSN group of 12–18 individuals. Modules will be one-week in length (i.e. module week of Monday through Sunday) for 6 months. Participants will receive contact information for study personnel, instructions and guidelines for appropriate online posting and discussion, detailed descriptions of the diet and PA prescriptions, instruction on how to track energy intake, F/V intake and PA on a daily basis, and handouts/worksheets/assignments specific to each meeting. In addition, each lesson will include assignments and discussion forums that each participant must complete and submit to the OSN discussion board by the due date. As previously described, the meeting content will be identical for both the phone and OSN groups. However, the OSN and phone conference interventions differ in several important aspects. OSN allows for both lessons and audio recordings to be posted and accessed at any time by the participants, which is not possible on the phone conference call. Participants can have access to materials 24 h a day seven days a week and are able to work at a rate that is comfortable for them within the program guidelines. Throughout the week the health educators will post in the discussion forum to highlight the major points of the lesson, and problem solve if necessary. Participants who are subscribed to the group will receive a notification any time someone submits a message and is able to comment or like the original post.
2.12. Outcome assessments
With the exception of PA, which will be assessed by accelerometry during free-living activity, outcome data for both intervention groups will be collected in the Center for Physical Activity and Weight Management laboratory by trained staff at baseline (0 months) and following weight loss (6 months). At baseline assessments participants received the Fitbit physical activity tracking device, wireless scale, and a 30 minute orientation on how to use each device.
2.13. Anthropometrics (weight, height, and waist circumference)
Anthropometric assessments will be obtained between the hours of 6:00 and 10:00 AM prior to breakfast and after attempting to void. Participants will be weighed wearing shorts and a t-shirt using a digital scale accurate to ±0.1 kg (Befour Inc. Model #PS6600, Saukville, WI). Height will be measured using a stadiometer (Model PE-WM-60-84, Perspective Enterprises, Portage MI) and body mass index (kg/m2) will be calculated. Waist circumference, a measure that will be used as a surrogate for abdominal adiposity, will be measured using the procedures of Lohman et al. [35]. Three measurements will be obtained and the average of the 2 closest measurements will be used for analysis.
2.14. Energy and macronutrient intake
Baseline and end study (6months) energy and macronutrient intake will be assessed using energy intake and macronutrient data obtained from the MyFitnessPal application for 3 days (2 weekdays, 1 weekend day) prior to their scheduled clinic visit to identify dietary habits prior to the intervention.
2.15. Physical activity
Participants will wear an ActiGraph GT1X portable accelerometer (ActiGraph LLC, Pensacola, FL) on a belt over the non-dominant hip for 7 consecutive days at each assessment time point. Matthews et al. [36] have shown that a 7-day monitoring period provides measures of both physical activity and inactivity with a reliability of 90%. Accelerometer data will be collected in 1-min epochs with a minimum of 10 h constituting a valid monitored day. Day 1 of the 7-day monitoring period will begin on the day following baseline data collection. At the completion of the 7-day period, participants will return the ActiGraph accelerometer using a padded postage-paid envelope provided by the investigators. At subsequent data collection points, ActiGraph accelerometers will be mailed to participants and returned in postage paid envelopes. The main outcome variable will be the average ActiGraph counts/min over the 7-day period. In addition, the average number of min/day over 7-day spent at various activity levels will be assessed using the cut-points used in the National Health and Nutrition Examination Survey as described by Troiano et al. [37]. A SAS data reduction program will be used to complete the analyses described.
2.16. Questionnaires
Participants will complete the Health Related Quality of Life short form health survey (SF-36) [38] and the quality of life changes related to weight will be assessed using the SHIELD-WQ-9 questionnaire [39]. Moderators and mediators of diet and physical activity change will be assessed using the weight efficacy life style questionnaire [40], exercise self-efficacy scale [41], barriers-specific self-efficacy scale [42], and the physical activity self-regulation questionnaire [43,44]. Changes in social support and social network will be assessed using the interpersonal self-evaluation list-12 [45] and the social network index [46].
2.17. Process analysis
To compare the level of participation across the intervention groups, health educators will record the following information over the course of the 6-month intervention collected from phone conference call or OSN group: 1) number of diet records submitted on MyFitnessPal™; 2) the number of diet records submitted on MyFitnessPal™ within ±100 kcal of the participants prescribed calorie goal; 3) physical activity (minutes and steps) each week collected by the Fitbit device; 4) the number of weights recorded with the wireless scale; and 5) attendance at scheduled meetings/OSN posts made.
In conjunction with end-study collection of anthropometric data (month 6), a brief survey will be collected using Redcap to assess: 1) overall satisfaction with the general features of the intervention; 2) attributes of the intervention important to the participant (i.e., convenience/ease of participation, timeliness, flexibility with scheduling, group rapport, cost); and 3) the extent to which the intervention met the participant's expectations; i.e., perceived quality of the intervention, suggestions for improvements, etc.
2.18. Cost analysis
A potential advantage to delivery of weight management by Facebook/OSN may be lower fixed and variable costs for both participants and providers. Fixed costs are independent of the number of individuals participating while variable costs are directly associated with the number of participants enrolled [47]. Costs depend on the resources used and the prices of those resources, and valid cost analyses are based on a clear understanding of the actual process being evaluated [48,49]. To assure a complete accounting of the resources used in the phone conference call and OSN groups, a process flow chart will be created and validated by consensus of the investigators [50]. Information about resource use will be obtained by conducting structured interviews with providers (i.e. investigators/health educators) and surveys of a random sample of participants (20%) equally distributed across the group conference call and OSN groups.
The cost of the conference line (Maestro) used to conduct the interventions will be determined based on the monthly bill received from the company. The costs of provider time (i.e. wages/benefits) will be estimated as the number of hours worked obtained from provider maintained logs, multiplied by the provider's wage. We anticipate that communications and provider costs will be lower for the OSN intervention. The cost of participant time associated attendance to the phone meetings will be estimated from self-report of time spent in these activities multiplied by the median wage in the region. Whether participant costs will differ between the groups is not known.
2.19. Analysis plan — primary outcomes
The primary goal of this feasibility trial is to evaluate weight loss achieved at 6 months by intervention delivered by conference call as compared to one delivered using OSN [51]. Sample demographics and all outcome measures will be summarized by descriptive statistics; means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Two sample t-test will be used to compare weight loss from 0 to 6 months between groups randomized to conference call and OSN delivery. An intent-to-treat analysis for the primary comparison will be used. Secondarily, a per-protocol analysis will also be performed. Per-protocol will be defined as attending ≥75% of all scheduled meetings and weight data at all assessments (baseline, 6 months). The impact of baseline characteristics (age, sex, race/ethnicity, weight, etc.) on weight loss will be determined using linear regression controlling for treatment. The main effects of each of these variables as well as the potential interaction effect with treatment will also be examined. All statistical analyses will be conducted using SAS versions 9.4 or higher with a type 1 error rate of 5%.
2.20. Analysis plan — process evaluation
To look at the influence of participant characteristics that may contribute to or detract from intervention effects self-reported data from the weekly reports (i.e. number of reports, number of reports within calorie range, physical activity) will be examined to monitor adherence to the diet and physical activity program components in the conference call and OSN groups. Best-subsets analysis will be used to examine the impact of these variables, as well as baseline demographic characteristics, to identify variables that explain weight loss at 6 months. while controlling for treatment. We will examine both main effects and potential variable by treatment interactions.
2.21. Analysis of plan cost
A two-sample t-test will be used to compare average costs for participants, providers, and the totals for the conference call and OSN groups. If adjustments for demographics are needed despite the randomization, the t-test will be part of a regression model. (This assumes that the OSN group will have equal or better weight loss outcomes.) If not, we will use Wilan's [52] approach to estimate the cost-effectiveness acceptability curve. For participants the costs will primarily be time costs, but we will also collect data on incidental costs (including travel). Provider costs will include personnel, communications, supply, and equipment costs. We anticipate that personnel and communications savings will result in lower costs for the SM group. Total costs will sum participant and provider costs. Again, we anticipate significantly lower costs for the SM group.
3. Discussion
There is a need for the development and evaluation of effective alternative strategies for producing weight loss that diminish or eliminate barriers and/or enhance approaches to behavioral weight loss interventions. The internet has become a popular platform for delivering behavioral, health-related interventions as they may offer a cost-effective alternative to traditional interventions, with the potential to reach large numbers of individuals while reducing barriers to participation (e.g. travel, child care costs, etc.). The dramatic growth in technology and OSN (i.e. Facebook) has generated recent interest in OSN-based strategies as a delivery medium of health behavior change campaigns. OSN delivered programs have potential to be a more cost-effective approach to reach a large group of individuals. Using OSN to produce health behavior change is in its early stages of development and while several studies show promise, more research is needed to acquire information about optimizing these interventions to increase their efficacy.
This paper describes the rationale and design for a randomized preliminary study to compare a behavioral weight loss intervention (6 months) delivered by group phone conference call or SM. Several conceptual aspects of intervention delivery through OSN suggest that this approach may be effective for weight loss. Behavior change in OSN is reinforced by social group support and distance learning strategies that continue to remove the time commitment barrier to delivery of weight loss interventions. The OSN learning environment allows for unlimited access to intervention materials that can be completed at a work rate that is comfortable for the individual and the ability for constant group feedback. For example, in OSN participants can post about their success and struggles with the intervention at any time during the day through the private group page.
Strengths of this study include: 1) a design specific to evaluating two potentially effective strategies for the delivery of a weight loss intervention. 2) Both technologies evaluated are readily available and accessible. Phone use is ubiquitous in the US and 70% of Americans over the age of 18 have high-speed internet in their homes [16] as well as 74% of adults report using OSN [53].Thus, if successful, the interventions could be widely disseminated. 3) Phone comparison group is a proven technology. Phone delivery of weight management has been previously shown to produce equal and significant weight loss compared to traditional face to face intervention with reduced cost and time burdens [12]. 4) Inclusion of both cost and process analyses. While lower cost of delivery is commonly cited as a benefit to OSN delivered interventions to date the literature lacks a formal cost analysis for OSN interventions. However, this study is not without its limitations. The purpose of this study is to inform future larger scale adequately powered trials. Due to funding and supply restraints the sample size is relatively small and was not powered to detect between group differences.
Overall, the dramatic increase in technology and popularity of OSN has presented healthcare providers an innovative way to deliver weight management programs. If successful this study will provide an alternative technique, using distance learning strategies and readily available technology, to deliver weight management interventions.
Acknowledgments
Disclosure of funding: This study was supported by Blue Cross Blue Shield of Kansas City.
Footnotes
Conflict of interest
The authors report no conflict of interest.
Clinical Trials Registration: NCT02496871.
Contributor Information
Erik A. Willis, Email: ewillis@ku.edu.
Amanda N. Szabo-Reed, Email: aszabo2@ku.edu.
Lauren T. Ptomey, Email: lptomey@kumc.edu.
Felicia L. Steger, Email: fsteger@ku.edu.
Jeffery J. Honas, Email: jhonas@ku.edu.
Eyad M. Al-Hihi, Email: eal-hihi@kumc.edu.
Robert Lee, Email: rlee2@kumc.edu.
Lisa Vansaghi, Email: lvansaghi@kumc.edu.
Richard A. Washburn, Email: rwashburn@ku.edu.
Joseph E. Donnelly, Email: jdonnelly@ku.edu.
References
- 1.Ogden CL. N.C.f.H. Statistics, Prevalence of obesity in the United States, 2009–2010, US Department of Health and Human Services, Centers for Disease Control and Prevention. National Center for Health Statistics; 2012. [Google Scholar]
- 2.Algazy J, et al. Why governments must lead the fight against obesity. Medicine. 2009;361(23):2252–2260. [Google Scholar]
- 3.Finkelstein EA, et al. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff. 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 4.Foreyt JP, Goodrick GK. Evidence for success of behavior modification in weight loss and control. Ann. Intern. Med. 1993;119(7):689–701. doi: 10.7326/0003-4819-119-7_part_2-199310011-00014. [DOI] [PubMed] [Google Scholar]
- 5.Racette S, et al. Effects of aerobic exercise and dietary carbohydrate on energy expenditure and body composition during weight reduction in obese women. Am. J. Clin. Nutr. 1994;61:486–494. doi: 10.1093/ajcn/61.3.486. [DOI] [PubMed] [Google Scholar]
- 6.Meckling KA, O'Sullivan C, Saari D. Comparison of a low-fat diet to a low-carbohydrate diet on weight loss, body composition, and risk factors for diabetes and cardiovascular disease in free-living, overweight men and women. J. Clin. Endocrinol. Metab. 2004;89(6):2717–2723. doi: 10.1210/jc.2003-031606. [DOI] [PubMed] [Google Scholar]
- 7.Jensen MD, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J. Am. Coll. Cardiol. 2014;63(25_PA):2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 8.Raynor HA, Champagne CM. Position of the Academy of Nutrition and Dietetics: interventions for the treatment of overweight and obesity in adults. J. Acad. Nutr. Diet. 2016;116(1):129–147. doi: 10.1016/j.jand.2015.10.031. [DOI] [PubMed] [Google Scholar]
- 9.Dietz WH, et al. Management of obesity: improvement of health-care training and systems for prevention and care. Lancet. 2015;385(9986):2521–2533. doi: 10.1016/S0140-6736(14)61748-7. [DOI] [PubMed] [Google Scholar]
- 10.Donnelly JE, et al. American College of Sports Medicine Position stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med. Sci. Sports Exerc. 2009;41(2):459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 11.Wadden TA, et al. Managing obesity in primary care practice: an overview with perspective from the POWER-UP study. Int. J. Obes. 2013;37:S3–S11. doi: 10.1038/ijo.2013.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donnelly JE, et al. Equivalent weight loss for weight management programs delivered by phone and clinic. Obesity. 2013 doi: 10.1002/oby.20334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turner JW, Grube JA, Meyers J. Developing an optimal match within online communities: an exploration of CMC support communities and traditional support. J. Commun. 2001;51(2):231–251. [Google Scholar]
- 14.Eysenbach G, et al. Health related virtual communities and electronic support groups: systematic review of the effects of online peer to peer interactions. BMJ. 2004;328(7449):1166. doi: 10.1136/bmj.328.7449.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jayanti RK, Singh J. Pragmatic learning theory: an inquiry–action framework for distributed consumer learning in online communities. J. Consum. Res. 2010;36(6):1058–1081. [Google Scholar]
- 16.File T. Computer and internet use in the United States. Population Characteristics. 2013 [Google Scholar]
- 17.Napolitano MA, et al. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity. 2013;21(1):25–31. doi: 10.1002/oby.20232. [DOI] [PubMed] [Google Scholar]
- 18.Turner-McGrievy GM, Tate DF. Weight loss social support in 140 characters or less: use of an online social network in a remotely delivered weight loss intervention. Transl. Behav. Med. 2013;3(3):287–294. doi: 10.1007/s13142-012-0183-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Valle CG, et al. A randomized trial of a Facebook-based physical activity intervention for young adult cancer survivors. J. Cancer Surviv. 2013;7(3):355–368. doi: 10.1007/s11764-013-0279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cawley J, et al. Savings in medical expenditures associated with reductions in body mass index among US adults with obesity, by diabetes status. PharmacoEconomics. 2015;33(7):707–722. doi: 10.1007/s40273-014-0230-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gormally J, et al. The assessment of binge eating severity among obese persons. Addict. Behav. 1982;7(1):47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 22.Garner DM, et al. The eating attitudes test: psychometric features and clinical correlates. Psychol. Med. 1982;12(04):871–878. doi: 10.1017/s0033291700049163. [DOI] [PubMed] [Google Scholar]
- 23.Harris PA, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Armstrong T, Bull F. Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ) J. Public Health. 2006;14(2):66–70. [Google Scholar]
- 25.Eaton WW, et al. Center for Epidemiologic Studies Depression Scale: Review and Revision (CESD and CESD-R) 2004 [Google Scholar]
- 26.Moher D, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J. Clin. Epidemiol. 2010;63:e1–e37. doi: 10.1016/j.jclinepi.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Bandura A. Self-efficacy: toward a unifying theory of behavior change. Psychol. Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 28.Bandura A. Health promotion by social cognitive means. Health Educ. Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 29.Marlatt G, Gordon J. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behavior. New York: Guilford Press; 1985. [Google Scholar]
- 30.Prochaska JO, Marcus BH. The transtheoretical model: applications to exercise. Exercise Adherence II. 1998 [Google Scholar]
- 31.Prochaska JO, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol. 1994;13(1):39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- 32.Mifflin MD, et al. A new predictive equation for resting energy expenditure in healthy individuals. Am. J. Clin. Nutr. 1990;51(2):241–247. doi: 10.1093/ajcn/51.2.241. [DOI] [PubMed] [Google Scholar]
- 33.Cummings S, Parham ES, Strain GW. Position of the American Dietetic Association: weight management. J. Am. Diet. Assoc. 2002;102(8):1145–1155. doi: 10.1016/s0002-8223(02)90255-5. [DOI] [PubMed] [Google Scholar]
- 34.U.S Department of Agriculture. Choose MyPlate. 2013 Available from: www.choosemyplate.gov.
- 35.Lohman TG, Roche AF, Martorell R. Anthropometric Standardization Reference Manual. Champaign, Ill: Human Kinetics Books; 1988. [Google Scholar]
- 36.Matthews CE, et al. Sources of variance in daily physical activity levels as measured by an accelerometer. Med. Sci. Sports Exerc. 2002;34(8):1376–1381. doi: 10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 37.Troiano RP, et al. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 38.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med. Care. 1992:473–483. [PubMed] [Google Scholar]
- 39.Grandy S, et al. Changes in weight loss-related quality of life among Type 2 diabetes mellitus patients treated with dapagliflozin. Diabetes Obes. Metab. 2014 doi: 10.1111/dom.12263. [DOI] [PubMed] [Google Scholar]
- 40.Clark MM, et al. Self-efficacy in weight management. J. Consult. Clin. Psychol. 1991;59(5):739. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- 41.McAuley E. Self-efficacy and the maintenance of exercise participation in older adults. J. Behav. Med. 1993;16(1):103–113. doi: 10.1007/BF00844757. [DOI] [PubMed] [Google Scholar]
- 42.McAuley E. The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. J. Behav. Med. 1992;15(1):65–88. doi: 10.1007/BF00848378. [DOI] [PubMed] [Google Scholar]
- 43.Umstattd MR, et al. Self-regulation and physical activity: the relationship in older adults. Am. J. Health Behav. 2008;32(2):115–124. doi: 10.5555/ajhb.2008.32.2.115. [DOI] [PubMed] [Google Scholar]
- 44.Umstattd MR, et al. Measuring physical activity self-regulation strategies in older adults. J. Phys. Act. Health. 2009;6(1):S105. doi: 10.1123/jpah.6.s1.s105. [DOI] [PubMed] [Google Scholar]
- 45.Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. J. Appl. Soc. Psychol. 1983;13(2):99. [Google Scholar]
- 46.Cohen S, et al. Social ties and susceptibility to the common cold. JAMA. 1997;277(24):1940–1944. [PubMed] [Google Scholar]
- 47.McLean RA. Financial Management In Healthcare Organizations. Albany, NY: Delmar Publishers; 1997. [Google Scholar]
- 48.McLaughlin CP, Kaluzny AD. Continuous Quality Improvement in Health Care: Theory, Implementation, and Applications. Aspen, Gaithersburg, MD: 1999. [Google Scholar]
- 49.Lee RH, et al. Process-based costing. J. Nurs. Care Qual. 2003;18(4):259–266. doi: 10.1097/00001786-200310000-00003. [DOI] [PubMed] [Google Scholar]
- 50.Dranove D. Measuring costs. In: Sloan FA, editor. Valuing Health Care: Costs, Benefits, and Effectiveness of Pharmaceuticals and Other Medical Technologies. New York, NY: Cambridge University Press; 1996. pp. 61–80. [Google Scholar]
- 51.Wellek S. Testing Statistical Hypotheses of Equivalence. Boca Raton FL: Chapman Hall; 2003. [Google Scholar]
- 52.Willan AR. Statistical analysis of cost–effectiveness data from randomized clinical trials. Expert Rev. Pharmacoeconomics Outcomes Res. 2006;6(3):337–346. doi: 10.1586/14737167.6.3.337. [DOI] [PubMed] [Google Scholar]
- 53.S.N.F. Sheet. Pew Research Internet Project. 2014 [Google Scholar]