Abstract
Purpose
The purpose of this research was to describe the application of a model of knowledge exchange, the Knowledge Exchange-Decision Support (KE-DS) Model, to the Canadian pilot of Cancer Transitions, a psychosocial program for cancer survivors.
Method
We compared and contrasted the program planning and implementation processes across three diverse sites offering Cancer Transitions. The KE-DS Model guided the collection and analysis of observations and written data according to specific model components.
Results
The use of the KE-DS Model highlighted four pertinent factors that influenced knowledge exchange during planning and implementation processes of this psychosocial program. First, the geographic diversity of where these programs were offered affected strategies for program promotion, recruitment and means of access. Second, the variation of the professional and organizational capacity of the three sites was critical to program planning and delivery. Third, cultural values and norms shaped each site’s approach. Fourth, the KE-DS Model identified populations who were included and excluded from participation.
Conclusions
The KE-DS Model was useful in elucidating the processes of knowledge exchange during the planning and implementing of an intervention for survivor care. This process information will inform future offerings of Cancer Transitions.
Keywords: Knowledge exchange, Psychosocial, Cancer survivor
Introduction
The number of cancer survivors worldwide has risen considerably in recent decades as the result of early detection and advances in treatment. Currently, there are nearly one million cancer survivors in Canada (Canadian Partnership Against Cancer) and 9.8 million survivors in the United States (U.S.) (Rowland et al.,). This dramatic increase has resulted in the recognition of cancer survivorship as a distinct phase in the cancer trajectory (Hewitt et al., 2006). During this phase, cancer survivors may face a host of difficulties due to the physical, psychological, and social consequences of cancer and its treatments. As such, health services for cancer survivors are essential to ensure that these issues are appropriately managed and to improve cancer survivor outcomes. The unique and unmet needs of cancer survivors have recently been highlighted in national and international reports by A National Coalition for Cancer Survivorship and the Institute of Medicine (2007), the National Cancer Institute (2007), and the Canadian Partnership Against Cancer (2010). Although cancer survivorship is an international phenomenon, countries and heath care systems worldwide have focused their attention on cancer care and research at different times and in different ways. A recent U.S. publication titled National Action Plan for Cancer Survivorship: Advancing Public Health Strategies authored by the US National Coalition for Cancer Survivorship, the National Cancer Institute Office of Survivorship, the US Centers for Disease Control and Prevention and the Lance Armstrong Foundation, provides an expanded definition of survivorship (2004). Survivors are defined as individuals living with cancer, their families as well as their care givers, “from the day of diagnosis through the remainder of their lives” (Shapiro et al., 2009:6). Rather than focus solely on the cancer-free time, this definition conceptualizes survivorship as a continuum with different phases (Shapiro et al., 2009). As cancer survivorship increasingly appears on other national health care agendas, as it has in the US and Canada, the importance of engaging in dialog and collaboration with fellow researchers, clinicians and decision makers as a first step in developing effective, evidence-informed strategies requires immediate attention.
Further to the international discourse on evidence-based practice and policy, the exchange of information and evidence has been recognized as critical to promoting best practices in health care, including cancer survivorship. This process has been referred to using many different terms. In Canada, knowledge exchange (KE) is defined as “collaborative problem-solving between researchers and decision makers that happens through linkage and exchange. Effective KE involves interaction between decision makers and researchers and results in mutual learning through the process of planning, producing, disseminating and applying existing or new research in decision making” (Canadian Health Services Research Foundation). Although substantial work has gone into developing KE strategies, there remain significant barriers including time, culture, resources and incentives (Lomas, 2000). Moreover, systematic approaches targeting health care providers, administrators and policy makers to facilitate KE remain underdeveloped.
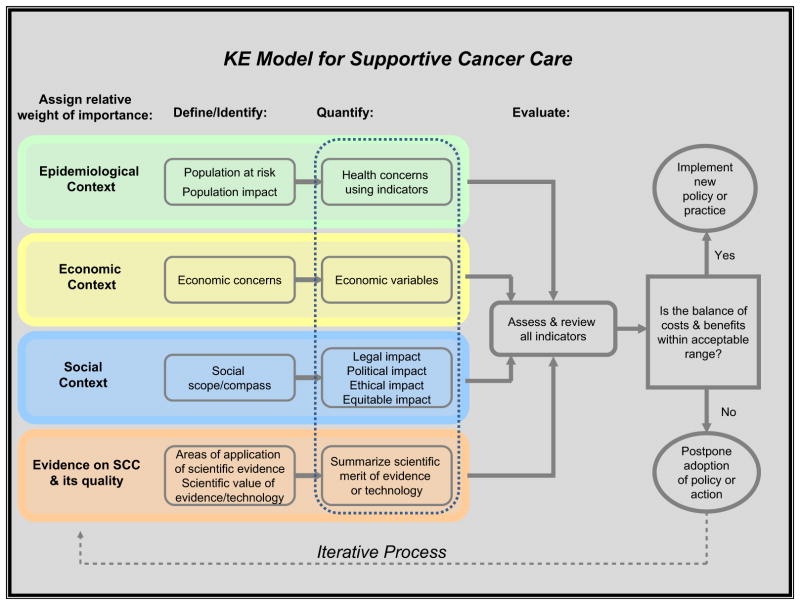
Traditionally, the process of KE has been viewed as linear and unidirectional, whereby researchers and scientists disseminate data on the effectiveness of an intervention, and clinicians and policy makers adopt it. This conceptualization does not accurately depict the dynamic and complex set of relationships between knowledge producers and users (Baumbusch et al., 2008; Graham et al., 2006). In order for researchers to translate data and evidence into a meaningful product for knowledge users, and for knowledge users to inform the research agenda so that meaningful questions and issues are investigated, dialog and interaction at all stages of the research process is key (Lavis, 2006; Ross et al., 2003). For that purpose, we developed a structured approach to KE designed to delineate the iterative set of interactions between the creation of new information, strategies for dissemination and translation, and activities related to implementation of new knowledge into current practice. The Knowledge Exchange - Decision Support (KE-DS) Model was developed reflecting the principles of evidence-informed medicine and tailored specifically for the field of cancer survivorship (Kazanjian et al., 2009a) (Fig. 1).
Fig. 1.
KE-DS Model for Supportive Cancer Care.
The development of the KE-DS Model was informed by a Health Technology Assessment (HTA) approach. HTA is a systematic, multi-disciplinary process that examines the effectiveness and cost-effectiveness of health interventions and delineates social, ethical and legal implications (Banta and Luce, 1993). It incorporates a diversity of theoretical perspectives including epidemiology, economics and ethics. The KE-DS Model is an iterative model that positions the processes involved in bringing evidence to the development and implementation of an intervention as central to program success. The focus on process aims to be inclusive of different types of knowledge, such as experiential, tacit as well as scientific, recognizing that both producers and end users of knowledge draw from a diversity of knowledge forms acquired over a period of time (Baumbusch et al., 2008; Bartunek et al., 2003; Goldenberg, 2006; Lambert, 2006). By engaging program managers in the initial planning stages of a program, it is assumed that they will share their knowledge as well as their knowledge needs through explicit seeking of information and health interventions. In contrast, research findings are often presented as effectiveness studies, devoid of context, that is, under controlled conditions, and often reported as “absolute” patient outcomes that may have little relevance to end users (Bartunek et al., 2003). We aimed to develop a model that moves beyond implicit conceptual underpinnings of knowledge development, synthesis and translation, by making explicit the dynamic nature of knowledge exchange in context. Thus, moving beyond measures of efficacy and effectiveness usually reported in HTA assessments, the KE-DS Model encourages managers to consider at the outset what measures of program success they will use. Consequently, dissemination activities are more likely to be tailored to the needs of these specific end users in their particular context because they have been engaged throughout program planning and delivery. Furthermore, the KE-DS Model assists with organization and communication between program managers and officials in their organization by facilitating transparent reporting during all stages of program planning and implementation.
Knowledge exchange activities are vital to promoting evidenced-informed health care for cancer survivors. Therefore, early in the development of the KE-DS Model and on an on-going basis, we verified the value of the Model through one on one discussions with clinician managers and system level decision makers involved in different cancer survivorship initiatives. Support for the utility of this model was also expressed by clinicians implementing supportive cancer care navigation programs in Canada (Kazanjian et al., 2009c). While early use of the Model as a KE tool for several supportive cancer care programs across Canada has been encouraging, refinement of the Model is ongoing. Cancer Transitions (CT) is a U.S. cancer survivorship program developed specifically to meet the needs of cancer survivors in the U.S. (The Wellness Community). This program also shows promise in addressing the needs of Canadian cancer survivors. Here, we discuss the application of the KE-DS Model to the Canadian pilot of the CT program.
Methods
The purpose of this study was to use the KE-DS Model to identify and describe the knowledge exchange processes pertaining to the development and implementation of the CT pilot program in three different Canadian sites. In the absence of a structured approach, usually KE activities remain unidentified. Guided by the assertion that the context is equally as important as the intervention itself (Geertz, 1973), we aimed to illustrate, through the use of the KE-DS Model, how the different social environments of the CT program would require different types of knowledge and evidence to support program delivery. We also sought to describe the processes of program planning and implementation in a range of health care and community settings. A qualitative approach was deemed the most appropriate for this study. The structured KE-DS Model assisted us in organizing each site-specific program’s experiences into common themes, while at the same time allowing for the richness of their experiences to remain intact. The aim, therefore, was not to evaluate the effectiveness of the intervention (the CT program) or the resulting patient outcomes.
Description of participants
The KE-DS Model was used to describe the attributes of the CT program that was piloted in three locations across Canada. These three sites constituted the cases in this KE study. Two program sites were located in the province of British Columbia. The site located in the Northern region of the province is rural and remote. The health authority in this region serves 300,000 people over an area of 600,000 square kilometers (Northern Health, 2010). There is no cancer centre in this region, rather, treatment and services are administered through regional and local hospitals. The second site in British Columbia was an urban location on the West Coast of the province. Here, a full service cancer centre provides oncology consultations, chemotherapy and radiotherapy treatments, and provides a broad range of services including prevention, treatment, screening, education and survivorship care for patients, family and friends. A variety of cancer specific support groups are available through the centre. The third site was a metropolitan centre in the province of Quebec. The program operated out of a peer-support, volunteer based oncology centre that is managed by professional staff and comprised of more than 300 volunteers. The centre is a member and supporter of the clinical care teams at the partnering hospitals and is connected to a network of community and academic organizations. Ethics approval for the CT pilots was secured by the individual site’s respective agency or associated university.
The CT program aims to assist survivors in making the transition from active treatment to post-treatment care by focusing on emotional well-being, exercise, nutrition, medical management, and survivorship care planning (Ward, 2010). Stakeholders across sites and on different levels endorsed the need for psychosocial services for cancer survivors. The CT program aligned with national cancer control priorities (Canadian Strategy for Cancer Control), as well as patient demands in each of the three Canadian communities. The U.S. originated CT program has a set curriculum and provides guidelines for personnel requirements and the outcome measures that each program site is to utilize. The program consists of six, 2.5 h sessions, a booster session and a 3 month follow up. Participants were eligible for the program if they had completed cancer treatment within the last 24 months and had no known recurrence or secondary cancer. Participants received a workbook, exercise log, food diary, action plan and health journal. The recommended human resources included a fitness expert, dietician, medical expert, facilitator and psychosocial expert. The CT program utilized specific proxy outcome measures to assess the early impact of the program, reported elsewhere (Ward, 2010). The use of the KE-DS Model was intended to highlight the variations in the evidentiary base in planning and implementation processes across the CT sites as a complement to the program outcome measures. Through this process, the knowledge ecology of each site reflected how the CT program was delivered at these locations.
Data collection
The KE-DS Model was initially introduced by the research team at an in-person meeting with the three program leads. They were instructed about the development of the KE-DS Model and how it could be used as a planning and implementation tool. The KE researcher followed up this meeting with a phone call to each site lead regarding their understanding of the KE-DS Model and its application and continued to check in with the site lead over the course of the piloting of the CT program.
Detailed descriptions that captured the nuances and subtleties of CT program planning and implementation in a Canadian health care system and at the three different sites were necessary for a comprehensive documentation of program operationalization and implementation. These descriptions included detailed notes stemming from ongoing phone interviews, informal correspondence, email exchanges, and exit phone interviews between the researchers and site leads. The important details on program implementation are usually lost to memory when a program is eventually evaluated for effectiveness. During the exit phone interviews, the KE researcher posed closed- and open-ended questions related to each module in the KE-DS Model (see Table 1). For example, close-ended questions asked whether potential stakeholder groups relevant to the program had been involved, while open-ended questions queried how the program teams dealt with opportunities and barriers. Throughout data collection, the researcher verified notes through email with CT program leads who contributed comments, clarified details and elaborated on the processes involved in planning and implementing the program where these intersected with knowledge mobilization activity. Program documents were also reviewed. These data were collected from March through to September, 2009.
Table 1.
Modules and Module steps of the KE-DS model.
| Module | Module steps |
|---|---|
| Outline the intervention | Summarize the intervention |
| Establish the need | |
| Establish the literature and evidence | |
| Create a site reflection | Indentify the stakeholders |
| Consider the population context | |
| Population of interest | |
| Population impact | |
| Outcome Indicators | |
| Re-visit the program initiative | |
| Consider the economic context | |
| Consider the social context | |
| Consider the evidence context | |
| Reflect and report | Re-visit and evaluate the program |
Data analysis
During the analysis of data we coded site-specific notes according to the modules of KE-DS Model, treating each of these modules as a theme. These modules/themes included: establishing the need, site description, stakeholders, population of interest, population impact, social context and economic context and the type and quality of evidence incorporated (explicitly and implicitly) in program implementation. This involved two members of the research team reading through all the notes and categorizing these data according to the KE-DS modules/themes. We then prepared descriptive summaries for each program site according to these themes. These summaries were then compared and contrasted noting similarities and differences among sites throughout the process of planning and implementing CT. As a means of member-checking, the summaries were shared with the respective program leads to verify our interpretations. Comments made by program leads were then incorporated into the summaries. Once finalized with all program leads, the summaries were compiled into a report and made available electronically (Kazanjian et al., 2009b).
Results
There was appreciable variation in the development and implementation of Cancer Transitions at the specific sites. Here we describe those components that most influenced the delivery and the success of the program in each site that only became apparent through systematic use of the KE-DS Model. We will focus on four salient themes that emerged through the use of the KE-DS Model at each site: community geography; professional and organizational capacity; community culture; and inclusivity.
Community geography
The three communities where the CT program was piloted were geographically diverse. The northern area of British Columbia is rural and remote, while the West Coast region of the province serves both rural and urban populations. The site in Quebec was in a centrally located urban setting. The weather conditions experienced by these areas are also diverse, with northern British Columbia and Quebec experiencing heavy snow fall and short days in the long winter months, while the West Coast of British Columbia experiences temperate weather. The geographic diversity of these communities required strategies for promotion and recruitment as well as accessibility, thus drawing on different knowledge and evidence to support these activities.
Promotion and recruitment strategies reflected the centrality of services in each community. The more centralized the program site was, the less resources required to market the program and recruit participants. The marketing and promotion strategies utilized by the Quebec team were fairly minimal – the team sent information via their email list to registered clients who were post-treatment. The team found that word of mouth was effective as volunteers and staff spoke to potential participants, and participants to each other. Outside advertising via newspaper or radio were unnecessary because posters on bulletin boards and internal advertising in the hospital were sufficient for reaching their community of interest. Similarly, the West Coast site’s most successful promotion and recruitment strategies were those that occurred through the central cancer centre, such as word of mouth, emails, internal flyers and direct referrals from oncologists, nurses and counselors. While public service announcements and newspapers were marginally useful in raising the program’s profile over the long term, the program lead found their value limited as a promotional tool to attract participants.
In contrast, the Northern site required a large media presentation that consumed half of the program budget. As there is no central cancer centre, patients move through a number of separate hospitals resulting in little walk-through contact with potential CT participants. This resulted in a promotion strategy utilizing media outlets, including newspaper, radio and TV advertisements that reached the large geographic region.
The ability to access the CT program was complicated for those living in the Northern region by the fact that some participants had to travel up to 200 km to attend the program. The long commute was a burden for many; however, despite the time and distance, these participants continued to attend because of the support they received. The program was scheduled for Saturday delivery since the sun sets early during the winters in this area and thus residents tend to “hibernate” during the week. Leaving the house and having an activity to participate in on a Saturday morning was deemed motivating. City traffic and parking were taken into consideration by the Quebec team who also scheduled their program on Saturday mornings. There were no reported issues of access to the program for the West Coast site.
Professional & organizational capacity
The variation of the professional and organizational capacity of the three sites was a critical aspect of program planning and delivery. Different types of knowledge and evidence were considered by the program leads to address organizational capacity. With its established centre, the Quebec site was well supported to complete the administrative duties associated with the program, such as screening participants, follow-up phone calls and scheduling of expert speakers. In contrast, the West Coast and Northern sites had limited administrative capacity to carry out these tasks in addition to their already busy service schedules.
Professional capacity varied amongst sites. In accordance with the curriculum of the CT program, program sites were required to include a nutritionist, an oncologist and a fitness expert. Although there were nutritionists and oncologists available in all three sites, access to a qualified and experienced fitness expert posed significant challenges for both the West Coast and Northern sites in British Columbia. While both sites had difficulty locating a fitness expert with experience in working with individuals suffering from chronic illness, the Northern site was able to train a qualified fitness instructor who was eager to learn new skills and commit to future programs. The facilitator assisted the fitness expert with slide presentations, and consulted before the sessions to answer questions or offer feedback from previous sessions. This mentoring, encouragement and feedback was considered essential to developing the role and speaks to the ability of the program facilitator to spend time on this training. The experience of the West Coast team in training the available fitness experts was met with some difficulty. The fitness expert’s unfamiliarity with the medical needs and physical ability of the participants was difficult to overcome despite efforts by the facilitator to offer literature, presentation material and other resources. In contrast, the Quebec team had an exercise specialist on staff with expertise in exercise physiology.
There was also diversity amongst sites in their access to well equipped and appropriate exercise facilities. The Quebec team had an existing exercise facility on site, and many of the participants had taken part in previous exercise programs tailored to the needs of cancer survivors. While the West Coast team did not have an exercise facility on site, they were able to move to a better equipped location after realizing that their designated space was too small and too warm. Having now offered the CT program more than once, the West Coast team has been successful in engaging a fitness facility in the ongoing program delivery and the exercise component.
Community culture
The cultural norms and values of each community shaped the team’s approach to program delivery. As each program lead was also a local community member, they had insight into the norms and values of the community, as well as available resources and lessons learned from previous programs. For example, the facilitator for the Northern team described the largest city in the area as a “last minute city”, meaning people sign up for programs at the last moment possible. Promotion of the program was scheduled for the 2 weeks leading up to the start date, and, as was expected, 75% of participants signed up the week before the program began. In contrast, the West Coast team noted that 5–6 weeks was a more realistic amount of promotion time in their community. The respective approaches reflected the special knowledge and experiential evidence each team possessed regarding their community.
Knowledge that community members were reluctant to engage or commit to support groups offered in the past directed the facilitator of the Northern site to promote the CT program as educational rather than solely supportive. Furthermore, the facilitator was acutely aware of the community need for accessible resources and a variety of forms of physical activity.
Community values and norms regarding food and nutrition were apparent amongst residents of the West Coast and the North. The CT program curriculum strongly emphasizes the importance of eating organic foods and recommends particular food brands popular in the U.S. Our data from the West Coast program indicated that tailored discussions needed to take into consideration the community perception that eating organic foods is expensive, and that buying U.S. brands is not a practical or desirable option. Furthermore, this feedback from the community was incorporated into the revised Canadian version of the CT program. The program lead was aware that the participants were highly literate and had conducted their own research on nutrition related to their particular cancers. They were “hungry” for good and credible information, as they had read a great deal that was contradictory. It was, therefore, essential that the program has the latest nutrition information to draw from when responding to local concerns. The perceptions of some participants in the North around healthy eating differed from participants in the other sites. For example, some believed that white bread was as healthy a choice as whole wheat bread. Access to nutritional education through the CT program hopefully changed theses perceptions.
Inclusivity
The use of the KE-DS Model directed program leads to consider whose needs were being met and whose were not. The unique composition of each community had consequences for who was included and who was excluded from participation. In Quebec, the CT program was offered in a predominantly French speaking city. Offering an English program serves to effectively exclude the French speaking population. The Quebec team is planning to pilot a French version in the subsequent year. The West Coast program noted that they were concerned it was targeting only a small percentage of survivors – those who were highly motivated, literate and relatively more able bodied. The enormous geographic area that the Northern program site was serving required many participants to have access to their own vehicle, money to pay for gas and the time to commute. Potential solutions to overcome these barriers include the organizing of transportation to pick up participants in satellite communities, and the use of Telehealth or online groups to bring the service to remote communities.
Discussion
The piloting of the U.S. CT program in three diverse communities across Canada illustrated how necessary it was for program leads to tailor the planning and implementation to meet the unique needs of Canadians and the specific local communities served. The KE-DS Model was invaluable as a tool to highlight the diversity of experiential and other evidence pertinent to the processes of program planning and delivery. The program leads reported that the KE-DS Model was helpful in reflecting on the processes of program planning and delivery, and that this would improve future delivery. As a structured framework that prompts its users about making transparent what evidence and knowledge they are bringing to the program and its implementation, the KE-DS Model identified the most salient knowledge and evidence issues across the three program sites to be community geography; professional and organizational capacity; community culture; and inclusivity. In addition, the rich experiential evidence, as well as the research evidence, generated through the use of the KE-DS Model complemented the program evaluation data on proxy measures of patient outcomes.
The use of the KE-DS Model by program leads yields new evidence about the science of KE. As a KE tool, the KE-DS Model shares many common features with other models, such as the Ottawa Model for Research Use (OMRU) (Logan and Graham, 1998) or the University of Leeds Knowledge Brokering Model (Ward et al., 2010a,b). All three models share a multi-disciplinary approach. The OMRU is a useful model for facilitating the uptake of evidence in practice settings, whereas the KE-DS Model shifts the focus to the broader social context, highlighting the importance of capturing the interactive processes in planning and implementation. The Knowledge Brokering Model was developed and validated very recently in the mental health field. While it is very similar to our KE-DS Model, the former is more complex to use and designed to be applied by a knowledge broker. The KE-DS Model is more parsimonious in nature, raising the same questions to consider in identifying the evidence and knowledge needs of its users as the Knowledge Brokering Model, and could easily by applied by a program manager/lead, as demonstrated by our three cases.
In these early stages of national strategy development and collaboration it is particularly important that attention to program implementation processes be considered as important opportunities for knowledge exchange. Beyond local and national boundaries, the KE-DS Model illustrates the importance of involving pertinent stakeholders throughout all stages in order to maximize effective KE (Gagnon et al., 2009). Knowledge of and attention to the beliefs and values of the communities being served allowed program leads to tailor the development and implementation processes to these identified needs. The findings from the application of the KE-DS Model also contributed evidence that was used to further refine aspects of the Model. This included the development of practical tools such as worksheets and templates for reporting. The Model, along with these tools make up the KE-DS Toolkit, which can be used to promote KE in the fields of supportive cancer care, and elsewhere (Kazanjian et al., 2009a).
With cancer survivorship being a current priority in Canada as well as internationally, this research illustrates some of the complexities of developing health services to meet the needs of cancer survivors. It has previously been noted in the literature that people living in rural and remote communities face barriers to accessing health services (McGrath, 2001; Pesut et al., 2010; Wilkes et al., 2006). The results of this research indicate that access to services for cancer survivors are no exception. Rural and remote communities experience a host of barriers related to geography, professional capacity, and unique cultures. Despite these challenges, many individuals in these communities exhibit a willingness and creativity to overcome these barriers. Faced with limited resources, program managers drew on their local knowledge and experience in their communities to tailor services to meet patient demands. As developing capacity in the area of survivorship care is relatively new, results from this research illustrate that professional capacity is needed in a number of different areas, particularly in rural and remote regions. Time and resource allocation must be carefully considered in countries such as Canada that are geographically diverse and operate with a publicly funded health care system. Recognizing the post-treatment well being of cancer survivors is a necessary step, yet it is not sufficient if we fail to tend to individual and community diversity within system-specific contexts.
The KE-DS Model is relevant to cancer survivorship owing to the input of clinical and research experts and decision makers in its development. In this study, the Model was used by program managers and applied to the CT pilot programs in different sites. The tacit knowledge that the CT program leads possessed was specific to the context of cancer survivorship, and this evidence, along with research evidence, could inform future program planning and resource allocation nationally as well as internationally (Bartunek et al. 2003). While this program has been effective in a North American context, research is needed to investigate the applicability of the CT intervention for global implementation. Our findings regarding how evidence, experiential and research, was used by the managers may generate discussion within the field of survivorship research, but the KE-DS Model could also be valuable as a tool to identify the unique program characteristics appropriate for communities and populations other than cancer survivors.
There are two limitations apparent in this research. First, as the Model relies on self-reported assessments, program leads chose what to include in their reports. It is possible that some KE issues were underreported or omitted by one site but emphasized by another. Further depth of evidence and knowledge being utilized in planning and implementation of programs could have been obtained through the use of additional analytical measures, yet pilot program time constraints did not permit this. Second, due to the small number of participating sites, the Model requires further empirical verification and review. A larger number of applications would likely yield other details relevant to components of the Model that are pertinent to KE in other programs. Our future research on KE will focus on the utility of the KE-DS Model in different settings related to cancer survivorship.
Conclusion
The processes understood and discussed in KE remain somewhat opaque and complicated; the KE-DS Model provides transparency as a tool for bridging the knowledge to action gap. In this case, the KE-DS Model was used as a prompt to managers to make knowledge generation, translation and exchange more transparent.
The early successes of the Canadian pilot of the CT program has laid the foundation for the delivery of this program at 12 sites across the country this year, including cancer centers, hospitals, and community based organizations. Evidence generated using the KE-DS Model provides a more robust and structured approach to the planning and implementation processes at these diverse sites. In the future, survivorship programs can draw on this evidence to improve these processes that would ultimately lead to more successful initiatives. In addition, the systematic collection of new knowledge from future such initiatives will contribute optimally to the existing knowledge base. The structured exchnge of knowledge between researchers, program managers and health care practitioners facilitates communication through the use of a tool to document and organize the often neglected aspects of program implementation and lessons learned. Using a structured approach improves the exchange of this knowledge, and promotes the development of sustainable programs for cancer survivors.
Acknowledgments
Sources of support
Canadian Partnership Against Cancer (CPAC), Canadian Institute of Health Research (CIHR). Dr. Fuchsia Howard holds a Michael Smith Foundation for Health Research (MSFHR) Post Doctoral Research Trainee Award.
Footnotes
Conflict of interest
None declared.
References
- Hewitt M, Ganz P. A National Coalition for Cancer Survivorship and Institute of Medicine national cancer policy Forum Workshop, the Lance Armstrong foundation and the national cancer Institute. Implementing Cancer Survivorship Care Planning. The National Academies Press; 2007. rapporteurs. http://www.iom.edu/Reports/2006/Implementing-Cancer-Survivorship-Care-Planning-Workshop-Summary.aspx. [Google Scholar]
- Banta HD, Luce BR. Health Care Technology and It’s Assessment: An International Perspective. Oxford University Press; New York: 1993. [Google Scholar]
- Baumbusch JL, Kirkham SR, Khan KB, McDonald H, Semeniuk P, Tan E, Anderson JM. Pursuing common agendas: a collaborative model for knowledge translation between research and practice in clinical cettings. Research in Nursing & Health. 2008;31:130–140. doi: 10.1002/nur.20242. [DOI] [PubMed] [Google Scholar]
- Bartunek J, Trullen J, Bonet E, Sauquet A. Sharing and expanding academic and practitioner knowledge in health care. Health Services Research and Policy. 2003;8:62–68. doi: 10.1258/135581903322405199. [DOI] [PubMed] [Google Scholar]
- Canadian Health Services Research Foundation. Knowledge Exchange. Canada: [cited July 6, 2010]. Available from: http://www.chsrf.ca/knowledge_transfer/index_e.php. [Google Scholar]
- Canadian Partnership Against Cancer. Partnership’s Survivorship Initiative Addresses Needs of Patients and Families Moving beyond Cancer treatment. [Internet] Canada [cited June 4, 2010]. Available from: http://www.partnershipagainstcancer.ca/node/714.
- Canadian Strategy for Cancer Control. Canada: [cited November 12, 2010]. Available from: http://www.cancer.ca/Canada-wide/How%20you%20can%20help/Take%20action/Advocacy%20what%20were%20doing/Cancer%20control.aspx?sc_lang=en. [Google Scholar]
- Gagnon M, Lepage-Savary D, Gagnon J, St-Pierre M, Simard C, Rhainds M, et al. Introducing patient perspective in health technology assessment at the local level. Health Services Research. 2009;9:54. doi: 10.1186/1472-6963-9-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geertz C. Thick description: toward an interpretive culture of theory. In: Geertz C, editor. The Interpretation of Culture: Selected Essays. Clifford Geertz. Basic Books; New York: 1973. [Google Scholar]
- Goldenberg MJ. On evidence and evidence-based medicine: Lessons from the philosophy of science. Social Science & Medicine. 2006;62:2621–2632. doi: 10.1016/j.socscimed.2005.11.031. [DOI] [PubMed] [Google Scholar]
- Graham I, Logan J, Harrison M, Straus S, Tetroe J, Caswell W, et al. Lost in knowledge translation: time for a map? The Journal of Continuing Education in the Health Professions. 2006;26:13–24. doi: 10.1002/chp.47. [DOI] [PubMed] [Google Scholar]
- Hewitt ME, Greenfield S, Stovali E. From Cancer Patient to Cancer Survivor: Lost in Transition. National Academy Press; Washington, DC: 2006. [Google Scholar]
- Kazanjian A, Howett C, Chan V, Smillie K. Knowledge Exchange Decision-Support Toolkit for Supportive Cancer Care. Final Report. 2009a Available from: http://spph.ubc.ca/sites/healthcare/files/KE-DS_Toolkit_October2009.pdf.
- Kazanjian A, Howett C, Smillie K. Supportive Cancer Care Programs: Further Application of the Knowledge Exchange-Decision Support Toolkit Final Report, 2009. 2009b Available from: http://spph.ubc.ca/sites/healthcare/files/KEDS_Report_Cancer_Transitions_OCT09.pdf.
- Kazanjian A, Howett C, Smillie K. Two Navigation Programs: Further Application of the Knowledge Exchange-Decision Support (KE-DS) Toolkit, 2009. 2009c Available from: http://spph.ubc.ca/sites/healthcare/files/KEDS_Report_Navigation_OCT09.pdf.
- Lambert H. Accounting for EBM: notions of evidence in medicine. Social Science & Medicine. 2006;62:2633–2645. doi: 10.1016/j.socscimed.2005.11.023. [DOI] [PubMed] [Google Scholar]
- Lavis J. Research, public policymaking, and knowledge-translation processes: Canadian efforts to build bridges. The Journal of Continuing Education in the Health Professions. 2006;26:37–45. doi: 10.1002/chp.49. [DOI] [PubMed] [Google Scholar]
- Logan J, Graham ID. Toward a comprehensive interdisciplinary model of health care research use. Science Communication. 1998;20:227–246. [Google Scholar]
- Lomas J. Using ‘linkage’ and ‘exchange’ to move research into policy at a Canadian foundation. Health Affairs. 2000;19:236. doi: 10.1377/hlthaff.19.3.236. [DOI] [PubMed] [Google Scholar]
- McGrath P. Returning home after specialist treatment for hematological malignancies: an Australian study. Family and Community Health. 2001;24:36–48. doi: 10.1097/00003727-200107000-00007. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute (US) Facing Forward Life after Cancer Treatment. National Institute of Health; US: 2007. p. 68. (NIH publication; no. 07-2424) [Google Scholar]
- Northern Health. About Northern Health. 2010 Available from: http://www.northernhealth.ca/About/
- Pesut B, Robinson CA, Bottorff JL, Fyles G, Broughton S. On the road again: patient perspectives on commuting for palliative care. Palliative and Supportive Care. 2010;8:187–195. doi: 10.1017/S1478951509990940. [DOI] [PubMed] [Google Scholar]
- Ross S, Lavis J, Rodriguez C, Woodside J, Denis J. Partnership experiences: involving decision makers in the research process. Journal of Health Services Research & Policy. 2003;8:26–34. doi: 10.1258/135581903322405144. [DOI] [PubMed] [Google Scholar]
- Rowland J, Mariotto A, Aziz N, Tesauro G, Feuer EJ, Blackman D, et al. Cancer Survivorship - United States, 1971–2001. United States: [Internet] [cited June 25, 2004]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5324a3.htm. [Google Scholar]
- Shapiro CL, McCabe MS, Syrjala KL, Friedman KL, Jacobs LA, Ganz P, et al. The LIVESTRONG survivorship center of excellence network. Journal of Cancer Survivorship. 2009;3:4–11. doi: 10.1007/s11764-008-0076-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Wellness Community. Cancer Transitions. United States: [Internet] Available from: http://www.thewellnesscommunity.org/mm/Treatment-Ends/cancertransitions.aspx. [Google Scholar]
- US National Coalition for Cancer Survivorship, the National Cancer Institute Office of Survivorship, the US Centers for Disease Control and Prevention and the Lance Armstrong Foundation. National Action Plan for Cancer Survivorship: Advancing Public Health Strategies. 2004 Available from: http://www.cdc.gov/cancer/survivorship/pdf/plan.pdf.
- Ward A. Cancer Transitions: Moving Beyond Treatment. Report Prepared for the Cancer Journey Action Group of the Canadian Partnership Against Cancer. 2010 Available from: http://www.bccancer.bc.ca/RES/ResearchPrograms/SBR/default.htm.
- Ward A, Doll R, Ristovski-Slijepcevic S, Kazanjian A, Golant M. Cancer transitions a supportive care program for cancer survivors. Oncology Exchange. 2010a;9:12–14. [Google Scholar]
- Ward V, Smith S, Carruthers S, Hammer S, House A. Knowledge Brokering Exploring the Process of Transferring Knowledge into Action. 2010b doi: 10.1186/1472-6963-9-12. Available from: http://www.leeds.ac.uk/lihs/psychiatry/research/TransferringKnowledgeIntoAction/documents/Knowledge%20Brokering%20Final%20report.pdf. [DOI] [PMC free article] [PubMed]
- Wilkes LM, White K, Mohan S, Beale B. Accessing metropolitan cancer care services: practical needs of rural families. Journal of Psychosocial Oncology. 2006;24:85–101. doi: 10.1300/J077v24n02_06. [DOI] [PubMed] [Google Scholar]