Abstract
Objectives
To study the relationship between cardiovascular risk factors and detectable Cardiac troponin-T using a highly sensitive assay (hs-cTnT) among persons without a history of cardiovascular disease.
Design and Methods
We examined the cross-sectional associations between cardiovascular risk factors and hs-cTnT in 9,593 participants (mean age 65.6 (SD, 5.6), 41% female, 22% black) free of cardiovascular disease in a community-based cohort, the Atherosclerosis Risk in Communities (ARIC) Study. We used multivariable logistic regression to characterize the association between cardiovascular risk factors and detectable (≥3.0 to 13.9 ng/L) and elevated (≥14.0 ng/L) hs-cTnT.
Results
hs-cTnT was detectable in 59% and elevated in 7% of the study population. Among persons with ideal cardiovascular health, hs-cTnT was detectable in 44%. In models adjusting for significant determinants of hs-cTnT concentration, detectable hs-cTnT was more frequent among males, blacks and persons with diabetes and hypertension and less frequent among statin users, current smokers and drinkers. Other risk factors associated with detectable hs-cTnT were older age, lower kidney function and higher body mass index. These risk factors were associated with elevated hs-cTnT in a similar pattern.
Conclusion
In a community-based sample without cardiovascular disease hs-cTnT is detectable in most adults, even among those with ideal cardiovascular health. Although most traditional cardiovascular risk factors were significant determinants of detectable and elevated hs-cTnT, the associations were particularly robust for sex, age, race, hypertension and diabetes.
Keywords: troponin, risk factors, epidemiology and cardiovascular disease
Introduction
Cardiac troponin-T is an established marker of myocardial damage 1. Although traditionally used in the clinical setting of acute coronary syndromes, others have previously shown detectable cardiac troponin-T in a very small proportion of asymptomatic individuals in the general population (less than one percent) 2 and the presence of cardiac troponin-T in these individuals has been linked to cardiovascular risk factors.
In contrast to the conventional cardiac troponin T assay were ~1% of the general population has detectable cardiac troponin T2, the hs-cTnT assay is detectable in up to 66% of individuals from the general population3–5. Using this assay, troponin concentrations far below the conventional limit of measurement have been shown to predict cardiovascular events and death in the general population3–5. Furthermore, hs-cTnT was more commonly detectable among men and associated with multiple other cardiovascular risk factors3,6–9.
There is a paucity of data regarding the determinants of detectable cardiac troponin-T in persons without clinical cardiovascular disease. We sought to study the relationship between cardiovascular risk factors and detectable hs-cTnT among persons without a history of cardiovascular disease in a community-based cohort, the Atherosclerosis Risk in Communities (ARIC) Study.
Methods
Study Population
Details of the study design and examination procedures have been previously described 10. Briefly, the ARIC Study enrolled 15,792 men and women aged 45 to 64 years during 1987–1989 from four US communities: Forsyth County, North Carolina; suburban Minneapolis, Minnesota; Washington County, Maryland; and Jackson, Mississippi. Follow-up on-site examinations took place in 1990–1992 (visit 2), 1993–1995 (visit 3), 1996–1998 (visit 4), and 2011–2013 (visit 5). Institutional review boards at participating institutions approved the study and informed consent was obtained from all subjects
The present study used data from visit 4, for which hs-cTnT measurements were available. There were 11,656 eligible participants who attended visit 4; we excluded individuals with adjudicated coronary heart disease (n=1,153)11, adjudicated stroke (n=195), or a hospitalization for heart failure (n=106) at or before visit 4, self-reported race other than black or white (n=29), missing covariate data (n=329) or missing hs-cTnT (n=251) for a final study sample of 9,953 participants with complete data.
Potential determinants
Age, sex, race, alcohol use and smoking status were ascertained from interviews with participants. History of diabetes was defined as a self-reported physician diagnosis of diabetes or use of glucose lowering medication during visit 4. Trained examiners measured weight, height 12 and blood pressure 13. Systolic and diastolic blood pressures were calculated as the mean of the first and second readings and body mass index as weight in kilograms divided by height in meters squared. Hypertension was define as systolic blood pressure greater than 140 mmHg, diastolic greater than 90 mmHg or use of blood pressure lowering medication. Plasma lipids were measured as previously described 14 and serum creatinine concentration was measured using a modified kinetic Jaffe method. Estimated glomerular filtration rate was calculated using the CKD-EPI (CKD Epidemiology Collaboration) equation 15. Serum glucose was measured by the hexokinase method 16. The ARIC 10-year risk score for coronary heart disease was derived by assessing ROC curves improvements with the addition of nontraditional risk factors and markers of subclinical disease to the basic model containing only traditional risk factors as previously described 17.
High-Sensitivity Cardiac Troponin T
Plasma samples collected from participants visit 4 were stored centrally at −80°C and used for measurement of hs-cTnT in 2010. hs-cTnT concentration were measured using a high-sensitivity assay, Elecsys Troponin T (Roche Diagnostics, Indianapolis, IN), implemented on an automated Cobas e411 analyzer; the limit of blank is 3 ng/L; and the lower limit of detection is 5 ng/L18. The between-assay coefficient of variations were 2.6% and 6.9% for control materials with mean hs-cTnT concentrations of 2378 ng/L and 29 ng/L, respectively. We assessed the repeatability of measurements using masked duplicate samples (n=418) and the reliability coefficient was 0.9818. We defined elevated hs-cTnT as concentration above a previously reported 99th percentile cut-off (14 ng/L) (Roche Diagnostics, data on file), corresponding to the 90th percentile of the distribution of hs-cTnT in our study population. The 10% coefficient of variation of the high-sensitivity assay is 13 ng/L, close or below the 99th percentile of the reference population (14 ng/L) 19. While high sensitivity troponin assays are being adopted in Europe and Canada, such assays are not in clinical use in the United States.
Statistical Analysis
First, we categorized hs-cTnT into three groups: those with undetectable hs-cTnT (<3 ng/L), those with detectable hs-cTnT (3–13.9 ng/L) and those with elevated hs-cTnT (hs-cTnT ≥14.0 ng/L). Baseline characteristics of the study population were compared across these categories.
We calculated the proportion of persons with detectable and elevated troponin according to number of traditional risk factors and according to the recently proposed definitions of “ideal,” “intermediate,” and “poor” cardiovascular health for adults by the American Heart Association Strategic Planning Task Force and Statistics Committee 20. We used multivariable linear and logistic regression models to characterize the associations of cardiovascular risk factors with hs-cTnT as a continuous and a categorical value, respectively.
For linear regression analysis, cardiovascular risk factors were modeled with cubic splines to characterize the shape of the association with hs-cTnT. We used multivariable logistic regression to assess the association between cardiovascular risk factors with detectable and elevated hs-cTnT.
All models included for the following covariates: sex (male or female), history of diagnosed diabetes (yes or no), age (years), race (white or black), body mass index (kg/m2), hypertension (yes or no), estimated glomerular filtration rate (ml/min/1.73 m2), alcohol consumption (current, former, or never), statin use (yes or no), smoking (current or not), education (less than high school, high school or equivalent, or more than high school), total, low and high-density cholesterol levels (mg/dL), high-sensitivity C-reactive protein (mg/L) and N-terminal pro b-type natriuretic peptide (NT-proBNP, pg/mL).
With the purpose of ruling out other potential causes of elevated hs-cTnT, we performed sensitivity analyses by excluded persons with atrial fibrillation before or at visit 4 and also by excluding persons with incident coronary heart disease up to 6 months after hs-cTnT samples were obtained. All analyses were conducted using Stata 11.1 (Stata Corp, College Station, TX) and a P-value of <0.05 was considered statistically significant.
Results
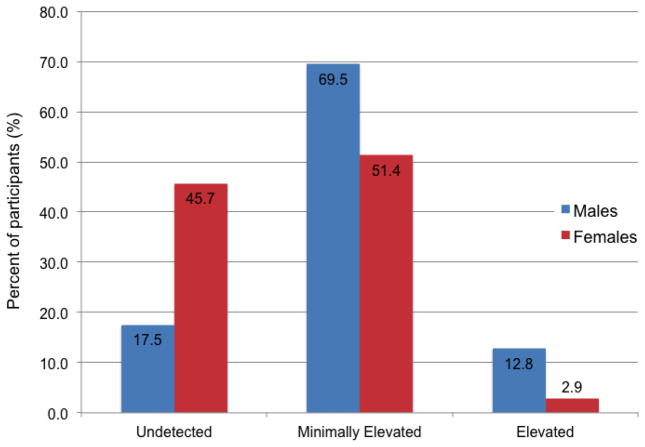
In our population of 9,593 persons without clinically evident cardiovascular disease, hs-cTnT was detectable in 59% (5,647 participants) and elevated in 7% (665 participants) of the study population. Figure 1 shows the distribution of hs-cTnT by sex in the study population. In contrast to females in whom 51% had detectable hs-cTnT and 3% had elevated hs-cTnT, 69% percent of males had detectable hs-cTnT while 13% had elevetad hs-cTnT. Increasing concentrations of hs-cTnT were associated with older age, male sex, black race, diabetes, and hypertension (Table 1).
Figure 1.
Distribution of highly sensitive cardiac troponin T (ng/L) by Sex
Table 1.
Baseline characteristics of participants by category of hs-cTnT, ARIC visit 4 (1996–1998)
| Undetectable | Detectable | Elevated | |
|---|---|---|---|
| Characteristic | n=3,281 | n=5,647 | n=665 |
| Range of hs-cTnT (ng/L) | Undetectable | 3.0 to 13.9 | ≥14.0 |
| Demographic characteristics | |||
| Age (years) | 60.7 | 63.4 | 65.2 |
| Male (%) | 20.9 | 48.4 | 75.2 |
| Black (%) | 21.9 | 21.4 | 29.3 |
| Smoking status (%) | |||
| Current | 20.8 | 11.4 | 12.0 |
| Former | 36.3 | 44.1 | 50.2 |
| Never | 42.9 | 44.4 | 37.7 |
| Education (%) | |||
| Less than high school | 15.1 | 18.7 | 25.1 |
| High School or equivalent | 45.4 | 41.3 | 34.6 |
| College or above | 39.4 | 40.0 | 40.3 |
| Alcohol use (%) | |||
| Current drinker | 52.5 | 49.9 | 44.1 |
| Former drinker | 26.9 | 28.4 | 37.4 |
| Never drinker | 20.5 | 21.7 | 18.5 |
| Medical history | |||
| Hypertension (%) | 38.1 | 46.6 | 63.2 |
| History of Diabetes (%) | 5.9 | 10.1 | 25.6 |
| Statin use (%) | 8.4 | 8.4 | 10.1 |
| Aspirin use (%) | 53.2 | 53.8 | 55.7 |
| Antihypertensive medication use (%) | 27.8 | 34.5 | 49.5 |
| Clinical measures | |||
| Systolic blood pressure (mmHg) | 124.2 | 128.2 | 132.6 |
| Diastolic blood pressure (mmHg) | 70.6 | 71.4 | 71.8 |
| Body-mass index (kg/m2) | 28.2 | 28.9 | 29.7 |
| Waist to Hip Ratio | 0.9 | 1.0 | 1.0 |
| Laboratory measures | |||
| hs-cTnT (ng/L) | - | 6.4 | 23.7 |
| Fasting glucose (mg/dl) ¶ | 104.0 | 110.2 | 124.2 |
| Total cholesterol (mg/dl) ¶ | 205.7 | 200.2 | 191.4 |
| LDL-cholesterol (mg/dl) ¶ | 124.4 | 123.3 | 118.1 |
| HDL-cholesterol (mg/dl) ¶ | 54.2 | 49.9 | 45.4 |
| Triglycerides (mg/dl) ¶ | 135.4 | 135.0 | 139.4 |
| eGFR (ml/min/1.73 m2) | 90.1 | 86.0 | 78.5 |
| hs-CRP (mg/L) | 4.5 | 4.1 | 5.9 |
| NT-pro-BNP (pg/mL) | 84.1 | 105.2 | 475.5 |
Values in table are mean (SD), median [IQR], or percentages.
Among participants fasting >=8 hours (n=10,037).
Abbreviations: BP denotes blood pressure, LVH left ventricular hypertrophy, hs-cTnT high sensitivity cardiac Troponin T, LDL low density lipoprotein, HDL high density lipoprotein, hs-CRP high sensitivity C-reactive protein, NT-proBNP N-terminal pro b-type natriuretic peptide.
P-value <0.001 for all baseline characteristics across hs-cTnT categories.
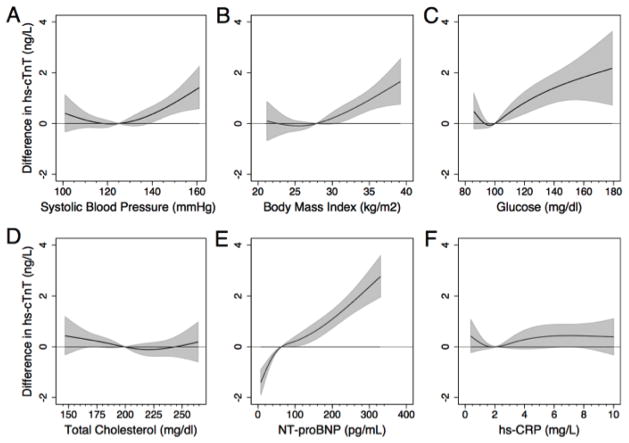
The continuous associations of systolic blood pressure, body mass index, glucose, total cholesterol, NT-proBNP, and hs-CRP with hs-cTnT after adjustment for traditional cardiovascular risk factors are shown in Figure 2. NT-proBNP (Figure 2, Panel E) was strongly and positively associated with higher hs-cTnT concentrations in a graded fashion. More moderate positive graded relationships were observed for systolic blood pressure, body mass index, and glucose but not with cholesterol or hs-CRP in this adjusted model.
Figure 2.
Restricted cubic spline models of the continuous association of selected cardiovascular risk factors with hs-cTnT levels.
The figures are centered at the median value of the cardiovascular risk factor on the X-axis. The shaded area represents the 95% confidence interval from the restricted-cubic-spline model. The plot was truncated at the 2.5th and 97.5th percentile of the risk factor on the X-axis (for hs-CRP truncated at values greater than 10 mg/L). All models were adjusted for age, sex, race/ethnicity (black or white), smoking (current, former or never), education (less than high school, high school or equivalent, or college or above), alcohol use (currently, former or never), hypertension (yes/no), body mass index, history of diabetes (yes/no), previous stroke, systolic blood pressure, hs-CRP, NT-proBNP, fasting glucose, estimated glomerular filtration rate, total, low-density and high-density cholesterol levels.
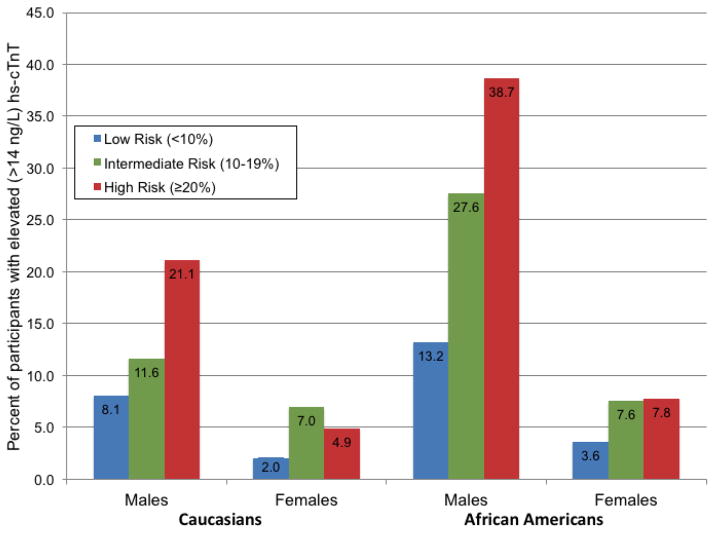
Having higher predicted 10-year coronary heart disease risk was associated with higher likelihood of having elevated hs-cTnT particularly among male participants (Figure 3). Irrespective of race or 10-year predicted cardiovascular risk, females were less likely to have elevated hs-cTnT concentration. Approximately 5% of white females at high predicted heart disease risk had elevated hs-cTnT concentration, compared to 21% of white males at high risk, and 39% of African American Males at high risk.
Figure 3.
Percent of Participants with Elevated Troponin (≥14.0 ng/L), by Sex, Race, and Estimated 10-year Risk of Coronary Heart Disease from the ARIC-CHD Risk Score
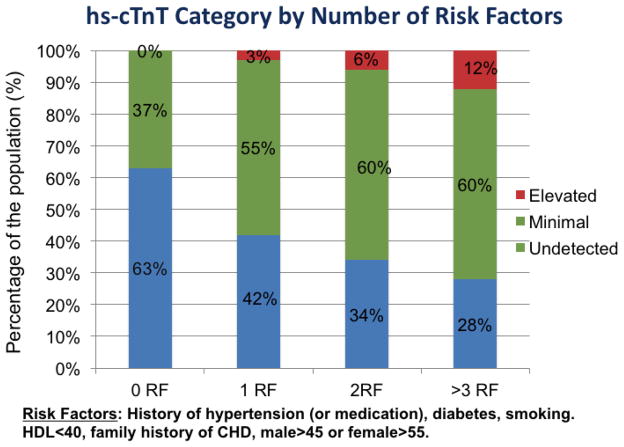
A higher burden of cardiovascular risk factors was associated with a higher prevalence of both detectable and elevated hs-cTnT (Figure 4). There were no participants with elevated hs-cTnT among those without cardiovascular risk factors. Hs-cTnT was detectable in 37% of persons without traditional cardiovascular risk factors, as compared to 55% of those with one risk factor, 60% in those with two risk factors, and 60% in those with three or more risk factors. Similarly, the prevalence of elevated hs-cTnT increased with greater number of cardiovascular risk factors.
Figure 4.
Percent of Participants with Detectable and elevated cTnT, by number of cardiovascular risk factors
Among persons with ideal cardiovascular health, 44% had detectable troponin and there were no individuals with elevated hs-cTnT (Figure 5). Among those with intermediate health, hs-cTnT was detectable and elevated in 59% and 4% respectively. Among those with poor health, the corresponding percentages were 59% and 7%.
Figure 5.
Percent of Participants with Detectable and elevated cTnT, by ideal, intermediate and poor cardiovascular health
In models adjusted for cardiovascular risk factors, male sex was associated with detectable hs-cTnT (OR 4.44, 95% CI 3.92, 5.14) (Table 2). Other significant risk factors included history of diabetes, older age, black race, body mass index and hypertension. Higher levels of eGFR, current alcohol consumption, and current smoking and statin use were all inversely associated with the prevalence of detectable hs-cTnT.
Table 2.
Adjusted* Odds Ratios (95% Confidence Intervals) for Detectable (≥3.0 to 13.9 ng/L) Cardiac Troponin T According to Cardiovascular Risk Factors
| Characteristic | OR | (95% CI) |
|---|---|---|
| Male (vs female) | 4.44 | (3.92, 5.14) |
| History of diabetes | 1.77 | (1.43, 2.16) |
| Age (per 5.6 years) | 1.58 | (1.50, 1.71) |
| African American (vs white) | 1.16 | (1.01, 1.33) |
| Body mass index (per 5.6 kg/m2) | 1.19 | (1.13, 1.26) |
| Hypertension | 1.19 | (1.03, 1.32) |
| eGFR (per 18.4 ml/min/1.73 m2) | 0.87 | (0.82, 0.92) |
| Current alcohol drinker (vs never) | 0.84 | (0.73, 0.96) |
| Statin use | 0.82 | (0.69, 0.98) |
| Current smoker (vs not) | 0.51 | (0.44, 0.58) |
Variables are expressed per 1 standard deviation unless otherwise noted.
Table shows risk factors significantly (p<0.05) associated with cTnT.
Adjusted for variables listed in the table and additionally for education, total, low and high-density cholesterol levels, high-sensitivity C-reactive protein and N-terminal pro b-type natriuretic peptide
After adjustment for cardiovascular risk factors, male sex remained strongly associated with elevated hs-cTnT (OR 6.80, 95% CI 5.36, 5.65) (Table 3). Other cardiovascular risk factors positively associated with elevated hs-cTnT were history of diabetes, older age, black race, body mass index, hypertension and hs-CRP. eGFR was inversely associated with elevated hs-cTnT.
Table 3.
Adjusted Odds Ratios (95% Confidence Intervals) for Elevated (≥14.0 ng/L) Cardiac Troponin T According to Cardiovascular Risk Factors
| Characteristic | OR | (95% CI) |
|---|---|---|
| Male (vs female) | 6.80 | (5.36, 5.65) |
| History of diabetes | 2.83 | (2.21, 3.62) |
| Age (per 5.6 years) | 1.48 | (1.34, 1.63) |
| African American (vs white) | 1.73 | (1.36, 2.20) |
| Body mass index (per 5.6 kg/m2) | 1.22 | (1.10, 1.35) |
| Hypertension | 1.48 | (1.23, 1.80) |
| hs-CRP (per 6.7 mg/L) | 1.16 | (1.08, 1.24) |
| eGFR (per 18.4 ml/min/1.73 m2) | 0.75 | (0.68, 0.83) |
Variables are expressed per 1 standard deviation unless otherwise noted.
Table shows risk factors significantly (p<0.05) associated with cTnT.
Adjusted for variables listed in the table and additionally for education, alcohol and statin use, total, low and high-density cholesterol levels and N-terminal pro b-type natriuretic peptide
Discussion
In a community-based population of 9,593 individuals without clinically evident cardiovascular disease, traditional cardiovascular risk factors were independently associated with hs-cTnT. Although many risk factors were associated with detectable hs-cTnT, sex and diabetes appeared to have a particularly robust association with hs-cTnT. Interestingly, among individuals with “ideal cardiovascular health”, 44% of persons had detectable hs-cTnT. Furthermore, two thirds of individuals with both “intermediate health” and “poor health” had either detectable or elevated hs-cTnT
Using the current conventional cTnT assay, troponin can be detected in 0.7% of participants aged 30–65 years from a population-based cohort2 and is independently associated with myocardial infarction and death21. In contrast, the high-sensitivity troponin assay used in our study detects troponin at concentration far below previous detection limits and allowed us to detect hs-cTnT in 66% of our population of middle-aged and older persons without clinically evident cardiovascular disease. Gore et al compared the 99th percentile values for hs-cTnT amongst individuals without clinical cardiovascular disease from three different population based studies, including ARIC6. They demonstrated that the 99th percentile value varies considerably with age and sex, and showed that depending on the criteria used to exclude cardiovascular disease, the 99th percentile value ranged from 14 to 36 ng/L.
In a community-based population, Wallace et al described risk factors that were associated with the detection of troponin using the currently clinical available (third generation) cardiac troponin-T assay (>10 ng/L). Troponin T was detected in 1.15% of subjects and risk factors associated with cardiac troponin-T >10 ng/L were diabetes (OR4.6), left ventricular hypertrophy (OR 5.4), kidney disease (odds ratio 20.4) and “CHF ratio” (composite of CHF, LVEF<40% or BNP>100) (OR 5.3)2. Interestingly, in contrast to our results, Wallace et al did not find that age, sex or race were independent predictors of troponin. Similar to our study, they found a strong relationship between diabetes and troponin. Also similar to our findings, increasing risk factor burden was associated troponin.
Others have demonstrated that even detectable cardiac troponin-T concentration is associated with cardiovascular morbidity and mortality among persons with22 and without3–5 cardiovascular disease. We now show that hs-cTnT is detectable among persons without traditional cardiovascular risk factors and among persons considered to be in “ideal cardiovascular heath”. Given that even detectable hs-cTnT is associated with increased cardiovascular risk, hs-cTnT may prove to be a valuable tool in the identification of individuals at risk of cardiac events that would otherwise be missed using traditional risk scoring algorithms.
Various mechanisms have been proposed to explain the detection of hs-cTnT among asymptomatic individuals: myocyte necrosis, apoptosis, myocyte turnover, by-products of troponin degradation and increase wall permeability 23. Hickman et al. proposed that troponin is released after ischemia without necrosis via blebs from cardiac myocytes 24. Finally, it is also plausible that this at least some of the hs-cTnT detected is a result of microvascular damage that is difficult to test for in a large population-based study.
Our findings may also imply that by using higher sensitivity assays to detect troponin, we may be identifying persons with cardiovascular disease of a non-atherosclerotic origin (i.e. subclinical myocardial injury), rather than identifying subjects earlier in the atherosclerotic disease process. In line with this hypothesis, we did not find an independent association between more specific risk factors for atherosclerosis (total cholesterol, LDL or HDL) in our models but found robust associations with male sex and diabetes. Furthermore, others have previously demonstrated that hs-cTnT is a better predictor of total mortality and heart failure than CHD3 and that left ventricular mass but not coronary artery calcium –a marker of coronary atherosclerosis- is independently associated with detectable levels of hs-cTnT4. These findings further support the notion that persons with detectable hs-cTnT are at increased risk of cardiovascular events most likely related primarily to a non-atherosclerotic disease mechanism.
There are several implications of our findings. First, although the robust association with male sex may be secondary to more sub-clinical cardiovascular disease among males, sex may need to be accounted for in deciding relevant clinical cut-points and reference values for the identification of persons at risk for future cardiovascular events using the high-sensitivity troponin assay. Indeed, Gore et al have proposed sex- and age- specifics 99th percentile values for hs-cTnT6. Interestingly, Saunders et al demonstrated a significant interaction between hs-cTnT and sex for the prediction of coronary heart disease events3, again suggesting that cardiac injury among females is incompletely understood. Interestingly, we observed that while African American men had higher hs-cTnT levels than Caucasian men, the same was not the case among females. Gore et al reported similar findings from the ARIC cohort, but not among participants from the Dallas Heart Study or the Cardiovascular Health Study6. This may be explained by the relatively low number of African Americans in several age and race strata. Finally, hs-cTnT is not a target for therapy but it is possible that hs-cTnT may eventually be used as a primary and/or safety endpoint in clinical trials.
Interestingly, although our findings appear to show that smokers were less likely to have detectable hs-cTnT, this may be explained by the fact that sicker individuals may have been more likely to quit smoking. Alternatively, residual confounding, potentially related to the fact that current smokers are likely younger and have less cumulative exposure (less pack-years) than past smokers. Finally, this could also signify that smoking is related to atherosclerosis but hs-cTnT is a measure of myocardial damage and not necessarily atherosclerosis mediated cardiovascular disease.
Our study has important limitations: Although we excluded persons with clinical cardiovascular disease (including persons with “silent MI” detected by electrocardiogram), we cannot rule out the possibility that some persons had underlying coronary artery disease. Furthermore, most of the African Americans in our study (88%) were from Jackson, Mississippi and thus our findings may not be generalizable to African Americans across the United States. Given the observational nature of our study, we cannot exclude the possibility of residual confounding nor can we establish temporality. Nonetheless, this represents one of the largest community-based cross-sectional studies of cardiovascular risk factors and hs-cTnT. Additional strengths of this study include the large number of females and African Americans, rigorous measurement of cardiovascular risk factors, and our ability to exclude clinical cardiovascular disease cases utilizing comprehensive and adjudicated surveillance data for clinical events.
In conclusion, in this community-based study of persons without clinically evident cardiovascular disease hs-cTnT was associated with most traditional cardiovascular risk factors. Despite this, hs-cTnT was detectable among almost half of persons with ideal cardiovascular health. Although only hypothesis generating our findings suggest that among persons considered healthy and at low cardiovascular risk by traditional risk scoring algorithms, hs-cTnT may allow for the identification of individuals not identified by other methods.
Highlights.
Using a high sensitivity assay cardiac troponin T is detectable in 66% of the population
Male sex and diabetes were strongly associated with hs-cTnT
44% of individuals with ideal cardiovascular health had detectable hs-cTnT.
Acknowledgments
Funding Sources:
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). The authors thank the staff and participants of the ARIC study for their important contributions. Dr. Rubin was supported by NIH/NHLBI grant T32HL007024 at the time of this work. This research was also supported by NIH/NIDDK grants R01DK089174 and K24DK106414 to Dr. Selvin. Dr. Coresh was supported by NIH and National Kidney Foundation.
Footnotes
Role of the Sponsor: The National Institutes of Health had no role in the collection, management, analysis, or interpretation of the data and had no role in the preparation, review, or approval of the manuscript.
Conflicts: Drs. Selvin and Ballantyne have served on a Roche Diagnostics Advisory Board. Drs. Hoogeveen and Ballantyne have received grant support from Roche Diagnostics (and the National Institutes of Health). The other authors declare no commercial conflicts of interest (but receive National Institutes of Health grant funding). Drs Ballantyne, Hoogeveen, and Nambi are co-investigators on a provisional patent (# 61721475) filed by Baylor and Roche for use of biomarkers in heart failure prediction
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Newby LK, Jesse RL, Babb JD, et al. ACCF 2012 expert consensus document on practical clinical considerations in the interpretation of troponin elevations: a report of the American College of Cardiology Foundation task force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2012;60:2427–63. doi: 10.1016/j.jacc.2012.08.969. [DOI] [PubMed] [Google Scholar]
- 2.Wallace TW, Abdullah SM, Drazner MH, et al. Prevalence and determinants of troponin T elevation in the general population. Circulation. 2006;113:1958–65. doi: 10.1161/CIRCULATIONAHA.105.609974. [DOI] [PubMed] [Google Scholar]
- 3.Saunders JT, Nambi V, de Lemos JA, et al. Cardiac troponin T measured by a highly sensitive assay predicts coronary heart disease, heart failure, and mortality in the Atherosclerosis Risk in Communities Study. Circulation. 2011;123:1367–76. doi: 10.1161/CIRCULATIONAHA.110.005264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Lemos JA, Drazner MH, Omland T, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. Jama. 2010;304:2503–12. doi: 10.1001/jama.2010.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.deFilippi CR, de Lemos JA, Christenson RH, et al. Association of serial measures of cardiac troponin T using a sensitive assay with incident heart failure and cardiovascular mortality in older adults. JAMA. 2010;304:2494–502. doi: 10.1001/jama.2010.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gore MO, Seliger SL, Defilippi CR, et al. Age- and sex-dependent upper reference limits for the high-sensitivity cardiac troponin T assay. Journal of the American College of Cardiology. 2014;63:1441–8. doi: 10.1016/j.jacc.2013.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McEvoy JW, Lazo M, Chen Y, et al. Patterns and determinants of temporal change in high-sensitivity cardiac troponin-T: The Atherosclerosis Risk in Communities Cohort Study. International journal of cardiology. 2015;187:651–7. doi: 10.1016/j.ijcard.2015.03.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McEvoy JW, Chen Y, Nambi V, et al. High-Sensitivity Cardiac Troponin T and Risk of Hypertension. Circulation. 2015;132:825–33. doi: 10.1161/CIRCULATIONAHA.114.014364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martinez-Rumayor AA, de Lemos JA, Rohatgi AK, et al. Addition of highly sensitive troponin T and N-terminal pro-B-type natriuretic peptide to electrocardiography for detection of left ventricular hypertrophy: results from the Dallas Heart Study. Hypertension. 2013;61:105–11. doi: 10.1161/HYPERTENSIONAHA.112.195289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 11.White AD, Folsom AR, Chambless LE, et al. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49:223–33. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 12.Operations Manual No. 2: Cohort Component Procedures, Version 1.0. Chapel Hill: ARIC Coordinating Center, School of Public Health, University of North Carolina; 1987. [Google Scholar]
- 13.Operations Manual No. 11: Sitting Blood Pressure, Version 1.0. Chapel Hill: ARIC Coordinating Center, School of Public Health, University of North Carolina; 1987. [Google Scholar]
- 14.National Heart, Lung, and Blood Institute. Atherosclerosis Risk in Communities Study: Manual 8: Lipid and lipoprotein determinations. Chapel Hill, NC: ARIC Coordinating Center; 1994. Version 2.0 ed. [Google Scholar]
- 15.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Operations Manual No. 10: Clinical Chemistry Determinations, Version 1.0. Chapel Hill: ARIC Coordinating Center, School of Public Health, University of North Carolina; 1987. [Google Scholar]
- 17.Chambless LE, Folsom AR, Sharrett AR, et al. Coronary heart disease risk prediction in the Atherosclerosis Risk in Communities (ARIC) study. J Clin Epidemiol. 2003;56:880–90. doi: 10.1016/s0895-4356(03)00055-6. [DOI] [PubMed] [Google Scholar]
- 18.Agarwal SK, Avery CL, Ballantyne CM, et al. Sources of variability in measurements of cardiac troponin T in a community-based sample: the atherosclerosis risk in communities study. Clinical chemistry. 2011;57:891–7. doi: 10.1373/clinchem.2010.159350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Giannitsis E, Kurz K, Hallermayer K, Jarausch J, Jaffe AS, Katus HA. Analytical validation of a high-sensitivity cardiac troponin T assay. Clinical Chemistry. 2010;56:254–61. doi: 10.1373/clinchem.2009.132654. [DOI] [PubMed] [Google Scholar]
- 20.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 21.Daniels LB, Laughlin GA, Clopton P, Maisel AS, Barrett-Connor E. Minimally elevated cardiac troponin T and elevated N-terminal pro-B-type natriuretic peptide predict mortality in older adults: results from the Rancho Bernardo Study. J Am Coll Cardiol. 2008;52:450–9. doi: 10.1016/j.jacc.2008.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McQueen MJ, Kavsak PA, Xu L, Shestakovska O, Yusuf S. Predicting myocardial infarction and other serious cardiac outcomes using high-sensitivity cardiac troponin T in a high-risk stable population. Clinical biochemistry. 2013;46:5–9. doi: 10.1016/j.clinbiochem.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 23.White HD. Pathobiology of troponin elevations: do elevations occur with myocardial ischemia as well as necrosis? J Am Coll Cardiol. 2011;57:2406–8. doi: 10.1016/j.jacc.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 24.Hickman PE, Potter JM, Aroney C, et al. Cardiac troponin may be released by ischemia alone, without necrosis. Clin Chim Acta. 2010;411:318–23. doi: 10.1016/j.cca.2009.12.009. [DOI] [PubMed] [Google Scholar]