Abstract
Objective
To synthesize qualitative evidence on linkage to care interventions for people living with HIV.
Design
Systematic literature review.
Methods
We searched nineteen databases for studies reporting qualitative evidence on linkage interventions. Data extraction and thematic analysis were used to synthesize findings. Quality was assessed using the CASP tool and certainty of evidence was evaluated using the CERQual approach.
Results
Twenty-five studies from eleven countries focused on adults (24 studies), adolescents (8 studies), and pregnant women (4 studies). Facilitators included community-level factors (i.e. task-shifting, mobile outreach, integrated HIV and primary services, supportive cessation programs for substance users, active referrals, and dedicated case management teams) and individual-level factors (encouragement of peers/family and positive interactions with healthcare providers in transitioning into care). One key barrier for people living with HIV was perceived inability of providers to ensure confidentiality as part of linkage to care interventions. Providers reported difficulties navigating procedures across disparate facilities and having limited resources for linkage to care interventions.
Conclusions
Our findings extend the literature by highlighting the importance of task-shifting, mobile outreach, and integrated HIV and primary services. Both community and individual level factors may increase the feasibility and acceptability of HIV linkage to care interventions. These findings may inform policies to increase the reach of HIV services available in communities .
Keywords: Barrier, Facilitator, HIV, Linkage to Care, Systematic Review Qualitative
Introduction
HIV is a global public health threat and a comprehensive response demands coordinated action. The results of the HPTN 052 trial [1, 2] suggest that universal testing and treatment may increase the number of people living with HIV (PLHIV) who achieve viral suppression, preventing onward transmission. However, this benefit is contingent on PLHIV being retained throughout the care continuum, including linkage to care. We define linkage to care as confirmation of HIV diagnosis and first HIV-specific clinical visit [3, 4]. Recent studies demonstrate the importance of early linkage to care and therapy initiation [5–9]. Early linkage to care may decrease HIV-associated morbidity and mortality [10, 11].
Most evaluations of linkage to care interventions have focused on quantitative assessment [5]. Although large quantitative studies have been conducted in many settings, there are many questions that quantitative methods cannot adequately address [12–16]. Qualitative research can more effectively elucidate the local factors impacting linkage to care for individuals. Social and behavioral factors are known to play a large role in the effectiveness of HIV interventions [17] and qualitative evaluations are increasingly integrated into interventions focused on promoting linkage to care [5, 18–21].
Qualitative meta-synthesis is useful in evaluating interventions for several reasons [13, 16, 22]: 1) It facilitates understanding of the mechanism of the intervention; 2) it examines acceptability and feasibility directly related to implementation; 3) it helps identify intervention adjustments to optimize impact. Our review builds on these advantages by synthesizing qualitative evidence on PLHIV and their care providers to identify facilitators and barriers to linkage to care interventions.
Methods
We conducted a systematic review of qualitative evidence of linkage to care for individuals testing positive for HIV. Following Cochrane guidelines, we conducted a comprehensive search strategy (Supplemental Table 1) to identify all relevant studies regardless of language or publication status publically available without prior date restrictions on Feb 21 2015. We developed this strategy in accordance with PRISMA guidelines and registered our study in PROSPERO (CRD42015017252). An important step in our strategy was devising a broad list search terms to encompass the scope of relevant HIV linkage to care intervention research (Supplement Table 1). We queried search terms in nineteen journal and thesis databases: CENTRAL (Cochrane Central Register of Controlled Trials), EMBASE, LILACS, PsycINFO, PubMed (MEDLINE), Web of Science/Web of Social Science, CINAHL, British Nursing Index and Archive, Social Science Citation Index, AMED (Allied and Complementary Medicine Database), DAI (Dissertation Abstracts International), EPPI-Centre (Evidence for Policy and Practice Information and Coordinating Centre), ESRC (Economic and Social Research Council), Global Health (EBSCO), Anthrosource, and JSTOR. We then checked for abstracts from Conferences on Retroviruses and Opportunistic Infections (CROI), International AIDS Conference (IAC), and alternating years of International AIDS Society (IAS) clinical meetings from their inception dates (1993, 1985 and 2001, respectively). We also contacted researchers and relevant organizations and reviewed references from all included studies.
Study inclusion criteria
Our goal was to evaluate studies that used qualitative methodology and analysis to examine interventions with an aim to improve HIV linkage to care. Intervention designs included research aimed to accelerate initiation of HIV-specific medical services and/or enhancing multiple steps within the care continuum. We identified all relevant studies from low, middle, and high-income countries. Qualitative methodologies included ethnographic research, case studies, and process evaluations. Qualitative analysis included framework analysis, thematic analysis, and content analysis. Studies using mixed methods were included if qualitative methods and findings could be extracted and analyzed.
Exclusions
Studies were excluded if they met any of the following criteria: did not report an intervention, did not examine linkage to care, did not focus on PLHIV, was comprised of only a literature review, did not use or report qualitative data. Studies that solely used quantitative methods to investigate interventions for HIV linkage were excluded, as were mixed studies that only reported on quantitative findings.
Assessment of the quality of included studies
Once relevant studies were identified, we conducted a quality assessment using a seven-question measure adapted from the CASP tool [23]. We chose this measurement because it has been used in similar studies [24, 25]. This tool evaluates study context, researcher reflexivity, sampling methods, the appropriateness of data collection methods, analysis techniques, and sufficiency of qualitative evidence (Supplement Table 2). We then used the SPICE model to review a study’s setting, perspective, intervention, comparison, and evaluation (Supplement Table 3). The SPICE model frames the systematic review question and is analogous to the PICO (population, intervention, comparison, and evaluation) model used in quantitative systematic reviews[28, 29].
Assessment of the certainty of evidence of qualitative studies
We used the CERQual approach to assess the methodological limitations, coherence, relevance, and adequacy of our review findings [27, 30]. CERQual is a tool analogous to GRADE for evaluating the confidence of review findings in qualitative systematic reviews [27, 31]. CERQual confidence levels were assigned based on an overall assessment of four scores from composite studies: methodological concern, coherence, relevance, and adequacy. Themes from studies assessed as having only minor methodological concern and high coherence, relevancy, and adequacy accordingly received high CERQual confidence. Themes from studies with major methodological concerns and low relevance or coherence scores were assigned low CERQual confidence. Themes from studies that received mixed scores across the four criteria were assigned moderate confidence.
Data extraction and synthesis for emergent themes
We used a framework thematic synthesis approach based on the theory of conceptual saturation [32, 33]. Thematic synthesis is one of the approaches [33–36] recommended by the Cochrane Qualitative Review Methods Group [31]. Data extraction was applied to primary (source data) and secondary (main findings, interpretation of data) information from original qualitative research exploring the experiences and attitudes of stakeholders towards HIV linkage interventions. We extracted the following data from reviewed studies: country of study, rural/urban locality, linkage to care definition, qualitative data types, primary data findings, elements from the CASP tool, acceptability/feasibility issues, and main findings addressed in discussion or conclusion sections. Two coders (LT, JB) examined a subset of the selected literature to harmonize data extraction. All studies were independently coded by one individual and cross-checked by a second individual. Emergent themes were identified from studies by reviewing primary and secondary data. We reviewed the data for common themes. Subanalyses among key populations, adults, adolescents, children, and pregnant women were undertaken where sufficient data was available.
Results
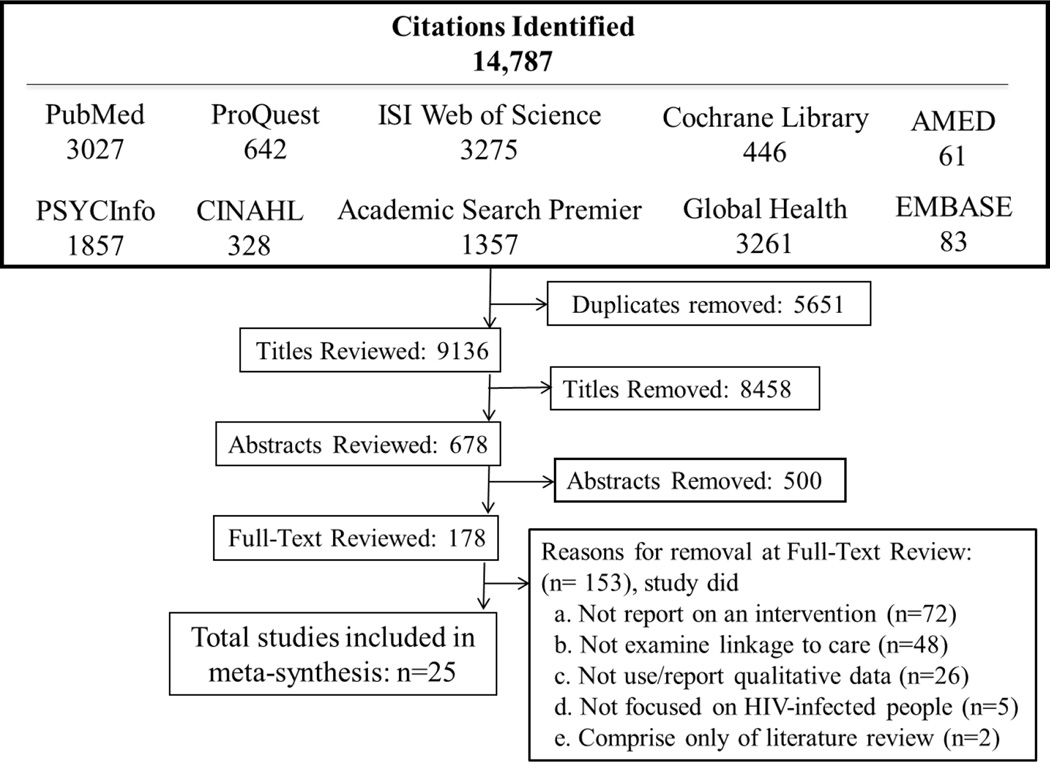
From 9136 citations, 678 abstracts were assessed for studies reporting qualitative data on linkage to care interventions (Table 1). The abstract review yielded 178 citations for a full-text review (Table 1). Of these, 175 manuscripts were excluded because they did not report on intervention (72), did not examine linkage to care (48), did not report qualitative finding (26), did not focus on PLHIV (5), or were reporting on literature reviews (2) (Table 1). We identified twenty-five manuscripts comprised of twenty-two peer-reviewed articles [18, 19, 21, 37–55], two theses/dissertations [56, 57] and one conference abstract [58] (Figure 1). Among these, seventeen studies were single component interventions [19, 21, 37–42, 45, 47, 49, 50, 53, 54, 56–58] and eight were multiple component interventions [18, 43, 44, 46, 48, 51, 52, 55]. We identified cross-sectional (16) [18, 19, 39, 41–46, 49–51, 53–55, 58], longitudinal (6) [21, 37, 47, 48, 52, 57], and longitudinal-quantitative parent studies (3) study designs [38, 40, 56]. Twelve studies [18, 37–41, 44, 47, 49–51, 53] were from high-income countries (HIC: USA, UK, Canada), eight [19, 43, 45, 46, 52, 54, 56, 58] from middle-income countries (MIC: South Africa, India, Botswana), and five [21, 42, 48, 55, 57] from low-income countries (LIC: Haiti, Tanzania, Cambodia, Malawi, Kenya). Overall, 24 studies focused on adults [18, 19, 21, 37–43, 45–58], eight included adolescents (defined as ages 10–19) [21, 37, 44–48, 57], and four included pregnant women [21, 43, 55, 57]. None included children. We identified five intervention-specific themes and ten cross-cutting themes (Table 1).
Table 1.
Full evidence profile for qualitative findings of ARV linkage-to-care for single and multiple intervention studies
| Review finding | Relevant papers |
Methodological limitations |
Coherence | Relevance | Adequacy | CERQual Confidence |
Explanation of confidence in the evidence assessment |
|---|---|---|---|---|---|---|---|
| Findings from single intervention studies | |||||||
|
(1) TASK SHIFTING: An effective way to increase linkage to care, but without proper planning can place increased burden on healthcare providers. While increasing linkage, this process can also affect continuity of care of PLHIV |
Ivers 2011; Jama 2013; Kroeger 2011; Uebel 2013 |
Overall: Minor concerns 4 minor |
Overall: High Coherence Data similar within and across studies |
Overall: Highly relevant 4 high relevance |
4 studies total (MIC, LIC); 3 countries, 2 SSA (South Africa, Botswana), 1 North America (Haiti) |
High | 4 studies in MIC and LIC in SSA and North America. Most studies of high quality with high coherence with highly relevant findings |
|
(2) COMMUNITY-BASED MOBILE OUTREACH (TESTING) and LINKAGE: based on two home-based testing and counseling interventions and one workplace-based voluntary testing and counseling intervention in rural/mining areas |
Bhagwanjee 2008; Kroeger 2011; Naik 2013 |
Overall: Minor concerns 3 minor |
Overall: High Coherent Data similar within and across studies |
Overall: Highly relevant 3 high relevance |
3 studies total (MIC); 2 SSA countries (2 South Africa, 1 Botswana) |
Moderate | 3 studies in MIC in SSA with high quality, coherence, and relevance, but downgraded confidence from high to moderate because studies are only from SSA |
|
(3) INTEGRATED CARE: Integration of HIV care into primary care services can improve linkage. Considerations of administrative barriers, provider preferences, and preferences of PLHIV for continuity with a dedicated HIV provider should be taken into account |
Johnson 2003; Uebel 2013 |
Overall: Minor to moderate concerns 1 minor 1 moderate |
Overall: Moderate coherence Data on different populations |
Overall: Moderately relevant 1 high relevance, 1 moderate relevance |
2 studies total; 2 countries (MIC, HIC), 1 SSA (South Africa), 1 North America (USA) |
Moderate | 2 total studies in MIC and HIC in SSA and North America. Varied quality of studies with medium level of coherence and relevance |
|
(4) PROVIDER INITIATED TESTING AND COUNSELING (PITC) and LINKAGE: a successful model for improving linkage, but difficult to implement on a larger scale. Many supposed PITC are actually operating at VTC |
Ferguson 2014; Macpherson 2013 |
Overall: Minor to moderate concerns 1 minor 1 moderate |
Overall: Low coherence Data on different populations |
Overall: Low relevance 1 moderate relevance, 1 low relevance |
2 studies total (LIC); 2 SSA (Kenya, Malawi) |
Low | 2 studies in LIC in SSA. Mixed study quality with low coherence and relevance |
|
(5) SUBSTANCE USE SUPPORT: successful treatment of substance use is vital to linkage to care for marginalized populations (Youth and Homeless) |
Johnson 2003; Nunn 2010 |
Overall: Minor to high concerns 1 minor 1 high |
Overall: High Coherence Data similar within and across studies |
Overall: Highly relevant 1 high relevance, 1 moderate relevance |
2 studies total; 1 country (HIC: USA) |
Moderate | 2 total studies in HIC (US). Mixed study quality, has high coherence and relevance of finding for marginalized individuals (key pops), but downgraded because findings based on marginalized populations in US |
| Findings from Multiple Intervention Studies | |||||||
|
(1) DIVERSE PROVIDER FEEDBACK reports on providers and lay healthcare workers experiences in carrying- out diverse intervention implementation. Feedback was generally positive, with many interventions reported as acceptable for providers and care workers. Three subthemes emerged from analysis of linkage to care for PLHIV: implementation process, facilitators, and barriers |
Anaya 2015; Cameron 2009; Gruber 2011; Ivers 2011; Jama 2013; Lazarus 2012; Macpherson 2013; Rajabiun 2011; Uebel 2013; White 2013 |
Overall: Minor to high concerns 6 minor 1 moderate 3 high |
Overall: High Coherence Data similar within and across studies |
Overall: Highly relevant 5 high relevance, 4 moderate relevance, 1 low relevance High Relevant |
10 studies total (LMIC, HIC); 6 countries, 4 studies North America (3 US, 1 Haiti) , 1 Europe (England), 3 SSA (2 South Africa, 1 Malawi), 2 Asia (India, Cambodia) |
High | 10 total studies from multiple countries. Mixed study quality but finding have high coherence and relevance |
|
(2) IMPLEMENTATION PROCESS: providers discussed how successful implementation of linkage to care on their part required greater clarity in coordinating the referral process across centers to improve the quality of references to other providers. At the institutional level, developing a focus on client-centered care, and devising plans to work as an administrative team for getting PLHIV linked into care were essential for successful linkage programs |
Anaya 2015; Cameron 2009; Gruber 2011; Ivers 2011; Jama 2013; Lazarus 2012; Macpherson 2013; Rajabiun 2011; Uebel 2013; White 2013 |
Overall: Minor to high concerns 6 minor 1 moderate 3 high |
Overall: High Coherence Data similar within and across studies |
Overall: Highly relevant 5 high relevance, 4 moderate, relevance 1 low relevance |
10 studies total (LMIC, HIC); 6 countries, 4 studies North America (3 US, 1 Haiti) , 1 Europe (England), 2 Asia (India, Cambodia,) 3 SSA (2 South Africa, 1 Malawi) |
High | 10 total studies from multiple countries. Mixed study quality but finding have high coherence and relevance |
|
(3) FACILITATORS: providers reported that having guidance protocols for integrated services simplified assistance in navigating complex medical system(s) for PLHIV. Simplification enabled improvement in perceptions of PLHIV for trust and knowledge of referrals. Task-shifting of care from doctors to nurses increased the range of responsibilities of CHW, thereby improving linkage to care because of elevated levels of HIV knowledge in community-wide setting. Increases in community knowledge further improved linkage to care by reducing stigma and improving family support |
Anaya 2015; Cameron 2009; Gruber 2011; Ivers 2011; Jama 2013; Rajabiun 2011; White 2013 |
Overall: Minor to high concerns 3 minor 1 moderate 3 high |
Overall: High Coherence Data similar within and across studies |
Overall: Highly Relevant 3 high relevance 4 moderate relevance |
7 studies total; 5 from LMIC and 2 HIC; 4 North America: 3 US, 1 Haiti; 1 Europe: 1 England; 1 SSA: South Africa , 1 Asia: Cambodia |
High | 7 total studies from multiple countries. Mixed study quality but finding have high coherence and relevance |
|
(4) BARRIERS TO INTERVENTIONS: need to calibrate different procedures and cultures across institutions to improve linkage to care. Lack of dedicated staff and staff shortages hindered implementation for providers. Need to integrate volunteers into existing tasks carried out by employees at medical facilities. Current WHO staging guidelines complicated integration at local levels because fulfillment and compliance to guidelines required resources not available at all clinics. Providers experienced high workload, often felt like they were gatekeepers in offering care to PLHIV as they had to subjectively choose which individuals would receive treatment. Medical professionals also discussed how task-shifting for staff can hinder HIV work – primarily, additional clinical/administrative burden for non-HIV specialized nurses in task-shifting environments were not trained to provide HIV- integrated care, so they are trained to perform care and hence uncomfortable/unwilling to do so (esp. reproductive health and youth) |
Anaya 2015; Cameron 2009; Lazarus 2012; Macpherson 2013; Uebel 2013; White 2013 |
Overall: Minor to high concerns 4 minor 2 high |
Overall: High Coherence Data similar within and across studies |
Overall: Highly Relevant 3 high relevance, 2 moderate relevance, 1 low relevance |
6 studies total (LMIC, HIC) 6 countries , 1 North America (US), 1 Europe (England), 2 SSA (Malawi, South Africa), 2 Asia (Cambodia, India) |
High | 6 total studies from multiple countries. Mixed study quality but finding have high coherence and relevance |
|
(5) CONFIDENTIALY ISSUES: participants of interventions such as workplace testing, home based testing service, comprehensive HIV centers, and VCT testing all had reported concerns about confidentiality |
Bhagwanjee 2008; Jama 2013; Kroeger 2011; Naik 2013; Sarna 2014; |
Overall: Minor to high concerns 4 minor 1 high |
Overall: High Coherence Data similar within and across studies |
Overall: Moderately Relevance 1 high relevance, 2 moderate relevance, 2 low relevance |
5 studies total (MIC); 3 countries, 2 SSA (3 South Africa, 1 Botswana), 1 Asia (India) |
Moderate | 5 studies in MIC with moderate thickness of data. High quality studies with high coherence but mixed relevance |
|
(6) REFERRALS: Active referrals preferable to non-active or no referrals: Active referrals included interventions where PLHIV particularly youths, women, and homeless, receive assistance in scheduling appointments for medical follow-up and related services (taxi vouchers, help navigating and getting enrolled in public health insurance, mental health, housing, food assistance services) after a positive HIV- test. These activities improved linkage. Non-active referrals included tester receiving HIV literature or phone numbers for HIV center, or being informed they should make an appointment for further care with no direct assistance from counselor/HIV test administrator |
Anaya 2015; Cameron 2009; Christopoulos 2013; Ferguson 2014; Garland 2011; Gruber 2011; Johnson 2003; Kroeger 2011; Macpherson 2013; Nunn 2010; Nsigaye 2009; Rajabiun 2011 |
Overall: Minor to high concerns 4 minor 2 moderate 6 high |
Overall: High Coherence Data similar within and across studies |
Overall: Moderately Relevance 2 high relevance, 7 moderate relevance, 3 low relevance |
12 studies total (LMIC, HIC); 6 countries; 7 studies North America (US), 4 SSA (Botswana, Kenya, Malawi, Tanzania), 1 Europe (England) |
High | 12 studies from LMIC and HIC. Mostly high quality studies. Moderately relevant because of subpopulations in a number of studies but highly coherent findings across studies |
|
(7) CASE MANAGEMENT and SUPPORT TEAMS FOR COORDINATED LINKAGE TO-CARE SERVICES: positive impact of having counseling and referrals, particularly in a concerted way, either from a case manager, or a multi-service one-stop center. Intervention well received by PLHIV, improving linking to Care |
Christopoulos 2009; Garland 2011; Gruber 2011; Johnson 2003; Nunn 2010; Prentice 2011; Rajabiun 2011; Sullivan 2015 |
Overall: Minor to high concerns 3 minor 1 moderate 4 high |
Overall: Low Coherence Scattered data on different populations |
Overall: Moderately Relevance 2 high relevance, 3 moderate relevance, 2 low relevance |
8 studies total (HIC); 2 North America countries: 7 US, 1 Canada |
Moderate | 8 total studies, all HIC, North America. Mixed study quality of scattered findings leading to low coherence but high relevance to HIC |
|
(8) PERSISTANT PRE-POST TEST ISSUES: Lack of knowledge, awareness, or mis- information about HIV/AIDS. Anxiety and negative feelings, fear of stigma linked to confirmation of HIV-positive status-as reasons provided for not attending follow-up especially among pregnant women and youths |
Bhagwanjee 2008; Broadhead 2012; Ferguson 2014; Garland 2011; Jama 2013; Kroeger 2011; Naik 2013; Prentice 2013; White 2013 |
Overall: Minor to high concerns 3 minor 2 moderate 4 high |
Overall: Moderate coherence Data on different populations |
Overall: Moderately Relevance 2 high relevance, 5 moderate relevance, 2 low relevance |
9 studies total (LMIC, HIC); 6 countries; 5 studies in 3 SSA (1 Botswana, 1 Kenya, 3 South Africa), 3 studies in North America (2 US, 1 Canada), 1 Asia (Cambodia) |
Moderate | 9 total studies (LMIC, HIC) with moderate relevance, coherence and quality |
|
(9) FAMILY AND PEER SUPPORT: Importance of support from close family members, friends, and peers from within one’s community. Family involvement, such as care providers contacting family members to try to enroll HIV- positive individuals, particularly pregnant women, into linkage to care for HIV primary care. While concerns of PLHIV are about disclosure, distress and conflict with partners, family, and friends, before HIV diagnosis, involvement of family and peers is vital to successful linkage after diagnosis |
Bhagwanjee 2008; Ferguson 2014; Jama 2013; Kroeger 2011; Lazarus 2012; MacPherson 2013; Naik 2013; Prentice 2011; White 2013 |
Overall: Minor to high concerns 5 minor 2 moderate 2 high |
Overall: Moderate coherence Scattered data on different populations |
Overall: Moderately Relevance 4 high relevance, 3 moderate relevance, 1 low relevance, 1 unclear |
9 studies (LMIC, HIC); 7 countries, 4 studies SSA (1 Botswana, 1 Kenya, 1 Malawi, 3 South Africa), 1 North America (Canada), 2 Asia (Cambodia, India) |
Moderate | 10 studies (LMIC/HIC) with moderate quality, relevance, and coherence. Of note, multiple subcategories in how close contacts affect linkage to care |
|
(10) IMPORTANCE OF POSITIVE INTERACTIONS WITH HEALTHCARE WORKERS AND CASE MANAGERS: client perception that a trusting relationship with linkage/referral staff emphasized by PLHIV. An HIV positive staff member or support worker advocating on behalf of PLHIV improved testing access to services for linkage to care. Negative interactions correlated with less linkage because of reduced accessibility for test results and assistance in linking to HIV services |
Cameron 2009; Ferguson 2014; Gruber 2011; Johnson 2003; Kemp 2014; Lazarus 2012; Macpherson 2013; Naik 2013; Nunn 2010; Rajabiun 2011; Sarna 2014; Sullivan 2015 |
Overall: Minor to high concerns 7 minor 2 moderate 3 high |
Overall: High Coherence Data similar within and across studies |
Overall: Moderately Relevance 3 high relevance, 8 moderate relevance, 1 unclear |
12 studies total (LMIC, HIC); 6 Countries, 4 SSA (1 Kenya, 1 Malawi, 2 South Africa), 5 North America (5 US) , 1 Europe (England) 2 Asia (2 India) |
High | 12 studies (LMIC, HIC) from 6 countries. High study quality and coherence, medium relevancy mostly due to special populations in studies |
Figure 1.
Flow of reviewed literature on HIV linkage to care interventions reporting qualitative data
Intervention Specific Themes
Task-Shifting (Four studies, CERQual high confidence)
Task-shifting was identified as effective in increasing linkage to care among PLHIV in four studies [42, 43, 45, 54]. The four studies were from Botswana, Haiti, and South Africa. Task-shifting interventions entailed any “process whereby specific tasks are moved, where appropriate, to health workers with shorter training and fewer qualifications [59],” particularly in low- and middle-income country (LMIC) settings affected by human resource shortages [60]. Task-shifting increased the range of responsibilities of community health workers, and improved linkage to care by increasing HIV knowledge in the community. This increased knowledge reduced HIV-related stigma and improved family support, both of which also facilitated linkage to care. Unfortunately, without clear administrative plans for implementation, task-shifting placed an increased burden on healthcare providers [42, 57]. Discussion with healthcare providers elaborated on how task-shifting hindered HIV work, mainly due to additional clinical/administrative burden [54]. Difficulties were exacerbated for non-HIV specialized nurses in task-shifting environments because they were not trained to provide HIV-integrated care [52, 54]. This trend was particularly salient for providers in reproductive health and staff who worked with youth populations [42, 52].
Community-based mobile outreach testing and linkage (Three studies, CERQual high confidence)
Community mobile outreach testing and linkage interventions facilitated linkage to care [19, 45, 58]. These three studies were from Botswana and South Africa. This intervention program involved implementing home-based testing and counseling [45, 58] and workplace-based voluntary testing and counseling intervention in rural/mining areas [19], with subsequent linkage to care at community health centers or on-site health services at rural worksites. Community-based programs were reported as acceptable to both PLHIV and healthcare providers as useful for improving linkage.
Integration of HIV-specific and primary medical care (Two studies, CERQual moderate confidence)
Two studies examined interventions targeting systematic, institutional coordination and integration of specialized HIV care into primary care services. These two studies were from South African and the United States. The intervention aimed to reduce costs, appointment wait times, and the total number of medical clinics necessary for linkage to care. Two studies reported that integration of HIV care into primary care services was acceptable and feasible to PLHIV and health providers. These studies identified several factors (administrative barriers, provider preferences, and patient preferences for having a dedicated HIV provider) that warrant further consideration in integration.
Provider Initiated Testing, Counseling (PITC), and Linkage (Two studies, CERQual low confidence)
PITC and linkage to care facilitated improvements in linkage to care. These two studies were from Kenya and Malawi. This intervention had healthcare providers at non HIV-specific medical centers initiate HIV testing for clients who originally scheduled medical visits for other services. One study based in pregnancy- services centers intervened by administering a qualitative survey to determine best supports (presence of social support, interactions with healthcare workers, and reduced health services costs) for linkage to care [21]. Another study evaluated two interventions using a community-based cluster randomized trial of a facility-based initiated HIV care compared to home initiation of HIV care after home self-testing [57]. These studies [21, 57] showed that PITC-linkage improved linkage to care for PLHIV, and indicated challenges in scaling-up of interventions beyond individual facilities.
Cessation support for people who use drugs to prepare for HIV linkage (Two studies, CERQual high confidence)
The impact of providing cessation support for PLHIV who use drugs as enrollment preparation was effective in facilitating linkage programs [44, 49]. These studies were from the United States. These programs targeted less-studied, marginalized populations of individuals recently released from jail [49] and young adults [50]. The main finding was that substance use cessation support is vital and a necessary precursor before effective linkage to care implementation.
Cross Cutting Themes
Diverse provider feedback for intervention implementation, facilitators, and barriers (Ten studies, CERQual high confidence)
Ten studies reported on providers’ experiences with linkage to care interventions [18, 38, 41–43, 46, 51, 54, 55, 57]. These studies were from the United States, England, Haiti, South Africa, Malawi, and Cambodia. This theme focused on synthesizing the experiences providers encountered in implementing diverse interventions across HIC and LMIC for general and key HIV populations. Three subthemes emerged, each focused on processes of implementation, facilitators for successful intervention, and barriers inhibiting linkage interventions for PLHIV.
Subtheme: intervention implementation processes (Ten studies, CERQual: high confidence)
Ten studies reported feedback about implementation processes [18, 38, 41–43, 46, 51, 54, 55, 57]. Providers discussed how successful implementation of linkage interventions required greater clarity in coordinating referrals for PLHIV between health centers.
Subtheme: intervention facilitators (Seven studies, CERQual high confidence)
Seven studies reported on intervention facilitators [18, 38, 41–43, 51, 55]. Healthcare providers reported that having guidance protocols for integrated services simplified navigation of medical systems on behalf of PLHIV. Guidance protocols also helped improve patient-physician trust and PLHIV knowledge about referral patterns [18, 38, 41–43, 51, 55].
Subtheme: barriers to interventions (Six studies, CERQual high confidence)
Six studies identified barriers to successful implementation of linkage to care interventions [18, 38, 46, 54, 55, 57]. Providers discussed how lack of dedicated staff and staff shortages hindered implementation. Studies also reported the need to integrate volunteers into existing tasks carried out by employees at medical facilities. Current WHO staging guidelines complicated integration at local levels because fulfillment of and compliance to guidelines required resources not available at all clinics [57]. Providers reported experiencing high workload, feeling like they were gatekeepers in selecting which patients would be subjectively chosen to receive treatment.
Confidentiality concerns among PLHIV (Five studies, CERQual moderate confidence)
Confidentiality concerns of PLHIV adversely influenced the effectiveness of linkage interventions [19, 43, 45, 52, 58]. These studies were from South Africa, India, and Botswana. PLHIV who initially participated in several HIV testing interventions (workplace testing, home based testing service, multiple-service or one-stop HIV care centers, and VCT testing) withdrew from subsequent linkage to care interventions because they lived near the intervention facility and feared unintended serostatus disclosure to their local community.
Referral systems (Twelve studies, CERQual high confidence)
Twelve studies reported on active referral systems [18, 21, 38–41, 44, 45, 48, 49, 51, 57], defined as provider assistance for PLHIV in scheduling appointments for medical follow-up and related services (taxi vouchers, enrollment in public health insurance, references to mental health, housing, food assistance services) after a positive HIV test. These studies were from the United States, Tanzania, England, Kenya, Botswana, and Malawi. Active referral systems and processes were effective in linking PLHIV into the care cascade, with active referrals being preferred over non-active or no referrals. Non-active referrals included tester receiving HIV literature or phone numbers for HIV center, or being informed they should make an appointment for further care with no direct assistance from a counselor. Active referral systems were feasible and acceptable to health providers and PLHIV, particularly for youths, women, and the homeless.
Case management and support teams for coordinating linkage to care services (Eight studies, CERQual moderate confidence)
Case management and support teams for coordinating linkage to care services facilitated successful linkage [39–41, 44, 49–51, 53]. Seven were from the United States and one was from Canada. This theme focused on comprehensive interventions where HIV-infected individuals had access to case managers who coordinated counseling testing, referral, and designated linkage provider teams. All eight studies were from HIC, and all reported that PLHIV and health care providers found the intervention acceptable.
Persistent pre-post intervention issues regarding anxiety, fear, and misinformation of HIV (Nine studies, CERQual moderate confidence)
Persistent issues present prior to and after linkage interventions hindered linkage to care initiatives [19, 21, 37, 40, 43, 45, 50, 55, 58]. These studies were from the South Africa, Kenya, United States, Canada, Cambodia, and Botswana. Persistent issues were defined as a lack of knowledge, awareness, or misinformation about HIV and the anxiety and fear of stigma linked to confirmation of HIV-positive status. These issues were most evident as reasons provided for not attending follow-up among pregnant women and youth.
Family and peer support (Ten studies, CERQual moderate confidence)
Ten studies evaluated the importance of support from close family members, friends, and peers from within one’s community as facilitating interventions by encouraging PLHIV to enter HIV specialized care [19, 21, 43, 45–47, 50, 55, 57, 58]. These studies were from South Africa, India, Kenya, Botswana, Malawi, United States, Canada, and Cambodia. Studies reported on how family involvement assisted care providers in contacting and enrolling PLHIV, particularly pregnant women, into linkage to care for HIV primary care [19, 21, 43, 45–47, 50, 55, 57, 58]. Another component of involvement centered on concerns about disclosure, distrust and conflict with close contacts such as partners, family and friends before HIV diagnosis.
Importance of positive interactions with health workers and case managers (Twelve studies, CERQual high confidence)
Twelve studies assessed how healthcare providers and support workers living with HIV and advocating on behalf of PLHIV improved linkage interventions [21, 38, 41, 44, 46, 49, 51–53, 56–58]. These studies were from the United States, India, England, Kenya, South Africa and Malawi. Reports emphasized the importance of perceptions among PLHIV towards providers, stressing the positive impact of having trusting relationships with providers. Negative interactions correlated with less effective linkage because PLHIV were less motivated to return for test results, hindering progression onto assistance in linking to HIV services.
Our findings extend the literature by highlighting the importance of task-shifting, mobile outreach, and integrated HIV and primary services. Both community and individual level factors may increase the feasibility and acceptability of HIV linkage to care interventions.
Discussion
We found a number of linkage to care interventions that were feasible and acceptable in low, middle, and high-income country contexts. This review expands the literature by including a formal assessment of qualitative literature [27, 60, 61], assessing potential harms of interventions, and examining human rights implications of interventions [62, 63].
We found that task shifting interventions improved linkage to care. This is consistent with a quantitative review [17] and existing WHO guidance on task shifting [42, 43, 45, 54]. Community health workers noted the importance of adequate training and institutional support to servicing diversified populations of PLHIV, including pregnant women, adolescents, teens, and other minorities to deliver linkage interventions [42–44, 52, 54, 55]. The relative low cost and limited harms associated with this type of intervention across many settings suggest that it could be scaled up in a variety of low and middle-income countries.
We found that community-based mobile outreach testing and linkage programs enhanced linkage to care [19, 45, 58]. These interventions decreased the travel barriers that often prevent prompt linkage to care [15, 40, 53]. Mobile outreach services also helped to reduce stigma associated with accessing HIV services [15, 40, 53].
We found that integrating HIV and primary care services was feasible and acceptable in a many settings in high-income countries. This finding is consistent with a small quantitative literature on HIV and primary care integration [64, 65] and found effective in high income settings [66, 67]. Several themes supported this finding (cessation support services for substance users, active referrals, and case management team counseling), highlighting the many ways in which integration could be effectively implemented [14, 17, 33–36, 39, 40, 43, 44–46, 48, 52]. Health care providers supported integrated service models because of improved navigation in coordinated team settings across several health facilities.
Several limitations should be considered in the interpretation of these findings. First, we did not identify any linkage to care interventions specifically focused on men who are known to have poor linkage [68–70]. This has been noted in the quantitative literature as well and underlines the need for greater programs focused on serving men. Second, all data was cross-sectional. The lack of multiple observations introduces recall bias and limits the inferences that can be made about changes over time.
Our study has several research implications. First, task shifting holds great promise as a scalable intervention to promote linkage to care in low, middle, and high-income countries. Given that task shifting has not been widely implemented in locations with poor linkage to care [60, 61, 66], implementation research on how best to facilitate task shifting is needed, especially in settings with poor linkage to care. Second, research on linkage to care among women, adolescents, and children should be a priority given their under-representation in linkage to care research [3, 5, 63, 65–67]. Third, as task shifting expands HIV service delivery into a wider range of settings, research on maintaining confidentiality and privacy will be important. PLHIV and health providers both identified that a lack of training in task shifting and confidentiality practices are major barriers in successful linkage to care programs [19, 21, 37, 40, 43, 45, 50, 55, 58].
HIV linkage to care interventions will be increasingly important in order to achieve the UNAIDS 90–90–90 as larger numbers of individuals receive testing and enter the continuum of care. Our review findings provide a number of policy-relevant suggestions for the design and implementation of linkage to care programs.
Supplementary Material
Table 2.
Summary of evidence-to-policy implications for qualitative findings of ARV linkage-to-care single interventions
| Intervention | Relevant papers |
Potential harms |
Feasibility | Equity & human rights considerations |
Acceptability | Evidence and research gaps |
|---|---|---|---|---|---|---|
|
(1) TASK SHIFTING: Expansion of HIV care services to other health care professionals and CHW beyond primary care doctors from centralized testing and counseling centers to regional and local community centers. Non-HIV specialist doctors and nurses, and lay health workers assist PLHIV in accessing medical care |
Ivers 2011; Jama 2013; Kroeger 2011; Uebel 2013 |
Overall low potential harm
|
Overall feasible within several low and middle income settings
|
|
|
Overall acceptable to PLHIV providers, and lay health workers
|
|
(2) COMMUNITY
BASED MOBILE OUTREACH (TESTING) and LINKAGE: home- based testing and counseling and workplace-based voluntary testing and counseling intervention in rural/mining areas, with subsequent linkage to community health centers or on-site health services at therural worksite |
Bhagwangee 2008; Kroeger 2011; Naik 2013 |
Overall low potential harm
|
Overall feasible within several low income settings
|
|
|
Overall limited acceptability to PLHIV, providers, and acceptable to lay health workers
|
|
(3) INTEGRATED
CARE: systematic, institutional coordination and integration ofspecialized HIV care into general/ primary care services, with goalof reducing costs, the total number of medical facilities to travel to, andappointment wait times necessary for PLHIV seeking medical professionals for primary care, HIV linked care, and other health related services |
Johnson 2003; Uebel 2013 |
Overall low/moderate potential harm
|
Overall feasible within high income settings
|
|
|
Overall acceptable to PLHIV, and limited acceptability to providers and lay health workers
|
|
(4) PROVIDER
INITIATED TESTING AND COUNSELING (PITC) and LINKAGE: HIV testing intervention where health care providers at non HIV-specific medical centers initiate HIV testing for clients who originally scheduled health care visit for other services, such as seeking care at voluntary testing centers, primary care centers, and antenatal care centers |
Ferguson 2014; Macpherson 2013 |
Overall low/moderate potential harm
|
Overall limited feasibility in several low- income rural contexts
|
|
|
Overall limited acceptability to PLHIV and acceptable to providers and lay health workers
|
|
(5) CESSATION
SUPPORT FOR SUBSTANCE USERS TO PREPARE HIV LINKAGE: intervention of giving PLHIV who are substance-users support to cease usage, and helping them understand the health and social benefits of entering linkage to care. Intervention was particularly useful for helping marginalized populations (Youth and Homeless) transition into linkage to care medical visits and related services |
Johnson 2003; Nunn 2010 |
Overall limited potential harm |
Overall feasible within high income settings
|
|
|
Overall acceptable to PLHIV, providers, and lay health workers
|
Acknowledgments
We thank the WHO HIV/AIDS Department and the Guangdong Provincial Centers for Skin Diseases and STI Control for their contribution and support. We would like to thank Eyerusalem Negussie and Nathan Ford of the WHO and Simon Lewin of the Norwegian Knowledge Centre for the Health Services for their support during concept development and manuscript review processes. Lai Sze Tso and Joseph D. Tucker are supported by grants (NIAID 1R01AI114310-01 and FIC 1D43TW009532-01) from the National Institutes of Health. John Best is supported by the UJMT Fogarty Fellowship (R25TW0093).
Footnotes
Competing Interests: None reported.
References
- 1.Cohen M, Chen Y, McCauley M, Gamble T, Hosseinipour M, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen M, McCauley M, Sugarman J. Establishing HIV treatment as prevention in the HIV Prevention Trials Network 052 randomized trial: An ethical odyssey. Clinical Trials. 2012;9:340–347. doi: 10.1177/1740774512443594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dombrowski J. Linkage to Care. Northwest AIDS Education and Training Center. 2013 [Google Scholar]
- 4.WHO . Chapter 6. Clinical guidelines across the continuum of care: Linking people diagnosed with HIV infection to HIV care and treatment. In: Po HIV, editor. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Geneva: 2013. Jun, [Google Scholar]
- 5.Govindasamy D, Meghij J, Negussi E, Baggaley R, Ford N, Kranzer K. Interventions to improve or facilitate linkage to or retention in pre-ART (HIV) care and initiation of ART in low- and middle-income settings - a systematic review. Journal of the International AIDS Society. 2014;17:19032. doi: 10.7448/IAS.17.1.19032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.When To start Consortium Sterne J, May M, Costagliola D, de Wolf F, Phillips A, et al. Timing of initiation of antiretroviral therapy in AIDS-free HIV-1-infected patients: a collaborative analysis of 18 HIV cohort studies. Lancet. 2009;373:1352–1363. doi: 10.1016/S0140-6736(09)60612-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siegfried N, Uthman O, Rutherford G. Optimal time for initiation of antiretroviral therapy in asymptomatic, HIV-infected, treatment-naive adults. Cochrane Database Syst Rev. 2010;17:CD008272. doi: 10.1002/14651858.CD008272.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siegfried N, Davies M, Penazzato M, Muhe L, Egger M. Optimal time for initiating antiretroviral therapy (ART) in HIV-infected, treatment-naive children aged 2 to 5 years old. Cochrane Database Syst Rev. 2013;10:CD010309. doi: 10.1002/14651858.CD010309.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ulett K, Willig J, Lin H, Routman J, Abroms S, Allison J, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS. 2009;23:41–49. doi: 10.1089/apc.2008.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geng EH, Odeny TA, Lyamuya RE, Nakiwogga-Muwanga A, Diero L, Bwana M, et al. Estimation of mortality among HIV-infected people on antiretroviral treatment in east Africa: A sampling based approach in an observational, multisite, cohort study. The Lancet HIV. 2015;2:e107–e116. doi: 10.1016/S2352-3018(15)00002-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Z, Zhao Y, Ge X, Mao Y, Tang Z, Shi CX, et al. Simplified HIV Testing and Treatment in China: Analysis of Mortality Rates Before and After a Structural Intervention. PLOS Medicine. 2015 doi: 10.1371/journal.pmed.1001874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowling A. Research Methods in Health: Investigating Health and Health Services. Buckingham: Open University Press; 2002. [Google Scholar]
- 13.Brookes D. Understanding Qualitative Research and its value in healthcare. Nursing times.net. 2007:32–33. [Google Scholar]
- 14.Bryman A. Social Research Methods. Oxford: University Press; 2001. [Google Scholar]
- 15.Greenhalgh T, Taylor R. How to read a paper: papers that go beyond numbers (qualitative research) British Medical Journal. 1997;315:740–743. doi: 10.1136/bmj.315.7110.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holloway I, Wheeler S. Qualitative Research in Nursing and Healthcare. Wiley - Blackwell: 2009. [Google Scholar]
- 17.Govindasamy D, Ford N, Kranzer K. Risk factors, barriers and facilitators for linkage to antiretroviral therapy care: a systematic review. AIDS. 2012;26:2059–2067. doi: 10.1097/QAD.0b013e3283578b9b. [DOI] [PubMed] [Google Scholar]
- 18.Anaya HD, Butler JN, Knapp H, Chan K, Conners EE, Rumanes SF. Implementing an HIV Rapid Testing-Linkage-to-Care Project Among Homeless Individuals in Los Angeles County: A Collaborative Effort Between Federal, County, and City Government. Am J Public Health. 2015;105:85–90. doi: 10.2105/AJPH.2014.302213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhagwanjee A, Petersen I, Akintola O, George G. Bridging the gap between VCT and HIV/AIDS treatment uptake: Perspectives from a mining-sector workplace in South Africa. African Journal of AIDS Research. 2008;7:271–279. doi: 10.2989/AJAR.2008.7.3.4.651. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention . Linkage to and Retention in HIV Medical Care. In: Division of HIV/AIDS Prevention NCfHA, Viral Hepatitis, Sexual Transmitted Diseases and Tuberculosis Prevention. Centers for Disease Control and Prevention, editor. HIV/AIDS. 2013. [Google Scholar]
- 21.Ferguson L, Grant AD, Lewis J, Kielmann K, Watson-Jones D, Vusha S, et al. Linking women who test HIV-positive in pregnancy-related services to HIV care and treatment services in Kenya: a mixed methods prospective cohort study. PLoS One. 2014;9:e89764. doi: 10.1371/journal.pone.0089764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hannes K. Chapter 4: Critical appraisal of qualitative research. In: Noyes J, Booth A, Hannes K, et al., editors. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. Cochrane Collaboration Qualitative Methods Group; 2011. [Google Scholar]
- 23.Critical Appraisal Skills Programme. Qualitative Appraisal Checklist for Qualitative Research. 2006 [Google Scholar]
- 24.Munro S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLOS Medicine. 2007;4:e238. doi: 10.1371/journal.pmed.0040238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carlsen B, Glenton C, Pope C. Thou shalt versus thou shalt not: a meta-synthesis of GPs’ attitudes to clinical practice guidelines. Br J Gen Pract. 2007;57:971–978. doi: 10.3399/096016407782604820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12:181. doi: 10.1186/1471-2288-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lewin S, Glenton C, Munthe-Kaas H, Carlsen B, Colvin CJ, Gülmezoglu M, et al. Using Qualitative Evidence in Decision Making for Health and Social Interventions: An Approach to Assess Confidence in Findings from Qualitative Evidence Syntheses (GRADE-CERQual) PLOS Medicine. 2015;12:e1001895. doi: 10.1371/journal.pmed.1001895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The Joanna Briggs Institute . Section 1: Introductory Information. In: The Joanna Briggs Institute, editor. Reviewers’ Manual 2011 Edition. South Australia: The University of Adelaide; 2011. p. 13. [Google Scholar]
- 29.Swedish Council of Health Technology Assessment (SBU) Evaluation and of synthesis qualitative studies using of methods analysis. Swedish Council of Health Technology Assessment; 2013. Feb, Evaluation and synthesis of qualitative studies; pp. 16–17. [Google Scholar]
- 30.Glenton C, Colvin C, Carlsen B, Swartz A, Lewin S, Noyes J, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev. 2013 Oct;:CD010414. doi: 10.1002/14651858.CD010414.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Noyes JSL. Chapter 6: Supplemental Guidance on Selecting a Method of Qualitative Evidence Synthesis, and Integrating Qualitative Evidence with Cochrane Intervention Reviews. In: Noyes J, Booth A, Hannes K, et al., editors. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. Cochrane Collaboration Qualitative Methods Group; 2011. [Google Scholar]
- 32.Booth A, Papaioannou D, Sutton A. Systematic Approaches to a Successful Literature Review. Sage Publications; 2012. [Google Scholar]
- 33.Thomas J, Harden A. Methods for the Thematic Synthesis of Qualitative Research in Systemic Reviews. BMC Med Res Methodol. 2008;8:45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haley DF, Golin CE, Farel CE, Wohl DA, Scheyett AM, Garrett JJ, et al. Multilevel challenges to engagement in HIV care after prison release: a theory-informed qualitative study comparing prisoners’ perspectives before and after community reentry. BMC Public Health. 2014;14:1253. doi: 10.1186/1471-2458-14-1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nunn A, Eng W, Cornwall A, Beckwith C, Dickman S, Flanigan T, et al. African American Patient Experiences With a Rapid HIV Testing Program in an Urban Public Clinic. Journal of the National Medical Association. 2012;104:5–13. doi: 10.1016/s0027-9684(15)30125-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quinlivan EB, Messer LC, Adimora AA, Roytburd K, Bowditch N, Parnell H, et al. Experiences with HIV Testing, Entry, and Engagement in Care by HIV-Infected Women of Color, and the Need for Autonomy, Competency, and Relatedness. AIDS Patient Care STDS. 2013;27:408–415. doi: 10.1089/apc.2012.0434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Broadhead RS, Borch C, van Hulst Y, Gauchat G, Tehrani S, Stringer KL, et al. Relying on Injection Drug Users to Access and Adhere to HIV Therapeutics: Bittersweet Lessons Using Respondent-Driven Sampling and a Peer-Driven Intervention. Journal of Drug Issues. 2012;42:127–146. [Google Scholar]
- 38.Cameron A, Lloyd L, Turner W, Macdonald G. Working across boundaries to improve health outcomes: a case study of a housing support and outreach service for homeless people living with HIV. Health Soc Care Community. 2009;17:388–395. doi: 10.1111/j.1365-2524.2008.00837.x. [DOI] [PubMed] [Google Scholar]
- 39.Christopoulos KA, Massey AD, Lopez AM, Geng EH, Johnson MO, Pilcher CD, et al. “Taking a half day at a time:” patient perspectives and the HIV engagement in care continuum. AIDS Patient Care STDS. 2013;27:223–230. doi: 10.1089/apc.2012.0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Garland PM, Valverde EE, Fagan J, Beer L, Sanders C, Hillman D, et al. HIV counseling, testing and referral experiences of persons diagnosed with HIV who have never entered HIV medical care. AIDS Educ Prev. 2011;23:117–127. doi: 10.1521/aeap.2011.23.3_supp.117. [DOI] [PubMed] [Google Scholar]
- 41.Gruber D, Campos P, Dutcher M, Safford L, Phillips K, Craw J, et al. Linking recently diagnosed HIV-positive persons to medical care: perspectives of referring providers. AIDS Care. 2011;23:16–24. doi: 10.1080/09540121.2010.498865. [DOI] [PubMed] [Google Scholar]
- 42.Ivers LC, Jerome JG, Cullen KA, Lambert W, Celletti F, Samb B. Task-shifting in HIV care: a case study of nurse-centered community-based care in Rural Haiti. PLoS One. 2011;6:e19276. doi: 10.1371/journal.pone.0019276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jama NM, Tshotsho N. Strategies for follow-up care of non-compliant HIV-positive pregnant women. African Journal for Physical, Health Education, Recreation and Dance. 2013;19:14–28. [Google Scholar]
- 44.Johnson RL, Botwinick G, Sell RL, Martinez J, Siciliano C, Friedman LB, et al. The utilization of treatment and case management services by HIV-infected youth. Journal of Adolescent Health. 2003;33:31–38. doi: 10.1016/s1054-139x(03)00158-7. [DOI] [PubMed] [Google Scholar]
- 45.Kroeger K, Taylor A, Marlow H, Fleming DT, Beyleveld V, Alwano MG, et al. Perceptions of door-to-door HIV counselling and testing in Botswana. Sahara J-Journal of Social Aspects of Hiv-Aids. 2011;8:171–178. doi: 10.1080/17290376.2011.9725001. [DOI] [PubMed] [Google Scholar]
- 46.Lazarus L, Reza-Paul S, Pasha A, Jairam S, Hafeez Ur Rahman S, O’Neil J, et al. Exploring the Role of Community-Based Peer Support in Improving Access to Care and Antiretroviral Treatment for Sex Workers in Mysore, India. Journal of HIV/AIDS & Social Services. 2012;11:152–168. [Google Scholar]
- 47.Martinez O, Carballo-Dieguez A, Ibitoye M, Frasca T, Brown W, Balan I. Anticipated and actual reactions to receiving HIV positive results through self-testing among gay and bisexual men. AIDS Behav. 2014;18:2485–2495. doi: 10.1007/s10461-014-0790-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nsigaye R, Wringe A, Roura M, Kalluvya S, Urassa M, Busza J, et al. From HIV diagnosis to treatment: evaluation of a referral system to promote and monitor access to antiretroviral therapy in rural Tanzania. J Int AIDS Soc. 2009;12:31. doi: 10.1186/1758-2652-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nunn A, Cornwall A, Fu J, Bazerman L, Loewenthal H, Beckwith C. Linking HIV-positive jail inmates to treatment, care, and social services after release: results from a qualitative assessment of the COMPASS Program. J Urban Health. 2010;87:954–968. doi: 10.1007/s11524-010-9496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Prentice T, Mill J, Archibald CP, Sommerfeldt S, Worthington C, Jackson R, et al. Aboriginal Youth Experiences of Accessing HIV Care and Treatment. Journal of HIV/AIDS & Social Services. 2011;10:395–413. [Google Scholar]
- 51.Rajabiun S, Coleman S, Drainoni ML. Keeping at-risk persons living with HIV/AIDS in care: a qualitative study of staff perspectives. Journal of HIV/AIDS & Social Services. 2011;10:120–138. [Google Scholar]
- 52.Sarna A, Sebastian M, Bachani D, Sogarwal R, Battala M. Pretreatment loss-to-follow-up after HIV diagnosis from 27 counseling and testing centers across India: Findings from a cohort study. Journal of the International Association of Providers of AIDS Care. 2014;13:223–231. doi: 10.1177/1545109712469686. [DOI] [PubMed] [Google Scholar]
- 53.Sullivan KA, Schultz K, Ramaiya M, Berger M, Parnell H, Quinlivan EB. Experiences of Women of Color with a Nurse Patient Navigation Program for Linkage and Engagement in HIV Care. AIDS Patient Care STDS. 2015;29(Suppl 1):S49–S54. doi: 10.1089/apc.2014.0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Uebel K, Guise A, Georgeu D, Colvin C, Lewin S. Integrating HIV care into nurse-led primary health care services in South Africa: a synthesis of three linked qualitative studies. BMC Health Serv Res. 2013;13:171. doi: 10.1186/1472-6963-13-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.White J, Delvaux T, Chhea C, Saramony S, Ouk V, Saphonn V. The linked response: lessons emerging from integration of HIV and reproductive health services in Cambodia. AIDS Research and Treatment. 2013;2013 doi: 10.1155/2013/504792. Article ID 504792-Article ID 504792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kemp C. Mixed-Methods Evaluation of a Novel Community-Based Support and Education Intervention for Individuals with HIV/AIDS in KwaZulu-Natal, South Africa [Master’s] Ann Arbor: University of Washington; 2014. p. 35. [DOI] [PubMed] [Google Scholar]
- 57.MacPherson P. Improving linkage into HIV care among adults in Blantyre, Malawi [Ph.D.] Ann Arbor: The University of Liverpool (United Kingdom); 2013. [Google Scholar]
- 58.Naik R, Doherty T, Jackson D, Zembe W, Feeley F. Interational AIDS Society. Kuala Lumpur, Malaysia: 2013. Client experiences and perspectives on the linkage to care following home-based HIV counseling and testing: a qualitative study in rural South Africa. [Google Scholar]
- 59.World Health Organization (WHO) Summary of methods. In: World Health Organization (WHO), editor. Task Shifting: rational redistribution of tasks among health workforce team. Global recommendations and guidelines. Geneva: 2008. p. 13. [Google Scholar]
- 60.World Health Organization (WHO) Task Shifting: rational redistribution of tasks among health workforce team. In: World Health Organization (WHO), editor. Global recommendations and guidelines. Geneva: 2008. [Google Scholar]
- 61.Callaghan M, Ford N, Schneider H. A systematic review of task-shifting for HIV treatment to care in Africa. Human Resources for Health. 2010:8. doi: 10.1186/1478-4491-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.World Health Organization (WHO) Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. HIV/AIDS. 2014 [PubMed] [Google Scholar]
- 63.World Health Organization (WHO) Chapter 4: Organization of Guidelines. Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. 2014:54–66. [PubMed] [Google Scholar]
- 64.Mapp F, Hutchinson J, Estcourt C. A systematic review of contemporary models of shared HIV care and HIV in primary care in high-income settings. Int J STD AIDS. 2015;26:991–997. doi: 10.1177/0956462415577496. [DOI] [PubMed] [Google Scholar]
- 65.Wong W, Luk C, Kidd M. Is there a role for primary care clinicians in providing shared care in HIV treatment? A systematic literature review. Sex Transm Infect. 2012;88:125–131. doi: 10.1136/sextrans-2011-050170. [DOI] [PubMed] [Google Scholar]
- 66.Okeke NL, Ostermann J, Thielman NM. Enhancing Linkage and Retention in HIV Care: a Review of Interventions for Highly Resourced and Resource-Poor Settings. Current HIV/AIDS Reports (Behavioral-Bio-Medical Interface) 2014;11:376–392. doi: 10.1007/s11904-014-0233-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liau A, Crepaz N, Lyles CM, Higa DH, Mullins MM, DeLuca J, et al. Interventions to Promote Linkage to and Utilization of HIV Medical Care Among HIV-diagnosed Persons: A Qualitative Systematic Review, 1996–2011. Aids and Behavior. 2013;17:1941–1962. doi: 10.1007/s10461-013-0435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kakalou E, Papastamopoulos V, Ioannidis P, Papanikolaou K, Georgiou O, Skoutelis A. Early HIV diagnosis through use of rapid diagnosis test (RDT) in the community and direct link to HIV care: a pilot project for vulnerable populations in Athens, Greece. J Int AIDS Soc. 2014;17:19619. doi: 10.7448/IAS.17.4.19619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Qvist T, Cowan S, Graugaard C, Helleberg M. High linkage to care in a community-based rapid HIV testing and counseling project among men who have sex with men in Copenhagen. Sex Transm Dis. 2014;41:209–214. doi: 10.1097/OLQ.0000000000000096. [DOI] [PubMed] [Google Scholar]
- 70.Yan H, Zhang R, Wei C, Li J, Xu J, Yang H, et al. A peer-led, community-based rapid HIV testing intervention among untested men who have sex with men in China: an operational model for expansion of HIV testing and linkage to care. Sex Transm Infect. 2014;90:388–393. doi: 10.1136/sextrans-2013-051397. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.