Abstract
With their transition from adverse to affluent environments, developing populations experience a rapid increase in the number of individuals with noncommunicable diseases. Here, we emphasize that developing populations are more susceptible than western populations to acquire these chronic diseases, because their genetic, cultural, and epigenetic characteristics do not match with the eagerly awaited affluent environments. In regard to this, there is an urgent need for public health organizations to reorganize current environments in developing populations so as to fit their inherited characteristics. Unfortunately, this need is neglected as an essential part of the Sustainable Development Goals that form the core of the United Nations' Post-2015 Development Agenda. Only through global collaborative efforts can the environments in developing populations be reorganized and, thereby, the emerging epidemic of noncommunicable diseases be stalled.
Introduction
Developing populations have long been troubled by poverty, malnutrition, infectious diseases, and disorders related to pregnancy and childbirth, but now face a new challenge. In only 12 years, the burden of these traditional diseases in developing populations has decreased from 49% to 38%, whereas the burden of noncommunicable diseases has increased from 40% to 51%, measured in disability-adjusted life years relative to all causes of disease. Likewise, the number of deaths due to the traditional diseases has decreased from 37% to 27%, whereas the number of deaths due to noncommunicable diseases has increased from 53% to 63% of all deaths. Most of the burden and deaths because of noncommunicable diseases are caused by cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes, together accounting for 636 million disability-adjusted life years and 23 million deaths per year. Currently, the burden of noncommunicable diseases is more than 3.5 times higher and the number of deaths due to noncommunicable diseases is more than 2.5 times higher as compared with western populations. The rapid rise of noncommunicable diseases in developing populations is projected to continue, whereas their occurrence remains stable in western populations. It is expected that the number of deaths due to noncommunicable diseases comprises 71% of all deaths in developing populations and is more than four times higher as compared with western populations in only 15 years.1–3
The rapid rise in noncommunicable diseases in developing populations is explained by their rapid transition from adverse to affluent environments. Public health organizations, supported by global collaborative efforts like the Millennium Development Goals, have made remarkable progress in restricting poverty, malnutrition, infectious diseases, and disorders related to pregnancy and childbirth. The necessity of physical activity is reduced as rural communities with manual agriculture are replaced by urban settlements with office jobs and motorized means of transportation and housekeeping. Diets are enriched as vegetables and coarse grains are replaced by refined sugars and animal fats. The affluent environments lead to obesity, dyslipidemia, hypertension, and ultimately noncommunicable diseases, such as cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes. Developing populations progress through the transition from adverse to affluent environments more rapidly than western populations.1–6
Meanwhile, it is debated to what extent public health organizations should prioritize the prevention and treatment of noncommunicable diseases in developing populations. Here, we emphasize that developing populations are more susceptible than western populations to acquire noncommunicable diseases in affluent environments, because, as a consequence of their rapid transition, their genetic, cultural, and epigenetic characteristics do not match with these new environments.
Genetic mismatch.
During most of history, humans have lived under adverse environmental conditions, whereby notably malnutrition and infectious diseases compromised survival. Because of these environmental stressors, preferentially those individuals survived who carried genetic variants benefiting efficient nutrient consumption and resistance against infections. As a result of this natural selection, humans are bestowed with genes that program thrifty and proinflammatory characteristics.7–10
Western populations have passed through a transition from adverse to affluent environments over multiple generations. This transition has minimized the burden of malnutrition and infectious diseases, improved survival of individuals with wasteful and anti-inflammatory characteristics, and consequently, relaxed the selection of genetic variants that program thrifty and proinflammatory characteristics. It is unlikely, however, that a population's genome has changed dramatically over few generations. Many individuals carry the genetic variants that have been selected to match previous adverse environments, but mismatch the current affluent environments. The thrifty and proinflammatory genetic variants expressed in an environment with abundance and hygiene contribute to noncommunicable diseases.7–10
In developing populations, the transition from adverse to affluent environments has started only recently and is completed within one generation. Here, the selection of thrifty and proinflammatory genetic variants has acted on generations up to those born today. The genetic characteristics of these populations mismatch the new affluent environments as much as in western populations, but natural selection has had even less time than in western populations to substitute mismatched genetic variants for better matching ones. Like western populations, the genetically programmed thrifty and proinflammatory characteristics of developing populations render them susceptible to noncommunicable diseases. In both types of populations, recent selection has been revealed for genetic variants that are associated with resistance against infections as well as with susceptibility to chronic inflammatory diseases including cardiovascular disease and diabetes.11
Cultural mismatch.
Cultural customs and beliefs are transmitted from generation to generation and largely influence behavior and health. The transgenerational transmission of culture is subject to evolutionary processes similarly to genes. Since the transmission of culture is dependent on the survival and reproduction of its executors, culture adapts to changes in the environment like the genes they carry.12
It has long been the cultural ideal to be corpulent and physically inactive, because these characteristics represent wealth and fitness in adverse environments where food is scarce and manual labor necessary. In western populations, after their transition to affluent environments, the ideal has changed over a few generations into a new ideal of being slim and physically active with wealthy individuals in the vanguard.13–15 The new ideal matches the new environments, in which being slim and physically active conserves health and prosperity by preventing noncommunicable diseases.
The cultures of many developing populations still embrace corpulence and physical inactivity, because they are still regarded to represent wealth, beauty, health, and fertility. Here, terms for corpulence have positive connotations and are popular names of artists and songs, whereas slimness is linked to malnutrition and infectious diseases like acquired immune deficiency syndrome (AIDS) and tuberculosis. Corpulent women are esteemed as attractive partners and suitable mothers; corpulent men are ascribed power and status. Some developing populations practice ritual fattening to prepare young women for marriage.13–15 Since the transition of these populations to affluent environments has started recently and takes place within a generation, the cultural ideal cannot adapt timely to the new environmental conditions. The ideal of corpulence and physical inactivity that has represented survival and fertility until recently now stimulates adherence to unhealthy diets and inactive lifestyles and puts developing populations at increased risk of noncommunicable diseases.
Epigenetic mismatch.
During development in the first period of life, the human genome is adjusted by environmental cues through epigenetic changes. These changes modulate the transcription and the actions of genes to maximize fitness under the expected environmental conditions during life. The epigenetic programming is attuned to the environment experienced in early life and continues to have its effects in later life.10,16
Western populations are hardly exposed to food shortage and infections early in life. Several generations have been epigenetically attuned to abundance and hygiene, which matches the affluent environments being present throughout their later lives.
In developing populations going through a rapid transition from adverse to affluent environments, all but the latest generations have been exposed to food shortage and infections early in life, whereas many more enjoy abundance and hygiene later in life. Their epigenetic adjustments, promoting thriftiness and proinflammatory characteristics, match the expected adverse environment, but mismatch the current affluent environment. When children are exposed to environmental stress before or shortly after birth, like malnutrition manifested as impaired growth, they retain health if food remains scarce throughout their lives.7 However, if food becomes abundant later in life, these children are at increased risk to develop obesity and noncommunicable diseases like cardiovascular diseases and diabetes.10,16 As a well-studied example, epigenetic adjustments have been found that explain the increased risks of noncommunicable diseases in children born during the Dutch Hunger Winter, while afterward raised in economic prosperity.17
A triple evolutionary mismatch.
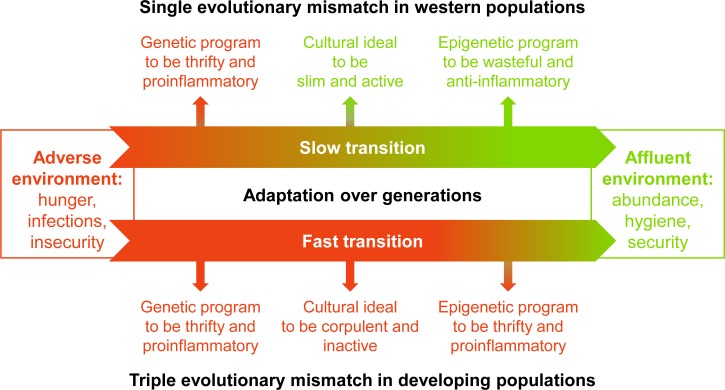
As summarized in Figure 1 , the radical transition from adverse to affluent environments elapses within a generation in developing populations, whereas it has elapsed in western populations over multiple generations. Consequently, developing populations remain not only genetically, but also culturally and epigenetically mismatched with the new affluent environments, whereas western populations have had the time to adapt culturally and epigenetically to the affluent environments. This triple evolutionary mismatch renders developing populations more susceptible to acquire noncommunicable diseases in the affluent environments than western populations, explains why noncommunicable diseases rise here to overshadow those in western populations, and affirms an urgent and increasing necessity for public health organizations to invest in the prevention of noncommunicable diseases in developing populations.
Figure 1.
A triple evolutionary mismatch in developing populations. Developing populations experience a fast transition from adverse environments (red, dark) to affluent environments (green, light) within a single generation. Western populations have experienced such a transition over multiple generations. While western populations have had the time to adapt culturally and epigenetically to the affluent environments, developing populations have had little time for adaptation and remain not only genetically, but also culturally and epigenetically mismatched with the new affluent environments. This triple evolutionary mismatch renders them more susceptible to noncommunicable diseases than western populations.
Together with a triple evolutionary mismatch, the rapid transition of developing populations has led to a coexistence of communicable and noncommunicable diseases. This so-called “double burden of disease” is widely acknowledged to contribute to the rise of noncommunicable diseases. As survival after infection has improved, human immunodeficiency virus (HIV)/AIDS, tuberculosis, and many other infectious diseases have become chronic. The chronic infections, their proinflammatory effects, and their treatments predispose to the development of noncommunicable diseases in affluent environments. For example, chronic HIV/AIDS and tuberculosis are associated with cardiovascular diseases and diabetes.18
Healthy environments.
From 2015 onward, the Millennium Development Goals are succeeded by newly formulated Sustainable Development Goals, which form the core of the United Nations' (UN) Post-2015 Development Agenda. The new goals have been adopted during a Special Summit last September. Although noncommunicable diseases are addressed with the goal to “reduce by one third premature mortality from non-communicable diseases through prevention and treatment,” the Sustainable Development Goals persist to view the eradication of poverty and hunger as the greatest global challenge, next to the combat of diseases that have long been dominant in developing populations, such as infectious diseases and disorders related to pregnancy and childbirth.19 Some have supported this prioritization, also in this journal.20 By contrast, organizations like the NCD Alliance and the Lancet NCD Action Group have endeavored after the recognition of noncommunicable diseases as an urgent threat to global health and development.6,21 Here we add evolutionary arguments to their plea.
In western populations, malnutrition, infectious diseases, and disorders related to pregnancy and childbirth have largely been brought under control by environmental interventions ensuring, for example, clean drinking water, sewage systems, and safe housing. A similar approach is needed to control noncommunicable diseases. Western populations have learnt from bitter experience how noncommunicable diseases can be prevented by a nutritionally thrifty and physically active lifestyle. Meanwhile, they have found to their cost that prevention of noncommunicable diseases after their occurrence is very difficult: despite a decennia-long encouragement of a healthy lifestyle, western populations have become more obese and sedentary. The control of noncommunicable diseases is instead pursued by better treatment, especially for cardiovascular disease. Although western populations have missed their opportunity, developing populations are at the decisive moment to adapt the newly acquired environments to their inherited characteristics, so that they can prevent what western populations attempt to treat.3,6,21,22
The mismatch between the inherited characteristics and the new affluent environments of developing populations can be minimized when these environments are reorganized to facilitate and encourage a healthy diet and physical activity in daily life. Based on the preventive knowledge and skills obtained in western populations, detailed cost-effective practicable guidelines have been written to create such environments in developing populations, for example, by the World Health Organization.3,4,22 In short, they recommend opportunities of physical exercise in the environment, campaigns and regulations to counteract advertisements and attractiveness of unhealthy diets, public education about unhealthy and healthy lifestyles, and collaborations between political, commercial, and health-care sectors as well as investments by these organizations for the prevention, screening, and treatment of noncommunicable diseases. The implementation of these guidelines is essential for the prevention of noncommunicable diseases. Global collaborative efforts like the UN's Post-2015 Development Agenda should acknowledge and support this important and urgent task of public health organizations. Only in such a way can we protect the current and future generations of developing populations from the emerging epidemic of noncommunicable diseases.
Footnotes
Authors' addresses: Jacob J. E. Koopman, Section of Gerontology and Geriatrics, Department of Internal Medicine, Leiden University Medical Center, Leiden, The Netherlands, E-mail: j.j.e.koopman@lumc.nl. David van Bodegom, Leyden Academy on Vitality and Ageing, Leiden, The Netherlands, and Section of Gerontology and Geriatrics, Department of Internal Medicine, Leiden University Medical Center, Leiden, The Netherlands, E-mail: bodegom@leydenacademy.nl. Juventus B. Ziem, Department of Clinical Laboratory Sciences, School of Medicine and Health Sciences, University for Development Studies, Tamale, Ghana, E-mail: jbziem@yahoo.com. Rudi G. J. Westendorp, Department of Public Health and Center of Healthy Aging, University of Copenhagen, Copenhagen, Denmark, and Section of Gerontology and Geriatrics, Department of Internal Medicine, Leiden University Medical Center, Leiden, The Netherlands, E-mail: westendorp@sund.ku.dk.
References
- 1.World Health Organization Global Health Estimates. 2013–2014. http://www.who.int/healthinfo/global_burden_disease/en/ Available at. Accessed December 8, 2015.
- 2.World Health Organization . Global Status Report on Noncommunicable Diseases 2014. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 3.World Bank . The Growing Danger of Non-Communicable Diseases: Acting Now to Reverse Course. Washington, DC: World Bank; 2011. [Google Scholar]
- 4.Joint WHO/FAO Expert Consultation Diet, nutrition and the prevention of chronic diseases. World Health Organ Tech Rep Ser. 2003;916:1–149. [PubMed] [Google Scholar]
- 5.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, Baugh V, Bekedam H, Billo N, Casswell S, Cecchini M, Colagiuri R, Colagiuri S, Collins T, Ebrahim S, Engelgau M, Galea G, Gaziano T, Geneau R, Haines A, Hospedales J, Jha P, Keeling A, Leeder S, Lincoln P, McKee M, Mackay J, Magnusson R, Moodie R, Mwatsama M, Nishtar S, Norrving B, Patterson D, Piot P, Ralston J, Rani M, Reddy KS, Sassi F, Sheron N, Stuckler D, Suh I, Torode J, Varghese C, Watt J. Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 7.Prentice AM, Rayco-Solon P, Moore SE. Insights from the developing world: thrifty genotypes and thrifty phenotypes. Proc Nutr Soc. 2005;64:153–161. doi: 10.1079/pns2005421. [DOI] [PubMed] [Google Scholar]
- 8.Drenos F, Westendorp RGJ, Kirkwood TBL. Trade-off mediated effects on the genetics of human survival caused by increasingly benign living conditions. Biogerontology. 2006;7:287–295. doi: 10.1007/s10522-006-9027-9. [DOI] [PubMed] [Google Scholar]
- 9.Van Bodegom D, May L, Meij HJ, Westendorp RGJ. Regulation of human life histories: the role of the inflammatory host response. Ann N Y Acad Sci. 2007;1100:84–97. doi: 10.1196/annals.1395.007. [DOI] [PubMed] [Google Scholar]
- 10.Gluckman P, Hanson M. Mismatch: The Lifestyle Diseases Timebomb. Oxford, United Kingdom: Oxford University Press; 2008. [Google Scholar]
- 11.Brinkworth JF, Barreiro LB. The contribution of natural selection to present-day susceptibility to chronic inflammatory and autoimmune disease. Curr Opin Immunol. 2014;31:66–78. doi: 10.1016/j.coi.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jablonka E, Lamb MJ. Evolution in Four Dimensions: Genetic, Epigenetic, Behavioral, and Symbolic Variation in the History of Life. Cambridge, MA: MIT Press; 2005. [Google Scholar]
- 13.Ulijaszek SJ, Lofink H. Obesity in biocultural perspective. Annu Rev Anthropol. 2006;35:337–360. [Google Scholar]
- 14.Brown PJ, Sweeney J. The anthropology of overweight, obesity and the body. AnthroNotes. 2009;30:6–12. [Google Scholar]
- 15.Scott A, Ejikeme CS, Clottey EN, Thomas JG. Obesity in sub-Saharan Africa: development of an ecological theoretical framework. Health Promot Int. 2013;28:4–16. doi: 10.1093/heapro/das038. [DOI] [PubMed] [Google Scholar]
- 16.Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359:61–73. doi: 10.1056/NEJMra0708473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tobi EW, Goeman JJ, Monajemi R, Gu H, Putter H, Zhang Y, Slieker RC, Stok AP, Thijssen PE, Müller F, van Zwet EW, Bock C, Meissner A, Lumey LH, Slagboom PE, Heijmans BT. DNA methylation signatures link prenatal famine exposure to growth and metabolism. Nat Commun. 2014;5:5592. doi: 10.1038/ncomms6592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Young F, Critchley JA, Johnstone LK, Unwin NC. A review of co-morbidity between infectious and chronic disease in Sub Saharan Africa: TB and diabetes mellitus, HIV and metabolic syndrome, and the impact of globalization. Global Health. 2009;5:9. doi: 10.1186/1744-8603-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.United Nations Transforming Our World: The 2030 Agenda for Sustainable Development. 2015. https://sustainabledevelopment.un.org/post2015/summit Available at. Accessed December 8, 2015.
- 20.Sharp D, Millum J. The post-2015 development agenda: keeping our focus on the worst off. Am J Trop Med Hyg. 2015;92:1087–1089. doi: 10.4269/ajtmh.15-0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alleyne G, Binagwaho A, Haines A, Jahan S, Nugent R, Rojhani A, Stuckler D. Embedding non-communicable diseases in the post-2015 development agenda. Lancet. 2013;381:566–574. doi: 10.1016/S0140-6736(12)61806-6. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization . Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-Resource Settings. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]