Abstract
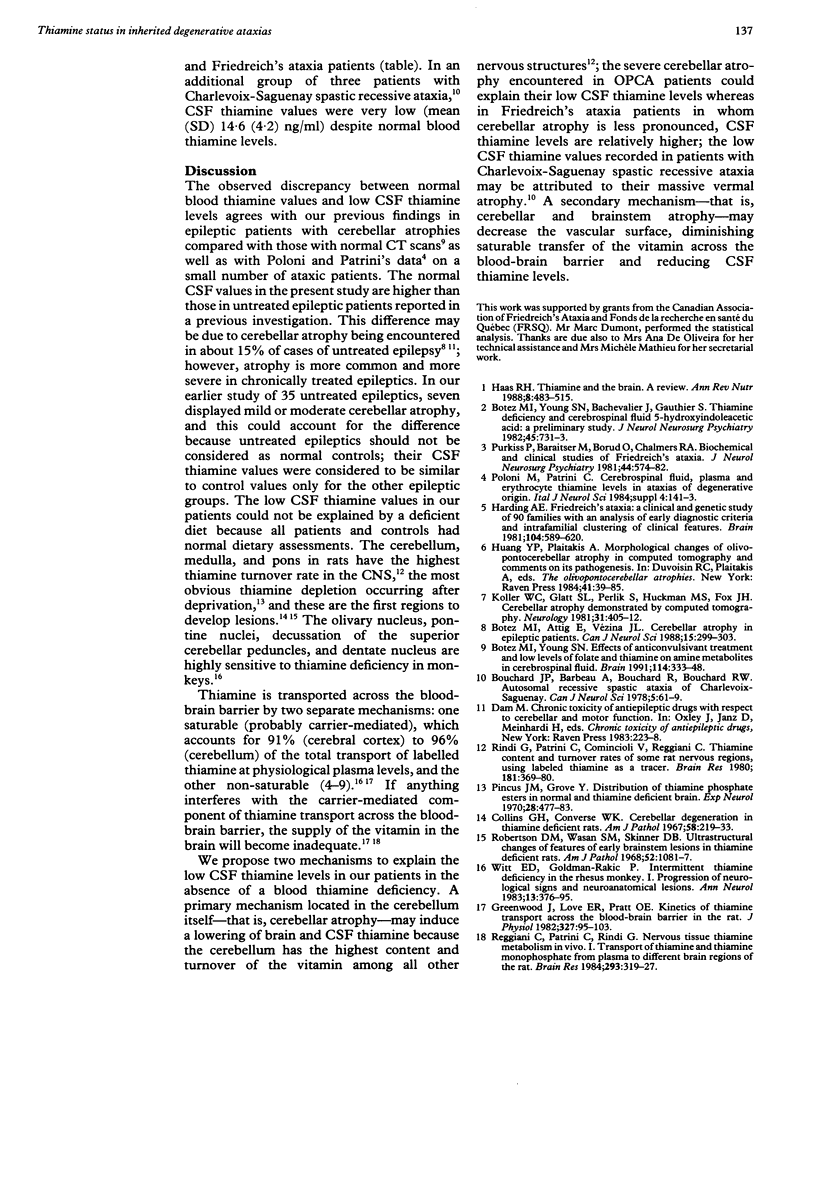
Blood thiamine levels in ataxia patients were studied. No significant differences were found between 30 patients with Friedreich's ataxia and 29 patients with olivopontocerebellar atrophy (OPCA) compared with control subjects. Both OPCA and Friedreich's ataxia patients presented significantly lower cerebrospinal fluid thiamine levels than their controls (p less than 0.001 and p less than 0.04 respectively). These results, discussed in terms of the high degree of cerebellar atrophy on CT scans in OPCA v Friedreich's ataxia patients, seem to correlate with cerebellar thiamine turnover and content.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Botez M. I., Attig E., Vézina J. L. Cerebellar atrophy in epileptic patients. Can J Neurol Sci. 1988 Aug;15(3):299–303. doi: 10.1017/s0317167100027785. [DOI] [PubMed] [Google Scholar]
- Botez M. I., Young S. N., Bachevalier J., Gauthier S. Thiamine deficiency and cerebrospinal fluid 5-hydroxyindoleacetic acid: a preliminary study. J Neurol Neurosurg Psychiatry. 1982 Aug;45(8):731–733. doi: 10.1136/jnnp.45.8.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botez M. I., Young S. N. Effects of anticonvulsant treatment and low levels of folate and thiamine on amine metabolites in cerebrospinal fluid. Brain. 1991 Feb;114(Pt 1A):333–348. [PubMed] [Google Scholar]
- Bouchard J. P., Barbeau A., Bouchard R., Bouchard R. W. Autosomal recessive spastic ataxia of Charlevoix-Saguenay. Can J Neurol Sci. 1978 Feb;5(1):61–69. [PubMed] [Google Scholar]
- Collins G. H., Converse W. K. Cerebellar degeneration in thiamine-deficient rats. Am J Pathol. 1970 Feb;58(2):219–233. [PMC free article] [PubMed] [Google Scholar]
- Greenwood J., Love E. R., Pratt O. E. Kinetics of thiamine transport across the blood-brain barrier in the rat. J Physiol. 1982 Jun;327:95–103. doi: 10.1113/jphysiol.1982.sp014222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas R. H. Thiamin and the brain. Annu Rev Nutr. 1988;8:483–515. doi: 10.1146/annurev.nu.08.070188.002411. [DOI] [PubMed] [Google Scholar]
- Harding A. E. Friedreich's ataxia: a clinical and genetic study of 90 families with an analysis of early diagnostic criteria and intrafamilial clustering of clinical features. Brain. 1981 Sep;104(3):589–620. doi: 10.1093/brain/104.3.589. [DOI] [PubMed] [Google Scholar]
- Huang Y. P., Plaitakis A. Morphological changes of olivopontocerebellar atrophy in computed tomography and comments on its pathogenesis. Adv Neurol. 1984;41:39–85. [PubMed] [Google Scholar]
- Koller W. C., Glatt S. L., Perlik S., Huckman M. S., Fox J. H. Cerebellar atrophy demonstrated by computed tomography. Neurology. 1981 Apr;31(4):405–412. doi: 10.1212/wnl.31.4.405. [DOI] [PubMed] [Google Scholar]
- Pincus J. H., Grove I. Distribution of thiamine phosphate esters in normal and thiamine-deficient brain. Exp Neurol. 1970 Sep;28(3):477–483. doi: 10.1016/0014-4886(70)90184-6. [DOI] [PubMed] [Google Scholar]
- Purkiss P., Baraitser M., Borud O., Chalmers R. A. Biochemical and clinical studies of Friedreich's ataxia. J Neurol Neurosurg Psychiatry. 1981 Jul;44(7):574–582. doi: 10.1136/jnnp.44.7.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reggiani C., Patrini C., Rindi G. Nervous tissue thiamine metabolism in vivo. I. Transport of thiamine and thiamine monophosphate from plasma to different brain regions of the rat. Brain Res. 1984 Feb 20;293(2):319–327. doi: 10.1016/0006-8993(84)91239-3. [DOI] [PubMed] [Google Scholar]
- Rindi G., Patrini C., Comincioli V., Reggiani C. Thiamine content and turnover rates of some rat nervous regions, using labeled thiamine as a tracer. Brain Res. 1980 Jan 13;181(2):369–380. doi: 10.1016/0006-8993(80)90619-8. [DOI] [PubMed] [Google Scholar]
- Robertson D. M., Wasan S. M., Skinner D. B. Ultrastructural features of early brain stem lesions of thiamine-deficient rats. Am J Pathol. 1968 May;52(5):1081–1097. [PMC free article] [PubMed] [Google Scholar]
- Witt E. D., Goldman-Rakic P. S. Intermittent thiamine deficiency in the rhesus monkey. I. Progression of neurological signs and neuroanatomical lesions. Ann Neurol. 1983 Apr;13(4):376–395. doi: 10.1002/ana.410130404. [DOI] [PubMed] [Google Scholar]



