Regulatory cytokines that target B cells
Keywords: B cell, BMP, regulatory T cell, TGF-beta
Abstract
Autoreactive B cells play a crucial role in the pathogenesis of autoimmune diseases by producing auto-antibodies and presenting antigens. Regulatory cytokines that simultaneously suppress multiple pathways have the potential to control autoreactive B cells. The generally inhibitory cytokine IL-10 may have a stimulatory effect on human B-cell survival and antibody production. TGF-β family cytokines can decrease or increase antibody production and can suppress B-cell proliferation and differentiation. In contrast to TGF-β1, which induces extensive fibrosis, TGF-β3 and bone morphogenetic protein 6 (BMP-6)/BMP-7 induce non-scarring wound healing and counteract tissue fibrosis. Therefore, TGF-β3 and BMP-6/BMP-7 may be clinically applicable as therapeutic cytokines that target B cells. Recent progress in protein engineering may enable us to generate novel biologic therapies based on TGF-β family cytokines.
Introduction
The role of autoreactive B cells has been a matter of active debate for many years. Auto-antibodies produced by autoreactive B cells contribute to chronic inflammation by binding to auto-antigens, forming immune complexes and activating antigen-presenting cells (APCs). In addition, autoreactive B cells are efficient APCs in a variety of autoimmune diseases (1–3). Therefore, autoreactive B cells are rational targets for the treatment of autoimmune diseases. The efficacy of rituximab, an anti-CD20 antibody that depletes B cells, for rheumatoid arthritis (RA) and vasculitis strongly supports this hypothesis. Although most current, non-specific immunosuppressants are accompanied with an increased risk of infection, understanding how autoreactive B cells are regulated may inform the development of novel therapeutic strategies.
Cytokines regulate nearly every aspect of immune responses. Pro-inflammatory cytokines are involved in the generalized immune dysregulation seen in systemic autoimmunity, as well as local inflammatory responses that lead to tissue injury. For example, the prominent roles of TNF-α and IL-6 have been demonstrated by the clinical efficacy of biologics in RA. Among 101 RA risk loci reported by Okada et al., at least 13 genes are related to cytokine signaling (4). The regulation of the pro-inflammatory activity of these cytokines is perceived to be mediated by anti-inflammatory and immunosuppressive cytokines. IL-4, IL-21 and B cell activating factor (BAFF) are pro-inflammatory cytokines that promote the proliferation and differentiation of B cells. Excessive production of these cytokines is common in autoimmune diseases, such as systemic lupus erythematosus (SLE) (5–7). Impaired regulatory systems have been proposed to cause the over-production of IL-4, IL-21 and BAFF (8–11).
Blockade strategies for cytokines have been demonstrated to be effective for a number of immune-mediated diseases, including RA, psoriasis and inflammatory bowel diseases. However, for systemic autoimmune diseases, such as SLE, blockade of type I interferons, of BAFF or of co-stimulation through CD28 shows only limited efficacy (12–14). It is possible that blockade of a specific pathway is not sufficient to control dysregulated immune responses in the presence of networks that link various immunological nodes. Using pleiotropic regulatory cytokines that simultaneously suppress multiple pathways may be an effective strategy for controlling systemic autoimmunity. Here, we discuss the therapeutic potential of various regulatory cytokines in terms of B-cell regulation. We describe the properties of classical regulatory cytokines and then look at the functions of recently identified regulatory cytokines.
The stimulatory capacity of IL-10 for human B cells
IL-10 and TGF-β1 are the two best-studied regulatory cytokines. In humans, IL-10 suppresses the expression of MHC class II and of co-stimulatory and adhesion molecules on monocytes. IL-10 also inhibits the production of pro-inflammatory cytokines and the activation of T cells via APCs (15, 16). Importantly, IL-10-deficient mice develop severe colitis in relation to commensal bacteria in the gut (17). Type-1 T regulatory (Tr1) cells inhibit the antigen-specific activation of autologous T cells and the development of colitis by producing IL-10 (18).
However, IL-10 does not suppress B-cell functions in some situations, and even promotes antibody production. Data from IL-10 transgenic mice, blocking IL-10 with neutralizing mAbs, and experiments using gene-targeted animals suggest that the in vivo impact of IL-10 on murine B-cell function is limited (19). In contrast, IL-10 plays a more stimulatory role for human B cells. IL-10 enhanced the survival of normal human B cells (depending on their activation state), which correlated with increased expression of the anti-apoptotic protein bcl-2 (20). Although CD46-stimulated human CD4+ T cells produce IL-10 and share some similarities with Tr1 cells, CD46-stimulated IL-10-producing cells enhanced antibody production in an IL-10-dependent manner (21). Indeed, in SLE, there is a positive correlation between serum IL-10 levels and disease severity and between the production of IL-10 and auto-antibodies by B cells (22, 23). Administration of anti-IL-10 antibody delays onset of autoimmunity in NZB/W F1 mice and improved cutaneous lesions, joint symptoms and disease activity index in SLE patients (24, 25). Although treatment with recombinant IL-10 reduced anti-ds DNA antibody production in Fas-mutated lupus prone MRL-Faslpr/lpr (MRL/lpr) mice, the effect is mediated by the inhibition of pathogenic Th1 cytokine responses (26). Notably, there is a gene polymorphism in IL-10 that up-regulates IL-10 expression and confers an increased risk for SLE in Caucasians (27). Therefore, IL-10 is not a negative regulator of B-cell activity, especially in humans.
The regulatory effect of TGF-β1 for B cells
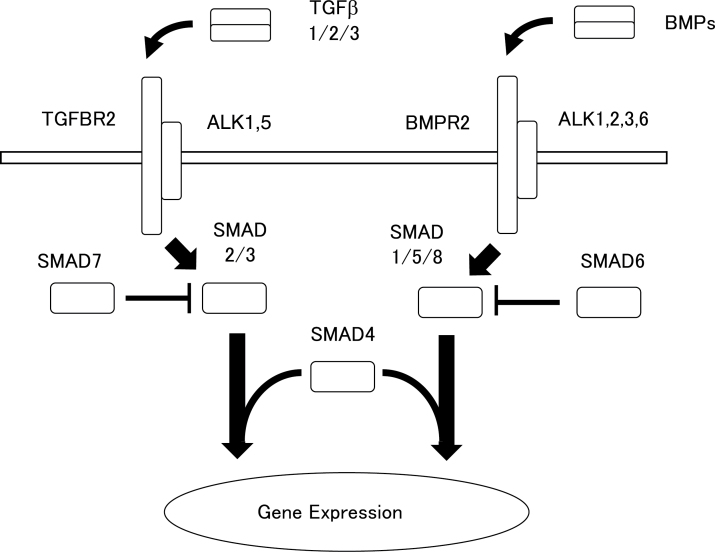
More than 40 molecules including TGF-β, bone morphogenetic proteins (BMPs) and activin/inhibin belong to TGF-β superfamily, and regulate tissue development and differentiation (28). The TGF-β subfamily comprises three members, TGF-β1, TGF-β2 and TGF-β3. The signaling pathway for TGF-β1 requires binding to a TGF-β type II receptor (TβRII) that recruits a TGF-β type I receptor (TβRI) with serine/threonine kinase activity. The phosphorylated type I receptors such as ALK1 and ALK5 phosphorylate the R-Smads (receptor-regulated Smads), which act as transcription factors activating or inhibiting selective genes. Whereas the TGFβRII–ALK5 complex activates Smad2 and Smad3, the TGFβRII–ALK1 complex activates Smad1, Smad5 and Smad8. Activated R-Smads form heteromeric complexes with the common partner Smad (co-Smad, or Smad4 in mammals) and translocate into the nucleus (Figure 1; 29). In addition to Smad-mediated transcription, TGF-β can regulate non-Smad pathways, such as Erk, p38 MAPK, NF-κB, Jun N-terminal kinase (JNK) and PI3K–Akt (30). Although TGF-β1 and TGF-β3 are both capable of binding directly to the TβRII, presentation of TGF-β2 to the receptor requires the presence of a co-receptor, beta glycan or endoglin (31).
Fig. 1.
A schematic illustration on the signaling of TGF-βs and BMPs. TGF-β family molecules bind to specific type II and type I receptors. In most cells, TGF-β binds to TGFBR2 and ALK5 (also known as TGF-β receptor-1; TGFBR1), and BMPs bind to the BMP type II receptor (BMPR2), and ALK1, ALK2, ALK3 and ALK6. Activated type I receptors induce the phosphorylation of specific receptor-regulated (R-) SMADs. In general, a TGF-β signal results in SMAD2/3 phosphorylation and a BMP signal induces SMAD1/5/8 phosphorylation. Activated R-SMADs form complexes with SMAD4 that accumulate in the nucleus to regulate the expression of target genes. SMAD6 and SMAD7 are recognized as inhibitory SMADs and antagonize the TGF-β signal by inhibiting the activation of R-SMADs.
TGF-β1 has been shown to have a wide range of effects on a variety of cell types and on immune cells in particular (32). In in vitro studies, TGF-β1 inhibited the proliferation and differentiation of effector T cells. In addition to a direct role for TGF-β1 in regulating effector T-cell function, proliferation and apoptosis, TGF-β1 signaling is required for the maintenance of forkhead box P3 (FoxP3)+CD4+CD25+ regulatory T cells (CD25+ Treg) (32). TGF-β1 induces B-cell apoptosis (33, 34) and inhibits immunoglobulin secretion and decreased surface immunoglobulin expression in stimulated human B cells (35, 36). TGF-β1 induces inhibitors of antigen receptor signaling (Ship-1, CD72) and inhibitors of the JAK–STAT pathway (SOCS1 and SOCS3) (37). Consistent with altered intracellular signaling, B-cell receptor-mediated activation of Syk and phospholipase C-2 (PLC2), as well as Stat6 phosphorylation, are inhibited by TGF-β1 (37).
Gene-targeted mice demonstrated the importance of TGF-β1 for the control of autoreactive B cells. Progressive inflammatory processes were evident in TGF-β1-deficient mice, which exhibit various autoimmune manifestations, including circulating antibodies to nuclear antigens including dsDNA, ssDNA and Sm ribonucleoprotein (38). The requirement of TGF-β1 for self-tolerance has been confirmed with a model of cell-autonomous deficiency of TGF-β1 signaling generated by the inducible disruption of TβRII using a dominant negative form of TβRII, dn-TβRII. Disruption of TβRII in hematopoietic cells results in an inflammatory infiltrate in the gut, pancreas and liver at 8–10 weeks of age (39, 40). Importantly, the absence of TβRII in B cells lead to a B-cell hyperplasia in Peyer’s patches, elevated serum immunoglobulin and production of anti-dsDNA antibody (41). Mice expressing a dn-TβRII under the control of a T-cell-specific promoter were also found to have increased immunoglobulins, particularly the levels of the T-cell-dependent IgG1 and IgG2a isotypes (42). These reports suggest that TGF-β controls humoral immunity via the suppression of both T-cell and B-cell responses.
Although a broad immune regulatory role for TGF-β1 has been established, some features of TGF-β1 inhibit its clinical application in human diseases. Accumulating evidence has demonstrated that the overexpression of TGF-β1 leads to fibrotic disease in kidney and liver (28). TGF-β1 promotes the differentiation of fibroblasts into activated myofibroblasts (43). Moreover, TGF-β1 induces the expression of extracellular matrix (ECM) proteins, including collagen I, III, IV, fibronectin, laminin and glycoproteins (44). TGF-β1 also decreases ECM degradation by inhibiting the matrix metalloproteinases that are responsible for ECM degradation (45). Adenoviral transfer of TGF-β1 to rat lung induces extensive lung fibrosis (46). In systemic sclerosis, fibrotic pathology is observed in several organs, and activated myofibroblasts, which are the main source of ECM compounds, are regulated by TGF-β1 (47). Therefore, we should be cautious before employing TGF-β1 as an immunosuppressive drug because of its pro fibrotic activity.
The pro-inflammatory role of TGF-β3 in Th17 cell differentiation
TGF-β3 was identified in 1988 (48), and decades of research have revealed the role of TGF-β3 in the development of tissues such as the heart, lung and breast. Although TGF-β1-deficient mice show severe autoimmune inflammation as mentioned above, mice lacking TGF-β3 exhibit cleft palate and die soon after birth (49). Functional studies demonstrated that while inhibition of TGF-β1 or TGF-β2 activity does not prevent normal mouse embryonic palate fusion, inhibition of TGF-β3 abrogated palate fusion. The differences observed in vivo may be due to differences in the temporal–spatial expression of individual isoforms rather than different biological activities. Nevertheless, the intrinsic differences in the biological activities of different isoforms were confirmed by the observation that TGF-β1 only partially rescued the cleft palate phenotype when TGF-β1 was knocked into the TGF-β3 locus.
Until recently, the role of TGF-β3 in immunity remained unrecognized. In 2012, Lee et al. reported that Th17 cells produce TGF-β3 and that TGF-β3-induced Th17 cells were functionally distinct from TGF-β1-induced Th17 cells (50). Moreover, TGF-β3-induced Th17 cells had a molecular signature similar to pathogenic effector Th17 cells present in autoimmune disease. Intriguingly, Th17 cells differentiated through the combination of TGF-β3 and IL-6 exhibited higher expression of the signal transducers Smad1 and Smad5 and lower expression of Smad2 and Smad3 than did those induced with TGF-β1 and IL-6. TRIM28 is a component of heterochromatin complexes that regulate IL-2 production. Chikuma et al. generated TRIM28-deficient mice and found that TRIM28-deficiency resulted in an autoimmune phenotype (51). These mice displayed enhanced Th17 cell differentiation due to derepression of TGF-β3. As the above studies indicate, the pro-inflammatory role of TGF-β3 has attracted significant attention.
TGF-β3 exerts significant control over humoral immunity
We recently identified a T-cell population that produces large amounts of TGF-β3 to regulate humoral immunity. LAG3 is a CD4 homolog that binds to MHC class II with 100-fold higher affinity than CD4 does (52). LAG3 negatively regulates T-cell homeostasis by mechanisms that are either dependent or independent of CD25+ Treg (53). We previously identified CD4+CD25–LAG3+ Treg cells (LAG3+ Treg) that produce large amounts of IL-10 (54). Transfer of LAG3+ Treg ameliorated colitis in a mouse model in an IL-10-dependent manner, indicating similarity between LAG3+ Treg and Tr1 cells. LAG3+ Treg specifically express an anergy-associated transcription factor, Egr2, which confers the phenotype of LAG3+ Treg on CD4+ T cells. Consistent with previous reports that IL-27 confers a Tr1 phenotype (55), IL-27 induces LAG3, IL-10 and Egr2 expression in CD4+ T cells in a Blimp-1-dependent manner (56, 57).
The idea of Egr2-mediated control of autoimmunity is supported by the observation that mice deficient for Egr2 in T cells and B cells develop a systemic autoimmune disease (58). Moreover, we found that Egr2 is a genetic risk factor for SLE and RA in a case–control association study (59). These results suggest that LAG3+ Treg are associated with the control of systemic autoimmunity. In fact, LAG3+ Treg were able to suppress disease progression and anti-dsDNA antibody production in Fas-mutated MRL/lpr mice, although transfer of CD25+ Treg failed to ameliorate disease (60). Furthermore, LAG3+ Treg strongly suppressed antibody production and the development of follicular helper T (TFH) cells and germinal center B cells (GCB) in 3-nitro-4-hydroxyphenyl acetic acid- conjugated chicken ovalbumin (NP-OVA)-immunized mice in an Egr2-dependent manner. These and other studies highlight the ability of LAG3+ Treg to regulate humoral immunity.
We next attempted to identify the mechanism responsible for the regulatory activity of LAG3+ Treg. IL-10 was not required for LAG3+ Treg-mediated suppression of antibody production. We focused on TGF-β3 because LAG3+ Treg express high levels of TGF-β3 mRNA, and not TGF-β1 and TGF-β2 mRNA, as assessed by microarray analysis and quantitative PCR. TCR stimulation induced high levels of TGF-β3, but no TGF-β1 or TGF-β2, in LAG3+ Treg culture supernatants. Blockade of TGF-β3 cancelled the suppressive activity of LAG3+ Treg in MRL/lpr mice and NP-OVA-immunized mice. Therefore, the suppressive activity of LAG3+ Treg is dependent mostly on TGF-β3 (60).
Because CD25+ Treg produce only limited amounts of TGF-β1, TGF-β3 could be the major source of TGF-β activity in murine CD4+ T cells. We are now evaluating the regulatory activity of TGF-β3 in a mouse model of SLE. Administration of a pCAGGS vector expressing TGF-β3, and not TGF-β1, in MRL/lpr mice significantly suppressed the production of anti-dsDNA antibody and nephritis progression (data not shown). Furthermore, TGF-β3-treated mice showed reduced development of TFH and GCB in the spleen. These observations also suggest a previously unrecognized regulatory activity of TGF-β3 for B cells.
Similarity and differences between TGF-β1 and TGF-β3
Alignment of the amino acid sequences of the three mammalian TGF-β isoforms demonstrates that the different isoforms share a high level of homology between the active domains; TGF-β3 is 86% similar to TGF-β1 (31). Although TGF-β1 and TGF-β3 are both capable of binding directly to the TGFβRII, TGF-β3 has been found to exhibit isoform-specific biological activity (31, 61). Hall et al. genetically exchanged the coding sequence of the mature TGF-β1 with the active domain from TGF-β3 using targeted recombination to create chimeric TGF-β1/TGF-β3 knock-in mice (TGF-β1 Lβ3 mice) (62). Unlike TGF-β1 –/– mice, the TGF-β1 Lβ3 mice exhibit neither embryonic lethality nor multiorgan inflammation, suggesting that knock-in of the TGF-β3 active domain prevented the vasculogenesis and autoimmunity associated with TGF-β1 deficiency. However, the TGF-β1 Lβ3 mice have a significantly shortened lifespan, probably because of tooth and bone defects, showing that the TGF-β homologues are not completely interchangeable.
One of the most striking differences between TGF-β1 and TGF-β3 is in cutaneous scarring (63). Mammalian embryos were reported to heal with no signs of scarring and complete restitution of the normal architecture of the skin with high levels of TGF-β3 expression and low levels of TGF-β1 and TGF-β2 expression (64). Exogenous addition of recombinant TGF-β3 or neutralization of TGF-β1 and/or TGF-β2 in cutaneous wounds reduced scarring and markedly improved the architecture of the neodermis in rodent models (65).
Moreover, TGF-β3 also improves scarring in humans (66). In a phase I/II study, recombinant human TGF-β3, avotermin, promoted the regeneration of healthy skin and improved scar appearance compared with controls. When low doses are injected locally around the time of surgery, avotermin is well tolerated. In accordance with this trial, TGF-β3 administered to rat lungs using transient overexpression by an adenovirus vector initiated profibrotic effects similar to those elicited by TGF-β1, but caused less severe and progressive changes. TGF-β3 does not induce fibrotic tissue repair by inhibiting matrix degradation as TGF-β1 does. Furthermore, TGF-β3 is able to down-regulate TGF-β1-induced fibrosis-associated gene expression (46). Therefore, TGF-β3, which induces ‘normal wound healing’, may be well tolerated in clinical applications as an immunosuppressant.
BMPs regulate B cells via Smad1 and Smad5
BMPs are members of the TGF-β superfamily that mediate their effects by binding to type I and type II BMP receptors. BMPs play significant roles during embryonic development, where they regulate cell growth, differentiation and apoptosis of various cell types. Whereas the TGF-βs are secreted in an inactive form containing latency-associated peptide, BMPs are secreted in their active form. In myoblasts, BMP-7 induces Smad1 and Smad5 phosphorylation by signaling through ALK1 receptor and differentiation inhibitor 1 (Id1), while Smad2 and Smad3 phosphorylation is impaired (Figure 1; 67).
In accordance with the similarity of receptor and intracellular signaling with TGF-β, BMP signaling has been reported to inhibit B-cell responses (68, 69). Human B cells express BMP type I and type II receptors and BMP-6 shows anti-proliferative effect both in naive and memory B cells (68). Co-culture with BMPs inhibited the CD40L/IL-2-induced production of IgM, IgG and IgA by human naive and memory B cells (69). BMPs also induce the phosphorylation of Smad1/Smad5/Smad8 in B cells. In particular, BMP-7 inhibits DNA synthesis and counteracts the viability-promoting effects of CD40L, whereas BMP-6 mainly inhibits plasmablast differentiation by suppressing the expression of XBP1, which is required for plasma cell differentiation. In animal models of renal fibrosis, BMP-7 exhibits a protective effect by antagonizing TGF-β1 activity (70). Intraperitoneal administration of BMP-7 induced higher Smad1 phosphorylation and reverted renal fibrosis after unilateral ureteral obstruction (71). Although the cellular source of BMPs in immune system has not been clarified, BMPs are expressed in the thymus, bone marrow, kidney and lung (72). Therefore, BMPs have the potential to affect the central and peripheral tolerance of T cells and B cells. These results suggested that BMPs are potent suppressors of naive and memory B cells in humans.
A therapeutic strategy using immunocytokines
The therapeutic potential of recombinant cytokines is often limited by the incidence of severe toxicities, even at low doses, thus preventing dose escalation to achieve an adequate concentration at target organs. Immunocytokines are antibody–cytokine fusion proteins designed for the treatment of cancer and immune-mediated disease. In terms of immunosuppression, IL-10 and IL-4 have been utilized to generate immunosuppressive immunocytokines (73). The antibody F8 targets the extra domains A of fibronectin and reacts with neovascular structures at sites of inflammation. A fusion protein of F8 and IL-10, F8-IL10 (dekavil; Philogen S.p.A., Siena, Italy), has been shown to inhibit progression of collagen-induced arthritis in mice (74, 75) and is currently in a phase I clinical trial for RA. A fusion protein of F8 and IL-4, F8-IL4, was able to selectively localize to arthritis sites and cured 100% of treated mice with established arthritis (76).
Thus, immunocytokines may be an effective strategy to target immune cells, and TGF-β3 and BMP-6/BMP-7 may be candidates for the future development of novel immunocytokines. Since TGF-β requires processing with proteases or integrins in order to produce fully active mature peptides, TGF-β-based immunocytokines may be useful for the control of inflamed organs with enhanced expression of proteases or integrins. Activated B cells including autoreactive B cells may be effectively targeted by TGF-β3 and BMP-6/BMP-7, because these B cells possibly express proteases and integrins. Although their relatively short half-life might preclude TGF-βs and BMPs from clinical application, modification of their protein structure may overcome this shortcoming.
Conclusions
Several recent reports have investigated regulatory cytokines that suppress B-cell activity. TGF-β3 and BMP-6/BMP-7 share some favorable features that suggest they may be effective for clinical application. Progress in antibody engineering has led to the generation of many different types of antibodies that differ in size and shape, including bispecific antibodies and immunocytokines. Future protein drugs seem likely to be more extensively engineered to improve their performance. Generating recombinant immunocytokines or induction of regulatory cytokines in vivo may hold great promise for controlling autoreactive B cells and autoimmune diseases.
Conflict of interest statement: K.Y. received financial support or fees from AbbVie, Astellas, BMS, Daiichi-Sankyo, MitsubishiTanabe, Pfizer, Sanofi, Santen, Takeda, Teijin., Boehringer Ingelheim, Chugai, Eisai, Ono, Taisho Toyama,UCB., ImmunoFuture, Asahi Kasei, and Janssen. K.F. received financial support or fees from Astellas, BMS, Daiichi-Sankyo, MitsubishiTanabe, Pfizer, Santen, Takeda, Chugai, Eisai, Taisho Toyama and UCB, and Janssen. All other authors declare no competing financial interests.
Funding
Ministry of Health, Labour and Welfare, Ministry of Education, Culture, Sports, Science and Technology KAKENHI Grant-in-Aid for Scientific Research (S) (23229007); Grant-in-Aid for Scientific Research (B) (24390252); Grant-in-Aid for Scientific Research (C) (25461493). The part of this work was supported by grant from The Cell Science Research Foundation and Bristol-Myers Squibb (BMS).
References
- 1. Yan J. Harvey B. P. Gee R. J. Shlomchik M. J. and Mamula M. J. 2006. B cells drive early T cell autoimmunity in vivo prior to dendritic cell-mediated autoantigen presentation. J. Immunol. 177:4481. [DOI] [PubMed] [Google Scholar]
- 2. Bouaziz J. D., Yanaba K., Venturi G. M., et al. 2007Therapeutic B cell depletion impairs adaptive and autoreactive CD4+ T cell activation in mice. Proc. Natl Acad. Sci. USA 104:20878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Giles J. R. Kashgarian M. Koni P. A. and Shlomchik M. J. 2015. B cell-specific MHC class II deletion reveals multiple nonredundant roles for B cell antigen presentation in murine lupus. J. Immunol. 195:2571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Okada Y., Wu D., Trynka G., et al. 2014. Genetics of rheumatoid arthritis contributes to biology and drug discovery. Nature 506:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cheema G. S. Roschke V. Hilbert D. M. and Stohl W. 2001. Elevated serum B lymphocyte stimulator levels in patients with systemic immune-based rheumatic diseases. Arthritis Rheum. 44:1313. [DOI] [PubMed] [Google Scholar]
- 6. Eilertsen G. Ø. Van Ghelue M. Strand H. and Nossent J. C. 2011. Increased levels of BAFF in patients with systemic lupus erythematosus are associated with acute-phase reactants, independent of BAFF genetics: a case-control study. Rheumatology (Oxford) 50:2197. [DOI] [PubMed] [Google Scholar]
- 7. Elkon K. B. and Wiedeman A. 2012. Type I IFN system in the development and manifestations of SLE. Curr. Opin. Rheumatol. 24:499. [DOI] [PubMed] [Google Scholar]
- 8. Zheng Y., Chaudhry A., Kas A., et al. 2009. Regulatory T-cell suppressor program co-opts transcription factor IRF4 to control T(H)2 responses. Nature 458:351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Elbeldi-Ferchiou A., Ben Ahmed M., Smiti-Khanfir M., et al. 2011. Resistance to exogenous TGF-beta effects in patients with systemic lupus erythematosus. J. Clin. Immunol. 31:574. [DOI] [PubMed] [Google Scholar]
- 10. Leonardo S. M. De Santis J. L. Malherbe L. P. and Gauld S. B. 2012. Cutting edge: in the absence of regulatory T cells, a unique Th cell population expands and leads to a loss of B cell anergy. J. Immunol. 188:5223. [DOI] [PubMed] [Google Scholar]
- 11. Vogelzang A., McGuire H. M., Liu S. M., et al. 2014. IL-21 contributes to fatal inflammatory disease in the absence of Foxp3+ T regulatory cells. J Immunol. 192:1404. [DOI] [PubMed] [Google Scholar]
- 12. Petri M., Wallace D. J., Spindler A., et al. 2013. Sifalimumab, a human anti-interferon-alpha monoclonal antibody, in systemic lupus erythematosus: a phase I randomized, controlled, dose-escalation study. Arthritis Rheum. 65:1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stohl W., Hiepe F., Latinis K. M., et al. 2012. Belimumab reduces autoantibodies, normalizes low complement levels, and reduces select B cell populations in patients with systemic lupus erythematosus. Arthritis Rheum. 64:2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Furie R., Nicholls K., Cheng T. T., et al. 2014. Efficacy and safety of abatacept in lupus nephritis: a twelve-month, randomized, double-blind study. Arthritis Rheumatol. 66:379. [DOI] [PubMed] [Google Scholar]
- 15. Allavena P., Piemonti L., Longoni D., et al. 1998. IL-10 prevents the differentiation of monocytes to dendritic cells but promotes their maturation to macrophages. Eur. J. Immunol. 28:359. [DOI] [PubMed] [Google Scholar]
- 16. Fujio K. Okamura T. and Yamamoto K. 2010. The Family of IL-10-secreting CD4+ T cells. Adv. Immunol. 105:99. [DOI] [PubMed] [Google Scholar]
- 17. Kuhn R. Lohler J. Rennick D. Rajewsky K. and Muller W. 1993. Interleukin-10-deficient mice develop chronic enterocolitis. Cell 75:263. [DOI] [PubMed] [Google Scholar]
- 18. Groux H. Bigler M. de Vries J. E. and Roncarolo M. G. 1998. Inhibitory and stimulatory effects of IL-10 on human CD8+ T cells. J. Immunol. 160:3188. [PubMed] [Google Scholar]
- 19. Moore K. W. de Waal Malefyt R. Coffman R. L. and O’Garra A. 2001. Interleukin-10 and the interleukin-10 receptor. Annu. Rev. Immunol. 19:683. [DOI] [PubMed] [Google Scholar]
- 20. Levy Y. and Brouet J. C. 1994. Interleukin-10 prevents spontaneous death of germinal center B cells by induction of the bcl-2 protein. J. Clin. Invest. 93:424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fuchs A. Atkinson J. P. Fremeaux-Bacchi V. and Kemper C. 2009. CD46-induced human Treg enhance B-cell responses. Eur. J. Immunol. 39:3097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Llorente L., Zou W., Levy Y., et al. 1995. Role of interleukin 10 in the B lymphocyte hyperactivity and autoantibody production of human systemic lupus erythematosus. J. Exp. Med. 181:839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hagiwara E. Gourley M. F. Lee S. and Klinman D. K. 1996. Disease severity in patients with systemic lupus erythematosus correlates with an increased ratio of interleukin-10:interferon-gamma-secreting cells in the peripheral blood. Arthritis Rheum. 39:379. [DOI] [PubMed] [Google Scholar]
- 24. Ishida H. Muchamuel T. Sakaguchi S. Andrade S. Menon S. and Howard M. 1994. Continuous administration of anti-interleukin 10 antibodies delays onset of autoimmunity in NZB/W F1 mice. J. Exp. Med. 179:305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Llorente L., Richaud-Patin Y., Garcia-Padilla C., et al. 2000. Clinical and biologic effects of anti-interleukin-10 monoclonal antibody administration in systemic lupus erythematosus. Arthritis Rheum. 43:1790. [DOI] [PubMed] [Google Scholar]
- 26. Yin Z., Bahtiyar G., Zhang N., et al. 2002. IL-10 regulates murine lupus. J. Immunol. 169:2148. [DOI] [PubMed] [Google Scholar]
- 27. Sakurai D., Zhao J., Deng Y., et al. 2013. Preferential binding to Elk-1 by SLE-associated IL10 risk allele upregulates IL10 expression. PLoS Genet. 9:e1003870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Munoz-Felix J. M. Gonzalez-Nunez M. and Lopez-Novoa J. M. 2013. ALK1-Smad1/5 signaling pathway in fibrosis development: friend or foe? Cytokine Growth Factor Rev. 24:523. [DOI] [PubMed] [Google Scholar]
- 29. ten Dijke P. and Arthur H. M. 2007. Extracellular control of TGFbeta signalling in vascular development and disease. Nat. Rev. Mol. Cell Biol. 8:857. [DOI] [PubMed] [Google Scholar]
- 30. Mu Y. Gudey S. K. and Landström M. 2012. Non-Smad signaling pathways. Cell Tissue Res. 347:11. [DOI] [PubMed] [Google Scholar]
- 31. Laverty H. G. Wakefield L. M. Occleston N. L. O’Kane S. and Ferguson M. W. 2009. TGF-beta3 and cancer: a review. Cytokine Growth Factor Rev. 20:305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rubtsov Y. P. and Rudensky A. Y. 2007. TGFbeta signalling in control of T-cell-mediated self-reactivity. Nat. Rev. Immunol. 7:443. [DOI] [PubMed] [Google Scholar]
- 33. Warner G. L. Ludlow J. W. Nelson D. A. Gaur A. and Scott D. W. 1992. Anti-immunoglobulin treatment of murine B-cell lymphomas induces active transforming growth factor beta but pRB hypophosphorylation is transforming growth factor beta independent. Cell Growth Differ. 3:175. [PubMed] [Google Scholar]
- 34. Lømo J. Blomhoff H. K. Beiske K. Stokke T. and Smeland E. B. 1995. TGF-beta 1 and cyclic AMP promote apoptosis in resting human B lymphocytes. J. Immunol. 154:1634. [PubMed] [Google Scholar]
- 35. Briskin M. Kuwabara M. D. Sigman D. S. and Wall R. 1988. Induction of kappa transcription by interferon-gamma without activation of NF-kappa B. Science 242:1036. [DOI] [PubMed] [Google Scholar]
- 36. Kehrl J. H. Thevenin C. Rieckmann P. and Fauci A. S. 1991. Transforming growth factor-beta suppresses human B lymphocyte Ig production by inhibiting synthesis and the switch from the membrane form to the secreted form of Ig mRNA. J. Immunol. 146:4016. [PubMed] [Google Scholar]
- 37. Roes J. Choi B. K. and Cazac B. B. 2003. Redirection of B cell responsiveness by transforming growth factor beta receptor. Proc. Natl Acad. Sci. USA 100:7241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Letterio J. J., Geiser A. G., Kulkarni A. B., et al. 1996. Autoimmunity associated with TGF-beta1-deficiency in mice is dependent on MHC class II antigen expression. J. Clin. Invest. 98:2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Levéen P., Larsson J., Ehinger M., et al. 2002. Induced disruption of the transforming growth factor beta type II receptor gene in mice causes a lethal inflammatory disorder that is transplantable. Blood 100:560. [DOI] [PubMed] [Google Scholar]
- 40. Aoki C. A., Borchers A. T., Li M., et al. 2005. Transforming growth factor beta (TGF-beta) and autoimmunity. Autoimmun. Rev. 4:450. [DOI] [PubMed] [Google Scholar]
- 41. Cazac B. B. and Roes J. 2000. TGF-beta receptor controls B cell responsiveness and induction of IgA in vivo. Immunity 13:443. [DOI] [PubMed] [Google Scholar]
- 42. Gorelik L. and Flavell R. A. 2000. Abrogation of TGFbeta signaling in T cells leads to spontaneous T cell differentiation and autoimmune disease. Immunity 12:171. [DOI] [PubMed] [Google Scholar]
- 43. Kelly M. Kolb M. Bonniaud P. and Gauldie J. 2003. Re-evaluation of fibrogenic cytokines in lung fibrosis. Curr. Pharm. Des. 9:39. [DOI] [PubMed] [Google Scholar]
- 44. Eikmans M. Baelde J. J. de Heer E. and Bruijn J. A. 2003. ECM homeostasis in renal diseases: a genomic approach. J. Pathol. 200:526. [DOI] [PubMed] [Google Scholar]
- 45. Leask A. and Abraham D. J. 2004. TGF-beta signaling and the fibrotic response. FASEB J. 18:816. [DOI] [PubMed] [Google Scholar]
- 46. Ask K., Bonniaud P., Maass K., et al. 2008. Progressive pulmonary fibrosis is mediated by TGF-beta isoform 1 but not TGF-beta3. Int. J. Biochem. Cell Biol. 40:484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Morris E., Chrobak I., Bujor A., et al. 2011. Endoglin promotes TGF-β/Smad1 signaling in scleroderma fibroblasts. J. Cell. Physiol. 226:3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Derynck R., Lindquist P. B., Lee A., et al. 1988. A new type of transforming growth factor-beta, TGF-beta 3. EMBO J. 7:3737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Proetzel G., Pawlowski S. A., Wiles M. V., et al. 1995. Transforming growth factor-beta 3 is required for secondary palate fusion. Nat. Genet. 11:409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lee Y., Awasthi A., Yosef N., et al. 2012. Induction and molecular signature of pathogenic TH17 cells. Nat. Immunol. 13:991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Chikuma S. Suita N. Okazaki I. M. Shibayama S. and Honjo T. 2012. TRIM28 prevents autoinflammatory T cell development in vivo. Nat. Immunol. 13:596. [DOI] [PubMed] [Google Scholar]
- 52. Baixeras E., Huard B., Miossec C., et al. 1992. Characterization of the lymphocyte activation gene 3-encoded protein. A new ligand for human leukocyte antigen class II antigens. J. Exp. Med. 176:327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Workman C. J. and Vignali D. A. 2005. Negative regulation of T cell homeostasis by lymphocyte activation gene-3 (CD223). J. Immunol. 174:688. [DOI] [PubMed] [Google Scholar]
- 54. Okamura T., Fujio K., Shibuya M., et al. 2009. CD4+CD25-LAG3+ regulatory T cells controlled by the transcription factor Egr-2. Proc. Natl Acad. Sci. USA 106:13974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Awasthi A., Carrier Y., Peron J. P., et al. 2007. A dominant function for interleukin 27 in generating interleukin 10-producing anti-inflammatory T cells. Nat. Immunol. 8:1380. [DOI] [PubMed] [Google Scholar]
- 56. Iwasaki Y., Fujio K., Okamura T., et al. 2013. Egr-2 transcription factor is required for Blimp-1-mediated IL-10 production in IL-27-stimulated CD4+ T cells. Eur. J. Immunol. 43:1063. [DOI] [PubMed] [Google Scholar]
- 57. Heinemann C., Heink S., Petermann F., et al. 2014. IL-27 and IL-12 oppose pro-inflammatory IL-23 in CD4+ T cells by inducing Blimp1. Nat. Commun. 5:3770. [DOI] [PubMed] [Google Scholar]
- 58. Zhu B., Symonds A. L., Martin J. E., et al. 2008. Early growth response gene 2 (Egr-2) controls the self-tolerance of T cells and prevents the development of lupuslike autoimmune disease. J. Exp. Med. 205:2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Myouzen K., Kochi Y., Shimane K., et al. 2010. Regulatory polymorphisms in EGR2 are associated with susceptibility to systemic lupus erythematosus. Hum. Mol. Genet. 19:2313. [DOI] [PubMed] [Google Scholar]
- 60. Okamura T., Sumitomo S., Morita K., et al. 2015. TGF-β3-expressing CD4+CD25(-)LAG3+ regulatory T cells control humoral immune responses. Nat. Commun. 6:6329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Taya Y. O’Kane S. and Ferguson M. W. 1999. Pathogenesis of cleft palate in TGF-beta3 knockout mice. Development 126:3869. [DOI] [PubMed] [Google Scholar]
- 62. Hall B. E., Wankhade U. D., Konkel J. E., et al. 2013. Transforming growth factor-β3 (TGF-β3) knock-in ameliorates inflammation due to TGF-β1 deficiency while promoting glucose tolerance. J. Biol. Chem. 288:32074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ferguson M. W. and O’Kane S. 2004. Scar-free healing: from embryonic mechanisms to adult therapeutic intervention. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 359:839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Whitby D. J. and Ferguson M. W. 1991. The extracellular matrix of lip wounds in fetal, neonatal and adult mice. Development 112:651. [DOI] [PubMed] [Google Scholar]
- 65. Shah M. Foreman D. M. and Ferguson M. W. 1995. Neutralisation of TGF-beta 1 and TGF-beta 2 or exogenous addition of TGF-beta 3 to cutaneous rat wounds reduces scarring. J. Cell Sci. 108 (Pt 3):985. [DOI] [PubMed] [Google Scholar]
- 66. Ferguson M. W., Duncan J., Bond J., et al. 2009. Prophylactic administration of avotermin for improvement of skin scarring: three double-blind, placebo-controlled, phase I/II studies. Lancet 373:1264. [DOI] [PubMed] [Google Scholar]
- 67. Scherner O. Meurer S. K. Tihaa L. Gressner A. M. and Weiskirchen R. 2007. Endoglin differentially modulates antagonistic transforming growth factor-beta1 and BMP-7 signaling. J. Biol. Chem. 282:13934. [DOI] [PubMed] [Google Scholar]
- 68. Kersten C. Sivertsen E. A. Hystad M. E. Forfang L. Smeland E. B. and Myklebust J. H. 2005. BMP-6 inhibits growth of mature human B cells; induction of Smad phosphorylation and upregulation of Id1. BMC Immunol. 6:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Huse K., Bakkebø M., Oksvold M. P., et al. 2011. Bone morphogenetic proteins inhibit CD40L/IL-21-induced Ig production in human B cells: differential effects of BMP-6 and BMP-7. Eur. J. Immunol. 41:3135. [DOI] [PubMed] [Google Scholar]
- 70. Zeisberg M., Hanai J., Sugimoto H., et al. 2003. BMP-7 counteracts TGF-beta1-induced epithelial-to-mesenchymal transition and reverses chronic renal injury. Nat. Med. 9:964. [DOI] [PubMed] [Google Scholar]
- 71. Sato M. Muragaki Y. Saika S. Roberts A. B. and Ooshima A. 2003. Targeted disruption of TGF-beta1/Smad3 signaling protects against renal tubulointerstitial fibrosis induced by unilateral ureteral obstruction. J. Clin. Invest. 112:1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Passa O. Tsalavos S. Belyaev N. N. Petryk A. Potocnik A. J. and Graf D. 2011. Compartmentalization of bone morphogenetic proteins and their antagonists in lymphoid progenitors and supporting microenvironments and functional implications. Immunology 134:349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Ferrari M. Onuoha S. C. and Pitzalis C. 2015. Trojan horses and guided missiles: targeted therapies in the war on arthritis. Nat. Rev. Rheumatol. 11:328. [DOI] [PubMed] [Google Scholar]
- 74. Schwager K., Kaspar M., Bootz F., et al. 2009. Preclinical characterization of DEKAVIL (F8-IL10), a novel clinical-stage immunocytokine which inhibits the progression of collagen-induced arthritis. Arthritis Res. Ther. 11:R142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Doll F. Schwager K. Hemmerle T. and Neri D. 2013. Murine analogues of etanercept and of F8-IL10 inhibit the progression of collagen-induced arthritis in the mouse. Arthritis Res. Ther. 15:R138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Hemmerle T. Doll F. and Neri D. 2014. Antibody-based delivery of IL4 to the neovasculature cures mice with arthritis. Proc. Natl Acad. Sci. USA 111:12008. [DOI] [PMC free article] [PubMed] [Google Scholar]