Abstract
Introduction:
Compared to the majority of non-Hispanic white (“white”) cigarette smokers, many African American smokers demonstrate a later age of initiation. The goal of the present study was to examine African American late-onset smoking (ie, regular smoking beginning at age 18 or later) and determine whether late-onset (vs. early-onset) smoking is protective in terms of quit rates and health outcomes.
Methods:
We used data from the National Survey of Midlife Development in the United States (MIDUS) because the wide age range of participants (20–75 at baseline) allowed the examination of smoking cessation and mortality incidence across the lifespan.
Results:
Consistent with previous research, results indicated a later average age of smoking onset among African Americans, compared to whites. Disentangling effects of race from age-of-onset, we found that the cessation rate among late-onset African American smokers was 33%, whereas rates for early-onset African American smokers and early- and late-onset white smokers ranged from 52% to 57%. Finally, results showed that among white, low-socioeconomic status (SES) smokers, the hazard rate for mortality was greater among early- versus late-onset smokers; in contrast, among African American smokers (both low- and high-SES) hazard rates for mortality did not significantly differ among early- versus late-onset smokers.
Conclusions:
Although late (vs. early) smoking onset may be protective for whites, the present results suggest that late-onset may not be similarly protective for African Americans. Tobacco programs and regulatory policies focused on prevention should expand their perspective to include later ages of initiation, in order to avoid widening tobacco-related health disparities.
Implications:
This study indicates that late-onset smoking is not only the norm among African American adult smokers, but that late- versus early-onset smoking (ie, delaying onset) does not appear to afford any benefits for African Americans in terms of cessation or mortality. These results suggest that prevention and intervention efforts need to consider individual groups (not just overall averages) and that tobacco control efforts need to be targeted beyond the teenage years. Tobacco programs and regulatory policies focused on prevention should expand their perspective to include later ages of initiation, to avoid widening tobacco-related health disparities.
Introduction
Compared to other racial/ethnic groups, African Americans have the highest mortality rates for coronary heart disease and stroke1,2 and suffer higher incidence and mortality rates from lung cancer than any other population in the United States.3 One factor linked with these racial health disparities is different patterns for health-undermining behavior, such as smoking.4 Research suggests that, compared to non-Hispanic whites (whites), African Americans tend to have a different smoking pattern across the age continuum. Specifically, during early adolescence, smoking prevalence is lower among African Americans than whites, but during late adolescence and early adulthood, smoking initiation rates in African Americans begin to rise.5,6 By the time individuals are in their late 20s and early 30s, greater onset among African Americans and greater cessation among whites causes the prevalence of African American smoking to equal—and often exceed—that of whites.4,6–8 This pattern is varyingly referred to as a “crossover”9,10 or “convergence” in smoking.11,12
Many factors may explain this racial convergence in smoking. For example, African Americans may have fewer resources to quit smoking.12 Factors such as peer substance use,13 parent tobacco use,14 targeted advertising,15 and discrimination16–20 may also differentially influence initiation among African Americans. One useful framework for conceptualizing the potential pathways is Moolchan’s model of factors influencing tobacco use throughout the life-span.21 This model assumes the nature of the relations between predictive factors and tobacco-use factors will vary across populations (eg, whites and African Americans). Also integral to the model is the recognition that the factors influencing use may affect people differentially across the lifecourse. For example, sources of stress (eg, discrimination, low wage work) can increase during early adulthood.
Recent findings suggest that age-of-onset itself may be a culturally-specific predictor of smoking persistence: Kandel and colleagues6 found that among whites, persistence of smoking declines with increasing age-of-onset. However, among African Americans, persistence of smoking increases with increasing age-of-onset. Thus, their findings suggest that smoking age-of-onset has opposite effects on smoking persistence among white and African American smokers.
Implications of the Racial Convergence in Smoking
Although all cigarette smoking is harmful, African American late-onset smoking is often assumed to be safer than early-onset smoking (all other factors being equal, a delay in onset should be protective against dependence and mortality). Yet the racial convergence has two important implications for how researchers and policy-makers should conceptualize African American smoking. First, it implies African American smokers are at greater risk than white smokers to remain smoking throughout adulthood and, thereby, forgo the health benefits that come from quitting.22–24 Thus, although African Americans have lower smoking prevalence than whites during their adolescence and early 20s, African Americans lose their “advantage” as they approach their 30s. Studies that examine only young samples (which identify African American race/culture as a protective factor25) are misleading, because they do not account for changes over the lifecourse. Likewise, studies that examine only lifetime smoking, rather than current smoking, are misleading, because they do not account for the greater rates of smoking cessation among whites in adulthood.
The second implication is that prevailing assumptions about smoking onset and duration may not be true for all subpopulations. Rather, notions of the “at risk” window need to be extended, because a substantial proportion of African Americans (as well as other racial/ethnic groups26) initiate smoking in their early 20s rather than during adolescence. These later ages of onset are well beyond the target of most prevention policies and programs. Furthermore, Kandel’s work6 described above would suggest that although delaying onset may be an effective strategy for reducing prevalence among whites, it may not be effective for African Americans.
Limitations to the Previous Work
All previous work on the racial convergence in smoking has examined only average trajectories for each race (eg, the African American smoking trajectory7), rather than trajectory groups within a race (eg, early- and late-onset African American smokers). Conversely, a separate line of research27,28 has investigated different onset groups, but has undertaken this work collapsing across race. Both of these lines of research essentially confound race and smoking behavior. Thus, although research has identified the African American late-onset smoking trajectory, knowledge is incomplete regarding how African American late-onset smoking differs relative to other African American smoking groups (eg, early-onset smokers) and relative to other racial/ethnic late-onset groups (eg, whites).
Along similar lines, there remains incomplete information about the relation between African American late-onset smoking and health outcomes. Although findings indicate that later smoking onset reduces the likelihood of nicotine dependence among whites,29,30 there is some evidence that late initiation does not have this benefit for African Americans.20,31 The findings are consistent with the racial convergence in smoking, as well as health disparities more generally. Thus, although late-onset (compared to early-onset) smoking appears to be protective for whites in terms of quit rates and health outcomes, more work is needed to examine whether or not it is similarly protective for African Americans.
Study Overview
Compared to the white majority, many African Americans demonstrate a unique smoking trajectory, marked by a later age-of-onset and greater continuance into mid-adulthood. In fact, late-onset smokers comprise such a sizable proportion of African American smokers that they are a critical group to understand. Moolchan’s model21 led us to postulate that the factors surrounding early-onset smoking for whites will not necessarily be the same as those surrounding late-onset smoking for African Americans. Therefore, the goal of the present study was to examine African American late-onset smoking in terms of its characteristic features and determine whether late-onset (compared to early-onset) smoking is protective in terms of quit rates and health outcomes.
Data came from the National Survey of Midlife Development in the United States (MIDUS32,33), a national survey developed to study age-related differences in physical and mental health. The wide age range of participants (20–75 at baseline and 28–84 at follow-up) allowed us to compare cessation and mortality incidence across the lifespan.
Our first hypothesis was that we would find late-onset smoking to be more prevalent among African Americans than whites. Our second hypothesis was that cessation rates would be particularly low among the late-onset African American smokers (compared to early- and late-onset white smokers and early-onset African American smokers). Finally, our third hypothesis was that late-onset African American smokers would present different characteristics than late-onset white smokers. In particular, we expected late-onset (compared to early-onset) smoking would not be as protective (in terms of age-of-mortality) for African Americans as it was for whites. For these analyses, it was important to also account for differences in socioeconomic status (SES), so that race and SES were not confounded. Rather, we sought to examine the interactions between race and SES, and expected that the protective effects of high SES and late-onset (compared to early-onset) smoking would be more pronounced among whites. We also conducted exploratory analyses to examine whether people classified into different smoking categories differed on other demographic measures (eg, gender).
Methods
Participants
The original MIDUS participants were recruited between 1995 to 1996 (referred to here as T1). All eligible participants were non-institutionalized, English-speaking adults in the contiguous US. Participants were recontacted approximately 10 years later for a follow-up between 2004 to 2006 (referred to here as T2). Of the original 7108 T1 participants, 4963 (70%) were successfully recontacted and participated at T2. Excluding those who were confirmed deceased at T2, retention rates were higher among whites (vs. African Americans), high (vs. low) SES individuals, and women (vs. men); retention rates were highest among quitters and lowest among early-onset smokers (all Ps < .001; for more thorough discussion of MIDUS attrition see Radler and Ryff34). Data were excluded for participants who had missing data for the variable “smoking category” (n = 197; see measures section). After these reductions, a final sample of 4766 was available; the majority of analyses were conducted on this sample of 4766 respondents who participated at T2. When indicated, mortality analyses alternatively used a larger sample (N = 5236) that included participants who were confirmed deceased by T2 (see measures section for more details).
Measures
The MIDUS survey included an initial 30-minute phone interview and was followed by self-administered questionnaires (SAQs) mailed to individuals who completed the phone interview. For the present article, items of interest derived from the phone interview because it had a better response rate.
Smoking Category
At T1, participants who reported ever regularly smoking cigarettes (“Have you ever smoked cigarettes regularly—that is, at least a few cigarettes every day?”) were asked the age at which they began smoking regularly. Individuals were also asked how old they were when they had their very first cigarette, and ever-regular-smokers were asked how old they were the last time they smoked cigarettes regularly. Responses to these items were used to classify individuals into four groups: Nonusers included both lifetime abstainers and never-regular-smokers; Quitters included ever-regular-smokers who had not smoked within the last 2 years; all other ever-regular-smokers (“current smokers”) were coded as either Early-Onset Smokers (those who began regular smoking before age 18) or Late-Onset Smokers (those who began regular smoking at age 18 or later). To be classified as a quitter (rather than an early- or late-onset smoker), participants also needed to report not smoking regularly at T2. Smoking category status was coded as missing (n = 197) if T1 smoking information was missing/incomplete, if T1 and T2 responses conflicted (eg, discrepancies in recalled age-of-onset that varied by >1 year) and/or if responses indicated that smoking initiation occurred between assessments (eg, reporting never-use at T1 but regular smoking at T2—the majority of these participants were over age 30 at T1).
Period-of-Onset
Several analyses were focused only on differences between early- versus late-onset smokers. Therefore, a separate construct, “period-of-onset,” was created based off of the preceding variable (smoking category) but excluding nonusers and quitters.
Ever-Regular-Smoking
For analyses examining ever-regular-smoking, quitters were re-classified as either early-onset or late-onset smokers, based on the age they began smoking regularly.
Maximum Packs per Day
At T2, participants were asked “On average, about how many cigarettes did you smoke per day during the one year in your life when you smoked most heavily?” (“open response”). To calculate maximum packs/d, this number of cigarettes smoked/d was divided by 20.
Other Tobacco Use
At T2, all participants were asked “Have you ever smoked a pipe or cigars, or used snuff or chewing tobacco regularly during your life?” (yes, no).
Age
Participant-reported date of birth at T1 was used to compute age.
Race/Ethnicity
The MIDUS questionnaire at T2 was more in line with current recommendations for assessing Americans’ cultural backgrounds in terms of both race (eg, white, African American) and ethnicity (Hispanic/Latino or non-Hispanic/Latino). Therefore, T2 reports of race/ethnicity were used when available, but were supplemented with responses at T1. Ultimately, race/ethnicity was coded as: African American (non-Hispanic), Asian, Hispanic/Latino, Native American/Alaska Native, Multiracial, white (non-Hispanic), or other.
Socioeconomic Status
Education at T1 was used as a proxy for SES. It was coded dichotomously as high school or less and some college or more.
Other Demographic Characteristics
Additional T1 variables of interest included gender, whether participants were currently married, and whether they had any children.
Morbidity
We used overall self-rated health as our health/morbidity outcome. Self-rated health was measured at T2 with a single item: “In general, would you say your physical health is excellent, very good, good, fair, or poor?” Responses were dichotomized into good health (excellent, very good, and good) and poor health (fair and poor).
Mortality
All-cause mortality information was confirmed by the National Death Index (available at www.cdc.gov/nchs/ndi.htm). Year of death was included with this information; by subtracting year of birth from year of death, we were also able to approximate age of death.
Analyses
Analyses began with descriptive statistics to characterize cigarette use in the sample. For our first hypothesis, independent samples t tests and chi-square were used to examine racial differences in mean age-of-onset and smoking category prevalence. For our second hypothesis, chi-square tests and logistic regression were used to examine racial differences in cessation among ever-regular-smokers; analysis of variance was also used to test among current smokers whether maximum packs/d differed by smoking category. All significant interactions were followed up with a series of simple effects analyses.35
For our third hypothesis (tested using just the white and African American participants), we began with chi-square tests to examine whether individuals in different smoking categories differed on demographic factors and morbidity. Next, to examine the effects of race, period-of-onset, and SES on mortality, we used Cox proportional hazards models36 with age as the time scale. In this survival analysis framework, the event of interest is mortality, and the independent variables are race, period-of-onset, and SES. We used the Cox model rather than the logistic model to account for survival time and censoring information. We used age (rather than time since T1) as the time scale to directly account for the substantial impact of age on mortality, thereby adjusting for its confounding effect.37,38 The parameter estimated from a Cox model is the hazard rate, which is the likelihood of experiencing an event in a given time period, conditional on surviving to that time period. We first ran a main effects model, which tested the simple main effects of race, period-of-onset, and SES; we next ran models that added two-way interactions. Finally, we tested the three-way, Race × Period-of-Onset × SES interaction of interest.
Results
This sample was 54% female, with a mean baseline age of 46.6 (SD = 12.5, range: 20–75). Table 1 provides further descriptive statistics. For the full sample (all races/ethnicities included), 22.5% of adults were coded as current smokers. Current smokers reported smoking an average of 1.3 packs/d during their heaviest year and 14.8% reported ever using other tobacco products. African American and white current smokers did not differ significantly by age (P > .8).
Table 1.
Participant Characteristics (N = 4766)
| Characteristics | Mean (SD) or N (%) |
|---|---|
| Age | 46.6 (12.5) |
| Gender (Female) | 2531 (53%) |
| Race/ethnicity | |
| African American (non-Hispanic) | 215 (4.5%) |
| Asian or Pacific Islander | 29 (0.6%) |
| Hispanic/Latino | 145 (3.0%) |
| Multiracial | 18 (0.4%) |
| Native American | 56 (1.2%) |
| Other race | 57 (1.2%) |
| White | 4245 (89.1%) |
| Educationa | |
| Low | 1652 (34.7%) |
| High | 3106 (65.2%) |
| Educationa by race | |
| African Americans—low | 95 (44.2%) |
| Whites—low | 1453 (34.2%) |
| African Americans—high | 120 (55.8%) |
| Whites—high | 2785 (65.6%) |
aLow education = high school or less; high education = some college or more.
Hypothesis 1: Late-Onset Smoking Prevalence
As expected, African American, compared to white, current smokers had a later age-of-onset, both when looking at age of first cigarette [M age = 16.9 vs. 15.6; t(995) = −2.03, P = .04] and age of beginning to smoke regularly [M age = 21.6 vs. 18.9; t(57.6) = −2.50, P = .015, equal variance not assumed].
Table 2 provides the distribution of adults in each smoking category among African Americans and whites. Providing further support for our hypothesis of race-based differences in smoking onset, chi-square analyses indicated a relation between smoking category and race (χ2 = 15.9, P = .001). African Americans, compared to whites, had a lower prevalence of quitters and early-onset smokers, but a higher prevalence of late-onset smokers (19.5% of all African Americans vs. 12.8% of all whites). Subsequent analyses indicated that although African Americans, compared to whites, had a somewhat lower prevalence of ever-regular-smoking, the difference was not statistically significant (P = .14). Among all African American ever-regular-smokers, 66% were late-onset, whereas among all white ever-regular-smokers, 60% were late-onset. Among all African American current smokers, 75% were late-onset, whereas among all white current smokers, 58% were late-onset.
Table 2.
Distribution of the Sample and its Morbidity and Mortality Characteristics Across the Four Smoking Categories, By Race (African Americans and Whites)
| Nonusers | Quitters | Early-onset | Late-onset | |
|---|---|---|---|---|
| Overall % in each smoking categorya | ||||
| African American | 55.3 | 18.6 | 6.5 | 19.5 |
| White | 50.3 | 27.4 | 9.4 | 12.8 |
| % in poor health at Time 2b | ||||
| African American | 50.0 | 13.6 | 9.1 | 27.3 |
| White | 35.2 | 29.5 | 15.4 | 19.8 |
| Mean (SD) age of deathc | ||||
| African American | 57.7 (12.2) | 58.7 (18.9) | 65.3 (7.8) | 58.7 (11.7) |
| White | 67.6 (11.0) | 69.6 (9.3) | 62.9 (11.1) | 65.9 (10.7) |
a P < .01 for the chi-square on Race × Smoking Category.
b P < .05 for the chi-square on Race × Smoking Category.
c P > .2 for the analysis of variance on Race × Smoking Category; this analysis was run on those who died during the study period, and thus results are conditional on mortality occuring during the study period.
Hypothesis 2: Cessation Rates
When examining ever-regular-smokers who had been late-onset, we found quitting prevalence was much lower among African Americans than whites (33.3% vs. 57.2%; χ2 = 13.9, P < .001). The same was not true for early-onset smokers: When examining ever-regular-smokers who had been early-onset, we found no difference in quitting prevalence between African Americans and whites (56.3% vs. 52.0%; χ2 = 0.2, P = .64). A similar effect was found using a logistic regression to predict quit status among African American and white ever-regular-smokers: There was a significant Race × Period-of-Onset interaction (P = .003), such that quit rates were particularly low among late-onset African Americans (this analysis controlled for age and gender).
This low rate of cessation among late-onset African Americans does not appear to be due to group-based differences in smoking heaviness. Specifically, in a Race × Period-of-onset analysis of variance predicting maximum packs/d among current smokers, packs/d was, in fact, significantly greater among early-onset smokers, compared to late-onset smokers [F(1, 622) = 28.3, P < .001], and marginally greater among white, compared to African American smokers [F(1, 622) = 3.5, P = .06].
Hypothesis 3: Characterizing Late-Onset African American Smokers
Among white current-smokers, education (our proxy for SES) was lower among early- compared to late-onset smokers (χ2 = 15.7, P < .001); however, there was no significant education difference among African American early- and late-onset smokers (P > .63). Likewise, among white current-smokers, women were less likely to be early- compared to late-onset smokers (χ2 = 17.4, P < .001); however, there was no gender difference among African American early- and late-onset smokers (P > .27). Among current smokers, marital and parental status did not vary significantly by period-of-onset for either race.
Nearly 15% of the sample reported poor health at T2. As shown in Table 2, morbidity was more prevalent among non-smokers than smokers. For both races, morbidity rates were higher among late-onset smokers, compared to early-onset smokers.
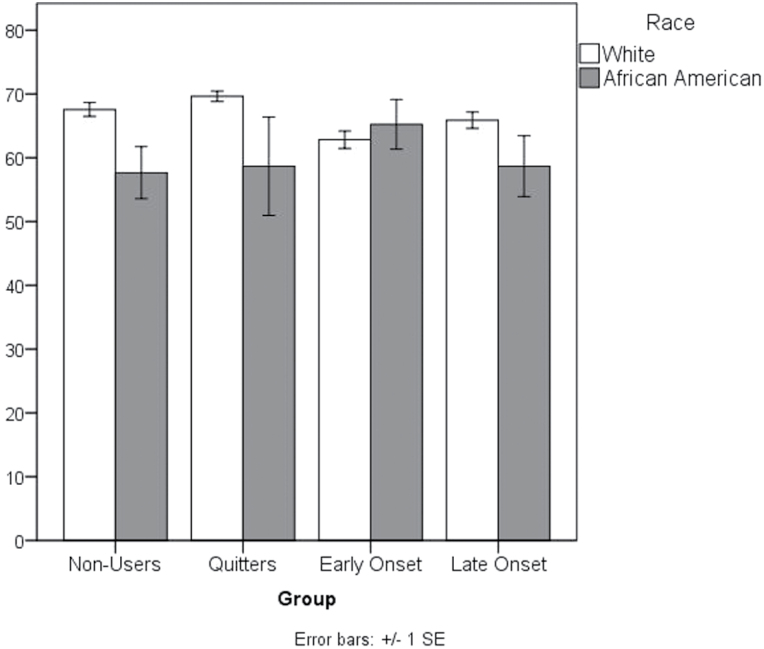
When examining the mortality sample, rates of mortality between T1 and T2 (for all races/ethnicities) were lowest among nonusers (5.3%), followed by quitters (10.4%), late-onset smokers (13.8%) and early-onset smokers (16.2%). A one-way analysis of variance on age-of-death (conditional on dying during the study period) revealed a similar pattern: There was a main effect of smoking category [F(3, 431) = 7.15, P < .001], and Games-Howell post hoc comparisons indicated that nonusers and quitters lived significantly longer than early-onset smokers (Ps ≤ .02) and quitters lived significantly longer than late-onset smokers (P = .04, see Figure 1 for outcomes among whites and African Americans only). A Kaplan-Meier analysis (which accounts for right-censored cases) also indicated a significant group-based difference in survival times (Log Rank χ2 = 206.3, df = 3, P < .001); nonusers lived the longest, followed by quitters, late-onset smokers, and early-onset smokers, respectively.
Figure 1.
Average age of death by race among those who died during the study period. Error bars indicate ± 1 standard error.
For the survival analysis, the main effects model indicated that the mortality hazard for an early-onset smoker was 1.5 times that of a late-onset smoker (P = .009). Race and SES had no significant effects in the main-effects model, and the Race × Period-of-Onset interaction was not significant (P > .6). As expected, there was a significant Race × Period-of-Onset × SES effect (P = .01); in this full model, the effect of SES was significant (see Table 3). Simple effects analyses allowed us to test the effect of Period-of-Onset for each combination of Race and SES (operationalized as Education; see Table 3). Findings indicated that among the white, low-SES group, the mortality hazard for an early-onset smoker was 2.5 times that of a late-onset smoker (P < .001). There were no differences in hazard rates between early- and late-onset smokers for the other groups. Thus, there was no evidence that a later age-of-onset was protective for African American smokers.
Table 3.
Outcomes of the Cox Proportional Hazards Models Predicting Cessation Among Ever-Regular-Smokers
| Factor of interest | Full model | Simple effects models | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| White, low SES | White, high SES | African American, low SES | African American, high SES | |||||||
| B (SE) | HR (95% CI) | B (SE) | HR (95% CI) | B (SE) | HR (95% CI) | B (SE) | HR (95% CI) | B (SE) | HR (95% CI) | |
| Racea | −0.57 (0.36) | 0.57 (0.28, 1.15) | ||||||||
| Period-of-Onsetb | 0.01 (0.24) | 1.01 (0.63, 1.62) | 0.90 (0.25) | 2.47 (1.51, 4.02) | −0.06 (0.26) | 0.95 (0.57, 1.58) | 1.43 (0.89) | 4.18 (0.73, 24.1) | −3.2 (9.7) | 0.04 (0, >100) |
| SESc | −0.52 (0.23) | 0.59 (0.38, 0.92) | ||||||||
| Race × Period-of-Onset × SES | 0.86 (0.34) | 2.4 (1.22, 4.60) | ||||||||
CI = confidence interval; HR = hazards ratio; SE = standard error; SES = socioeconomic status. Bold text indicates statistical significance (P < .05).
aReference group = African Americans.
bReference group = late-onset smokers.
cReference group = high education.
Discussion
Consistent with previous findings, our results indicate a later average smoking age-of-onset among African Americans, compared to whites. This finding appeared for both age of first cigarette (16.9 vs. 15.6) and age of beginning to smoke regularly (21.6 vs. 18.9). Late-onset African Americans also had the lowest cessation rates. Indeed, the cessation rates for all other groups of ever-smokers (early-onset African Americans and early- and late-onset whites) ranged from 52% to 57%; however, the cessation rate was only 33% for late-onset African Americans. This finding is consistent with recent work6 suggesting that, among African-Americans, persistence of smoking increases with increasing age-of-onset. Our data suggest this difference in cessation rates is not due to differences in the heaviness of smoking; future research will need to investigate both physiological and psychosocial factors that may contribute to the pattern. For example, dependence was not assessed in MIDUS, but is likely an important factor. Likewise, our finding that poor health is more common among white quitters than among African American quitters suggests that whites who become sick may be more likely to quit in response.
Finally, results showed that across SES levels, hazard rates for mortality did not differ among early- versus late-onset African American smokers. It should also be noted that among white, high-SES individuals, the mortality hazards also did not differ between early- versus late-onset smokers. In contrast, among white, low-SES individuals, the mortality hazard for an early-onset smoker was 2.5 times that of a late-onset smoker. Accordingly, although a late (vs. early) age of smoking onset may be protective for whites (in terms of cessation and age-of-mortality), there is some evidence that late onset is not particularly beneficial for African Americans. Overall, findings from this study are consistent with previous work,4,9 which suggests that different lifecourse patterns of cigarette use among whites and African Americans may contribute to America’s racial differences in health.
Strengths and Limitations
By using the MIDUS dataset, we were able to track smoking over the entire adult lifecourse; this allowed us to differentiate a truly late-onset smoking group, to identify quitters and never-regular-smokers, and also to examine a sizeable proportion of mortality outcomes. Another strength of this study is that it examined early- and late-onset smoking separately for each race, which prevented race and period-of-onset from being confounded. Likewise, mortality analyses examined interactions with SES, which prevented race and SES from being confounded.
Findings were limited by the self-report nature of MIDUS (although prior work suggests retrospective reports of age-of-onset are highly reliable39). MIDUS also assessed regular smoking in terms of smoking at least a few cigarettes every day, which excluded light and intermittent smokers. As African Americans are more likely than whites to be intermitent and light daily smokers,40 there was likely greater imprecision in the results for African American smokers; this is yet another area where future research should better appreciate racial/ethnic differences in smoking.
Power was low for some of the interactions (eg, there were few African American early-onset smokers and African American high-SES smokers), and so these analyses should be replicated with larger samples. Likewise, as attrition was greater among African Americans and early-onset smokers, some effects may be under/overestimated. Larger samples would also allow for analyses that stratify by age. Additionally, this study was limited by having only two time points of assessment. Future research should use data with multiple time points to examine smoking trajectories with advanced analytical approaches.
Moving Forward
The present study provides further evidence that African American late-onset smoking merits concerted attention. Not only is there a substantial proportion of African Americans who demonstrate late-onset smoking (here, 19.5% of all African Americans and 75% of all African American current smokers), but delaying onset does not appear to afford any cessation or longevity benefits for African Americans. Smoking initiation during the late teens and early adulthood is also an important public health issue because these ages coincide with the peak childbearing and child-rearing ages.8 The present results suggest prevention and intervention efforts need to consider individual groups (not just overall averages) and tobacco control efforts need to be targeted beyond the teenage years. For instance, one suggested US tobacco policy is to raise the minimum age for legal access to cigarettes from 18 to 21; analyses on the impact of such policies need to consider race, to test whether they are more effective among whites than other racial/ethnic groups, with the potential consequence of widening tobacco-related health disparities. As population-level approaches have at times exacerbated health disparities,41 answering this question is important. Likewise, developing and pursuing policies that have a pro-equity approach is critical; for example, restricting marketing at the external point of sale and banning tobacco advertising around schools may be equitable approaches.42,43 Prevention/intervention efforts that are culturally appropriate and targeted should also be used to reduce onset and persistence of smoking among African Americans.
More research is also needed to better understand the links between tobacco use, late-onset smoking and racial health disparities, including the risk and protective factors. It is also important to mention that late-onset smoking is not unique to African Americans, but is demonstrated by other racial/ethnic groups as well—notably, Asians/Pacific Islanders26—and research is also needed in these areas. Understanding the pattern of factors that predict late- versus early-onset smoking, including those patterns that are racially-specific, awaits further investigation.
Funding
This work was supported by the National Cancer Institute under grant P50CA180908.
Declaration of Interests
None declared.
Disclaimer
The findings and conclusions are the author’s, not necessarily the CDC’s.
Supplement Sponsorship
This article appears as part of the supplement “Critical Examination of Factors Related to the Smoking Trajectory among African American Youth and Young Adults,” sponsored by the Centers for Disease Control and Prevention contract no. 200-2014-M-58879.
References
- 1. Safford MM, Brown TM, Muntner PM, et al. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308(17):1768–1774. doi:10.1001/jama.2012.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Center for Disease Control and Prevention. MMWR Supplement: Coronary Heath Disease and Stroke Deaths – United States, 2009. MMWR. 2013;62(3):157–160. [PubMed] [Google Scholar]
- 3. American Lung Association. Too Many Cases, Too Many Deaths: Lung Cancer in African Americans 2015. www.lung.org/lung-disease/disparities-reports/lung-cancer-in-african-americans. Accessed August 5, 2015.
- 4. Belgrave FZ, Johnson J, Nguyen A, et al. Stress and tobacco use among African-American adolescents: the buffering effect of cultural factors. J Drug Educ. 2010;40(2):173–188. doi:http://dx.doi.org/10.2190/de.40.2.e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Freedman KS, Nelson NM, Feldman LL. Smoking initiation among young adults in the United States and Canada, 1998–2010: a systematic review. Prev Chronic Dis. 2012;9:E05. www.ncbi.nlm.nih.gov/pmc/articles/PMC3277388/ Accessed August 6, 2015. [PMC free article] [PubMed] [Google Scholar]
- 6. Kandel D, Schaffran C, Hu M-C, Thomas Y. Age-related differences in cigarette smoking among whites and African-Americans: evidence for the crossover hypothesis. Drug Alcohol Depend. 2011;118(2–3):280–287. doi:10.1016/j.drugalcdep.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen P, Jacobson KC. Developmental trajectories of substance use from early adolescence to young adulthood: gender and racial/ethnic differences. J Adolesc Health. 2012;50(2):154–163. doi:10.1016/j.jadohealth.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Moon-Howard J. African American women and smoking: starting later. Am J Public Health. 2003;93(3):418–420. doi:10.2105/AJPH.93.3.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Geronimus AT, Neidert LJ, Bound J. Age patterns of smoking in US black and white women of childbearing age. Am J Public Health. 1993;83(9):1258–1264. doi:10.2105/AJPH.83.9.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Arnett JJ, Brody GH. A fraught passage: the identity challenges of African American emerging adulthood. Hum Dev. 2008;51(5–6):291–293. doi:http://dx.doi.org/10.1159/000170891. [Google Scholar]
- 11. Keyes KM, Vo T, Wall MM, et al. Racial/ethnic differences in use of alcohol, tobacco, and marijuana: is there a cross-over from adolescence to adulthood? Soc Sci Med. 2015;124(12):132–141. doi:10.1016/j.socscimed.2014.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pampel FC. Racial convergence in cigarette use from adolescence to the mid-thirties. J Health Soc Behav. 2008;49(4):484–498. [PMC free article] [PubMed] [Google Scholar]
- 13. Brook JS, Zhang C, Finch SJ, Brook DW. Adolescent pathways to adult smoking: ethnic identity, peer substance use, and antisocial behavior. Am J Addict. 2010;19(2):178–186. doi:10.1111/j.1521-0391.2009.00018.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Brody GH, Chen Y, Kogan SM, et al. Family-centered program deters substance use, conduct problems, and depressive symptoms in Black adolescents. Pediatrics. 2012;129(1):108–115. doi:10.1542/peds.2011-0623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Primack BA, Bost JE, Land SR, Fine MJ. Volume of tobacco advertising in African American markets: systematic review and meta-analysis. Public Health Rep. 2007;122(5):607–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bennett GG, Wolin KY, Robinson EL, Fowler S, Edwards CL. Perceived racial/ethnic harassment and tobacco use among African American young adults. Am J Public Health. 2005;95(2):238–240. doi:10.2105/AJPH.2004.037812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gerrard M, Stock ML, Roberts ME, et al. Coping with racial discrimination: the role of substance use. Psychol Addict Behav. 2012;26(3):550–560. doi:10.1037/a0027711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gibbons FX, O’Hara RE, Stock ML, Gerrard M, Weng C-Y, Wills TA. The erosive effects of racism: reduced self-control mediates the relation between perceived racial discrimination and substance use in African American adolescents. J Pers Soc Psychol. 2012;102(5):1089–1104. doi:10.1037/a0027404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fagan P, Brook JS, Rubenstone E, Zhang C, Brook DW. Longitudinal precursors of young adult light smoking among African Americans and Puerto Ricans. Nicotine Tob Res. 2009;11(2):139–147. doi:10.1093/ntr/ntp009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100(5):933–939. doi:10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moolchan ET, Fagan P, Fernander AF, et al. Addressing tobacco-related health disparities. Addiction. 2007;102(s2):30–42. doi:10.1111/j.1360-0443.2007.01953.x. [DOI] [PubMed] [Google Scholar]
- 22. Centers for Disease Control and Prevention (US), National Center for Chronic Disease Prevention and Health Promotion (US), Office on Smoking and Health (US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention (US); 2010. www.ncbi.nlm.nih.gov/books/NBK53017/ Accessed August 6, 2015. [PubMed] [Google Scholar]
- 23. Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341–350. doi:10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- 24. Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Eng J Med. 2013;368(4):351–364. doi:10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nichter M. Smoking: what does culture have to do with it? Addiction. 2003;98(suppl 1):139–145. doi:10.1046/j.1360-0443.98.s1.9.x. [DOI] [PubMed] [Google Scholar]
- 26. Trinidad DR, Gilpin EA, Lee L, Pierce JP. Do the majority of Asian-American and African-American smokers start as adults? Am J Prev Med. 2004;26(2):156–158. doi:10.1016/j.amepre.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 27. Chassin L, Curran PJ, Presson CC, Sherman SJ, Wirth RJ. Developmental trajectories of cigarette smoking from adolescence to adulthood. In: USDHHS Publication, ed. Phenotypes and Endophenotypes: Foundations for Genetic Studies of Nicotine Use and Dependence (Tobacco Control Monograph No 20). Bethesda, MD: US Department of Health and Human Services, NIH, National Cancer Institute: NIH Publication, (09-6366); 2009:189–244. [Google Scholar]
- 28. Brook JS, Pahl K, Ning Y. Peer and parental influences on longitudinal trajectories of smoking among African Americans and Puerto Ricans. Nicotine Tob Res. 2006;8(5):639–651. doi:10.1080/14622200600789627. [DOI] [PubMed] [Google Scholar]
- 29. Breslau N, Peterson EL. Smoking cessation in young adults: age at initiation of cigarette smoking and other suspected influences. Am J Public Health. 1996;86(2):214–220. doi:http://dx.doi.org/10.2105/ajph.86.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Khuder SA, Dayal HH, Mutgi AB. Age at smoking onset and its effect on smoking cessation. Addict Behav. 1999;24(5):673–677. doi:10.1016/S0306-4603(98)00113-0. [DOI] [PubMed] [Google Scholar]
- 31. Thompson AB, Moon-Howard J, Messeri PA. Smoking cessation advantage among adult initiators: does it apply to Black women? Nicotine Tob Res. 2011;13(1):15–21. doi:10.1093/ntr/ntq200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Brim OG, Baltes PB, Bumpass LL, et al. National Survey of Midlife Development in the United States (MIDUS), 1995–1996. ICPSR02760-v8. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2011. doi:http://doi.org/10.3886/ICPSR02760. v8. [Google Scholar]
- 33. Ryff C, David M, Almeida JS, et al. National Survey of Midlife Development in the United States (MIDUS II), 2004–2006. ICPSR04652-v6. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2012. doi:http://doi.org/10.3886/ICPSR04652.v6. [Google Scholar]
- 34. Radler BT, Ryaff CD. Who participates? Accounting for longitudinal retention in the MIDUS national study of health and well-being. J Aging Health. 2010;22(3):307–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Keppel G. Design and Analysis: A Researcher’s Handbook. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1991. [Google Scholar]
- 36. Cox DR. Regression models and life-tables. J R Stat Soc Series B Methodol. 1972;34(2):187–220. [Google Scholar]
- 37. Korn EL, Graubard BI, Midthune D. Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol. 1997;145(1):72–80. [DOI] [PubMed] [Google Scholar]
- 38. Thiébaut ACM, Bénichou J. Choice of time-scale in Cox’s model analysis of epidemiologic cohort data: a simulation study. Statist Med. 2004;23(24):3803–3820. doi:10.1002/sim.2098. [DOI] [PubMed] [Google Scholar]
- 39. Colby SM, Clark MA, Rogers ML, et al. Development and reliability of the lifetime interview on smoking trajectories. Nicotine Tob Res. 2012;14(3):290–298. doi:10.1093/ntr/ntr212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Trinidad DR, Pérez-Stable EJ, Emery SL, White MM, Grana RA, Messer KS. Intermittent and light daily smoking across racial/ethnic groups in the United States. Nicotine Tob Res. 2009;11(2):203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008;98(2):216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lee JGL, Henriksen L, Rose SW, Moreland-Russell S, Ribisl KM. A systematic review of neighborhood disparities in point-of-sale tobacco marketing. Am J Public Health. 2015;105(9):e8–e18. doi:10.2105/AJPH.2015.302777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Luke DA, Ribisl KM, Smith C, Sorg AA. Family smoking prevention and tobacco control act: banning outdoor tobacco advertising near schools and playgrounds. Am J Prev Med. 2011;40(3):295–302. doi:10.1016/j.amepre.2010.11.018. [DOI] [PubMed] [Google Scholar]