ABSTRACT
Introduction: Often people responsible for the oral care of children feel or believe that since primary teeth will eventually shed, it is not worthwhile to spend time/money on providing good oral health to children. Parents are the ones who take care of their children and make decisions for them. Hence, they should have knowledge about primary teeth, their health and caring in order to build confidence in their children through tiny teeth.
Aim: To assess the knowledge of primary teeth and their importance among parents with children below 12 years.
Materials and methods: A total of 1,000 questionnaires containing questions written both in English and in the local language (Kannada) were prepared for data collection and were personally distributed to parents visiting dental clinics for their children’s dental treatment.
Statistical analysis: Both descriptive statistics and Chi-square test were used.
Results: Complaints related to dental caries constituted 82% of children visiting dental clinics among children in Bengaluru city. Only 39% of respondents were aware of all functions of primary teeth.
Conclusion: The present study revealed that the parents of Bengaluru city had superficial or partial knowledge of primary teeth and that there is a need to improve this awareness.
How to cite this article: Setty JV, Srinivasan I. Knowledge and Awareness of Primary Teeth and Their Importance among Parents in Bengaluru City, India. Int J Clin Pediatr Dent 2016;9(1):56-61.
Keywords: Awareness, Knowledge, Parents, Primary teeth.
INTRODUCTION
Primary teeth are the valuable assets of a child. In children, milk teeth/primary teeth play a vital role for eating, phonetics, esthetics and also as a space maintainer for permanent teeth. Often problems in milk teeth in the form of pain and swelling can cause distress to the child, leading to inability to chew or speak properly or even may affect the appearance of a child.
Young children’s dental environment is complex as parental knowledge, attitudes and beliefs affect the child’s oral health.1,2 As parents are the primary caregivers of their children they should have knowledge about the primary teeth, its health and caring in order to build confidence in their children.3 Parents are decision makers for their children. Sarnat et al4 reported that at the age of 5-6 years, the more positive the mother’s attitude toward dental health the better is the child’s oral hygiene. Therefore, it is important to examine the attitudes and also the knowledge of the parents, as these may affect their behavior toward their child’s oral health.
There has been a significant decline in the prevalence of dental caries in children in most of the industrialized countries on account of a conscientious effort on their part to promote oral health care of children. Children from low-income and disadvantaged families have been found to have high caries prevalence and poor oral health.5 In developing countries like India, there is limited documented research on parental awareness of primary teeth. So, the present study was undertaken to assess the knowledge, attitude and perceptions of parents of primary teeth in Bengaluru city, India.
AIMS AND OBJECTIVES
To assess the knowledge of primary teeth and their importance among parents with children below 12 years of age.
To compare the influence of socioeconomic status on the knowledge, awareness and importance of primary teeth.
MATERIALS AND METHODS
The study was conducted among parents of Bengaluru city, Karnataka, India. Prior approval for the study was obtained from the Institutional Ethical Committee, Mathrushri Ramabai Ambedkar Dental College and Hospital, Bengaluru. All parents of children aged up to 12 years who reported to the Department of Pedodon-tics and Preventive dentistry of Mathrushri Ramabai Ambedkar Dental College were invited to participate in the study. Voluntariness and strict confidentiality were assured; 1,000 questionnaires both in English and in the local language (Kannada) were personally distributed for data collection. Assistance was offered for those who desired help in understanding the questions.
The demographic details were collected from the parents, such as name, age, sex, educational qualification, address, monthly income, child’s age, number of children and the reason for visit to dental clinic. The responders were then asked to indicate the most appropriate correct answer from the given list of options in order to assess their knowledge, awareness and perception regarding importance of primary teeth.
The questionnaire assessed the parental knowledge and awareness about primary teeth, their location, number, functions, shedding and effects on permanent teeth. Further assessments of parents’ attitude toward treatment of decayed, traumatized or infected primary teeth and their willingness to comply with the treatment options for such teeth and also beliefs or taboos associated with extractions were made.
All over the world, social scientists have considered occupation as the most important determinant of the level of social standing of an individual in society. In India, Prasad’s classification of 1961, further modified in 1968 and 1970, is based on per capita income. Prasad’s classification has been used in most Indian studies and has been found to be effective in its task. The income limits emphasize only the need for updating this classification with time. Realizing this need, Kumar6 linked Prasad’s classification with the All India Consumer Price Index, as both of them shared the same base year of 1961. Thus, using the above method, the recent update of Prasad’s classification was used in our study.7 We considered classes I and II as high socioeconomic groups, class III as middle and classes IV and V as low socioeconomic groups.8
A total of 1,000 questionnaires were completed by the participants; 100 of them were excluded because they were either incomplete or someone other than the parent had completed the questionnaire or more than one option in the answers was ticked.
Collected data were tabulated and subjected for statistical analysis using Statistical Package for Social Sciences (SPSS) version 13.0. Frequency distribution which includes number and percentage was calculated. Chi-square analysis was used for comparison between different socioeconomic groups. The level of significance was set at p < 0.05.
RESULTS
It was observed that mothers (58%) accompanied their children more than fathers (42%) for dental treatment (Table 1). Caries-related conditions, such as, pain/food impaction/sensitivity constituted 82% of reasons for the visit to dental clinic.
Table 1: Gender distribution among parents accompanying children for dental treatment
| Gender | n | Percentage | |||
| Male | 324 | 36 | |||
| Female | 576 | 64 | |||
| Total | 900 | 100 |
Results of the questionnaire are tabulated in Table 2.
Table 2: Responses to the questions by parents
| Question | Options | Responses in numbers (n) | Percentage | ||||
| Q1 | What are milk teeth/primary teeth/deciduous teeth? | ||||||
| Teeth which are present in the children drinking milk | 234 | 26 | |||||
| Present in all children | 144 | 16 | |||||
| First set of teeth which will be replaced by permanent teeth | 468 | 52 | |||||
| None of these | 54 | 6 | |||||
| Q2 | How many milk teeth/primary teeth are present totally? | ||||||
| All front teeth | 189 | 21 | |||||
| All teeth in the mouth of 4-year-old children | 459 | 51 | |||||
| Don’t know | 180 | 20 | |||||
| All upper teeth | 72 | 8 | |||||
| Q4 | How many teeth in the mouth of 3-year-old are primary? | ||||||
| 50% | 225 | 25 | |||||
| 25% | 234 | 26 | |||||
| None | 90 | 10 | |||||
| All | 351 | 39 | |||||
| Q7 | Total no. of primary teeth present | ||||||
| 8 | 180 | 20 | |||||
| 12 | 162 | 18 | |||||
| 18 | 135 | 15 | |||||
| 20 | 270 | 30 | |||||
| 4 | 153 | 17 | |||||
| Q3 | Do you think all primary teeth will shed? | ||||||
| Yes | 549 | 61 | |||||
| No | 153 | 17 | |||||
| Only front teeth | 189 | 21 | |||||
| Only back teeth | 9 | 1 | |||||
| Q5 | By what age do you think all primary teeth will be replaced by permanent teeth? | ||||||
| 4 years | 108 | 12 | |||||
| 6 years | 189 | 21 | |||||
| 12 years | 477 | 53 | |||||
| 18 years | 126 | 14 | |||||
| Q6 | Do you think all the permanent teeth erupt by replacing their respective milk tooth? | ||||||
| Yes | 423 | 47 | |||||
| No | 153 | 17 | |||||
| Some of them | 324 | 36 | |||||
| Q8 | Primary teeth help in: | ||||||
| Chewing | 225 | 25 | |||||
| Appearance of child | 54 | 6 | |||||
| Speech | 18 | 2 | |||||
| Maintains the space for permanent teeth/guides the eruption of permanent teeth | 63 | 7 | |||||
| I and ii | 45 | 5 | |||||
| i, ii and iii | 126 | 14 | |||||
| i, ii and iv | 18 | 2 | |||||
| All of the above | 351 | 39 | |||||
| Q9 | Do you think it is important to treat a decayed milk tooth? | ||||||
| Yes | 774 | 86 | |||||
| No | 826 | 14 | |||||
| Q10 | If a primary tooth is infected | ||||||
| It is important to save infected primary teeth if possible | 684 | 76 | |||||
| It is unnecessary, since anyway tooth is going to fall | 216 | 24 | |||||
| Q11 | If an infected primary teeth in your child’s mouth require extensive treatment probably requiring a few visits to the dental office and some expenditure | ||||||
| You will agree for treatment | 540 | 60 | |||||
| You will not agree for treatment | 360 | 40 | |||||
| Q11 | Reasons | ||||||
| Time | 105 | 29 | |||||
| Economically difficult/expenditure | 104 | 29 | |||||
| Unnecessary to spend time and money for a tooth which is anyway going to shed | 151 | 41 | |||||
| Q12 | If an infected primary tooth require extraction which is the only possible treatment option | ||||||
| You will agree for extraction | 666 | 74 | |||||
| You will not agree for extraction | 234 | 26 | |||||
| Q12 | Reasons | ||||||
| Eyes will get affected | 63 | 27 | |||||
| Brain will get affected | 28 | 12 | |||||
| As the tooth will shed there is no need for extraction | 63 | 27 | |||||
| Will cause pain/trauma in child | 52 | 23 | |||||
| Expenditure | 28 | 12 |
The answers to questions regarding what parents pursue milk teeth/primary teeth showed ignorance among almost half of the participating parents (questions 1, 2 and 4 in Table 2).
Only 30% of parents were aware of total number of primary teeth present (question 7 in Table 2).
Knowledge regarding shedding of primary teeth and eruption of permanent teeth was not clear at least among half of the parents who participated in the study (questions 3, 5 and 6 in Table 2).
Among the respondents, only 39% of the parents were aware of all the functions of primary teeth (question 8 in Table 2).
When asked about the importance of treating a decayed or infected primary tooth, majority of the parents (86 and 76%, questions 9 and 10 of Table 2) felt it is important to treat such teeth, although about 40% of them were not ready to spend time and money for treatment since they felt it is unnecessary as these teeth will shed (question 11 - Reasons; Table 2, Graph 1).
Graph 1:
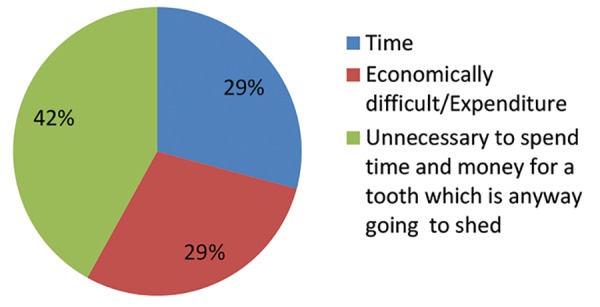
Reasons not willing for treatment
Willingness to comply with extraction as the only option left to treat the infected tooth was agreed by majority of them (74%) and only about 26% were not willing. This unwillingness was due to varied reasons like taboos associated with extraction, misconceptions like eyes and brain of the child may be affected, expenditure, procedures that might cause pain and trauma to the child or simply because primary tooth will anyway shed (question 12 - Reasons; Table 2, Graph 2).
Graph 2:
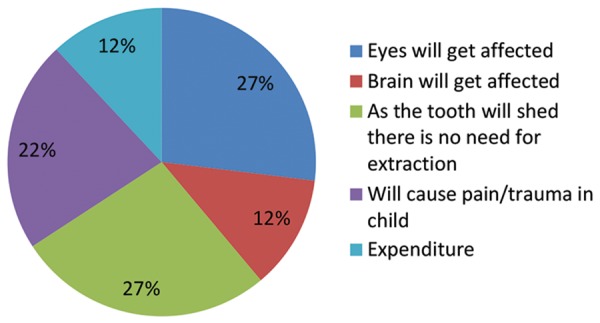
Reasons not willing for extraction
The results of the questionnaire when compared between different socioeconomic groups showed no statistical significance (Table 3). The knowledge of primary teeth was relatively less among low socioeconomic groups as compared with middle and high socioeconomic groups. Their willingness to comply with different options for treatment was also less, probably because of their socioeconomic status.
Table 3: Responses according to socioeconomic status
|
Class I (n = 270) |
Class II (n = 216) |
Class III (n = 233) |
Class IV (n = 9) |
||||||||||||||||||||
| Question | Options | n | % | n | % | n | % | n | % | X2 | p-value | ||||||||||||
| Q1 | Teeth which are present in the children drinking milk | 72 | 27 | 36 | 17 | 81 | 24 | 5 | 56 | 12.642 | 0.179 | ||||||||||||
| Present in all children | 49 | 23 | 9 | 4 | 63 | 19 | 1 | 11 | |||||||||||||||
| First set of teeth which will be replaced by | 108 | 40 | 153 | 71 | 180 | 54 | 3 | 33 | |||||||||||||||
| permanent teeth | |||||||||||||||||||||||
| None of these | 27 | 10 | 18 | 8 | 9 | 3 | 0 | 0 | |||||||||||||||
| Q2 | All front teeth | 54 | 20 | 63 | 29 | 63 | 19 | 1 | 11 | 18.083 | 0.034 | ||||||||||||
| All teeth in the mouth of 4-year-old | 180 | 67 | 99 | 46 | 153 | 46 | 3 | 33 | |||||||||||||||
| Do not know | 18 | 7 | 54 | 25 | 63 | 19 | 5 | 56 | |||||||||||||||
| All upper teeth | 18 | 7 | 0 | 0 | 54 | 16 | 0 | 0 | |||||||||||||||
| Q3 | Yes | 153 | 57 | 135 | 63 | 207 | 62 | 6 | 67 | 2.875 | 0.969 | ||||||||||||
| No | 54 | 20 | 36 | 17 | 54 | 16 | 1 | 11 | |||||||||||||||
| Only front teeth | 54 | 20 | 45 | 21 | 72 | 22 | 2 | 22 | |||||||||||||||
| Only back teeth | 9 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | |||||||||||||||
| Q4 | 50% | 81 | 30 | 36 | 17 | 99 | 30 | 1 | 11 | 5.247 | 0.812 | ||||||||||||
| 25% | 981 | 30 | 54 | 25 | 72 | 22 | 3 | 33 | |||||||||||||||
| None | 9 | 3 | 36 | 17 | 36 | 11 | 1 | 11 | |||||||||||||||
| All | 99 | 37 | 90 | 42 | 126 | 38 | 4 | 44 | |||||||||||||||
| Q5 | 4 years | 45 | 17 | 9 | 4 | 36 | 11 | 2 | 22 | 10.809 | 0.289 | ||||||||||||
| 6 years | 27 | 10 | 36 | 17 | 90 | 27 | 4 | 44 | |||||||||||||||
| 12 years | 162 | 60 | 126 | 58 | 162 | 49 | 3 | 33 | |||||||||||||||
| 18 years | 36 | 13 | 45 | 21 | 45 | 14 | 0 | 0 | |||||||||||||||
| Q6 | Yes | 153 | 57 | 108 | 50 | 126 | 38 | 4 | 44 | 8.003 | 0.238 | ||||||||||||
| No | 54 | 20 | 36 | 17 | 36 | 11 | 3 | 33 | |||||||||||||||
| Some of them | 63 | 23 | 72 | 33 | 171 | 51 | 2 | 22 | |||||||||||||||
| Q7 | 8 | 81 | 30 | 18 | 8 | 72 | 22 | 1 | 11 | 10.812 | 0.545 | ||||||||||||
| 12 | 54 | 20 | 35 | 21 | 54 | 16 | 1 | 11 | |||||||||||||||
| 18 | 45 | 17 | 36 | 17 | 36 | 11 | 2 | 22 | |||||||||||||||
| 20 | 81 | 30 | 63 | 29 | 108 | 32 | 2 | 22 | |||||||||||||||
| 24 | 9 | 3 | 54 | 25 | 63 | 19 | 3 | 33 | |||||||||||||||
| Q8 | Chewing | 72 | 27 | 45 | 21 | 90 | 27 | 18 | 22 | 17.856 | 0.658 | ||||||||||||
| Appearance of child | 0 | 0 | 27 | 13 | 18 | 5 | 9 | 11 | |||||||||||||||
| Speech | 0 | 0 | 0 | 0 | 9 | 3 | 9 | 11 | |||||||||||||||
| Maintains the space for permanent teeth | 18 | 7 | 18 | 8 | 27 | 8 | 0 | 0 | |||||||||||||||
| I and ii | 32 | 13 | 0 | 0 | 9 | 3 | 0 | 0 | |||||||||||||||
| i, ii and iii | 32 | 13 | 27 | 13 | 54 | 16 | 9 | 11 | |||||||||||||||
| i, ii and iv | 9 | 3 | 0 | 0 | 9 | 3 | 0 | 0 | |||||||||||||||
| All of the above | 99 | 37 | 99 | 46 | 117 | 35 | 36 | 44 | |||||||||||||||
| Q9 | Yes | 234 | 87 | 207 | 96 | 261 | 78 | 72 | 89 | 3.786 | 0.286 | ||||||||||||
| No | 36 | 13 | 9 | 4 | 72 | 22 | 9 | 11 | |||||||||||||||
| Q10 | It is important to save infected primary teeth if possible | 243 | 90 | 135 | 63 | 252 | 76 | 54 | 67 | 6.054 | 0.109 | ||||||||||||
| It is unnecessary, since anyway tooth is going to fall | 27 | 10 | 81 | 38 | 81 | 24 | 27 | 33 | |||||||||||||||
| Q11 | You will agree for treatment | 243 | 90 | 198 | 92 | 243 | 73 | 63 | 78 | 5.130 | 0.163 | ||||||||||||
| You will not agree for treatment | 27 | 10 | 18 | 8 | 90 | 27 | 18 | 22 | |||||||||||||||
| Q12 | You will agree for extraction | 198 | 73 | 189 | 88 | 207 | 62 | 72 | 89 | 6.012 | 0.111 | ||||||||||||
| You will not agree for extraction | 72 | 27 | 27 | 13 | 126 | 38 | 9 | 11 | |||||||||||||||
DISCUSSION
Maintaining healthy primary teeth is essential to a child’s overall oral and general development.9 Parents and family members are considered the primary source for knowledge about child rearing and health habits for children, which undoubtedly have a long-term influence in determining a child’s oral health status.10 They are considered the key persons in achieving the best oral health outcomes and assuring well-being for children.
Frequently in pediatric dental practice we find parents ignorant about the primary tooth, its function and importance. They often question the necessity of treatment to save and maintain the milk tooth in function.
There is no good reason for leaving primary teeth decayed and untreated in a child’s mouth. No other branch of medicine would willingly leave disease untreated.11
Untreated carious primary tooth can give rise to different complications, such as pain, oral infection, problems in eating and sleeping, malnutrition and alterations in growth and development12-15 and probably early loss of teeth, which might lead to short-term effects like problems in eating and speaking and long-term effects like malalignment of permanent teeth and increased risk of malocclusion later on.16
In the present study, 82% of parents visited the dental clinic only after their child had complaints of untreated carious teeth; 39% of parents were aware of all the functions of primary teeth. The reason for poor knowledge among parents and low value about primary teeth might be due to cultural-based opinions or the fact that these are temporary teeth and they will shed and be replaced by a new set of secondary teeth. Some authors have reported that certain cultures place little value on primary teeth and that caries and early loss of the primary dentition is an accepted occurrence.17
A qualitative study of caregivers in Saipan found that the low value attributed to baby teeth was an obstacle to developing effective preventive program.18 In another qualitative study, Finnish caregivers of preschool children gave less importance to primary teeth when compared with general health.19
Conversely a Canadian study indicated that parents who believed baby teeth were important had children with significantly lower caries rates than those who believed otherwise.20 Thus, parental knowledge of primary teeth appears to have a direct effect on the oral health of the child.
CONCLUSION
The present study revealed that the parents of Bengaluru city had superficial or partial knowledge and awareness of primary teeth and importance. There is a need to cultivate and reinforce positive attitude among parents and substantially raise their dental awareness through child dental health-oriented programs with active parental involvement. Such awareness programs should be developed for parents imparting knowledge about primary teeth, their function and preventive primary care of these teeth. To achieve this, young and prospective parents should be directed by the medical professionals, obstetricians, gynecologists and pediatricians to seek professional oral health counseling.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Crawford AN, Lennon MA. Dental attendance patterns among mother and their children in an area of social deprivation. Community Dent Health. 1992 Sep;9(3):289–291. [PubMed] [Google Scholar]
- 2.Grytten J, Rossow I, Holst D, Steele I. Longitudinal study of dental health behaviours and other caries predictors in early childhood. Community Dent Oral Epidemiol. 1988 Dec;16(6):356–359. doi: 10.1111/j.1600-0528.1988.tb00581.x. [DOI] [PubMed] [Google Scholar]
- 3.Nagaveni NB, Radhika NB, Umashankar KV. Knowledge, attitude and practices of parents regarding primary teeth care of their children in Davangere city, India. Pesq Bras Odontoped Clin Integr, Joao Pessoa. 2011 Jan;11(1):129–132. [Google Scholar]
- 4.Sarnat H, Kagan A, Raviv A. The relation between mother’s attitude towards dentistry and oral health status of their children. Pediatr Dent. 1984;6(3):128–131. [PubMed] [Google Scholar]
- 5.Woosung S, Susan TL, Amid I, Susan R. Caregiver’s perception of child oral health status among low-income African Americans. Pediatr Dent. 2008 Nov-Dec;30(6):480–487. [PubMed] [Google Scholar]
- 6.Kumar P. Social classification―need for constant updating. Indian J Community Med. 1993;18(2):60–61. [Google Scholar]
- 7.Sharma R. Letter to editor. South Asian J Cancer. 2013 Jul-Sep;2:224. [Google Scholar]
- 8.Tyagi R. The prevalence of nursing caries in Davanagere preschool children and its relationship with feeding practices and socioeconomic status of the family. J Indian Soc Pedod Prev Dent. 2008 Dec;26(4):153–157. doi: 10.4103/0970-4388.44030. [DOI] [PubMed] [Google Scholar]
- 9.Pinkham JR. Examination, diagnosis, and treatment planning of the infant and toddler. In: Casamassimo PS, Warren JJ, editors; Paediatric dentistry infancy: through adolescence. 4th ed. New York: Elsevier Inc.; 2005. pp. 206–219. [Google Scholar]
- 10.Watt RG. Parental knowledge and attitudes to oral health. Br Dent J. 2002 Dec;193:651–654. [Google Scholar]
- 11.Curzon MEJ, Pollard MA. Do we still care about children’s teeth? Br Dent J. 1997 Apr 12;182(7):242–246. doi: 10.1038/sj.bdj.4809356. [DOI] [PubMed] [Google Scholar]
- 12.Clarke M, Locker D, Berall G, Pencharz P, Kenny DJ, Judd P. Malnourishment in population of young children with severe early childhood caries. Pediatr Dent. 2006 May-Jun;28(3):254–259. [PubMed] [Google Scholar]
- 13.Schroth RJ, Harrison RL, Moffatt ME. Oral health of indigenous children and the influence of early childhood caries: on childhood health and wellbeing. Pediatr Clin North Am. 2009 Dec;56(6):1481–1499. doi: 10.1016/j.pcl.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 14.Schroth RJ, Jeal NS, Kliewer E, Sellers EAC. The relationship between vitamin D and Severe Early Childhood Caries: a pilot study. Int J Vitam Nutr Res. 2012 Feb;82(1):53–62. doi: 10.1024/0300-9831/a000094. [DOI] [PubMed] [Google Scholar]
- 15.Schroth RJ, Levi J, Kliewer E, Friel J, Moffatt ME. Association between iron status, iron deficiency anaemia, and severe early childhood caries: a case-control study. BMC Pediatr. 2013 Feb 7;13:22. doi: 10.1186/1471-2431-13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kagihara LE, Miedehauser VP, Stark M. Assessment, management and prevention of ECC. J Am Acad Nurse Pract. 2009 Jan;21(1):1–10. doi: 10.1111/j.1745-7599.2008.00367.x. [DOI] [PubMed] [Google Scholar]
- 17.Ng MW. Multicultural influences on child-rearing practices: implications for today’s pediatric dentist. Pediatr Dent. 2003 Jan-Feb;25(1):19–22. [PubMed] [Google Scholar]
- 18.Riedy CA, Weinstein P, Milgrom P. An ethnographic study for understanding children’s oral health in a multi-cultural community. Int Dent J. 2001 Aug;51(4):305–312. doi: 10.1002/j.1875-595x.2001.tb00843.x. [DOI] [PubMed] [Google Scholar]
- 19.Lahti SM, Hausen HW, Vaskilampi T. The perceptions of users about barriers to the use of free systematic oral care among Finnish pre-school children - a qualitative study. Acta Odontol Scand. 1999 Jun;57(3):139–143. doi: 10.1080/000163599428869. [DOI] [PubMed] [Google Scholar]
- 20.Schroth RJ, Brothwell DJ, Moffatt ME. Caregiver knowledge and attitudes of preschool oral health and early childhood caries (ECC) Int J Circumpolar Health. 2007 Apr;66(2):153–167. doi: 10.3402/ijch.v66i2.18247. [DOI] [PubMed] [Google Scholar]


