Abstract
Leptomeningeal dissemination of a primary brain tumor is a condition which is challenging to treat, as it often occurs in rather late disease stages in highly pretreated patients. Its prognosis is dismal and there is still no accepted standard of care. We report here a good clinical effect with a partial response in three out of nine patients and a stable disease with improvement on symptoms in two more patients following systemic anti-angiogenic treatment with bevacizumab (BEV) alone or in combination with chemo- and/or radiotherapy in a series of patients with leptomeningeal dissemination from primary brain tumors (diffuse astrocytoma WHO°II, anaplastic astrocytoma WHO°III, anaplastic oligodendroglioma WHO°III, primitive neuroectodermal tumor and glioblastoma, both WHO°IV). This translated into effective symptom control in five out of nine patients, but only moderate progression-free and overall survival times were reached. Partial responses as assessed by RANO criteria were observed in three patients (each one with anaplastic oligodendroglioma, primitive neuroectodermal tumor and glioblastoma). In these patients progression-free survival (PFS) intervals of 17, 10 and 20 weeks were achieved. In three patients (each one with diffuse astrocytoma, anaplastic astrocytoma and primitive neuroectodermal tumor) stable disease was observed with PFS of 13, 30 and 8 weeks. Another three patients (all with glioblastoma) were primary non-responders and deteriorated rapidly with PFS of 3 to 4 weeks. No severe adverse events were seen. These experiences suggest that the combination of BEV with more conventional therapy schemes with chemo- and/or radiotherapy may be a palliative treatment option for patients with leptomeningeal dissemination of brain tumors.
Introduction
Leptomeningeal dissemination (LMD) of primary brain tumors such as low-grade and anaplastic gliomas, glioblastomas, medulloblastomas (MB) and primitive neuroectodermal tumors (PNET) is a condition which considerably worsens the prognosis of the underlying disease [1,2]. Its frequency is most likely underestimated as in autopsy series it is found more commonly than in clinical series: while LMD was clinically reported in 2–4% [1,3] of patients with malignant glioma, autopsy studies reported a higher frequency of 6–21% [4,5]. Furthermore the incidence of LMD seems to be increasing over the last decades due to the improvement of both primary therapies and diagnostic means [4]. Spinal and leptomeningeal deposits of glioblastoma, in particular, are mainly recognized in advanced stages [6] and occur more frequently in younger patients [1]. Established therapy regimes include involved-field radiotherapy (IFXRT) of symptomatic lesions with a total dose of 25–40 Gy. This may result in some palliation, in particular of meningeal signs and cauda equina syndromes but its effect is rather vague with a median overall survival (mOS) between 2.8 and 16.8 months and no effect on median progression-free survival (mPFS) [5,7,8]. Furthermore, in patients with nerve compression or radicular syndromes like radicular pain due to compression of nerval structures in bony nerve channels caused by LMD, involved-field radiation therapy (IFXRT) and whole brain radiation therapy (WBXRT) have a good palliative effect [9]. Intrathecal therapy with methotrexate, cytosine arabinoside, Depocyt (cytarabine liposome) or thioTEPA has been used in LMD, with only modest differences in respect to toxicity and efficacy [10,11]. Published series report median progression-free survival (mPFS) intervals between 3.0 and 4.9 months and median overall-survival (mOS) intervals between 3.5 and 11.3 months for patients with LMD from malignant gliomas [1,7,12]. These diverging reports could be explained by varying timepoints of diagnosis of LMD, pretreatment and histology of the underlying primary brain tumor as well as the different therapy schemes used. On intrathecal administration of Depocyt in LMD of malignant glioma, only three out of nine patients received at least six weeks of treatment before further progression and the longest duration of treatment was 14 weeks [7]. Comparable to the multimodal treatment strategies for primary brain tumors in general, combinatorial approaches (i.e. combining radiotherapy with systemic or intrathecal chemotherapy) seem to be most promising [1,12]. However, intrathecal chemotherapy penetrates only few millimeters into brain tissue or subarachnoideal tumor nodules and therefore is not sufficient for the common nodular subtype of LMD [13]. Established systemic chemotherapies like temozolomide (TMZ) or alkylator regimens can be potent, however many patients have already received extensive pretreatment and therefore further chemotherapeutic treatment may not be highly promising. The rationale for combining anti-angiogenic therapies, e.g. bevacizumab (BEV) with these established therapy regimes in leptomeningeal gliomatosis is unclear, since often a significant portion of the malignant cells is dispersed in the cerebrospinal fluid (CSF). For this reason, anti-angiogenic strategies at first look do not seem to be purposeful. On the other hand, high VEGF levels in the CSF are known as a negative prognostic marker in LMD of solid tumors [14]. Increased proliferation through autocrine VEGF signalling under cell culture conditions has been described both for glioblastoma and medulloblastoma cells [15,16]. Further, clinical symptoms mostly arise from the compression of nerve roots or the spinal cord by tumor nodules or infiltration of these structures. While small nodular metastases and a diffuse “sugarcoating” of superficial neural structure can be supplied with nutrients solely by convection from the CSF, for the process of growth of leptomeningeal metastases beyond a certain size neo-angiogenesis is an essential step [17]. Therefore adding anti-angiogenic therapies like BEV may bring further benefit. BEV may alleviate edema and compression of cranial nerves, the spinal cord and nerve roots, by normalizing leaky blood-brain-barrier function.
For glioblastoma, one case report of a patient with combined intramedullary and leptomeningeal spread treated with radiotherapy and BEV monotherapy exists [18]. In this patient stable disease (SD) was achieved with a progression-free survival (PFS) of three months and an overvall survival (OS) of six months. Bae et al. [19] included in their patient series three patients with LMD treated with intrathecal methotrexate (MTX) additionally to systemic BEV and irinotecan. Two of those patients suffered from secondary glioblastoma, the third from pleomorphic xanthoastrocytoma with atypical features. OS after dissemination was 2, 5 and 2 months, respectively. While there is no such case report for primitive neuroectodermal tumor (PNET), one case report included one adult patient with recurrent medulloblastoma and LMD treated with BEV [20]. In this patient, monotherapy with BEV resulted in complete response (CR) with a progression-free survival (PFS) of almost 17 months, after which the patient died from an unrelated cause.
Bevacizumab has been used repeatedly in our center for the treatment of LMD of primary brain tumors, mostly in combination with chemo- and/or radiotherapy. However, the scientific knowledge of the benefits of bevacizumab in this situation is still very limited and up to date no case series focusing on the use of BEV in patients with LMD from brain tumors exist. Therefore, we performed a retrospective data analysis of all patients with LMD from primary brain tumors treated with BEV alone or in combination at our institution.
Patients and Methods
We report on nine consecutive patients treated during a time period of seven years between July 2008 and June 2015 with BEV (10mg/kg IV every 2 weeks) in combination with lomustine (CCNU), temozolomide (TMZ), irinotecan and/or radiotherapy or as a single agent on an individual basis. One patient suffered from an astrocytoma WHO°II, one from an anaplastic astrocytoma WHO°III, one from an anaplastic oligodendroglioma WHO°III, two patients from a primitive neuroectodermal tumor (PNET) WHO°IV and four patients from a glioblastoma WHO°IV (see Table 1). During the observation period, we treated approximately 264 patients with glioma WHO°II-III, 7 patients with PNET WHO°IV and 701 patients with glioblastoma (GB) WHO°IV in our center. In 6 patients (2.3%) with glioma WHO°II-III, 2 patients (28.6%) with PNET WHO°IV and 25 patients (3.6%) with GB WHO°IV the diagnosis of symptomatic LMD was established. These rates with a rather low incidence of LMD in gliomas WHO°II-III, a high incidence in PNET and a medium incidence in GB are in accordance with published data [2,7]. The decision for anti-angiogenic therapy with bevacizumab was subjected to a negative and positive selection. Patients with a Karnofsky patient score of ≤50% were usually given a recommendation for best supportive care (BSC), and patients with limited alkylator pretreatment were usually treated with a chemotherapy based exclusively on temozolomide or lomustine (CCNU). As the effect of bevacizumab on overall survival (OS) is very controversial [21,22], the decision for therapy with bevacizumab was restricted to (I) patients with extensive alkylator pretreatment, (II) patients with relevant myelosuppression (thrombocytes < 100/nl or leukocytes < 3/nl) and (III) patients with ongoing or (IV) anticipated clinical deterioration (based on imaging results) where an alkylator monotherapy was deemed insufficient by the treating physician (see Table 1). The decision in favour of combination chemotherapy was based on prior treatment and discussed openly with the patients. Given the fact that all patients with exception of patients 1 and 8 have received involved-field radiation therapy (IFXRT) of the brain before, whole brain radiation therapy (WBXRT) was deferred if possible. Rather, the patients received IFXRT of clinically symptomatic areas. In none of the patients LMD was already present at initial diagnosis, typically the diagnosis was established late in the course of the disease (see Table 1), which is consistent with other published reports [23]. The diagnosis of LMD was based both on leptomeningeal enhancement in magnetic resonance imaging (MRI) scans and CSF analysis. Since none of the patients of our series had an Ommaya reservoir implanted, CSF was taken by lumbar puncture. In all but one patient (patient 6) malignant cells were verified by CSF cytology. In patient 6, suspicious cells were seen which did not fulfil the diagnostic criteria for atypical neoplastic cells and were negative for GFAP (glial fibrillary acid protein). However, diagnosis was established on the basis of indicative imaging in combination with typical CSF parameters (cell number 101/μl, total protein 14 g/dl, lactate 8.45mmol/l, CSF glucose 20.1mg/dl). All nine patients showed a mix of diffuse and nodular leptomeningeal dissemination on imaging. Contrast-enhanced MRI scans were done at intervals of four to eight weeks and assessed according to RANO criteria [24].
Table 1. Patient characteristics.
| Pat. No. | Age | Gender | Primary tumor localisation | Histology | Pretreatment | Decision criteria for BEV therapy | Time between diagnosis and evidence of LMD [months] |
|---|---|---|---|---|---|---|---|
| 1 | 35 | M | intra-medullar Th11 | A | S, XRT-TMZ, TMZ, Re-XRT, CCNU | I, III | 45 |
| 2 | 31 | M | thalamus | AA | XRT-TMZ, TMZ, CCNU, Depocyt | I, II*, III | 13 |
| 3 | 33 | M | left frontal | AO | S, TMZ, Re-S, XRT | IV | 10 |
| 4 | 35 | M | pontine | PNET | XRT, CCV | III | 14 |
| 5 | 56 | M | bifrontal | PNET | S, XRT-TMZ, TMZ | III | 9 |
| 6 | 37 | F | left frontal | GB | S, XRT-TMZ, TMZ | III | 25 |
| 7 | 44 | F | right parietal | GB | S, XRT-TMZ, TMZ | III | 7 |
| 8 | 46 | M | gliomatosis cerebri | GB | PC, CCNU, TMZ | I | 28 |
| 9 | 55 | M | left temporal | GB | S, XRT-TMZ, TMZ | IV | 7 |
I = extensive alkylator pretreatment; II = myelosuppression; III = ongoing deterioriation; IV = anticipated clinical deterioration;
* = thrombocyte nadir of 20/nl;
A = Diffuse Astrocytoma WHO°II; AA = Anaplastic Astrocytoma WHO°III; AO = Anaplastic Oligodendroglioma WHO°III; CCNU = lomustine; CCV = lomustine/cisplatin/vincristine; Depocyt = intrathecal Depocyt; F = female; GB = Glioblastoma WHO°IV; LMD = leptomeningeal dissemination; M = male; ND = not determined; PC = procarbacine/lomustine; PNET = primitive neuroectodermal tumor WHO°IV; Re-XRT repeat involved field radiation therapy; Re-S = repeat surgery; S = surgery; TMZ = temozolomide 5/28; XRT = involved field radiation therapy; XRT-TMZ = involved field radiation therapy with concomitant temozolomide.
Our institutional review board approved this retrospective study and patients gave their written consent for scientific work with clinical data including MRI scans (ethics committee at the University Hospital Frankfurt; reference number 04/09-SNO 01/09).
Results
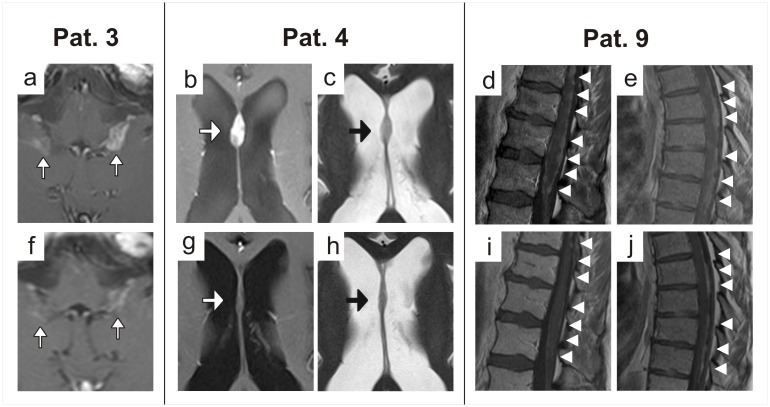
In patients 3, 4 and 9 rapid, impressive and sustained regression of nodular leptomeningeal contrast-enhancing lesions was achieved (partial response, PR). Contrast enhancing nodules considerably shrank and there was also some improvement of diffuse leptomeningeal enhancement (Fig 1a–1e and 1f–1j). Improvement was apparent in T2-weighted sequences as well. Pure pseudoregression through normalisation of the blood brain barrier therefore seems unlikely. Notably, in patient 9, regression of contrast enhancing lesions was observed beyond the field of involved-field radiotherapy (IFXRT; Fig 1e and 1j), therefore this effect cannot be explained by the radiotherapy but most likely is an effect of BEV therapy. Furthermore, the patient´s clinical condition improved clearly. An impressive clinical and radiological improvement was also observed in patients 3 and 4 (see Tables 2 and 3). However, as these patients received additional therapy in the form of involved-field radiotherapy (IFXRT) of the area affected or dose dense temozolomide chemotherapy, the determining factor for the observed response is not entirely clear. In patients 3, 4 and 9 progression-free survival (PFS) intervals of 17, 10 and 20 weeks and overall survival (OS) intervals of 20, 17 and 24 weeks respectively were achieved. In patients 1, 2 and 5 stable disease (SD) was reached. While patients 1 and 2 clinically improved, symptoms were stabilised in patient 5. In these three patients PFS intervals of 13, 30 and 8 weeks respectively were reached. In patients 1 and 5 OS intervals of 23 and 14 weeks were observed, whilst patient 2 is still alive. Patient 2 was initially a non-responder to a combination therapy with CCNU per os and Depocyt intrathecally over eight weeks (delate clinically and radiographically). After changing to monotherapy with BEV, clinical deterioration was halted and stabilisation of disease was achieved radiographically (see Table 2). Patients 5, 6 and 7 progressively deteriorated and the first imaging revealed progressive disease (PD). These patients had a PFS of 3, 4 and 4 weeks and an OS of 14, 11 and 11 weeks respectively. Summarized, the median progress-free survival (mPFS) of all nine patients was 10 weeks and the median overall-survival (mOS) was 15.5 weeks. In those five patients in which surveillance sampling of CSF was performed (patients 1–5), normalisation of CSF parameters was seen with a reduction of CSF cell number and/or protein concentration. Remarkably, clearing of malignant cells was attained in two out of five patients (patients 4 and 5). Additionally, in patient 2 an initially increased CSF pressure was normalised, which probably contributed to the marked clinical improvement observed (see Table 3). Five patients had clinical signs for raised CSF pressure at start of treatment. During treatment these symptoms disappeared in all patients, except for patient 6 (the only patient evidencing imaging compatible with malresorptive hydrocephalus). In all patients where steroid intake was necessary at start of treatment, a dose reduction was feasible (see Table 3). All patients tolerated BEV treatment well without suffering from typical side-effects like arterial hypertension or proteinuria. Two patients (patients 1 and 3) developed a common toxicity criteria (CTC) grade 3 leukopenia which spontaneously resolved. We attributed this side-effect to the simultaneous chemotherapies with CCNU or TMZ respectively.
Fig 1. MRI scans before (a-e) and under (f-j) therapy.
a, f: Reduced leptomeningeal enhancement (white arrows) after 8 weeks of therapy with bevacizumab and lomustine in patient 3. b, g: Regression of leptomeningeal contrast-enhancing nodule (white arrow) on the septum pellucidum on T1-weighted images after eight weeks of therapy with bevacizumab and temozolomide in patient 4. c, h: This regression (black arrow) in patient 3 was also visible on T2-weighted images, which makes pure pseudoresponse unlikely. d, i: Regression of leptomeningeal contrast-enhancing nodules (white arrowheads) on the surface of the medullar conus and the lumbar nerve roots on T1 weighted images (Th10-L2) in patient 9 before and after radiotherapy plus eight weeks of therapy with bevacizumab and lomustine. e, j: This regression of contrast-enhancement (white arrowheads) in patient 9 was also apparent in the thoracic spine (Th5-Th9) which was not treated with radiotherapy.
Table 2. Treatment and outcome.
| Pat. No. | Histology | Number of BEV cycles (10mg/kg every 2 weeks) | Simultaneous chemotherapy | Simultaneous radiotherapy | Best response (RANO criteria) | PFS [weeks] | OS [weeks] | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Substance | Dose [mg/m2] | Number of cycles | Length of each cycle [weeks] | Target area | Dose | Fractionating scheme | ||||||
| 1 | A | 6 | CCNU | 90 | 4 | 6 | WBXRT; IFXRT Th10 –Cauda equina | 40 Gy; 20 Gy | 20x 2 Gy; 5x 4 Gy | SD | 13 | 23 |
| 2 | AA | 15 | - | - | - | - | - | - | - | SD | 30 | NR |
| 3 | AO | 8 | CCNU | 110 | 3 | 6 | IFXRT posterior fossa | 36 Gy | 12x3 Gy | PR | 17 | 20 |
| 4 | PNET | 5 | TMZ 7/14 | 100 | 5 | 2 | - | - | - | PR | 10 | 17 |
| 5 | PNET | 4 | CCNU | 90 | 1 | 6 | - | - | - | SD | 8 | 14 |
| 6 | GB | 2 | - | - | - | - | IFXRT posterior fossa and IFXRT C1 –Th3 | 35 Gy | each 10x 3.5 Gy | PD | 3 | 14 |
| 7 | GB | 2 | CCNU | 90 | 1 | 6 | IFXRT posterior fossa—Th1 and IFXRT Th11 | 36 Gy | each 12x 3 Gy | PD | 4 | 11 |
| 8 | GB | 2 | IRI | 125 | 2 | 2 | - | - | - | PD | 4 | 11 |
| 9 | GB | 10 | CCNU | 90 | 4 | 6 | IFXRT Th11 –S1 | 36 Gy | 12x 3 Gy | PR | 20 | 24 |
A = Diffuse Astrocytoma WHO°II; AA = Anaplastic Astrocytoma WHO°III; AO = Anaplastic Oligodendroglioma WHO°III; BEV = bevacizumab; CCNU = lomustine; GB = Glioblastoma WHO°IV; IFXRT = involved field radiation therapy; IRI = irinotecan; NR = not reached; OS = overall survival; PD = progressive disease; PFS = progression free survival; PNET = primitive neuroectodermal tumor WHO°IV; PR = partial response; SD = stable disease; TMZ 7/14 = dose dense temozolomide (one week on / one week off); WBXRT = whole brain radiation therapy.
Table 3. Clinical course.
| Pat. No. | Presenting symptoms of LMD | Distribution of LMD | Clinical signs of raised intracranial pressure | Imaging compatible with hydrocephalus malresorptivus | Karnofsky patient score (KPS) | Steroid intake [mg of dexamethasone per day] | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| at start of therapy | under therapy | at start of therapy | under therapy | at start of therapy | development under therapy | at start of therapy | under therapy | |||
| 1 | headache | cerebral, spinal | + | - | - | - | 70 | +10 | 0 | 0 |
| 2 | headache, seizures | cerebral, spinal | + | - | - | - | 80 | +20 | 4 | 0 |
| 3 | headache, nausea | cerebral, spinal | + | - | - | - | 90 | +10 | 8 | 2 |
| 4 | headache, seizures, nausea, vomiting | cerebral, spinal | - | - | - | - | 60 | +20 | 0 | 0 |
| 5 | sensory loss | cerebral, spinal | - | - | - | - | 70 | ±0 | 4 | 0 |
| 6 | headache, pollacisuria | cerebral, spinal | + | + | + | ND | 60 | +10 | 16 | 12 |
| 7 | paresis, radicular pain | cerebral, spinal | - | - | - | - | 60 | -10 | 12 | 8 |
| 8 | paresis, radicular pain, sensory loss | cerebral, spinal | - | - | - | - | 80 | -20 | 12 | 6 |
| 9 | sensory loss, pollacisuria | spinal | - | - | - | - | 80 | +10 | 12 | 0 |
+ = present; - = not present; LMD = leptomeningeal dissemination; ND = not determined.
Discussion
In this cohort of patients suffering from LMD from primary brain tumors we report treatment responses to BEV in combination with lomustine, TMZ, irinotecan and/or radiotherapy, or as BEV monotherapy. We are able to demonstrate that these therapy strategies have a clinically meaningful response in this setting. In six out of nine patients, temporary symptom relief or stabilisation was seen. Consistent with the known imaging effects of bevacizumab in brain tumors [25], there was an improvement in nodular disease amongst the responders. The reduction of nodular disease indicates that the main mode of action of bevacizumab may be anti-angiogenic in LMD. However, we cannot rule out that inhibition of the direct autocrine effect of VEGF on tumor cells may be involved [15,16]. Since in most patients of our series, BEV was applied as part of a combination therapy, it remains difficult to attribute treatment response to BEV alone or to its use as cotherapy. However, we consider the following observations as rather convincing evidence for a distinct BEV effect: (I) regression of contrast enhancing lesions beyond the field of involved-field radiotherapy in patient 9, (II) the reversion of clinical deterioration by changeover from a CCNU/Depocyt combination therapy to a BEV monotherapy in patient 2 and (III) the normalisation of the initially elevated CSF pressure in the same patient. These effects cannot be attributed to steroids alone, since steroid doses in all steroid-dependent patients could be decremented during the course of therapy. The feasibility of reducing the steroid dose is also of high significance for the spectrum of adverse events suffered by the patients [26]. The reduction of the CSF pressure under BEV monotherapy and the improvement of several initially pathological CSF parameters strongly argue against the notion of BEV just being an “expensive super steroid” [27] in LMD. Patients with glioblastoma (GB) often exhibit a regression of contrast-enhancement accompanied with a reduction of cerebral oedema after the first BEV infusions [28]. However, an increase in hyperintense alterations is typically seen on T2- and FLAIR-sequences in the case of tumor progression [29,30]. This is of special interest for assessing the imaging of patients which achieved partial responses (patients 3, 4 and 9). In those patients regression of contrast-enhancing tumor areas was seen as well as regression of non-enhancing tumor nodules on T2 sequences, which cannot be explained by pure reduction of oedema. Interestingly enough, in patients with GB the treatment seemed to have a worse effect compared to the patients with non-GB primary brain tumors: While in GB patients, three out of four patients were primary non-responders, all patients with non-GB brain tumors in this series (five out of five) at least reached SD. This striking difference may be due to the enhanced aggressiveness or invasiveness of LMD from GB than that from non-GB brain tumors [7]. Still we consider that the patient number in this series is too low and the underlying histologies and the prior treatment modalities are too diverse to answer such a specific question. More reports on patients with LMD of primary brain tumors and BEV therapy have to be compiled to make a statement on the differential effects on particular primary brain tumor entities. The most significant limitation for the interpretation of this case series is that in all but one patient BEV was used as a combination partner to other therapy modalities. This multimodal therapeutic approach was applied due to the advanced disease stages and critical clinical situation of the patients reported on. Despite these unavoidable shortcomings, this series provides the novel reference that the addition of BEV to more established therapy regimens may have a good effect on the symptoms caused by LMD of brain tumors.
Summarized, the addition of BEV to established therapy regimens may represent a novel palliative treatment option for patients with leptomeningeal disseminated primary brain tumors. Similarly, BEV therapy seems to have a good therapeutic effect in brain metastases from NSCLC [31] and a combination of BEV with irinotecan in patients with refractory brain metastases from breast cancer has shown convincing results [32]. However, while there may be a good symptomatic effect, it is more than doubtful if overall survival (OS) can be improved. Furthermore, treatment with BEV is associated with considerable risks like gastrointestinal perforation, venous thromboembolism or intracranial hemorrhages [33]. To accurately determine the benefit of adding anti-angiogenic therapy to chemo- and/or radiotherapy in leptomeningeal dissemination in brain tumors, prospective clinical trials would be needed. However, these are difficult to perform due to the restricted number of patients with this rare complication of a rare disease, the variable pretreatments and therefore high variation in the course of the disease. The only conceivable approach in successfully realising such trials would be through large multi-institutional initiatives.
Data Availability
All relevant data are within the paper.
Funding Statement
The authors have no support or funding to report.
References
- 1.Mandel JJ, Yust-Katz S, Cachia D, Wu J, Liu D, de Groot JF, et al. (2014) Leptomeningeal dissemination in glioblastoma; an inspection of risk factors, treatment, and outcomes at a single institution. Journal of neuro-oncology 120: 597–605. 10.1007/s11060-014-1592-1 [DOI] [PubMed] [Google Scholar]
- 2.Hsieh PC, Wu CT, Lin KL, Jaing TH, Tseng CK, Lui TN, et al. (2008) The clinical experience of medulloblastoma treatment and the significance of time sequence for development of leptomeningeal metastasis. Childs Nerv Syst 24: 1463–1467. 10.1007/s00381-008-0697-2 [DOI] [PubMed] [Google Scholar]
- 3.Macdonald DR, Cascino TL, Schold SC Jr., Cairncross JG (1990) Response criteria for phase II studies of supratentorial malignant glioma. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 8: 1277–1280. [DOI] [PubMed] [Google Scholar]
- 4.Saito R, Kumabe T, Jokura H, Shirane R, Yoshimoto T (2003) Symptomatic spinal dissemination of malignant astrocytoma. J Neurooncol 61: 227–235. [DOI] [PubMed] [Google Scholar]
- 5.Vertosick FT Jr., Selker RG (1990) Brain stem and spinal metastases of supratentorial glioblastoma multiforme: a clinical series. Neurosurgery 27: 516–521; discussion 521–512. [DOI] [PubMed] [Google Scholar]
- 6.Schwaninger M, Patt S, Henningsen P, Schmidt D (1992) Spinal canal metastases: a late complication of glioblastoma. J Neurooncol 12: 93–98. [DOI] [PubMed] [Google Scholar]
- 7.Dardis C, Milton K, Ashby L, Shapiro W (2014) Leptomeningeal metastases in high-grade adult glioma: development, diagnosis, management, and outcomes in a series of 34 patients. Frontiers in neurology 5: 220 10.3389/fneur.2014.00220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karaca M, Andrieu MN, Hicsonmez A, Guney Y, Kurtman C (2006) Cases of glioblastoma multiforme metastasizing to spinal cord. Neurology India 54: 428–430. [DOI] [PubMed] [Google Scholar]
- 9.Alatakis S, Malham GM, Thien C (2001) Spinal leptomeningeal metastasis from cerebral glioblastoma multiforme presenting with radicular pain: case report and literature review. Surgical neurology 56: 33–37; discussion 37–38. [DOI] [PubMed] [Google Scholar]
- 10.Glantz MJ, LaFollette S, Jaeckle KA, Shapiro W, Swinnen L, Rozental JR, et al. (1999) Randomized trial of a slow-release versus a standard formulation of cytarabine for the intrathecal treatment of lymphomatous meningitis. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 17: 3110–3116. [DOI] [PubMed] [Google Scholar]
- 11.Noh JH, Lee MH, Kim WS, Lim do H, Kim ST, Kong DS, et al. (2015) Optimal treatment of leptomeningeal spread in glioblastoma: analysis of risk factors and outcome. Acta neurochirurgica 157: 569–576. 10.1007/s00701-015-2344-5 [DOI] [PubMed] [Google Scholar]
- 12.Chamberlain MC (2003) Combined-modality treatment of leptomeningeal gliomatosis. Neurosurgery 52: 324–329; discussion 330. [DOI] [PubMed] [Google Scholar]
- 13.Huang TY, Arita N, Hayakawa T, Ushio Y (1999) ACNU, MTX and 5-FU penetration of rat brain tissue and tumors. Journal of neuro-oncology 45: 9–17. [DOI] [PubMed] [Google Scholar]
- 14.Herrlinger U, Wiendl H, Renninger M, Forschler H, Dichgans J, Weller M (2004) Vascular endothelial growth factor (VEGF) in leptomeningeal metastasis: diagnostic and prognostic value. Br J Cancer 91: 219–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knizetova P, Ehrmann J, Hlobilkova A, Vancova I, Kalita O, Kolar Z, et al. (2008) Autocrine regulation of glioblastoma cell cycle progression, viability and radioresistance through the VEGF-VEGFR2 (KDR) interplay. Cell cycle 7: 2553–2561. [DOI] [PubMed] [Google Scholar]
- 16.Slongo ML, Molena B, Brunati AM, Frasson M, Gardiman M, Carli M, et al. (2007) Functional VEGF and VEGF receptors are expressed in human medulloblastomas. Neuro-oncology 9: 384–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li K, Zhang G, Zhao J, Wang X, Li Y, Hu Y (2011) Vascular endothelial growth factor antisense oligonucleotides inhibit leptomeningeal metastasis in vivo. Med Oncol 28: 1116–1122. 10.1007/s12032-010-9580-6 [DOI] [PubMed] [Google Scholar]
- 18.Fiorentino A, Caivano R, Chiumento C, Cozzolino M, Fusco V (2012) Radiotherapy and bevacizumab for intramedullary and leptomenigeal metastatic glioblastoma: a case report and review of the literature. The International journal of neuroscience 122: 691–694. 10.3109/00207454.2012.704456 [DOI] [PubMed] [Google Scholar]
- 19.Bae JS, Yang SH, Yoon WS, Kang SG, Hong YK, Jeun SS (2011) The clinical features of spinal leptomeningeal dissemination from malignant gliomas. Journal of Korean Neurosurgical Society 49: 334–338. 10.3340/jkns.2011.49.6.334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Privitera G, Acquaviva G, Ettorre GC, Spatola C (2009) Antiangiogenic therapy in the treatment of recurrent medulloblastoma in the adult: case report and review of the literature. Journal of oncology 2009: 247873 10.1155/2009/247873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sandmann T, Bourgon R, Garcia J, Li C, Cloughesy T, Chinot OL, et al. (2015) Patients With Proneural Glioblastoma May Derive Overall Survival Benefit From the Addition of Bevacizumab to First-Line Radiotherapy and Temozolomide: Retrospective Analysis of the AVAglio Trial. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 33: 2735–2744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taal W, Oosterkamp HM, Walenkamp AM, Dubbink HJ, Beerepoot LV, Hanse MC, et al. (2014) Single-agent bevacizumab or lomustine versus a combination of bevacizumab plus lomustine in patients with recurrent glioblastoma (BELOB trial): a randomised controlled phase 2 trial. The Lancet Oncology 15: 943–953. 10.1016/S1470-2045(14)70314-6 [DOI] [PubMed] [Google Scholar]
- 23.Scott BJ, van Vugt VA, Rush T, Brown T, Chen CC, Carter BS, et al. (2014) Concurrent intrathecal methotrexate and liposomal cytarabine for leptomeningeal metastasis from solid tumors: a retrospective cohort study. Journal of neuro-oncology 119: 361–368. 10.1007/s11060-014-1486-2 [DOI] [PubMed] [Google Scholar]
- 24.Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, et al. (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 28: 1963–1972. [DOI] [PubMed] [Google Scholar]
- 25.Thompson EM, Dosa E, Kraemer DF, Neuwelt EA (2011) Correlation of MRI sequences to assess progressive glioblastoma multiforme treated with bevacizumab. Journal of neuro-oncology 103: 353–360. 10.1007/s11060-010-0397-0 [DOI] [PubMed] [Google Scholar]
- 26.Vredenburgh JJ, Cloughesy T, Samant M, Prados M, Wen PY, Mikkelsen T, et al. (2010) Corticosteroid use in patients with glioblastoma at first or second relapse treated with bevacizumab in the BRAIN study. The oncologist 15: 1329–1334. 10.1634/theoncologist.2010-0105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Narita Y (2013) Drug review: Safety and efficacy of bevacizumab for glioblastoma and other brain tumors. Japanese journal of clinical oncology 43: 587–595. 10.1093/jjco/hyt051 [DOI] [PubMed] [Google Scholar]
- 28.Ruben JD, Dally M, Bailey M, Smith R, McLean CA, Fedele P (2006) Cerebral radiation necrosis: incidence, outcomes, and risk factors with emphasis on radiation parameters and chemotherapy. International journal of radiation oncology, biology, physics 65: 499–508. [DOI] [PubMed] [Google Scholar]
- 29.Norden AD, Young GS, Setayesh K, Muzikansky A, Klufas R, Ross GL, et al. (2008) Bevacizumab for recurrent malignant gliomas: efficacy, toxicity, and patterns of recurrence. Neurology 70: 779–787. 10.1212/01.wnl.0000304121.57857.38 [DOI] [PubMed] [Google Scholar]
- 30.Zuniga RM, Torcuator R, Jain R, Anderson J, Doyle T, Ellika S, et al. (2009) Efficacy, safety and patterns of response and recurrence in patients with recurrent high-grade gliomas treated with bevacizumab plus irinotecan. J Neurooncol 91: 329–336. 10.1007/s11060-008-9718-y [DOI] [PubMed] [Google Scholar]
- 31.De Braganca KC, Janjigian YY, Azzoli CG, Kris MG, Pietanza MC, Nolan CP, et al. (2010) Efficacy and safety of bevacizumab in active brain metastases from non-small cell lung cancer. Journal of neuro-oncology 100: 443–447. 10.1007/s11060-010-0200-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sengupta S, Rojas R, Mahadevan A, Kasper E, Jeyapalan S (2015) CPT-11/bevacizumab for the treatment of refractory brain metastases in patients with HER2-neu-positive breast cancer. Oxf Med Case Reports 4: 254–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, et al. (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. The New England journal of medicine 370: 699–708. 10.1056/NEJMoa1308573 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.