Abstract
Background and Aim
Because most colorectal cancer patients survive beyond five years, understanding quality of life among these long-term survivors is essential to providing comprehensive survivor care. We sought to identify personal characteristics associated with reported quality of life in colorectal cancer survivors, and sub-groups of survivors potentially vulnerable to very low quality of life.
Methods
We assessed quality of life using the Veterans RAND 12-item Health Survey within a population-based sample of 1,021 colorectal cancer survivors in the Seattle Colorectal Cancer Family Registry, approximately 5 years post-diagnosis. In this case-only study, mean physical component summary scores and mental component summary scores were examined with linear regression. To identify survivors with substantially reduced ability to complete daily tasks, logistic regression was used to estimate odds ratios for “very low” summary scores, defined as a score in the lowest decile of the reference US population. All cases were followed for vital status following QoL assessment, and mortality was analyzed with Cox proportional hazards regression.
Results
Lower mean physical component summary score was associated with older age, female sex, obesity, smoking, and diabetes or other co-morbidity; lower mean mental component summary score was associated with younger age and female sex. Higher odds of very low physical component summary score was associated with older age, obesity, less education, smoking, co-morbidities, and later stage at diagnosis; smoking was associated with higher odds of very low mental component summary score. A very low physical component score was associated with higher risk of mortality (hazard ratio (95% confidence interval): 3.97 (2.95–5.34)).
Conclusions
Our results suggest that identifiable sub-groups of survivors are vulnerable to very low physical components of quality of life, decrements that may represent meaningful impairment in completing everyday tasks and are associated with higher risk of death.
Introduction
A majority of patients with colorectal cancer (CRC) will survive five years or longer, and for those diagnosed with localized disease, 5-year survival exceeds 85%[1]. Thus a better understanding of quality of life (QoL) among survivors has become an essential component of providing comprehensive and directed survivor care. In particular, identification of survivors at highest risk of very low QoL may be important for developing appropriate and effective long-term survivorship plans.
Several studies of QoL in long-term (≥5 years) CRC survivors have been recently reviewed[2]. However, a limited number of these studies were population-based, investigated global measures of QoL, and included a large number of survivors [3–9]. The results of these studies suggest that, on average, long-term CRC survivors experience good QoL with only moderately lower physical functioning associated with older age, obesity, co-morbidities, smoking, and lower socioeconomic status [2, 7–10]. Psychological QoL has generally been observed to be comparable to the general population despite possibly higher depression scores[2, 3, 9–12].
In this study, we evaluated QoL in the Seattle Colorectal Cancer Family Registry (CCFR) [13]. Our aims were to identify personal characteristics of survivors associated with mean QoL among survivors in this large, population-based sample. In addition, the previously reported magnitudes of mean differences in QoL scores comparing groups of survivors were modest and may not reflect meaningful deficits in functioning.[14–18] Therefore, we investigated the distribution of QoL among survivors in order to identify sub-groups of CRC survivors potentially at higher risk of experiencing poor QoL associated with substantial impairment.
Finally, we investigated the extent to which QoL scores were associated with subsequent mortality. Prior studies of the relationship between health-related QoL and survival in CRC patients have suggested that QoL soon after diagnosis or early in treatment is prognostic independent of clinical characteristics; results suggest that QoL is an independent predictor of survival especially among patients with advanced CRC[19–25]. Much less has been reported regarding QoL and subsequent survival among long-term CRC survivors. In the general population, health-related QoL has also been associated with risk of mortality [26, 27] Therefore we explored the association of QoL with mortality among long-term CRC survivors.
Materials and Methods
Ethics statement
This study was approved by the Fred Hutchinson Cancer Research Center institutional review board, and conducted consistent with the 1964 Helsinki declaration and amendments. All participants provided written informed consent.
Study population
The Seattle CCFR is a population-based registry that includes primary invasive colorectal cancer cases diagnosed through Puget Sound Region Surveillance, Epidemiology, and End Results (SEER) cancer registry, and their first degree relatives. Details of the registry enrollment protocols, eligibility criteria, and response rates have been published[13, 28, 29]. Cases diagnosed 1998–2004 were typically enrolled within 8 months of diagnosis, and response rates averaged 75% among eligible cases alive at contact[28, 29].
Baseline data collection
Cases completed standardized telephone interviews covering CRC risk factors, including demographics, height and weight (2 years prior to baseline interview), smoking history (2 years prior to baseline interview), lifestyle and dietary factors, medications, cancer screening procedures, and history of digestive diseases (colitis, Crohn’s disease, irritable bowel syndrome, or diverticulitis) and diabetes. Body mass index (BMI, kg/m2) was calculated as weight divided by height squared. Data on stage at diagnosis and tumor site were obtained through the Puget Sound SEER cancer registry.
Follow-up data collection including quality of life (QoL)
Cases still alive approximately five years after diagnosis were re-contacted for follow-up telephone interviews (90%) or mailed questionnaires between 2004 and 2012. The mean time between baseline data collection and follow-up data collection was 5.5 years (interquartile range: 5.1 to 5.8 years).
Follow-up interviews covered cancer surveillance tests, incident cancers, medication use, and updates to family history of cancer since the baseline interview. QoL was assessed with the Veterans RAND 12-item Health Survey (VR-12), a standard and validated survey tool used to assess health-related physical and mental QoL and which is available in the public domain [14, 30]. The VR-12 has been validated in populations other than veterans, including Medicare enrollees[14]. The VR-12 was adapted from the copyright-protected 12-item Short-Form Health Survey (SF-12) [15, 31]. The physical component summary (PCS) score and mental component summary (MCS) score were each calculated from 6 questions following published procedures; in this method, PCS and MCS scores are scaled for comparison to a normative population[14, 30].[32][15]
Cases were followed for vital status through linkage to the National Death Index through the Puget Sound SEER cancer registry, from enrollment in the SCCFR to July 1, 2013.
Study participation rates
The population from which sample for this study was drawn included CRC cases enrolled 1998–2004 (N = 2,106 total). Of these cases, 1,533 were alive 5 years post-diagnosis and therefore eligible for follow-up; 1,095 (71%) responded to the follow-up questionnaire. We subsequently excluded cases with incomplete VR-12 or covariate data (N = 74 cases). Hence, in total, 1,021 survivors completed baseline and follow-up questionnaires including VR-12 components necessary for calculation of MCS and PCS scores, and had complete information on analytical variables, and were included in these analyses.
Compared to the 1,021 survivors included in the present analyses, the non-participating 1,011 CRC cases (“non-responders”, including deceased cases) were approximately the same age at diagnosis (mean 58.6 years and 58.2 years), and a larger proportion of non-responders were male (58% to 52%), smokers (14% to 10%), and diagnosed with distant CRC (15% to 3%).
Statistical analysis
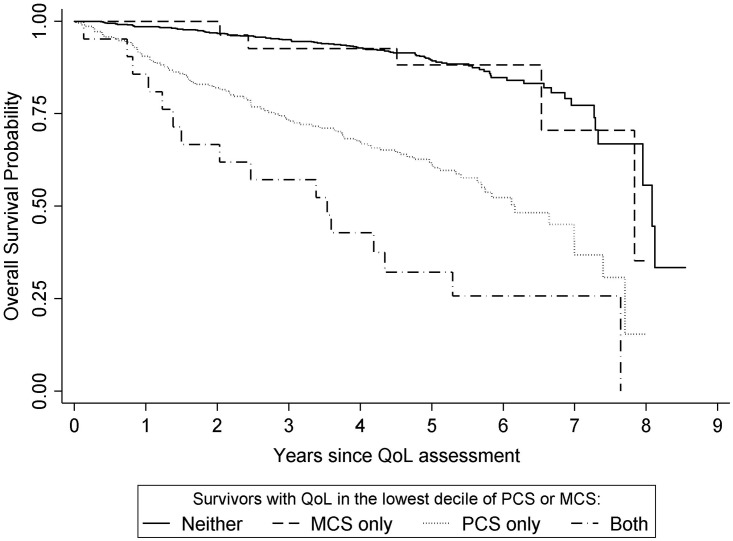
Unadjusted arithmetic mean PCS and MCS scores were calculated for survivors. We also constructed histograms to visually qualitatively examine the distribution of PCS and MCS scores in survivors.
Multivariate linear regression was used to estimate the association of mean PCS and MCS scores with personal characteristics. The significance of each personal characteristic in the model was assessed with a two-tailed Wald test (significance at P<0.05). For presentation, coefficients of the linear regression model are expressed as the difference in mean PCS or MCS score associated with each category compared to the reference category. The intercept of the linear regression model is the mean PCS or MCS predicted for (hypothetical) persons in the referent category of all variables.
In a separate analytical approach, to identify survivors with meaningfully lower QoL scores[15, 17], participants’ PCS and MCS scores were compared to the lowest decile in the normative score distribution for the general US population, i.e., a normal distribution with mean 50 and standard deviation 10 [15, 32]. Thus, PCS and MCS scores in survivors and relatives were categorized as either below, or equal to or above, the 10th percentile cut-off (<37.2 or ≥37.2 respectively) previously established for the US general population. Hence, scores less than 37.2 were labeled “very low.” Multivariate logistic regression was then used to estimate odds ratios (ORs) and 95% confidence intervals (95% CIs) for a PCS or MCS scores by category of personal characteristics. Therefore, in this case-only study, there were no controls; instead the normed QoL scores from the general population are used as a reference to identify cases with objectively very low QoL scores[15]. To examine sensitivity to the choice of the 10th percentile as the cut-off for “very low” PCS or MCS, in additional analyses the cut-off was changed to the lowest quartile (<43.3) or lowest 5th percentile (<33.6).
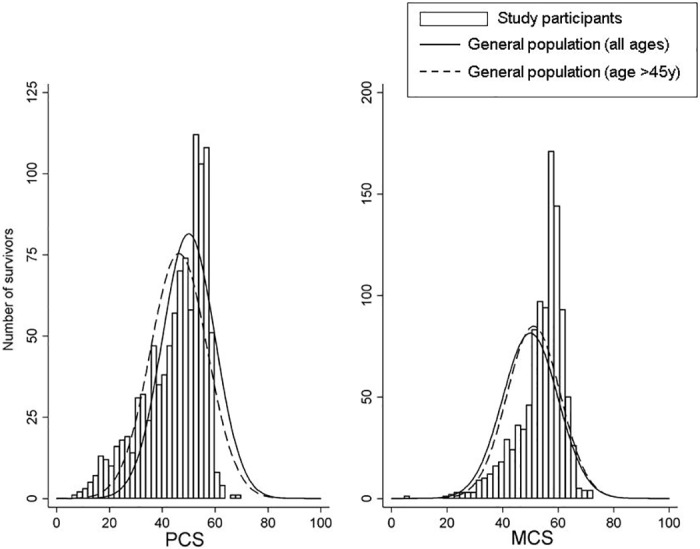
For statistical analysis of survival, time was measured in days from completion of the follow-up questionnaire assessing QoL. Kaplan-Meier product limits of overall survival probability were calculated comparing survivors according to PCS and MCS scores and compared with a global log-rank test. Subsequently, Cox proportional hazards regression was used to estimate hazard ratios (HRs) of death associated with very low PCS or MCS score (<37.2), compared to survivors with scores ≥37.2 (i.e., not “very low”). HR estimates for PCS were adjusted for MCS and estimates for MCS were adjusted for PCS, and additionally adjusted for age and sex and stratified by stage at diagnosis. In a second model, HRs for death was estimated comparing survivors in each stratum of one or both PCS and MCS scores <37.2 to survivors with both PCS and MCS ≥37.2. Additional adjustment for smoking, BMI, marital status, education, race and/or diabetes did not materially change the results of analysis.
Statistical analyses were completed using Stata/SE v14 (StataCorp, College Station, TX).
Results
Long-term CRC survivors in this study were typically over 50 years old at diagnosis, and the numbers of men and women were similar (Table 1). A majority of CRC survivors were either overweight or obese, had some history of smoking cigarettes, were married, and reported some post-secondary education. The majority of survivors who were alive and participated in the 5 year follow-up interview were diagnosed with local stage CRC, and were more likely to have had colon cancer than rectal cancer.
Table 1. Association of personal characteristics at enrollment with mean Physical Component Summary (PCS) and Mental Component Summary (MCS) scores from the VR-12, for survivors at 5 year follow-up in the Seattle Colorectal Cancer Family Registry.
| N (%) | PCS | MCS | |||||
|---|---|---|---|---|---|---|---|
| Difference in Mean PCS | (95%CI) | P | Difference in Mean MCS | (95%CI) | P | ||
| Age (y)a | |||||||
| <50 | 228 (22) | ref. | <0.001 | ref | <0.001 | ||
| 50–59 | 272 (27) | -1.5 | (-3.4, 0.3) | 2.6 | (1.1, 4.1) | ||
| 60–69 | 337 (33) | -3.1 | (-5.0, -1.2) | 4.5 | (3.0, 6.0) | ||
| ≥70 | 184 (18) | -5.9 | (-8.0, -3.7) | 3.7 | (1.9,5.4) | ||
| Sex | 0.001 | 0.001 | |||||
| Male | 530 (52) | ref | ref | ||||
| Female | 491 (48) | -2.3 | (-3.6, -0.9) | -1.7 | (-2.8, -0.7) | ||
| BMI (kg/m2)b | <0.001 | 0.70 | |||||
| <25 | 335 (33) | ref | ref | ||||
| 25–29.9 | 408 (40) | -0.9 | (-2.4, 0.6) | -0.3 | (-1.5, 0.9) | ||
| ≥30 | 278 (27) | -3.7 | (-5.6, -1.9) | 0.2 | (-1.2, 1.6) | ||
| Marital Statusa | 0.49 | 0.66 | |||||
| Not married | 259 (25) | -0.5 | (-2.1, 1.0) | -0.3 | (-1.5, 1.0) | ||
| Married or living as married | 762 (75) | ref | ref | ||||
| Race | 0.22 | 0.73 | |||||
| White | 933 (91) | ref | -0.3 | (-2.2, 1.6) | |||
| Other | 88 (9) | 1.3 | (-0.8, 3.4) | ref | |||
| Educationa | <0.001 | 0.19 | |||||
| High school or less | 318 (31) | -1.5 | (-3.2, 0.3) | -0.6 | (-1.9, 0.8) | ||
| Some college or technical education | 335 (33) | ref | ref | ||||
| College graduate | 368 (36) | 2.4 | (0.8, 4.0) | 0.6 | (-0.6, 1.7) | ||
| Cigarette Smokinga | <0.001 | 0.11 | |||||
| Never | 414 (41) | ref | ref | ||||
| Former | 502 (49) | -1.5 | (-2.9, -0.1) | -0.3 | (-1.4, 0.8) | ||
| Current | 105 (10) | -5.5 | (-8.1, -2.9) | -2.3 | (-4.5, 0.2) | ||
| Colorectal Co-morbiditiesa,c | 0.049 | 0.16 | |||||
| None | 837 (82) | ref | ref | ||||
| One or more | 184 (18) | -1.8 | (-3.5, 0.0) | -1.0 | (-2.4, 0.4) | ||
| Diabetesa,d | <0.001 | 0.18 | |||||
| No | 899 (88) | ref | ref | ||||
| Yes | 122 (12) | -5.0 | (-7.4, -2.6) | -1.2 | (-2.9, 0.6) | ||
| Stage at Diagnosis | 0.12 | 0.57 | |||||
| Local | 517 (51) | ref | ref | ||||
| Regional | 454 (44) | -0.5 | (-1.9, 0.9) | -0.8 | (-1.9, 0.2) | ||
| Distant | 30 (3) | -1.1 | (-5.7, 3.6) | 1.9 | (-0.2, 4.1) | ||
| Unstaged or unknown | 20 (2) | -6.3 | (-11.6, -1.1) | -0.8 | (-4.7, 3.1) | ||
| Site of Tumor | 0.59 | 0.74 | |||||
| Colon | 619 (61) | ref | ref | ||||
| Rectum | 349 (34) | -0.7 | (-2.1, 0.7) | 0.2 | (-0.9, 1.3) | ||
| Unknown | 53 (5) | -0.8 | (-3.9, 2.3) | -0.7 | (-2.9, 1.6) | ||
| Intercept e | 52.5 | (50.4, 54.8) | 53.2 | (51.4, 55.1) | |||
a At Colon Cancer Family Registry enrollment.
b Two years prior to baseline interview.
c Self-report of physician diagnosis of colitis, Crohns disease, diverticulitis, or irritable bowel syndrome.
d Self-report of physician diagnosis of diabetes.
e The intercept from the linear regression model is the mean PCS and MCS among (hypothetical) individuals in the referent category for all variables.
The unadjusted mean (95% CI) PCS score was 45.1 (44.4–45.8) among survivors, slightly lower than the US general population means previously reported for all adults (mean 50) and for persons age>45 (mean 46.3). Lower adjusted mean PCS score was associated with older age, female sex, higher BMI, lower educational attainment, and smoking history (Table 1). In the CRC survivors in the present study, digestive co-morbidities and self-report of physician diagnosis of diabetes were also associated with lower PCS. Overall, stage at diagnosis was not significantly associated with mean PCS although mean PCS was lower among the few unstaged survivors.
Unadjusted mean (95% CI) MCS score was 54.1 (53.6–54.6) among survivors, somewhat higher than the US general population of all adults (mean 50) and those >45 years old (mean 51.2)[33]. Among the CRC survivors in our sample, higher adjusted mean MCS was associated with older age and male sex (Table 1).
The histogram of PCS scores showed a distinct heavy tail at low values among survivors that was visually distinguishable from the normative curve for the general population and the population over 45 years old (Fig 1). MCS score distributions did not show a similar tail at low values, but did evidence a larger proportion of survivors above comparative population means. Quantitatively, 23% and 5% of survivors had very low (below the value of the lowest decile in the reference population, 37.2) PCS and MCS, respectively.
Fig 1. Distribution of Physical Component Summary (PCS) and Mental Component Summary (MCS) scores among survivors (black bars; bin width is 2 units), and normative reference populations.
Solid line represents the US general population, with normal distribution with mean (standard deviation) of 50 (10). Dashed line represents the US population over age 45 years, with mean PCS 46.3 (10.8) and mean MCS 51.1 (9.6)[14, 15, 33]. Curves have been scaled such that the area under each is equal to the number of participants, 1,021, and the y-axis is the number of survivors in each bar.
Logistic regression results showed that older age, obesity, lower educational attainment, smoking, and co-morbidities or diabetes were associated with higher odds of very low PCS (Table 2). Regional, distant or “unstaged or unknown” stage were progressively associated with higher odds of very low PCS. Higher odds of very low MCS were significantly associated only with smoking, and this association was most pronounced for “current smokers” at enrollment.
Table 2. Associations of survivor personal characteristics with VR-12 Physical Component Summary (PCS) or Mental Component Summary (MCS) score below 10th percentile value in the general population, among CRC survivors approximately 5 years after diagnosis, Seattle Colon Cancer Family Registry (enrolled 1998–2004).
| PCS below 10th percentile (<37.2) | MCS below 10th percentile (<37.2) | |||||
|---|---|---|---|---|---|---|
| ORa | (95% CI) | Pb | ORa | (95% CI) | Pb | |
| Age (y)c | 0.001 | 0.13 | ||||
| <50 | ref | ref | ||||
| 50–59 | 1.34 | (0.82, 2.21) | 0.37 | (0.15, 0.92) | ||
| 60–69 | 1.52 | (0.95, 2.43) | 0.52 | (0.25, 1.10) | ||
| ≥70 | 2.74 | (1.63, 4.62) | 0.69 | (0.29, 1.65) | ||
| Sex | 0.12 | 0.19 | ||||
| Male | ref | ref | ||||
| Female | 1.29 | (0.93, 1.78) | 1.48 | (0.82, 2.67) | ||
| BMI (kg/m2)d | 0.014 | 0.69 | ||||
| <25 | ref | ref | ||||
| 25–29.9 | 1.02 | (0.69, 1.50) | 1.13 | (0.59, 2.16) | ||
| ≥30 | 1.81 | (1.20, 2.74) | 0.80 | (0.34, 1.85) | ||
| Marital Statusc | 0.94 | 0.60 | ||||
| Not married | 0.99 | (0.69, 1.41) | 0.83 | (0.41, 1.66) | ||
| Married or living as married | ref | ref | ||||
| Race | 0.51 | 0.25 | ||||
| White | ref | |||||
| Other | 0.83 | (0.47, 1.46) | 1.71 | (0.69, 4.25) | ||
| Educationc | <0.001 | 0.35 | ||||
| High school or less | 1.58 | (1.10, 2.28) | 1.02 | (0.54, 1.93) | ||
| Some college or technical education | ref | ref | ||||
| College graduate | 0.64 | (0.43, 0.97) | 0.60 | (0.28, 1.29) | ||
| Cigarette Smokingd | <0.001 | 0.04 | ||||
| Never | ref | ref | ||||
| Former | 1.37 | (0.97, 1.96) | 1.60 | (0.78, 3.32) | ||
| Current | 2.79 | (1.65, 4.75) | 3.06 | (1.29, 7.23) | ||
| Colorectal Co-morbiditiesc,e | 0.005 | 0.30 | ||||
| None | ref | ref | ||||
| One or more | 1.75 | (1.19, 2.58) | 1.46 | (0.72, 2.99) | ||
| Diabetesc,f | 0.013 | 0.46 | ||||
| No | ref | |||||
| Yes | 1.81 | (1.13, 2.88) | 1.40 | (0.58, 3.37) | ||
| Stage at Diagnosis | 0.01 | 0.19 | ||||
| Local | ref | ref | ||||
| Regional | 1.22 | (0.88, 1.70) | 1.14 | (0.63, 2.06) | ||
| Distant | 2.61 | (1.08, 6.30) | NEg | |||
| Unstaged or unknown | 3.72 | (1.33, 10.39) | 1.18 | (0.14, 10.01) | ||
| Site of Tumor | 0.45 | 0.80 | ||||
| Colon | ref | ref | ||||
| Rectum | 1.17 | (0.83, 1.66) | 1.20 | (0.66, 2.20) | ||
| Unknown | 1.41 | (0.73, 2.71) | 1.00 | (0.30, 3.29) | ||
a Adjusted for all variables listed.
b P value of joint Wald test of categorical coefficients in the logistic regression model.
c At Colon Cancer Family Registry enrollment.
d Two years prior to baseline interview.
e Self-report of physician diagnosis of colitis, Crohns disease, diverticulitis, or irritable bowel syndrome.
f Self-report of physician diagnosis of diabetes.
g Not estimated (NE); no survivors diagnosed with distant stage reported MCS below the 10th percentile.
Changing the cut-off for very low PCS and MCS to the 5th or 25th percentile values had no substantial impact on the interpretation of results.
During a median of 4.8 years follow-up after completion of the QoL survey (at ≥5 years post-diagnosis), 204 deaths occurred, 59 of which were due to CRC. The mean mortality rate was 44.6 (95% CI: 38.9–51.1) deaths per 1,000 person-years. Differences in overall survival between survivors with PCS or MCS scores <37.2 and survivors with PCS or MCS scores ≥37.2 were evident (Fig 2; log-rank P< 0.0001). A very low PCS score was associated with higher hazard of death (HR (95% CI): 3.97 (2.95, 5.34)), adjusted for MCS score (Table 3), and a very low MCS score was also associated with higher hazard of death (HR (95% CI): 1.98 (1.19, 3.28)) adjusted for PCS score. However, MCS was not significantly associated with mortality among survivors with PCS score above the lowest decile; in contrast, very low PCS was associated with higher risk of death among survivors in either stratum of MCS score (Fig 2 and Table 3).
Fig 2. Kaplan-Meier survival curves comparing survivors by Physical Component Summary (PCS) and Mental Component Summary (MCS) scores.
Table 3. Association of subsequent survival with quality of life Physical Component Summary (PCS) and Mental Component Summary (MCS) score assessed approximately 5 years after colorectal cancer diagnosis.
| PCS | deaths / N | HRa,b | 95% CI | |
| ≥10th %tile | 94 / 783 | ref. | ||
| <10th %tile | 110 / 238 | 3.97 | (2.95, 5.34) | |
| per 10 points lower | 204 / 1021 | 1.71 | (1.53, 1.91) | |
| MCS | deaths / N | HRa,b | 95% CI | |
| ≥10th %tile | 183 / 970 | ref. | ||
| <10th %tile | 21 / 51 | 1.98 | (1.19, 3.28) | |
| per 10 points lower | 204 / 1021 | 1.39 | (1.20, 1.62) | |
| PCS | MCS | deaths / N | HRa | 95% CI |
| ≥10th %tile | ≥10th %tile | 89 / 753 | ref. | |
| ≥10th %tile | <10th %tile | 5 / 30 | 1.67 | (0.78, 3.58) |
| <10th %tile | ≥10th %tile | 94 / 217 | 3.90 | (2.87, 5.30) |
| <10th %tile | <10th %tile | 16 / 21 | 8.24 | (4.26, 15.96) |
a Adjusted for age and sex, and stratified by stage.
b HR for PCS adjusted for MCS category, HR for MCS adjusted for PCS category.
Discussion
In this study, unadjusted average physical QoL was modestly lower, and average mental QoL somewhat higher, than reference values for the general US population [15, 33]. Although an imperfect comparison, the difference in mean PCS score between CRC survivors and the population over 45 years old was approximately 1.2 points, an absolute difference on the VR-12 QoL scale that probably does not represent a meaningfully lower ability to complete daily tasks, and is unlikely to be clinically important[14, 15, 34]. Similarly, the difference of 3 points in mean MCS between survivors and the older general population may not be large enough to be important. Because earlier studies that have demonstrated lower QoL among patients in the year or so following CRC diagnosis[35, 36], our study provides some suggestive evidence that, on average, CRC patients who survive approximately 5 years from diagnosis can expect to return to quality of life typical for their age, in spite of possible continuing challenges stemming from CRC.
Visual inspection of the distribution of PCS and MCS scores among CRC survivors revealed a larger than expected sub-group of survivors with low PCS score. The lowest decile of PCS scores in the general population represents a PCS of 13 or more points below the general population mean of 50, or approximately 9 or more points below the mean PCS for the population over age 45, deficits large enough to reflect a meaningfully lower ability to complete daily tasks and usual activities[14, 15, 17]. We sought to characterize CRC survivors in this group with very low PCS scores. Our results showed that persons diagnosed at an older age, with higher BMI, less education, a history of smoking, and co-morbidities including diabetes may be particularly vulnerable to experiencing low physical QoL. The underlying reasons for lower physical QoL may not be specific to CRC survivorship. Our results nonetheless suggest sub-groups of CRC survivors that may be at higher risk of lingering physical disabilities that interfere with everyday life, and which previously published reports have associated with a higher risk of mortality[16, 17]. Thus continued survivorship support may be especially warranted in these groups.
In contrast to the physical domain of QoL, in the mental domain, CRC survivors qualitatively showed modestly higher QoL than the general population with little evidence of a tail at low values. We identified only cigarette smokers as a risk factor for very low mental QoL. These findings suggest the possibility of “benefit finding” among CRC survivors, as has been observed previously in survivors of disparate cancers including CRC[37, 38].
The characteristics of groups of survivors identified to have lower mean QoL scores, and those with higher odds of very low QoL score, were similar. The association of co-morbidities with odds of very low PCS score was somewhat stronger than might have been expected based on the modest association of co-morbidities with mean PCS score.
Our results regarding mean QoL, and factors associated with differences in mean QoL scores in both mental and physical dimensions, in long-term CRC survivors are largely consistent with previous reports from other studies[2–4, 6, 11]. However, most earlier studies have generally focused on the mean scores, with a few exceptions[7, 8]. Therefore our additional highlighting of the disproportionate number of survivors with “very low” PCS scores represents an under-utilized approach.
Previous reports have found that QoL assessed soon after CRC diagnosis was independently related to survival [19–25]. In our study of long-term CRC survivors, we observed a strong association between QoL, particularly physical QoL score, and risk of mortality. Interestingly, the associations of very low QoL with mortality that we found among CRC survivors were very similar to reports examining the association of QoL with mortality in general population populations [26] and among individuals of comparable age to the CRC survivors in our study years[27, 39–41]. Thus our results suggest that as in the general population, very low QoL identifies long-term CRC survivors at higher risk of death. However, the absolute mortality rate of long-term CRC survivors in the present study was 44.6 deaths per 1,000 years, which was likely higher than the rate in the US general population of comparable age (e.g., approximately 23 and 36 per 1,000 person-years for ages 70–74 years and 75–79 years, respectively [42]), even though the majority of deaths among our study participants were due to causes other than CRC. More research would be necessary to more fully understand differences in mortality between long-term CRC survivors and the general population of comparable age.
Some limitations of our study should be considered in interpreting our results. These include our use of the VR-12, rather than a longer 36-item survey such as the VR-36 or Short Form 36 (SF-36), although given the sample size of our study, the VR-12 has been shown to be adequate to assess the two summary measures of QoL[14, 15, 31]. By using only summary scores from the broadly applicable VR-12, rather than a disease-specific QoL survey, we did not capture in detail specific deficits such as bowel problems. Our study only included survivors who lived at least ~5 years post-diagnosis, but our objective was to examine long-term survivors. However, CRC patients who were alive at the time of the scheduled 5 year follow-up interview but did not respond may have experienced lower QoL. An additional limitation is our lack of detailed data on CRC treatment, but we did include information on stage at diagnosis, and tumor site, factors that are important in determining treatment received. We were also unable to adjust for other potential but unmeasured confounders such as financial status and social support. Finally, reflecting the population underlying the Seattle CCFR, our results included modest numbers of racial or ethnic minorities, and therefore further research is needed to generalize to sub-populations within the US.
In summary, our results show that approximately 5 years after diagnosis, on average, long-term CRC survivors QoL approaches the status of the general population. Nonetheless, some CRC survivors, particularly those with co-morbidities, obese survivors, smokers, older survivors, and survivors with less education, experience very low physical QoL and continued long-term support may be needed to mitigate the association of low QoL with higher risk of death. These important themes should be conveyed in communications with CRC patients, their families, and caregivers.
Data Availability
Due to ethical restrictions regarding patient privacy and consent, data are available upon request. Requests for the data may be sent to either Ms. Rachel Malen (rmalen@fredhutch.org) and Ms. Allyson Templeton (atemplet@fredhutch.org), or to author Dr. Newcomb (pnewcomb@fredhutch.org).
Funding Statement
This work was supported by the National Cancer Institute, National Institutes of Health grant UM1 CA167551 to R.M. Haile to support the Colorectal Cancer Family Registry Cohort infrastructure, grant U01CA074794 to P. A. Newcomb to support the Seattle Colorectal Cancer Family Registry, and grant K05 CA152715 to P. A. Newcomb. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):104–17. Epub 2014/03/19. 10.3322/caac.21220 . [DOI] [PubMed] [Google Scholar]
- 2.Jansen L, Koch L, Brenner H, Arndt V. Quality of life among long-term (>/ = 5 years) colorectal cancer survivors—systematic review. Eur J Cancer. 2010;46(16):2879–88. Epub 2010/07/08. [pii]. . [DOI] [PubMed] [Google Scholar]
- 3.Trentham-Dietz A, Remington PL, Moinpour CM, Hampton JM, Sapp A, Newcomb PA. Health-related quality of life in female long-term colorectal cancer survivors. The Oncologist. 2003;8(4):342–9. [DOI] [PubMed] [Google Scholar]
- 4.Ramsey SD, Berry K, Moinpour C, Giedzinska A, Andersen MR. Quality of life in long term survivors of colorectal cancer. Am J Gastroenterol. 2002;97(5):1228–34. [DOI] [PubMed] [Google Scholar]
- 5.Jansen L, Herrmann A, Stegmaier C, Singer S, Brenner H, Arndt V. Health-related quality of life during the 10 years after diagnosis of colorectal cancer: A population-based study. J Clin Oncol. 2011;29(24):3263–9. Epub 2011/07/20. [pii]. . [DOI] [PubMed] [Google Scholar]
- 6.Soerjomataram I, Thong MS, Ezzati M, Lamont EB, Nusselder WJ, van de Poll-Franse LV. Most colorectal cancer survivors live a large proportion of their remaining life in good health. Cancer Causes Control. 2012;23(9):1421–8. Epub 2012/06/27. 10.1007/s10552-012-0010-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weaver KE, Forsythe LP, Reeve BB, Alfano CM, Rodriguez JL, Sabatino SA, et al. Mental and physical health-related quality of life among u.S. Cancer survivors: Population estimates from the 2010 national health interview survey. Cancer Epidemiol Biomarkers Prev. 2012;21(11):2108–17. Epub 2012/11/01. [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez JL, Hawkins NA, Berkowitz Z, Li C. Factors associated with health-related quality of life among colorectal cancer survivors. Am J Prev Med. 2015;49(6 Suppl 5):S518–27. Epub 2015/11/23. [pii]. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thraen-Borowski KM, Trentham-Dietz A, Edwards DF, Koltyn KF, Colbert LH. Dose-response relationships between physical activity, social participation, and health-related quality of life in colorectal cancer survivors. J Cancer Surviv. 2013;7(3):369–78. Epub 2013/04/03. 10.1007/s11764-013-0277-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buffart LM, Thong MS, Schep G, Chinapaw MJ, Brug J, van de Poll-Franse LV. Self-reported physical activity: Its correlates and relationship with health-related quality of life in a large cohort of colorectal cancer survivors. PLoS One. 2012;7(5):e36164 Epub 2012/05/09. [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sapp AL, Trentham-Dietz A, Newcomb PA, Hampton JM, Moinpour CM, Remington PL. Social networks and quality of life among female long-term colorectal cancer survivors. Cancer. 2003;98(8):1749–58. [DOI] [PubMed] [Google Scholar]
- 12.Mosher CE, Sloane R, Morey MC, Snyder DC, Cohen HJ, Miller PE, et al. Associations between lifestyle factors and quality of life among older long-term breast, prostate, and colorectal cancer survivors. Cancer. 2009;115(17):4001–9. Epub 2009/07/29. 10.1002/cncr.24436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newcomb PA, Baron J, Cotterchio M, Gallinger S, Grove J, Haile R, et al. Colon cancer family registry: An international resource for studies of the genetic epidemiology of colon cancer. Cancer Epidemiol Biomarkers Prev. 2007;16(11):2331–43. . [DOI] [PubMed] [Google Scholar]
- 14.Selim AJ, Rogers W, Fleishman JA, Qian SX, Fincke BG, Rothendler JA, et al. Updated u.S. Population standard for the veterans rand 12-item health survey (vr-12). Qual Life Res. 2009;18(1):43–52. Epub 2008/12/04. 10.1007/s11136-008-9418-2 . [DOI] [PubMed] [Google Scholar]
- 15.Ware J Jr., Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. Epub 1996/03/01. . [DOI] [PubMed] [Google Scholar]
- 16.Ware JE, Kosinski M. Interpreting sf-36 summary health measures: A response. Qual Life Res. 2001;10(5):405–13; discussion 15–20. Epub 2002/01/05. . [DOI] [PubMed] [Google Scholar]
- 17.Ware JE Jr, Snow KK, Kosinski M, Gandek B. Sf-36 health survey manual and interpretation guide. Boston, MA: The Health Institute, New England Medical Center; 1993. [Google Scholar]
- 18.Yost KJ, Cella D, Chawla A, Holmgren E, Eton DT, Ayanian JZ, et al. Minimally important differences were estimated for the functional assessment of cancer therapy-colorectal (fact-c) instrument using a combination of distribution- and anchor-based approaches. J Clin Epidemiol. 2005;58(12):1241–51. Epub 2005/11/18. S0895-4356(05)00249-0 [pii] 10.1016/j.jclinepi.2005.07.008 . [DOI] [PubMed] [Google Scholar]
- 19.Gotay CC, Kawamoto CT, Bottomley A, Efficace F. The prognostic significance of patient-reported outcomes in cancer clinical trials. J Clin Oncol. 2008;26(8):1355–63. Epub 2008/01/30. [pii]. . [DOI] [PubMed] [Google Scholar]
- 20.Efficace F, Bottomley A, Coens C, Van Steen K, Conroy T, Schoffski P, et al. Does a patient's self-reported health-related quality of life predict survival beyond key biomedical data in advanced colorectal cancer? Eur J Cancer. 2006;42(1):42–9. Epub 2005/11/22. S0959-8049(05)00846-4 [pii] 10.1016/j.ejca.2005.07.025 . [DOI] [PubMed] [Google Scholar]
- 21.Fournier E, Jooste V, Woronoff AS, Quipourt V, Bouvier AM, Mercier M. Health-related quality of life is a prognostic factor for survival in older patients after colorectal cancer diagnosis: A population-based study. Dig Liver Dis. 2015. Epub 2015/10/24. S1590-8658(15)00619-2 [pii] 10.1016/j.dld.2015.09.006 . [DOI] [PubMed] [Google Scholar]
- 22.Diouf M, Chibaudel B, Filleron T, Tournigand C, Hug de Larauze M, Garcia-Larnicol ML, et al. Could baseline health-related quality of life (qol) predict overall survival in metastatic colorectal cancer? The results of the gercor optimox 1 study. Health Qual Life Outcomes. 2014;12:69 Epub 2014/06/03. [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma A, Walker LG, Monson JR. Baseline quality of life factors predict long term survival after elective resection for colorectal cancer. Int J Surg Oncol. 2013;2013:269510 Epub 2013/12/27. 10.1155/2013/269510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Montazeri A. Quality of life data as prognostic indicators of survival in cancer patients: An overview of the literature from 1982 to 2008. Health Qual Life Outcomes. 2009;7:102 Epub 2009/12/25. 10.1186/1477-7525-7-102 1477-7525-7-102 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong CK, Law WL, Wan YF, Poon JT, Lam CL. Health-related quality of life and risk of colorectal cancer recurrence and all-cause death among advanced stages of colorectal cancer 1-year after diagnosis. BMC Cancer. 2014;14:337 Epub 2014/06/03. [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ul-Haq Z, Mackay DF, Pell JP. Association between physical and mental health-related quality of life and adverse outcomes; a retrospective cohort study of 5,272 scottish adults. BMC Public Health. 2014;14:1197 Epub 2014/11/25. [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsai SY, Chi LY, Lee CH, Chou P. Health-related quality of life as a predictor of mortality among community-dwelling older persons. Eur J Epidemiol. 2007;22(1):19–26. Epub 2007/01/12. 10.1007/s10654-006-9092-z . [DOI] [PubMed] [Google Scholar]
- 28.Coghill AE, Newcomb PA, Campbell PT, Burnett-Hartman AN, Adams SV, Poole EM, et al. Prediagnostic non-steroidal anti-inflammatory drug use and survival after diagnosis of colorectal cancer. Gut. 2011;60(4):491–8. Epub 2010/11/06. gut.2010.221143 [pii] 10.1136/gut.2010.221143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phipps AI, Baron J, Newcomb PA. Prediagnostic smoking history, alcohol consumption, and colorectal cancer survival: The seattle colon cancer family registry. Cancer. 2011;117(21):4948–57. Epub 2011/04/16. 10.1002/cncr.26114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kazis LE, Miller DR, Clark JA, Skinner KM, Lee A, Ren XS, et al. Improving the response choices on the veterans sf-36 health survey role functioning scales: Results from the veterans health study. J Ambul Care Manage. 2004;27(3):263–80. Epub 2004/08/04. . [DOI] [PubMed] [Google Scholar]
- 31.Jenkinson C, Layte R, Jenkinson D, Lawrence K, Petersen S, Paice C, et al. A shorter form health survey: Can the sf-12 replicate results from the sf-36 in longitudinal studies? J Public Health Med. 1997;19(2):179–86. Epub 1997/06/01. . [DOI] [PubMed] [Google Scholar]
- 32.Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. How to score version 2 of the sf-12 health survey (with a supplement documenting version 1): QualityMetric Incorporated; 2002.
- 33.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of item selection and scoring for the sf-12 health survey in nine countries: Results from the iqola project. International quality of life assessment. J Clin Epidemiol. 1998;51(11):1171–8. Epub 1998/11/17. S0895435698001097 [pii]. . [DOI] [PubMed] [Google Scholar]
- 34.Jones D, Kazis L, Lee A, Rogers W, Skinner K, Cassar L, et al. Health status assessments using the veterans sf-12 and sf-36: Methods for evaluating otucomes in the veterans health administration. J Ambul Care Manage. 2001;24(3):68–86. Epub 2001/07/04. . [DOI] [PubMed] [Google Scholar]
- 35.Arndt V, Merx H, Stegmaier C, Ziegler H, Brenner H. Quality of life in patients with colorectal cancer 1 year after diagnosis compared with the general population: A population-based study. J Clin Oncol. 2004;22(23):4829–36. Epub 2004/12/01. 22/23/4777 [pii] 10.1200/JCO.2004.02.018 . [DOI] [PubMed] [Google Scholar]
- 36.Yost KJ, Hahn EA, Zaslavsky AM, Ayanian JZ, West DW. Predictors of health-related quality of life in patients with colorectal cancer. Health Qual Life Outcomes. 2008;6:66 Epub 2008/08/30. [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harding S, Sanipour F, Moss T. Existence of benefit finding and posttraumatic growth in people treated for head and neck cancer: A systematic review. PeerJ. 2014;2:e256 Epub 2014/04/02. [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jansen L, Hoffmeister M, Chang-Claude J, Brenner H, Arndt V. Benefit finding and post-traumatic growth in long-term colorectal cancer survivors: Prevalence, determinants, and associations with quality of life. Br J Cancer. 2011;105(8):1158–65. Epub 2011/09/01. [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brown DS, Thompson WW, Zack MM, Arnold SE, Barile JP. Associations between health-related quality of life and mortality in older adults. Prev Sci. 2015;16(1):21–30. Epub 2013/11/06. 10.1007/s11121-013-0437-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kroenke CH, Kubzansky LD, Adler N, Kawachi I. Prospective change in health-related quality of life and subsequent mortality among middle-aged and older women. Am J Public Health. 2008;98(11):2085–91. Epub 2008/05/31. [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dominick KL, Ahern FM, Gold CH, Heller DA. Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clin Exp Res. 2002;14(6):499–508. Epub 2003/04/04. . [DOI] [PubMed] [Google Scholar]
- 42.Kochanek KD, Murphy SL, Xu J. Deaths: Final data for 2011. Natl Vital Stat Rep. 2015;63(3):1–120. Epub 2015/07/30. . [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to ethical restrictions regarding patient privacy and consent, data are available upon request. Requests for the data may be sent to either Ms. Rachel Malen (rmalen@fredhutch.org) and Ms. Allyson Templeton (atemplet@fredhutch.org), or to author Dr. Newcomb (pnewcomb@fredhutch.org).