Abstract
There continues to be considerable public debate on the possible benefits regarding the growing popularity of the consumption of raw milk. However, there are significant concerns by regulatory, or public health, organizations like the Food and Drug Administration and the Centers for Disease Control and Prevention because of risk of contracting milkborne illnesses if the raw milk is contaminated with human pathogens. This review describes why pasteurization of milk was introduced more than 100 years ago, how pasteurization helped to reduce the incidence of illnesses associated with raw milk consumption, and the prevalence of pathogens in raw milk. In some studies, up to a third of all raw milk samples contained pathogens, even when sourced from clinically healthy animals or from milk that appeared to be of good quality. This review critically evaluates some of the popularly suggested benefits of raw milk. Claims related to improved nutrition, prevention of lactose intolerance, or provision of “good” bacteria from the consumption of raw milk have no scientific basis and are myths. There are some epidemiological data that indicate that children growing up in a farming environment are associated with a decreased risk of allergy and asthma; a variety of environmental factors may be involved and there is no direct evidence that raw milk consumption is involved in any “protective” effect.
BACKGROUND
In 1908, Chicago became the first US city to introduce cow’s milk pasteurization into municipal law (except for cows that were certified tuberculosis-free). However, it took another 8 years before it was fully adopted in Chicago owing to political wrangling and a debate over “pure milk” (raw milk) versus “purified milk” (pasteurized milk).1 Around that time, public health officials became greatly worried about the transmission of bovine tuberculosis from cow’s milk to humans. By 1900, it was estimated that as many as 10% of all tuberculosis cases in humans were caused by infection via milk consumption, and in 1910, a tuberculosis epidemic spread through Illinois, infecting over 300 000 cattle.1 Certification of herds as tuberculosis-free became very difficult to manage/administer, and pasteurization became increasingly popular because of its ability to process large quantities of milk in a cost-effective approach. Tuberculosis was 1 of the major human health concerns of the early part of the last century; for example, between 1912 and 1937, it is estimated that about 65 000 persons in England and Wales died of tuberculosis that originated from bovine sources.2
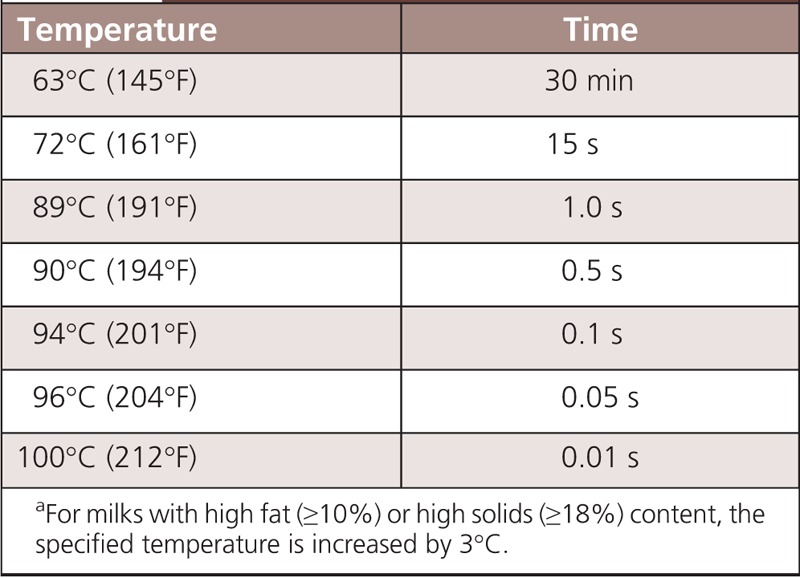
In 1924, the US Public Health Service developed a regulation known as the Standard Milk Ordinance for voluntary adoption by state and local agencies; this is now called the Grade “A” Pasteurized Milk Ordinance (PMO).3 Pasteurization is defined as “the process of heating every particle of milk or milk product, in properly designed and operated equipment, to any 1 of the specified pasteurization time/temperature combinations.”3 These time-temperature combinations are designed to destroy all human pathogens, and the most common pasteurization treatment is rapidly heating milk to not less than 72°C and holding that temperature for at least 15 seconds (Table 1).3 In some countries, milks are subjected to higher (ultra) heat treatments (eg, 138°C for 2–4 seconds); if the product is packaged normally, then this milk is called ultrapasteurized; if the process is done aseptically, then the milk can be stored at ambient temperature, this product is called ultra-high temperature (UHT). In the subsequent decades, more states started to use the PMO approach. If we look back to just before World War II, in 1938, it was estimated that milkborne outbreaks constituted 25% of all disease outbreaks (related to food/water) in the United States. Today, with the widespread use of pasteurization and other sanitation procedures outlined in the PMO, milk and fluid milk products account for less than 1% of reported outbreaks caused by food/water consumption.3 Today, tuberculosis is a forgotten disease in the United States because of the success of eradication programs and the implementation of milk pasteurization. There is an ongoing popular debate about the risks and potential benefits from the consumption of raw milk. A significant number (3.4%) of US consumers were recently reported to consume raw milk.4 The objective of this review is to discuss what are the scientifically demonstrated microbiological (health) risks and to determine if there are any proven health/nutritional benefits to the consumption of raw milk.
TABLE 1.
Pasteurization of Milk Involves Heating Milka to 1 of the Temperatures Listed Below and Holding at that Temperature for the Minimum Specified Time3
RISK: PRESENCE OF HUMAN PATHOGENS
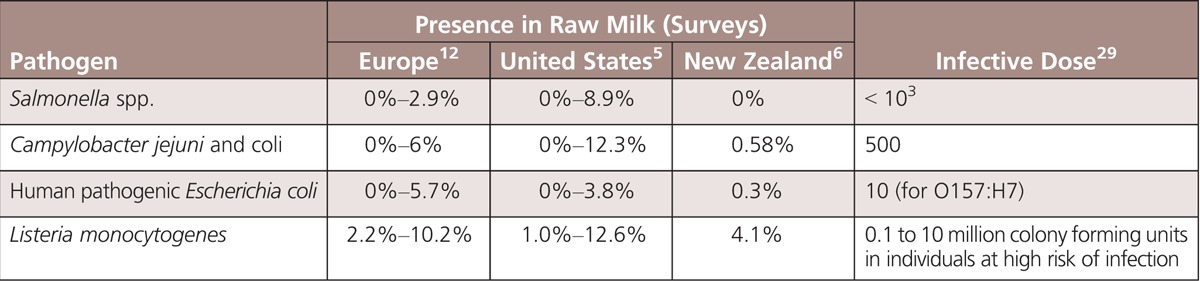
Surveys from various countries have monitored the presence of different types of pathogens in raw milk, with prevalence levels as high as 13% for bacteria like Campylobacter jejuni and Listeria monocytogenes (Table 2). In some studies, almost a third of all milk samples contained at least 1 type of pathogen.5 Thus, we must assume that raw milk is likely to contain pathogens. The prevalence of pathogens in milk is influenced by numerous factors, including farm size, number of animals on the farm, hygiene, farm management practices, milking facilities, season, and others.5 Raw milk can be contaminated with pathogens even when sourced from clinically healthy animals.6 Even milk that appears to be of good quality (ie, low total bacteria count) may contain pathogens.5,7 There are at least 4 different mechanisms by which raw milk becomes contaminated by pathogens: direct passage from the blood (of the cow) into milk (systemic infection), mastitis (udder infection), fecal contamination (external contamination of milk from the environment during or after milking), or contamination from human skin. Dairy farms are an important reservoir of various foodborne pathogens.8 The relative importance of the various sources of contamination depends on the farming practices and may be different for each pathogen.6 Pathogens are not visible to the naked eye, and measurements of their numbers can take several days to complete, so it can be extremely difficult to determine the safety of raw milk before that milk has been consumed. Occasional testing of raw milk does not guarantee that pathogens are absent from the milk supply on days when no testing is done (eg, because of possible contamination during a single milking occasion). Ensuring the safety of raw milk by occasional testing is difficult because of the following5:
TABLE 2.
Prevalence of Human Pathogens in Raw Milk According to Different Studies and Their Likely Infective Dose (by Ingestion of Contaminated Food)
Difficulties in having sufficient sampling since contamination of milk may be sporadic, and bacterial loads can vary from day to day (ie, sampling and testing every day provides more confidence to a claim of safety).
Bacteria/spores are often associated with the fat phase and are not evenly distributed in milk.
It is possible that the number of organisms (pathogens) present is too low to be detected by the test method but the numbers may be sufficient to cause illness if the effective dose is low (which is the case for several key pathogens; see Table 1).
There might have been very low initial numbers of a pathogen, which were below the limits of the test method at the time of sampling, but the pathogen might grow if milk was stored improperly.
It is impossible to test for every single different type of human pathogen.
Raw milk has frequently been identified as the source of foodborne illness outbreaks. US statistics for dairy-associated outbreaks of human disease during the period 1993–2006 have been reviewed.9 There were 121 dairy product outbreaks where the pasteurization status was known; among these, 73 (60%) involved raw milk products and resulted in 1571 reported cases, 202 hospitalizations, and 2 deaths. A total of 55 (75%) outbreaks occurred in the 21 states that permitted the sale of raw milk. States that restricted the sale of raw milk had fewer outbreaks and illnesses. In an updated report covering the 6-year period from 2007 to 2012, the average number of outbreaks associated with nonpasteurized milk was 4-fold higher during this 6-year period (average 13.5 outbreaks/year) than that reported in the previous review of outbreaks during 1993–2006.10 Even in states where raw milk sales are illegal, outbreaks due to the consumption of raw milk have been tracked; for example, between 1998 and 2009, in Wisconsin, there were 6 outbreaks resulting in 261 reported cases and 27 hospitalizations.11
However, the number of illnesses investigated as part of well-documented outbreaks likely only represents a small proportion (tip of the iceberg) of the actual number of illnesses associated with raw milk consumption. For example, analysis of routine surveillance data in Minnesota during 2001–2010 revealed that 3.7% of patients with sporadic, domestically acquired enteric infections had reported raw milk consumption during their exposure period.12 Children were disproportionately affected, and 76% of those younger than 5 years were served raw milk from their own or a relative’s farm.12 During the study period, the number of patients with sporadic laboratory-confirmed infections who reported raw milk consumption was 25 times greater than the number of raw milk–associated outbreak cases among Minnesota residents. Furthermore, they estimated that up to 20 500 Minnesotans, or 17% of raw milk consumers, may have become ill with enteric pathogens during the study period after they consumed raw milk.12
SUGGESTED HEALTH BENEFITS
A number of different claims have been made about the possible health benefits that could hypothetically be derived from the consumption of raw milk. Recent scientific reviews by various international groups have concluded that there was no reliable scientific evidence to support any of these suggested health benefits.13–15
Nutritional
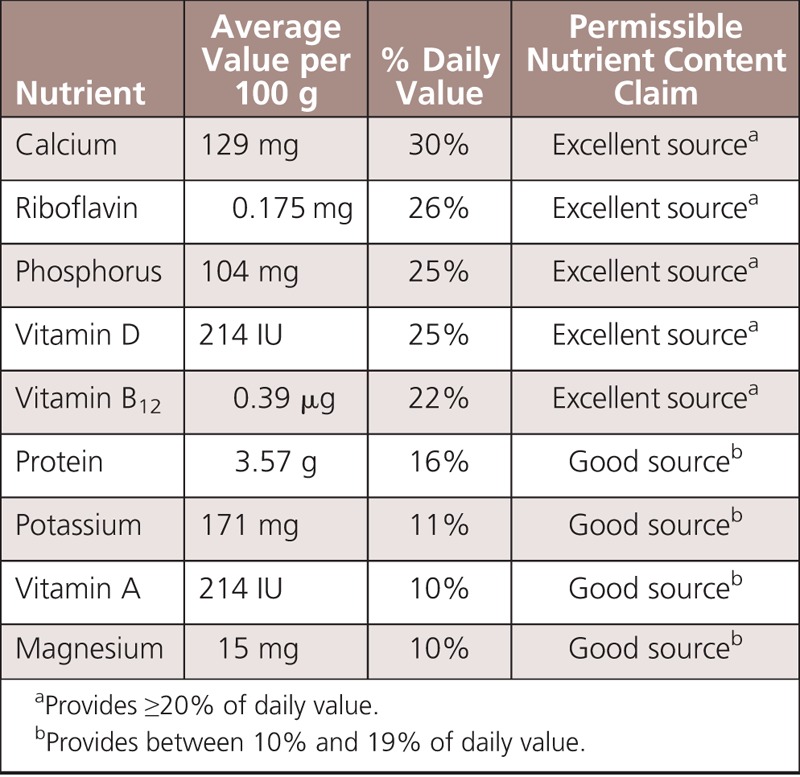
During pasteurization, there is no significant change in the nutritional quality of milk.16 Pasteurization does not cause any change in protein quality; minor levels (<7%) of denaturation of whey proteins have been reported due to pasteurization, but protein denaturation has no impact on protein nutritional quality. Pasteurization does not cause any change in the concentrations of minerals; minerals are very heat stable. Pasteurization may cause very minor losses (<10%) of vitamin C, folate (vitamin B9), vitamin B12, vitamin B6, and thiamine (vitamin B1). Of these vitamins, milk is an excellent source of only vitamin B12; milk has only low concentrations of most of the vitamins listed previously, which might show some minor losses on pasteurization. Pasteurization does not change the concentration of riboflavin (B2) (which is very heat stable) or fat-soluble vitamins like vitamin A or E.15 Other factors like type of packaging material, light exposure, and storage time/temperature have much larger impacts on vitamin losses in milk. Feed (like pasture grazing) can greatly influence milk composition, and sometimes proponents of raw milk confuse feed-related changes in milk composition with those caused directly by pasteurization. Other milk-processing approaches, like ultra-pasteurization and ultra-high temperature, have only a minor impact on the nutritional quality of milk.13
Allergy
Food allergy is an abnormal immunological response due to sensitization to a particular food (usually a protein). Cow’s milk proteins can trigger an immunoglobulin E–mediated reaction in patients called cow’s milk protein allergy (CMA). Young infants usually outgrow this allergy within the first year of life. Young infants may be more susceptible to CMA owing to their milder digestive systems (weaker pepsin/enzyme activity, higher stomach pH), which exposes them to more allergic responses from “intact” proteins or larger peptide sequences.17 In children with CMA, neither raw milk, unhomogenized and pasteurized milk, or homogenized and pasteurized milk was tolerated by CMA patients.18 It can also be mentioned that epidemiological data indicate that the dietary intake of pasteurized milk is not correlated with any increased risk of the development of respiratory allergies or atopic dermatitis.19
Several epidemiological studies have shown that growing up in a farming environment is associated with a decreased risk of allergy and asthma.20–22 A possible factor that has been hypothesized as being involved in this effect is the early ingestion of raw cow’s milk. One issue is that at the farm level, milk is either consumed raw or boiled (heated in a pot or container until the milk boils); boiling is a much more severe heat treatment than the mild pasteurization process used commercially. It is not clear why there would be much difference in the allergenicity of cow’s milk proteins from raw milk or from a mild heating process like pasteurization, which causes only minimal modification/denaturation of (the allergic) milk proteins.17 Loss et al22 hypothesized that any possible protective effect of raw or mildly heated (eg, pasteurized) milk on asthma might be associated with the whey protein fraction of milk, which would be impaired when farm milk was severely boiled (heating to >85°C).
The intestinal microbiome is getting significant attention for its potential impact on human health. This complex microflora is initially developed during infancy, and many factors, including the type of milk consumed (breast, raw, pasteurized), could influence this system, which in turn could impact the sensitivity of an infant to the development of allergy.23 It is important to note that most health organizations recommend that babies be exclusively breastfed for about the first 6 months of life.
It is known that farm kids also come into contact with a wider range of bacteria/allergens compared with children who live in modern cities. It is possible that early exposure to these farm allergens could help some infants develop a more robust immune system. Microorganisms have been identified from the farming environment (eg, barns and milk houses) that have been reported to have an allergy-protective effect.24 It should be noted that there would be considerable ethical concerns with intentionally exposing infants to raw milk in an attempt to try to boost their immune function because of the fact that human pathogens are routinely found in raw milk.20
Recently, using a murine model of gastrointestinal allergy, Hodgkinson et al25 demonstrated that drinking milks exposed to different treatments (raw, gamma-sterilized or heat treated) changed the allergic responses to a nonrelated dietary antigen. However, they found that the group fed raw milk had a greater allergic response than did those fed heated milk. Thus, at present, there is no direct evidence of any beneficial impact of raw milk consumption for CMA, but this topic needs further study.
Lactose Intolerance (Raw Milk Enzymes)
All types of milks (including human or breast milk) contain the sugar lactose, and when we consume milk, the lactase enzyme (β-galactosidase) hydrolyzes it into glucose and galactose, which are then absorbed by the body. Many individuals lose the ability to digest lactose as they age, and they can develop a condition known as lactose intolerance, in which people have digestive symptoms—such as bloating, diarrhea, and gas—after eating or drinking milk or milk products. One of the claims made about raw milk is that it alleviates lactose intolerance. A recent randomized controlled study found that raw milk failed to reduce lactose malabsorption or lactose intolerance symptoms compared with pasteurized milk among adults positive for lactose malabsorption.26 Because there is no β-galactosidase enzyme present in raw milk, there is no obvious reason why raw milk could assist with lactose intolerance. Yogurts, which contain high levels of bacteria that have this β-galactosidase enzyme, are tolerated better by individuals with lactose intolerance.
Although raw milk contains low levels of some proteases and lipases, no physiological role in human digestion has been demonstrated for these enzymes. Both the indigenous milk proteinase (plasmin) and lipase (lipoprotein lipase) are relatively heat stable, so there would be little loss of activity in pasteurized milk relative to raw milk. Anyway, raw milk enzymes are likely degraded/hydrolyzed in the human digestion system (due to the stomach acid, pepsin, etc).
Beneficial Microflora and Antibacterial Systems
Some media reports claim that raw milk is healthy because of the presence of “good bacteria.” Probiotics are defined as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host.”27 Some lactic acid bacteria are considered probiotics. However, key probiotic bacteria like Bifidobacteria or Lactobacillus acidophilus should be present only at quite low levels in raw bovine milk, as they do not compete well with the more common types of lactic acid bacteria. Instead Bifidobacteria are found at high numbers in the gastrointestinal tract of cows and humans, and the presence of Bifidobacteria in raw milk has been used as possible indicator of fecal contamination.28 When probiotic cultures are used in commercial products like yogurt, it is considered highly desirable that (a) the specific probiotic strain used was originally isolated from a human source (not from animals like cows), and (b) the specific strain conveys proven health benefits when used at high levels (ie, millions of colony forming units per milliliter). None of these conditions are met with any fecal contamination of raw milk by probiotic bacteria.
There are a number of potential antimicrobial systems in milk, including lactoferrin, lactoperoxidase, lysozyme, bovine immunoglobulin, bacteriocins, oligosaccharides, and xanthine oxidase. Lactoperoxidase and lysozyme retain 70% or more of their activity in pasteurized milk, whereas the other components listed above retain all their activity in pasteurized milk.5 Collectively, these antimicrobial systems are unable to prevent pathogen growth in raw milk. Mastitic milk often contains elevated levels of lactoferrin and immunoglobulins, which would indicate that the milk is infected and these antibacterial systems are elevated to help fight this bacterial infection.
At the farm level, prudent steps that can be taken by the farmer to reduce pathogen numbers in their raw milk include minimizing fecal/pathogen contamination and maintaining low storage temperatures to reduce growth of pathogens.
In conclusion, raw milk is not inherently safe and carries a significant food poisoning risk with its consumption.5,6 There is no evidence that raw milk has any inherent health or nutritional benefits those media claims were shown to be myths. Pasteurized milk has an excellent food safety record and remains an important dietary source for many important nutrients (Table 3), especially for children and young adults.29
TABLE 3.
Nutritional Content of Fat-Free Milk, Fortified With Vitamins A and D (Serving Size: 1 cup)30
Footnotes
The authors have no conflicts of interest to disclose.
REFERENCES
- 1. Czaplicki A. “Pure milk is better than purified milk”: pasteurization and milk purity in Chicago, 1908–1916. Soc Sci History. 2007; 31: 411– 433. [Google Scholar]
- 2. Wilson GS. The pasteurization of milk. Br Med J. 1943; 1( 4286): 261– 262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Grade “A” Pasteurized Milk Ordinance, US Department of Health and Human Services. 2009.
- 4. Buzby JC, Gould LH, Kendall ME, et al. Characteristics of consumers of unpasteurized milk in the United States. J Consum Aff. 2013; 47: 153– 166. [Google Scholar]
- 5. Griffiths MW. The microbiological safety of raw milk. In: Griffiths MW, ed. Improving the Safety and Quality of Milk, Volume 1: Milk Production and Processing. Boca Raton, FL: CRC Press; 2010: 27– 63. [Google Scholar]
- 6. Soboleva T. Assessment of the microbiological risks associated with the consumption of raw milk. MPI Technical Paper No. 2014/12. http://www.foodsafety.govt.nz/elibrary/industry/raw-milk-sales-2014/2014-12-microbiological-risks-assessment-consumption-of-raw-milk.pdf. Accessed November 25, 2014.
- 7. Desmasures NF, Bazin F, Gueguen M. Microbiological composition of raw milk from selected farms in the Camembert region of Normandy. J Appl Microbiol. 1997; 83: 53– 58. [DOI] [PubMed] [Google Scholar]
- 8. Oliver SP, Jayarao BM, Almeida RA. Foodborne pathogens in milk and the dairy farm environment: food safety and public health implications. Foodborne Pathog Dis. 2005; 2: 115– 129. [DOI] [PubMed] [Google Scholar]
- 9. Langer AJ, Ayers T, Grass J, et al. Nonpasteurized dairy products, disease outbreaks, and state laws-United States, 1993–2006. Emerg Infect Dis. 2012; 18: 385– 391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mungai EA, Behravesh CB, Gould LH. Increased outbreaks associated with nonpasteurized milk, United States, 2007–2012. Emerg Infect Dis. 2015; 21: 119– 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barrows R. Report of the raw milk policy working group. Department of Agriculture, Trade, and Consumer Protection. http://datcp.wi.gov/uploads/Food/pdf/WorkingGroupReport.pdf. Accessed November 25, 2014.
- 12. Robinson TJ, Scheftel JM, Smith KE. Raw milk consumption among patients with non–outbreak-related enteric infections, Minnesota, USA, 2001–2010. Emerg Infect Dis. 2014; 20: 38– 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Claeys WL, Cardoen S, Daube G, et al. Raw or heated cow milk consumption: review of risks and benefits. Food Control. 2013; 31: 251– 262. [Google Scholar]
- 14.Anonymous. An assessment of the effects of pasteurization on claimed nutrition and health benefits of raw milk. MPI Technical Paper No. 2014/13. http://www.foodsafety.govt.nz/elibrary/industry/2014-13-Assessment-of-effects-of-Pasteurisation-on-Claimed-Nutrition-and-Health-Benefits-of-Raw-Milk.pdf. Accessed November 25, 2014.
- 15. MacDonald LE, Brett J, Kelton D, et al. A systematic review and meta-analysis of the effects of pasteurization on milk vitamins, and evidence for raw milk consumption and other health-related outcomes. J Food Prot. 2001; 74: 1814– 1832. [DOI] [PubMed] [Google Scholar]
- 16. Andersson I, Oste R. Nutritional quality of heat processed liquid milk. In: Fox PF, ed. Heat-Induced Changes in Milk. 2nd ed Brussels, Belgium: International Dairy Federation; 1995: 279– 307. [Google Scholar]
- 17. Monaci L, Tregoat V, Hengel AJ, Anklam E. Milk allergens, their characteristics and their detection in food: a review. Eur Food Res Tech. 2006; 223: 149– 179. [Google Scholar]
- 18. Host A, Samuelsson EG. Allergic reactions to raw, pasteurized, and homogenized/pasteurized cow milk: a comparison. Allergy. 1988; 43: 113– 118. [DOI] [PubMed] [Google Scholar]
- 19. Wijga AH, Smit HA, Kerkhof M, et al. Association of consumption of products containing milk fat with reduced asthma risk in pre-school children: the PIAMA birth cohort study. Thorax. 2003; 58: 567– 572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van Neerven RJJ, Knol EF, Heck JML, et al. Which factors in raw cow’s milk contribute to protection against allergies? J Allergy Clin Immunol. 2012; 130: 853– 858. [DOI] [PubMed] [Google Scholar]
- 21. Braun-Fahrländer C, von Mutius E. Can farm milk consumption prevent allergic diseases? Clin Exp Allergy. 2010; 41: 29– 35. [DOI] [PubMed] [Google Scholar]
- 22. Loss G, Apprich S, Waser M, et al. The protective effect of farm milk consumption on childhood asthma and atopy: the GABRIELA study. J Allergy Clin Immunol. 2011; 128: 766– 773. [DOI] [PubMed] [Google Scholar]
- 23. Madan JC, Farzan SF, Hibberd PL, Karagas MR. Normal neonatal microbiome variation in relation to environmental factors, infection and allergy. Curr Opin Pediatr. 2012; 24: 753– 759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Debarry J, Garn H, Hanuszkiewicz A, et al. Acinetobacter lwoffii and Lactococcus lactis strains isolated from farm cowsheds possess strong allergy-protective properties. J Allergy Clin Immunol. 2007; 119: 1514– 1521. [DOI] [PubMed] [Google Scholar]
- 25. Hodgkinson AJ, McDonald NA, Hine B. Effect of raw milk on allergic responses in a murine model of gastrointestinal allergy. Br J Nutr. 2014; 112: 390– 397. [DOI] [PubMed] [Google Scholar]
- 26. Mummah S, Oelrich B, Hope J, et al. Effect of raw milk on lactose intolerance: a randomized controlled pilot study. Ann Fam Med. 2014; 12: 134– 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hill C, Guarner F, Reid G, et al. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014; 11: 506– 514. [DOI] [PubMed] [Google Scholar]
- 28. Beerens H, de la Perriere HB, Gravini F. Evaluation of the hygienic quality of raw milk based on the presence of bifidobacteria: the cow as a source of faecal contamination. Int J Food Microbiol. 2000; 54: 163– 169. [DOI] [PubMed] [Google Scholar]
- 29.Pathogen Safety Data Sheets and Risk Assessment. Public Health Agency of Canada. http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/index-eng.php. Accessed on November 25, 2014.
- 30.USDA National Nutrient Database for Standard Release 27 (2011). http://ndb.nal.usda.gov/. Accessed on November 25, 2014.


