Abstract
Objective
Conduct a pilot trial testing whether a new cognitive-behavioral (CB) group prevention program that incorporated cognitive-dissonance change principles was feasible and appeared effective in reducing depressive symptoms and major depressive disorder onset relative to a brochure control condition in college students with elevated depressive symptoms.
Method
59 college students (M age = 21.8, SD = 2.3; 68% female, 70% White) were randomized to the 6-session Change Ahead group or educational brochure control condition, completing assessments at pretest, posttest, and 3-month follow-up.
Results
Recruitment and screening methods were effective and intervention attendance was high (86% attended all 6 sessions). Change Ahead participants showed medium-large reductions in depressive symptoms at posttest (M d = .64), though the effect attenuated by 3-month follow-up. Incidence of major depression onset at 3-month follow-up was 4% for Change Ahead participants versus 13% (difference ns).
Conclusions
Change Ahead appears highly feasible and showed positive indications of reduced acute phase depressive symptoms and MDD onset relative to a minimal intervention control in this initial pilot. Given the brevity of the intervention, its apparent feasibility, and the lack of evidence-based depression prevention programs for college students, continued evaluation of Change Ahead appears warranted.
Keywords: depression, prevention, cognitive-behavioral, cognitive dissonance, college students
Major depressive disorder (MDD) in young people is common, recurrent, and impairing (Klein, Torpey, & Bufferd, 2008). However, 60-81% of depressed young people do not receive treatment (Cummings & Druss, 2011), underscoring the need for effective depression prevention programs. Several depression prevention interventions for young people, predominantly focused on high school samples, have been developed, with cognitive-behavioral (CB) prevention interventions having the largest evidence base (e.g., Stice, Shaw, Bohon, Marti, & Rohde, 2009). However, the average depressive symptom reductions by post (d = .30) and follow-up (d = .22) were small in magnitude and only 13% of trials significantly reduced future MDD onset (Stice et al., 2009).
We conducted an efficacy trial in which 341 high school students with elevated depressive symptoms were randomized to CB group, supportive expressive group, CB bibliotherapy, or brochure control (Stice, Rohde, Seeley, & Gau, 2008). At post, CB group participants showed significantly lower depressive symptoms than both active control conditions and brochure control. By 2-yr follow-up, MDD onset was significantly lower for CB group (14%) and bibliotherapy (3%) than brochure controls (23%); results for supportive expressive group were intermediate (15%). Based on these promising results, an effectiveness trial was conducted, in which high school personnel recruited 378 students with elevated depressive symptoms and delivered the CB group intervention, compared to CB bibliotherapy and brochure control (Rohde, Stice, Shaw, & Brière, 2014a; Rohde, Stice, Shaw, & Gau, 2015). At post, CB group resulted in lower symptoms than brochure control (results for CB bibliotherapy were intermediate). By 2-yr follow-up, CB group participants showed significantly lower MDD onset (10%) versus bibliotherapy (25%) though effects relative to brochure controls (17%) were nonsignificant (p = .15).
Given the generally encouraging results with high school students, we explored the impact of group and bibliotherapy CB interventions in a college sample with a design that paralleled the effectiveness trial (Rohde, Stice, Shaw, & Gau, 2014b). Depression is one of the most common mental health problems among college students (American College Health Association, 2012), a high-risk population for which effective prevention programs have been elusive (e.g., Garlow et al., 2008). Though college students are sometimes viewed as a privileged population, more than 65% of US high school graduates attend some form of post-high school education (US Department of Education, 2008). Further, the prevalence of unipolar depressive disorders appears comparable for college and non-college-attending young adults (Blanco et al., 2008), as do low levels of mental health treatment utilization (American College Health Association, 2008). In this pilot, 82 college students with elevated depressive symptoms were randomized to CB group, CB bibliotherapy, or brochure control condition, completing assessments through 1-year follow-up. Contrary to previous findings, reductions in depressive symptom at post for CB group vs brochure and CB bibliotherapy (d = .06 and −.08, respectively) were nonsignificant. However, by 1-year follow-up, MDD onset rates were substantially (albeit nonsignificantly) lower for CB group (7%) and CB bibliotherapy (5%) compared to brochure control (15%). To our knowledge, only two other randomized trials using diagnostic data have examined depression prevention with college students (Seligman, Schulman, DeRubeis, & Hollon, 1999; Seligman, Schulman, & Tryon, 2007). Though both studies were adequately powered (N = 231 and 240, respectively), had excellent engagement (attendance 84-85%), and found significant post effects for depressive symptoms (M across interview and questionnaire d = .42), neither reduced MDD onset.
The absence of acute-phase reductions in depressive symptoms for our standard CB prevention program with college students was surprising, given consistently significant effects post-intervention in younger samples. The college participants had lower attendance and fewer positive expectancies for CB group than high school students, implying poorer engagement. It appeared that a prevention program that increased motivation for change and produced stronger effects was needed. Given our past success in a cognitive dissonance-based eating disorder prevention intervention (e.g., Stice, Marti, Shaw, & O’Neil, 2008), we sought to incorporate elements of cognitive dissonance change principles to improve depression prevention, creating a new CB depression prevention program, which we entitled Change Ahead.
Cognitive dissonance has been shown to be maximized by four factors (e.g., Green, Scott, Diyankova, & Gasser, 2005): (1) underscoring the voluntary nature of completing dissonance-inducing activities; (2) absence of an external justification for completing dissonance-inducing activities (e.g., subject payments, school credits); (3) high public accountability for dissonance-inducing behaviors; and (4) dissonance-inducing behaviors required a high level of effort. The first factor that maximizes cognitive dissonance (i.e., voluntary engagement) was also incorporated into a second eating disorder prevention program (Healthy Weight) that relied on participant-driven changes to promote small but sustainable improvements in diet and physical activity; this intervention has reduced both eating disorder symptoms and disorder onset in multiple trials (e.g., Stice, Shaw, Burton, & Wade, 2006). In Healthy Weight, all lifestyle change plans are explicitly selected by the individual, with the goal of promoting internalization of health goals. We incorporated these principles into Change Ahead so that cognitive and behavioral changes were explicitly selected by the participant rather than prescribed by the therapist (i.e., voluntary engagement) and added dissonance-induction activities (e.g., discussing the costs of depression). We also focused on increasing positive thoughts and physical activity and minimized group discussion in which participants repeatedly articulate negative cognitions and actions, which could undermine counter-depressive attitudes and behaviors.
We explored the impact of this new intervention in a preliminary trial with a sample of 59 college students with elevated depressive symptoms. Participants were randomized to either Change Ahead or an educational brochure which covered the signs of depression and the importance of seeking treatment as needed. We decided to use an educational brochure control condition for several reasons. First, this was a preliminary evaluation of the new dissonance-based CB depression prevention program, which focused on acceptability and sought to gather qualitative input on how we could refine this new intervention. Second, we did not have a basis to predict that it would produce significantly stronger reductions than an active intervention such as CB bibliotherapy, which has proven effective in reducing depressive symptoms and future depressive disorder onset. Third, using the educational brochure control condition allowed us to benchmark effects for this intervention relative to the effects for standard CB group depression prevention programs from past trials that have used this control condition. Fourth, one typically needs a great deal of statistical power to detect differences between two active interventions and this preliminary study was not adequately powered to detect such differences. The first aim of the study was to assess feasibility, as indexed by achieving recruitment goals, screening efficacy, attendance rates, and study retention. The second aim was to explore whether Change Ahead participants showed greater reductions in depressive symptoms than controls, as measured by both diagnostic interview and self-report questionnaire. The third aim explored whether Change Ahead participants showed lower incidence of MDD onset over follow-up. Given that we had a power of .80 to detect only medium magnitude effects (d = .50) or greater, we focus primarily on the magnitude of effect sizes when interpreting study results, while recognizing that parameter estimates from small studies need to be interpreted with caution (Kraemer, Mintz, Noda, Tinklenberg, & Yesavage, 2006).
Method
Participants and Procedures
Participants were 59 college students (68% female) between 18 and 28 years of age (M = 21.8; SD = 2.3). The sample was composed of 70% Caucasians, 9% Asian Americans, 3% Hispanic, 2% Native American, and 16% other/mixed. Participants were recruited in 2013-2014 from a large state university using a mass postcard mailing and posters. Postcards invited students to participate in a study evaluating interventions aimed at helping students reduce depressive symptoms. If interested, they were directed to an enrollment webpage, which included the Center for Epidemiologic Studies-Depression Scale (Radloff, 1977). College students who endorsed scores of 20 or greater (primary inclusion criteria, as in Stice et al., 2008) were invited to enroll and complete the baseline assessment. If the student had a current diagnosis of MDD or acute suicidal ideation (exclusion criteria; n = 1), they were offered referrals and not enrolled. Participants were not excluded on the basis of prior or concomitant treatment, and 39% had received mental health treatment in the prior year. Eligible participants were randomly assigned by the project coordinator using computer-generated random numbers to either Change Ahead group (n = 28) or educational brochure control (n = 31).
Participants completed assessments at pretest, posttest, and 3-month follow-up; receiving $25 for each assessment. Assessors were blind to condition, had a Bachelor’s in psychology, and had received 40 hours of training and achieved a minimum symptom agreement kappa of .80 with experts before data collection. The Oregon Research Institute (ORI) Institutional Review Board approved this study.
Change Ahead Group
The program contains elements of prior cognitive-behavioral prevention interventions (Stice et al., 2008; Rohde et al., 2014a) but was modified to incorporate cognitive dissonance principles. Each of the 6 weekly 1-hour sessions (a) begins with a voluntary commitment to actively participate and to try something new in the upcoming week (underscoring voluntary participation); (b) includes a section devoted to selecting and publicly committing to one change focused on reducing negative/increasing positive cognitions and one change focused on increasing pleasant activities; and (c) ends with home practice assignments. Four mixed-gender groups of 6-8 participants (M = 7.0) were conducted, each of which was co-facilitated either by a Ph.D. psychologist (one of the first two authors) and a graduate student or by two psychologists. Sessions were videotaped and reviewed by the third author for supervision and intervention refinement. If a participant missed a session, a brief individual make-up session was conducted. A description of sessions elements and their intended purpose is provided in Table 1.
Table 1.
Content of Change Ahead Sessions and Intended Component Purpose
| Session 1 |
|
| Session 2 |
|
| Session 3 |
|
| Session 4 |
|
| Session 5 |
|
| Session 6 |
|
Note: CB = cognitive-behavioral content, DI = Dissonance-induction techniques
Educational Brochure Control
Participants were given an NIMH educational brochure describing MDD symptoms and treatment (“Let’s Talk About Depression” NIH Pub. 01-4162), as well as referral information.
Measures
Interview-based depressive symptoms and diagnosis
An adapted Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Kaufman et al., 1997) interview assessed DSM-IV MDD symptoms. Participants reported the severity of each symptom (4-point response) over the past 12 months (at pretest) or since last interview. Symptom severity ratings were made on a month-by-month basis and summed to a symptom composite for past month depression severity and used to diagnose MDD. The interview has shown test-retest reliability (κ = .63 - 1.00), inter-rater diagnostic reliability (κ = .73 - 1.00), and sensitivity to intervention effects (Stice et al., 2008). The interview included questions regarding treatment for emotional/behavioral problems (type, provider, duration, frequency, medication usage) in the year prior to study entry (at pretest) or during the study (at post and 3-month follow-up).
Self-reported depressive symptoms
We included the 21-item (4-point response scale) Beck Depression Inventory (BDI, Beck, Steer, & Garbin, 1988). The BDI has acceptable internal consistency (α = .73 - .95), test-retest reliability (r = .60 -.90), and convergent validity with clinician ratings of depressive symptoms (M r = .75; Beck et al., 1988). Internal consistency in the present study was α = .84.
Intervention expectancies, acceptability, and cross-contamination
After reading a description of conditions at pretest, participants completed items assessing credibility, expected improvement, and satisfaction (5-point scales). For Change Ahead group participants, after each group session, facilitators recorded attendance (absent, partial, full) and homework completion (none, some, all). Participants were asked four questions at posttest to assess cross-condition contamination.
Statistical Methods
Percentages of missing data were 0-2% at pretest, 3-5% at posttest, and 7-12% at 3-months. Missing data were replaced with imputed data in 10 data sets, which were analyzed separately. Model parameters and standard errors, which incorporate within and between model parameter variability, were combined following Rubin (1987). Condition was unrelated to number of completed assessments.
Random effects growth models in a hierarchical linear model framework were fit with PROC MIXED (SAS Institute Inc., 2011). Individual variability in level-1 change in outcomes from posttest to 3-month follow-up was modeled as a function of the level-2 predictor condition, with pretest scores as a covariate. Two parameter estimates from the growth models were examined to determine program effectiveness: (1) condition (represents posttest change in outcome for Change Ahead versus brochure; test of acute phase effects) and (2) condition X time (represents outcome change from posttest to 3-month follow-up for Change Ahead relative to brochure; a test of maintenance or later emergence of effects). To accommodate the partially nested data structure, controls were treated as a group of one and condition specified as a random effect (Bauer, Sterba, & Hallfors, 2008). Random effects estimated at zero were fixed. Effect size was computed using time scores, parameter estimates from the growth models and raw standard deviation units (Feingold, 2009) and interpreted as Cohen’s (1988) d with small, medium, or large effect at values of 0.2, 0.5 and 0.8, respectively.
Logistic regression generated odds ratios and 95% confidence intervals were used to explore incidence of onset of MDD through 3-month follow-up. One participant in the control condition was identified as meeting minimal criteria for MDD at baseline and excluded from analysis. Effect size was estimated with odds ratios and interpreted as a small, medium, or large effect at values of 1.48, 2.48, and 4.28, respectively (Lipsey & Wilson, 2001).
Results
Indicators of Study Feasibility
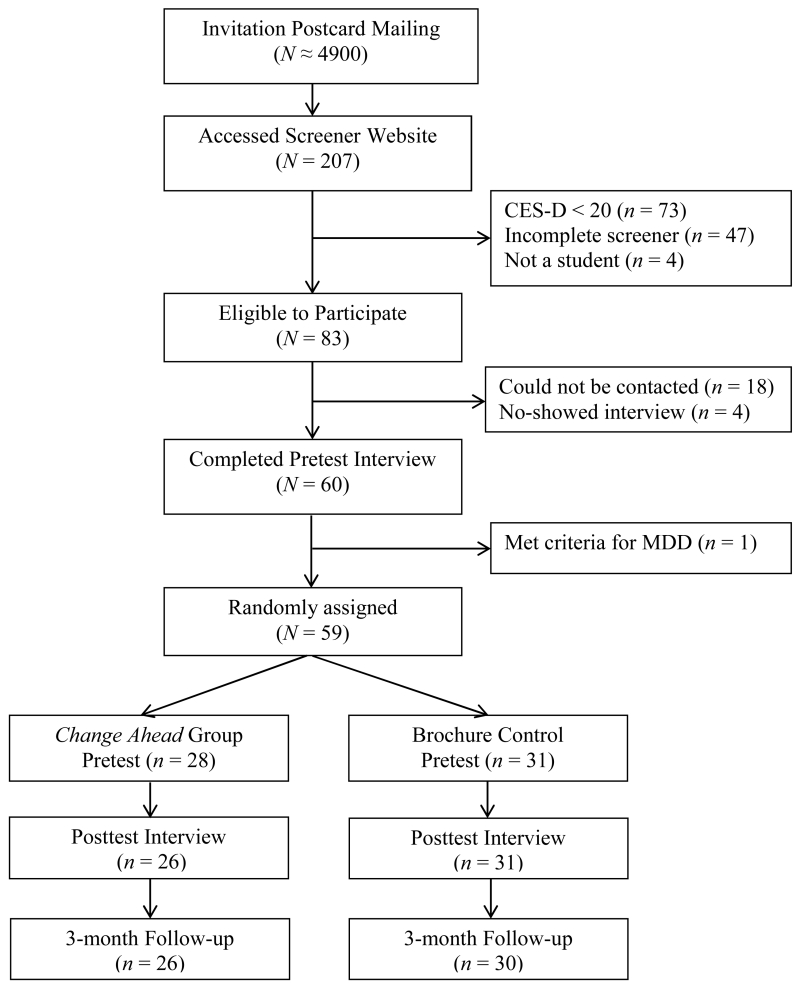
Participant flow through the study is illustrated in Figure 1. The screener was completed by approximately 4% of students sent the mailer. Among those who came to the web-based screener, 40% met the eligibility criteria. Screening efficacy (indicated by the percentage who entered the study among those meeting screener criteria) was high: 71% with elevated CES-D scores completed the pretest and were randomized. Randomization was effective and participants assigned to the two conditions did not differ on demographic variables (age, grade, race, and parental education), past year treatment service utilization, or baseline depressive symptoms (all p-values > .20).
Figure 1.
Participant Flow Chart
Participants rated the two conditions differently on perceived credibility (t[58] = 9.52, p < .001, d = 2.50) and expected benefit (t[58] = 10.59, p < .001, d = 2.78), but similarly on satisfaction with assignment to that condition (t(57] = 0.82, p = .42, d = 0.22); scores (1 = extremely disappointed, 5 = extremely pleased) suggested that participants found Change Ahead, versus brochure, more credible (M = 4.0, SD = 1.0 vs. M = 2.2, SD = 1.0) and beneficial (M = 3.9, SD = 0.9 vs. M = 2.0, SD = 0.9), but were neutral regarding condition assignment (M = 3.2, SD = 1.0 vs. M = 3.0, SD = 1.2). Models were re-run adjusting for perceived credibility and benefit and no outcome differences were noted. We also explored whether gender impacted symptom change, MDD onset, attendance, and homework completion; all gender effects were nonsignificant.
Change Ahead was engaging; mean attendance, including make-up sessions (15 make-ups were conducted, which represented 0.6 per group session conducted), was 5.5 of 6 sessions (SD =1.6); 86% (24/28) attended all 6 sessions (2 others attended 5 sessions and 2 did not attend any). Attendance was higher (t[53] = 3.19, p = .002, d = 0.88) than observed in the prior college depression prevention study (Rohde et al., 2014b), where the mean attendance was M = 3.9, SD = 2.1 and only 22% attended all 6 sessions. Homework completion for Change Ahead was moderately high – across the five sessions where homework was recorded (Sessions 2-6), on average 76% of Change Ahead participants completed all of the home practice assignments for that session, 10% completed some, and 14% either did none of the assignments for that week or failed to bring their written work to session (comparable data not available for the previous college pilot but 80% of homework assignments were recorded as completed in the high school effectiveness trial). There was no evidence of cross-condition contamination (e.g., 88% had not talked with anyone from the other condition; responses of those who had were vague).
Rates of non-study treatment utilization did not significantly differ by study condition in the year before the study (χ2[1,57] = 0.49, p = .48) or during the study (χ2[1,57] = 1.59, p = .21). Through the 3-month follow-up 23% of Change Ahead participants and 39% of controls reported receiving some form of non-study mental health counseling or treatment during their involvement in the project. Focusing specifically on more intensive treatment that might impact depression levels (which was defined as one month or more of receiving antidepressant medication and/or seeing a psychologist or psychiatrist), rates across conditions during the intervention (11% of Change Ahead participants and 10% of controls) or during the follow-up (15% vs. 23%, respectively) did not significantly differ (both p > .41) and controlling for non-study treatment utilization did not change the pattern of intervention effects.
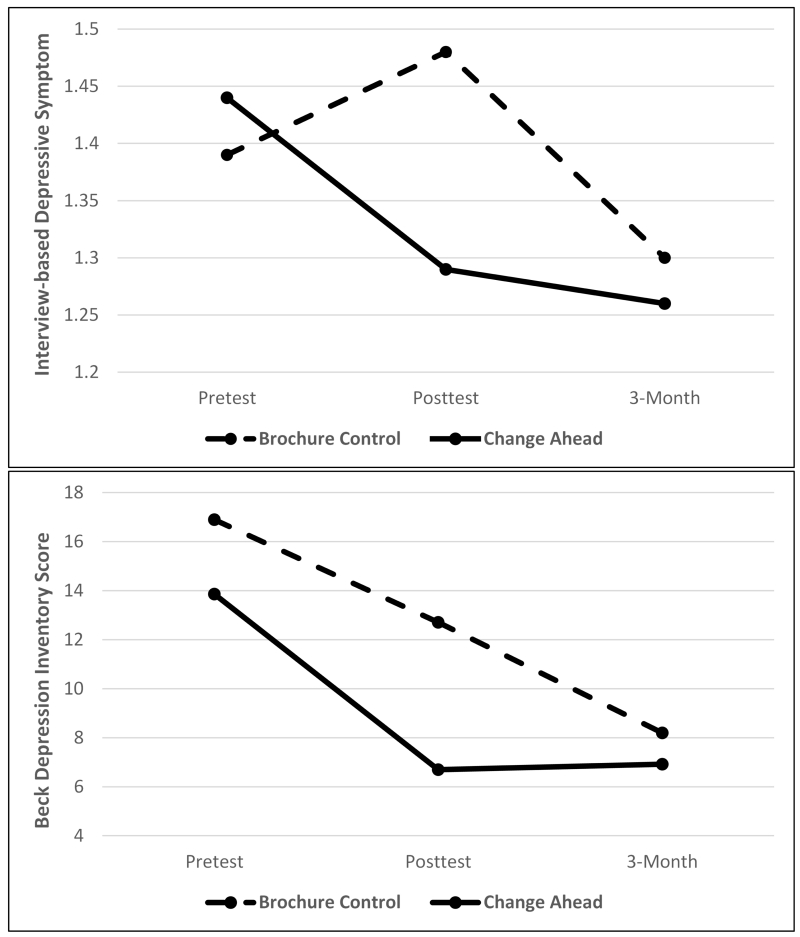
Intervention Effects for Change in Depressive Symptoms
Table 2 reports means and SD for outcomes across conditions and assessments (Figure 2 visually shows changes by condition). Planned contrasts are shown in Table 3. Condition estimates for depression measures were in the hypothesized direction and of medium-large magnitude; effects were statistically significant for posttest BDI scores but not interview-based symptoms.
Table 2.
Descriptive Statistics for Study Outcomes
| Pretest | Posttest | 3-Month Follow-up | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Depressive symptoms | ||||||
| Control | 1.39 | 0.37 | 1.48 | 0.35 | 1.30 | 0.40 |
| Change Ahead | 1.44 | 0.34 | 1.29 | 0.25 | 1.26 | 0.25 |
| Beck Depression Inventory | ||||||
| Control | 16.90 | 7.31 | 12.71 | 8.85 | 8.20 | 8.08 |
| Change Ahead | 13.86 | 8.14 | 6.70 | 5.27 | 6.92 | 5.68 |
Note: Means and standard deviations averaged across ten imputed data sets.
Figure 2.
Change in Depression Levels by Intervention Condition.
Table 3.
Model Fixed Effects Parameters for Change in Depressive Symptoms
| Variable | Parameter | Estimate | SE | t-value | p-value | d |
|---|---|---|---|---|---|---|
|
Depressive
symptoms |
Intercept | 1.48 | 0.06 | 24.61 | <.001 | 4.10 |
| Condition | −0.18 | 0.13 | −1.37 | .172 | −0.60 | |
| Time | −0.06 | 0.02 | −2.64 | .008 | −0.44 | |
| Condition X Time | 0.05 | 0.03 | 1.39 | .163 | 0.56 | |
|
Beck Depression
Inventory |
Intercept | 12.02 | 1.26 | 9.56 | <.001 | 1.48 |
| Condition | −4.73 | 2.32 | 2.04 | .041 | −0.69 | |
| Time | −1.45 | 0.40 | −3.60 | <.001 | −0.48 | |
| Condition X Time | 1.54 | 0.61 | 2.52 | .011 | 0.78 |
Note: SE = standard error, d = Cohen’s d-statistic. Fixed effects for baseline score not displayed.
The condition X time estimates were also medium-large in magnitude but in the opposite direction, suggesting that effects attenuated after intervention, as controls caught up with Change Ahead participants by follow-up.
Intervention Effects for Major Depression Onset
By 3-month follow-up, 5 (9%, 3 women and 2 men) of the 56 participants with complete data had shown onset of MDD: 4 controls (13%) and 1 Change Ahead participant (4%). Logistic regression models indicated that, controlling for pretest depressive symptoms, the lower rate of MDD in Change Ahead participants relative to controls was not statistically significant though medium-large in magnitude (b = −1.29, p =.26, OR = 3.64).
Discussion
This pilot study evaluated a new cognitive-behavioral indicated depression prevention program for college students that incorporated cognitive dissonance change principles in an effort to enhance the delivery of CB depression prevention efforts. The first study aim was to assess feasibility. Though the recruitment process required a large mass mailing, among potential participants who visited the screener, 71% enrolled in the trial. The finding that 4% of those receiving the postcard accessed the web screener is consistent with findings that research mass mailings generally result in enrollment rates of 2-8% (e.g., Alexander et al., 2008) but suggests that other recruitment methods (e.g., email invitations, snowball or chain-referral sampling) might be less costly.
The most positive indication of feasibility was intervention attendance. Change Ahead appeared more engaging to college students, compared to standard CB groups. Most Change Ahead participants (86%) attended all six sessions, which was higher than comparable previous rates (e.g., 26% of college participants, 44% in the high school efficacy trial, and 47% in the high school effectiveness trial). In addition, 76% of Change Ahead participants completed all of the home practice assignments each session, suggesting good engagement in the material, both in and out of session. These measures of engagement are encouraging because at baseline, students were neutral about their preference for receiving either the CB group or the brochure (even though they perceived the group as more credible and more beneficial), suggesting that they were not highly motivated to do something about their subthreshold depressive symptoms. It is possible that this increased engagement was a benefit of the added change principles. We attempted to enhance the voluntary nature of participation, create high public accountability to other group members and the leaders, and put the onus for change on participants rather than therapist prescription, in our efforts to create greater cognitive dissonance to take an anti-depressive stance. These factors may be more typical in individual CBT but we believe are less common in group CB interventions. Overall, our first aim suggested that web-based recruitment for indicated depression prevention and providing Change Ahead groups with at-risk college students are highly feasible.
Posttest reductions in depression symptoms by diagnostic interview and self-report measure were fairly comparable and both represented medium-large magnitude effects (d = .60, and .69, respectively), though values were statistically significant for only the self-report measure. These effect sizes are encouraging relative to the posttest effects for depressive symptoms in the high school efficacy trial (d = .46; Stice et al., 2008) and effectiveness trial (d = .29, Rohde et al., 2014a), and especially compared to the trivial effects noted in the college-based pilot examining the unmodified CB program (d = .06; Rohde et al., 2014b). However, by 3-month follow-up, reductions in depressive symptoms for Change Ahead were no longer present, which tempered enthusiasm. Though this pilot study was underpowered to detect statistically significant differences in MDD onset, the 4% MDD incidence rate for Change Ahead participants compared to 13% in controls was in a positive direction.
Several significant study limitations should be noted. First, the small sample resulted in limited power to detect small differences and more unstable effect values; confidence is strongest for the first aim examining program feasibility. Second, we had no measure of the presumed method of facilitating change: cognitive dissonance. Cognitive dissonance is an uncomfortable psychological state that emerges when people engage in a behavior that is inconsistent with an attitude. To measure dissonance induction would require the moment-by-moment assessment of physiological arousal, such as heart rate, during the group sessions for each participant, which currently is too disruptive (and expensive). Nonetheless, future research needs to examine more objectively the mechanisms that might be accounting for changes in depressive symptoms. Third, Change Ahead was compared solely to a non-active control condition that did not provide any contact beyond assessments and was not matched on nonspecific therapeutic factors. This was a reasonable but weak initial comparison condition and other active comparisons, such as CB bibliotherapy, would provide more stringent comparisons in future research. Fourth, consistent with the requirement that participants have elevated depressive symptoms, 10% of the sample reported receiving a fairly high dose of non-study mental health counseling during the intervention phase of this pilot when symptom change effects were strongest, but rates were comparable across conditions, and controlling for non-study treatment during either the intervention or follow-up did not change the pattern of findings. Fifth, assessment demands were purposely kept low but it would have been informative to have data on additional factors of interest as those variables might inform prevention efforts. For example, we did not assess the duration of current symptoms or past MDD history. We also did not collect information on current or past comorbid conditions, which may have impacted efficacy of the program.
Depression is a prevalent mental disorder in university students and there is a growing focus on active outreach efforts to prevent and treat both depression and suicidality on college campuses (e.g., Drum & Burton Denmark, 2012; Garlow et al., 2008). Given the feasibility of implementing Change Ahead groups and the lack of evidence-based MDD prevention programs for college students, continued evaluation of this new intervention appears justified. The present pilot data suggest that an engaging program that incorporates the factors found to enhance cognitive dissonance, and explicitly emphasizes participant choice in making positive changes to thinking and actions is potentially promising for at-risk college students. However, the intervention needs to be more rigorously compared to an active intervention, such as CB bibliotherapy, in an adequately powered trial to determine whether incorporating cognitive dissonance change principles into depression prevention enhances both engagement and depression outcomes.
Highlights.
-
-
Evaluated a new CB indicated depression prevention group for college students
-
-
Program incorporated cognitive dissonance change principles
-
-
Web-based recruitment was effective and intervention attendance rate was very high
-
-
Posttest symptoms reductions were encouraging relative to previous CB programs
-
-
Intervention participants showed a large (but ns) reduction in major depression onset
Acknowledgments
This study was partially supported by a research grant (MH080853) from the National Institute of Health.
Thanks go to the project research assistants and participants who made this study possible. We thank Julie Steyding, Maartje Mulders, and Julie Pope for their assistance in conducting Change Ahead groups.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alexander GL, Divine GW, Couper M,P, McCluer JB, Stopponi MA, Fortman KK, Tolsma DD, Strecher VJ, Cole Johnson C. Effect of incentives and mailing features on online health program enrollment. American Journal of Preventive Medicine. 2008;34:382–388. doi: 10.1016/j.amepre.2008.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College Health Association . American College Health Association—National College Health Assessment: Reference Group Data Report Spring 2008. American College Health Association; Baltimore, MD: 2008. [Google Scholar]
- American College Health Association . American College Health Association—National College Health Assessment II: Reference Group Data Report Spring 2012. American College Health Association; Hanover, MD: 2012. [Google Scholar]
- Bauer DJ, Sterba SK, Hallfors DD. Evaluating group-based interventions when control participants are ungrouped. Multivariate Behavioral Research. 2008;43:210–236. doi: 10.1080/00273170802034810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MC. Psychometric properties of the Beck Depression Inventory: Twenty-five years later. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BG, Liu S-M, Olfson M. Mental health of college students and their non-college-attending peers: Results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry. 2008;65:1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Cummings JR, Druss BG. Racial/ethnic differences in mental health service use among adolescents with major depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:160–170. doi: 10.1016/j.jaac.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drum DJ, Burton Denmark A. Campus suicide prevention: Bridging paradigms and forging partnerships. Harvard Review of Psychiatry. 2012;20:209–221. doi: 10.3109/10673229.2012.712841. [DOI] [PubMed] [Google Scholar]
- Feingold A. Effect Sizes for Growth-Modeling Analysis for Controlled Clinical Trials in the Same Metric as for Classical Analysis. Psychological Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garlow SJ, Rosenberg J, Moore JD, Haas AP, Koestner B, Hendin H, Nemeroff CB. Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depression and Anxiety. 2008;25:482–488. doi: 10.1002/da.20321. [DOI] [PubMed] [Google Scholar]
- Green M, Scott N, Diyankova I, Gasser C. Eating disorder prevention: An experimental comparison of high level dissonance, low level dissonance, and no-treatment control. Eating Disorders. 2005;13:157–169. doi: 10.1080/10640260590918955. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children - Present and Lifetime Version (KSADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Klein DN, Torpey DC, Bufferd SJ. Beauchaine TP, Hinshaw SP, editors. Depressive disorders. Child and Adolescent Psychopathology. 2008:477–509. [Google Scholar]
- Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry. 2006;63:484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical Meta-Analysis. Sage Publications; Thousand Oaks, CA: 2001. [Google Scholar]
- National Institute of Mental Health . Let’s talk about depression. Office of Communications and Public Liaison, NIMH; Bethesda, MD: 2001. NIH Publication 01-4162. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rohde P, Clarke GN, Made DE, Jorgensen JS, Seeley JR. An efficacy/effectiveness study of cognitive-behavioral treatment for adolescents with comorbid major depression and conduct disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:660–668. doi: 10.1097/01.chi.0000121067.29744.41. [DOI] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, Brière F. Indicated cognitive-behavioral depression prevention compared to bibliotherapy and brochure control: Acute effects of an effectiveness trial with adolescents. Journal of Consulting and Clinical Psychology. 2014a;82:65–74. doi: 10.1037/a0034640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, Gau JM. Cognitive-behavioral group depression prevention compared to bibliotherapy and brochure control: Nonsignificant effects in pilot effectiveness trial with college students. Behaviour Research and Therapy. 2014b;55:48–53. doi: 10.1016/j.brat.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, Gau JM. Effectiveness trial of an indicated cognitive- behavioral group adolescent depression prevention program versus bibliotherapy and brochure control at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology. 2015;83:736–747. doi: 10.1037/ccp0000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. J. Wiley & Sons; New York: 1987. [Google Scholar]
- SAS Institute Inc. SAS/STAT® 9.3 Procedures Guide. SAS Institute Inc; Cary, NC: 2011. [Google Scholar]
- Seligman MEP, Schulman P, DeRubeis J, Hollon SD. The prevention of depression and anxiety. Prevention & Treatment. 1999;2 np. [Google Scholar]
- Seligman ME, Schulman P, Tryon AM. Group prevention of depression and anxiety symptoms. Behaviour Research and Therapy. 2007;45:1111–1126. doi: 10.1016/j.brat.2006.09.010. [DOI] [PubMed] [Google Scholar]
- Stice E, Rohde P, Seeley JR, Gau JM. Brief cognitive-behavioral depression prevention program for high-risk adolescents outperforms two alternative interventions: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:595–606. doi: 10.1037/a0012645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Gau J. An effectiveness trial of a selected dissonance- based eating disorder prevention program for female high school students: Long-term effects. Journal of Consulting and Clinical Psychology. 2011;79:500–508. doi: 10.1037/a0024351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Education . The condition of education. US Department of Education; Washington, DC: 2008. [Google Scholar]