Abstract
OBJECTIVES:
To describe the prevalence of postdischarge outpatient rehabilitation among Medicaid-insured children hospitalized with a traumatic brain injury (TBI) and to identify factors associated with receipt of services.
METHODS:
Retrospective cohort of children <21 years, hospitalized for a TBI between 2007 and 2012, from a national Medicaid claims database. Outcome measures were receipt of outpatient rehabilitation (physical, occupational, or speech therapies or physician visits to a rehabilitation provider) 1 and 3 years after discharge. Multivariable regression analyses determined the association of demographic variables, injury severity, and receipt of inpatient services with receipt of outpatient rehabilitation at 1 and 3 years. The mean number of services was compared between racial/ethnic groups.
RESULTS:
Among 9361 children, only 29% received any type of outpatient rehabilitation therapy during the first year after injury, although 62% sustained a moderate to severe TBI. The proportion of children receiving outpatient therapies declined to 12% in the second and third years. The most important predictor of receipt of outpatient rehabilitation was receipt of inpatient therapies or consultation with a rehabilitation physician during acute care. Compared with children of other racial/ethnic groups, Hispanic children had lower rates of receipt of outpatient speech therapy.
CONCLUSIONS:
Hospitalized children who received inpatient assessment of rehabilitation needs were more likely to continue outpatient rehabilitation care. Hispanic children with TBI were less likely than non-Hispanics to receive speech therapy. Interventions to increase inpatient rehabilitation during acute care might increase outpatient rehabilitation and improve outcomes for all children.
What’s Known on This Subject:
Previous studies report lower access and less continuity of outpatient care among low-income children. No studies have examined receipt of outpatient rehabilitation services, or factors associated with receipt of such services, after traumatic brain injury for children insured by Medicaid.
What This Study Adds:
Few children on Medicaid received outpatient rehabilitation during the first year after discharge for traumatic brain injury. The best predictor of receipt of outpatient rehabilitation was receipt of inpatient therapies during hospitalization. Compared with other races/ethnicities, Hispanic children received outpatient speech therapy less often.
Traumatic brain injury (TBI) is the leading cause of long-term disability in children.1 Comprehensive postacute cognitive and physical rehabilitation improves functioning after TBI2–4 and is effective even among children with severe injuries.5 However, discharge decisions after a hospitalization for a TBI and referral to a rehabilitation unit or skilled nursing home are complex and influenced by multiple factors. Although the child’s overall physical condition and readiness to follow a comprehensive rehabilitation plan play a major role, unique family circumstances and preferences, and administrative factors related to insurance policies, affect and further complicate clinical decisions at the time of discharge. Yet there are no clear guidelines for the implementation of rehabilitation after TBI. Only 4% of US children hospitalized for TBI are discharged to an inpatient rehabilitation facility for postacute treatment.6 The initiation and provision of rehabilitation therapies during acute hospitalization also vary considerably.7 In a national data set of US pediatric hospitals, only 41% of children with severe TBI received inpatient physical therapy (PT) or occupational therapy (OT), and only 26% received speech therapy (ST).7 As a result, for most patients, TBI rehabilitation only begins in the outpatient setting, where continuity of care depends on insurance coverage and the caregiver’s ability to schedule and coordinate therapies. These factors can result in delay or nonreceipt of rehabilitation.
Children of low socioeconomic status are disproportionally affected by TBI.8–10 They are more likely to sustain severe and intentional injuries8,9 and to live in families with additional risk factors, such as inadequate social support,8,9 low insurance rates, and limited access to health care.11 All of these factors are associated with worse outcomes after TBI.12–16 Although the adoption of the Affordable Care Act (ACA) increased health care coverage for children and benefited low income children and their families,17 patients on Medicaid still face continuing gaps in care18,19 and difficulties in accessing primary care providers.20 Limited data are available on receipt of outpatient rehabilitation among low income children on Medicaid. The current study aims to: (1) describe the prevalence of postdischarge outpatient rehabilitation in a cohort of Medicaid insured children who were hospitalized with a TBI; (2) identify factors associated with receipt of outpatient rehabilitation services; and (3) evaluate if receipt of such services differed by race or ethnicity. We hypothesized that among this cohort of Medicaid-insured children with TBI, overall receipt of postdischarge outpatient rehabilitation would be low and that there would be differences in receipt of such services by age, severity of injury, and race and ethnicity.
Methods
This study is an analysis of a national data set of Medicaid claims, the Medicaid MarketScan database, which consists of individual-level inpatient and outpatient medical claims that can be tracked over time. It contains patient demographic information and dates of Medicaid enrollment; each claim provides information on the date, place, and type of medical service as well as the associated diagnosis. Our study used deidentified data provided by 14 different states between 2007 and 2012. Although the number of contributing states varied over the years, 4 states continuously provided data during this period, representing 60% of the total sample. Because all data were deidentified, including the names of the states, the study was considered exempt by the University of Washington institutional review board.
Study participants were patients 0 to 20 years old enrolled in Medicaid who were hospitalized for acute treatment of a TBI between 2007 and 2012 and who survived until discharge. Each participant was followed for a minimum of 12 months and a maximum of 36 months after discharge to determine receipt of outpatient rehabilitation services. Patients with intermittent Medicaid enrollment during the study period were included in analyses, but they contributed study data only during periods of enrollment. The cohort was not restricted to continuous enrollment because intermittent enrollment varies by state, given variability in reenrollment policies.18,19 Accordingly, we performed a sensitivity analysis to examine the potential effects of discontinuous versus continuous enrollment during the study period.
TBI was defined by using inpatient International Classification of Diseases, Ninth Revision (ICD-9) codes 800.0–801.99, 803.0–804.99, and 850.0–854.19. To identify the index TBI hospital admission, all hospital claims with a TBI diagnosis were identified. For patients with multiple hospitalizations, only the first claim was considered. Patients were excluded if, during the 30 days before the index admission, they had claims for PT, OT, or ST or claims for rehabilitation physician visits.
Definition of Outpatient Rehabilitation Services
The primary study outcome was receipt of outpatient rehabilitation services (yes/no), including PT, OT, ST, and follow-up by rehabilitation physicians. Receipt of these services was identified on the basis of provider or service claims, as coded in the data by provider type, service type, and revenue codes. Because a single rehabilitation service can be recorded more than once under provider and service claims, we initially identified all provider and service claims and subsequently used only 1 claim (provider or service) per type of therapy per day. In this way, we avoided counting the same therapy more than once, while maximizing our ability to identify services.
Definition of Covariates
Age in years (0–4, 5–9, 10–14, and 15–20) was used as a categorical variable. Race/ethnicity was used as provided by MarketScan: non-Hispanic white (NHW), non-Hispanic black (NHB), Hispanic, and Other. Severity of injury was measured by using Abbreviated Injury Scale (AIS) scores, calculated with the Stata-ICD9 Program for Injury Categorization (Stata Corp, College Station, TX).21 AIS scores describe 6 levels of injury severity: (1) minor, (2) moderate, (3) serious, (4) critical, (5) severe, and (6) unsurvivable. Table 1 presents the distribution of patients in each of these categories. For analyses, AIS scores of 1 and 2 were aggregated into a single category, as were scores 4 and 5. No patient had a score of 6 because the sample was restricted to children who survived until discharge. Medicaid plans were dichotomized as either fee-for-service or capitated (including health maintenance organizations that are fully capitated and preferred maintenance organizations that are partially capitated).
TABLE 1.
Demographic and Clinical Characteristics of Children Hospitalized With TBI
| Total | Any Outpatient Rehabilitationa | No Outpatient Rehabilitationa | Crude RR (95% CI)b | |
|---|---|---|---|---|
| Patient characteristics | N = 9361 | N = 2706 | N = 6648 | |
| Gender | ||||
| Boy | 65% | 63% | 66% | Ref |
| Girl | 35% | 37% | 34% | 0.9 (0.9–1.0) |
| Race/ethnicity | ||||
| NHW | 51% | 53% | 50% | Ref |
| NHB | 28% | 27% | 29% | 0.8 (0.8–1.0) |
| Hispanic | 7% | 7% | 7% | 1.0 (0.8–1.2) |
| Other | 14% | 13% | 14% | 1.1 (1.0–1.3) |
| Age categories, y | ||||
| 0–4 | 29% | 28% | 30% | Ref |
| 5–9 | 15% | 13% | 16% | 1.0 (0.9–1.1) |
| 10–14 | 15% | 15% | 16% | 1.2 (1.1–1.3) |
| 15–20 | 40% | 45% | 38% | 2.3 (2.1–2.5) |
| Max AIS head | ||||
| 1, minor | 2% | 2% | 2% | Ref |
| 2, moderate | 36% | 27% | 40% | 0.9 (0.7–1.2) |
| 3, serious | 26% | 26% | 26% | 1.2 (0.9–1.5) |
| 4, severe | 33% | 41% | 30% | 1.4 (1.0–1.8) |
| 5, critical | 2% | 4% | 1% | 2.8 (1.8–4.3) |
| Max AIS without head | ||||
| 1, minor | 33% | 24% | 38% | Ref |
| 2, moderate | 21% | 19% | 22% | 1.3 (1.2–1.5) |
| 3, serious | 21% | 34% | 16% | 2.4 (2.1–2.8) |
| 4, severe | 2% | 4% | 2% | 2.5 (1.9–3.2) |
| 5, critical | 2% | 3% | 1% | 2.0 (1.6–2.6) |
| Isolated TBI | 20% | 17% | 21% | 0.7 (0.6–0.8) |
| LOS days median (IQR25–75) | 3 (2–6) | 7 (3–18) | 2 (1–4) | 1.0 (1.0-1.0) |
| Plan typec | ||||
| Fee for service | 49% | 59% | 45% | Ref |
| Capitated | 51% | 41% | 55% | 0.7 (0.6–0.8) |
| Receipt of any inpatient rehabilitation | 45% | 74% | 32% | 4.1 (3.7–4.5) |
| Discharge status | ||||
| Home | 84% | 64% | 93% | Ref |
| Home under care | 4% | 9% | 2% | 3.0 (2.5–3.5) |
| Short-term facility | 5% | 12% | 2% | 2.9 (2.6–3.4) |
| Inpatient rehabilitation | 4% | 11% | 1% | 3.5 (3.1–4.0) |
| Long-term facility | 1% | 3% | 1% | 2.8 (2.1–3.6) |
| Other | 2% | 1% | 1% | 1.8 (1.1–3.0) |
LOS, length of stay; Ref, reference category.
Any outpatient rehabilitation over the 3-year follow-up period.
RR calculated using modified Poisson regression clustering by institution and accounting by exposure (enrollment months).
Capitated plans can be partially or fully capitated.
Receipt of outpatient rehabilitation depends on referral at the time of discharge, which can be influenced by receipt of inpatient rehabilitation. Therefore, we also examined receipt of inpatient PT, OT, ST, and consultation by rehabilitation physicians. Receipt of inpatient rehabilitation was defined on the basis of provider or service claims by following the same approach that we used for receipt of outpatient rehabilitation services. We included only services provided during the initial acute hospitalization; services received at an inpatient rehabilitation facility after discharge from the acute care facility were not counted.
Data Analyses
Our main outcome variable was receipt of outpatient therapies (yes/no). We conducted modified Poisson regressions to account for differential exposure times (ie, different Medicaid enrollment times),22 clustering by institution to account for institutional differences. Univariate modified Poisson regression was used to compare baseline demographic and clinical characteristics of children who received any outpatient rehabilitation services during the 36 months follow-up to those of children who received none. We also conducted univariate analyses of services received during 3 successive follow-up periods: discharge to 12 months, 13 to 24 months, and 25 to 36 months. We conducted bivariate analyses to determine the association between receipt of outpatient rehabilitation services during each follow-up period and the following independent variables: age, gender, race, severity of head injury, overall injury severity excluding head injury, type of Medicaid plan, length of hospital stay, and year of service. In the multivariable analyses, we examined the relative contribution of all independent variables and explored their association with receipt of rehabilitation services during 12 months and 13 to 36 months after discharge. We conducted regression analyses only for those 2 follow-up periods because the proportion of patients who received services after 12 months was small, and there was little variation in receipt of services between 13 to 24 and 25 to 36 months.
To evaluate the effect of receipt of inpatient rehabilitation on receipt of outpatient rehabilitation services, we conducted the multivariable analyses described above, both among the entire cohort (adjusting for receipt of inpatient rehabilitation services) and separately among patients who received any inpatient services and patients who received none. We also conducted a sensitivity analysis using Poisson regression without the exposure variable among the subgroup of patients who were continuously enrolled.
The median number of services for each type of rehabilitation therapy (PT, OT, and ST) and follow-up by a rehabilitation physician is reported for patients who received outpatient rehabilitation during the 3 follow-up periods.
Secondary analyses were performed to assess differences in the mean number of services received by race and ethnicity, with mean differences compared using negative binomial models adjusting for all independent variables listed above and clustering by institution. Baseline demographic and clinical characteristics were also compared between racial and ethnic groups by using F and χ2 tests. Total number of visits by predictors of rehabilitation is presented as supplemental material (Supplemental Table 5).
Results
The study sample included 9361 children hospitalized for acute management of a TBI between 2007 and 2012. Most were boys (65%), NHW (51%), and >15 years. Although all were insured by Medicaid, the type of Medicaid plan differed; half were insured under fee-for-service plans and the other half under capitated plans (Table 1).
Most patients had other associated injuries; only 19% had an isolated TBI. Overall, 62% of children had maximum head AIS scores >2. The overall median length of hospitalization was 3 days (interquartile range [IQR]25–75, 2–6 days). As inpatients, 45% of patients received at least 1 type of rehabilitation service. Most patients (84%) were discharged from the hospital after acute inpatient care (Table 1).
After discharge, only 29% of children with TBI received any type of outpatient rehabilitation therapy or were seen by a rehabilitation physician over the 36-month follow-up period. In bivariate analyses, children who received outpatient rehabilitation were more likely to be older, sustain more severe injuries, have longer hospitalizations, be insured by fee-for-service plans, receive inpatient rehabilitation, and be discharged to a rehabilitation facility (Table 1).
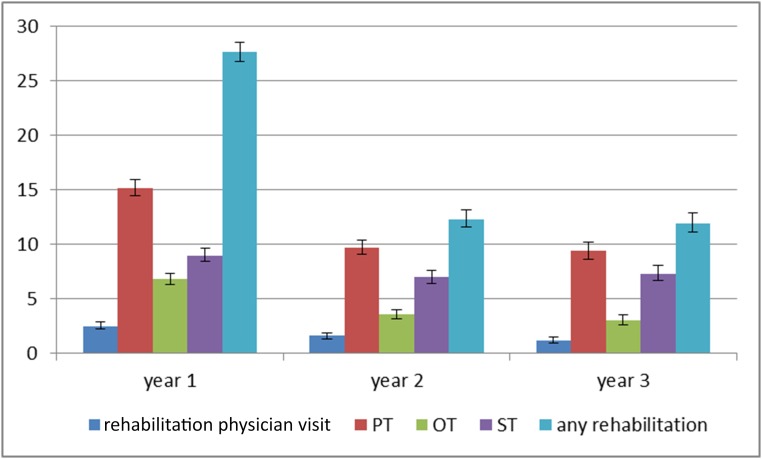
The proportion of children receiving outpatient rehabilitation therapies decreased over time, with 27% receiving services of any type during the first year, decreasing to 12% in the second and third years (Fig 1).
FIGURE 1.
Proportion of patients who received outpatient rehabilitation after TBI. Error bars represent 95% CIs.
PT was the most common outpatient rehabilitation therapy, with 32% of patients completing at least 1 follow-up PT visit. Smaller percentages received ST (17%) and OT (15%). Patients were most likely to receive therapies during the first 12 months after injury, with numbers falling at 24 and 36 months (Fig 1). Some patients did not receive therapy during the first 12 months, but did so subsequently, so that a larger proportion of children received therapy over the full 36 month follow-up period than during the initial 12 months.
In multivariable analyses, factors positively associated with receipt of outpatient rehabilitation included severity of head injury and other injuries, receipt of inpatient rehabilitation, and insurance under a fee-for-service plan (Table 2). Among these associations, the strongest was receipt of inpatient rehabilitation, with adjusted relative risks (RRs) between 2.8 and 35.1, depending on the type of rehabilitation therapy. When analyses were stratified by receipt of inpatient rehabilitation (instead of adjusting for it), the direction and magnitude of the associations remained similar. Therefore, we present only the overall analysis without stratification.
TABLE 2.
Adjusted RR for Predictors of Receipt of Outpatient Rehabilitation Services 1 and 3 Years After Hospitalization for TBI, Clustering by Institution
| Type of Outpatient Rehabilitation Services Received After Hospitalization | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Rehabilitation Physician | PT | OT | ST | Any Therapy | ||||||
| During Year 1 | During Year 2 to 3 | During Year 1 | During Year 2 to 3 | During Year 1 | During Year 2 to 3 | During Year 1 | During Year 2 to 3 | During Year 1 | During Year 2 to 3 | |
| RR (CI) | RR (CI) | RR (CI) | RR (CI) | RR (CI) | RR (CI) | RR (CI) | RR (CI) | RR (CI) | RR (CI) | |
| Receiving services as an inpatient | 35.1 (19.4–63.4) | 23.0 (10.9–48.4) | 3.6 (3.2–4.1) | 2.8 (2.5–3.2) | 6.7 (5.3–8.6) | 5.5 (4.7–6.7) | 5.4 (4.5–6.4) | 4.1 (3.5–4.8) | 4.0 (3.6–4.4) | 1.2 (1.1–1.3) |
| Age, y | ||||||||||
| 0–4 | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 5–9 | 1.0 (0.7–1.2) | 0.9 (0.6–1.5) | 0.5 (0.4–0.6) | 0.7 (0.6–0.8) | 0.6 (0.5–0.9) | 0.8 (0.7–1.0) | 0.7 (0.6–0.9) | 0.7 (0.6–0.8) | 0.8 (0.7–0.9) | 1.0 (0.9–1.1) |
| 10–14 | 1.0 (0.7–1.5) | 1.0 (0.7–1.4) | 0.6 (0.5–0.7) | 0.8 (0.7–0.9) | 0.7 (0.5–1.0) | 0.8 (0.6–1.1) | 0.9 (0.5–0.8) | 0.7 (0.6–0.8) | 0.8 (0.7–0.9) | 1.0 (0.9–1.1) |
| 15–20 | 1.0 (0.7–1.5) | 1.9 (1.4–2.6) | 0.6 (0.5–0.7) | 1.3 (1.1–1.4) | 0.6 (0.5–0.8) | 1.2 (1.0–1.3) | 0.5 (0.4–0.6) | 0.8 (0.5–0.9) | 0.9 (0.8–1.0) | 0.9 (0.8–1.6) |
| Gender | ||||||||||
| Boy | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Girl | 0.9 (0.7–1.3) | 0.9 (0.7–1.2) | 1.1 (1.0–1.2) | 1.0 (0.9–1.1) | 0.9 (0.7–1.1) | 0.9 (0.8–1.1) | 1.0 (0.8–1.1) | 1.0 (0.9–1.0) | 1.1 (1.0–1.2) | 0.9 (0.8–1.0) |
| Head max AIS score | ||||||||||
| 1–2, minor/moderate | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 3, serious | 1.2 (0.8–1.9) | 1.0 (0.6–1.4) | 1.1 (1.0–1.2) | 1.0 (0.9–1.2) | 1.5 (1.1–2.0) | 1.3 (1.1–1.5) | 1.4 (1.1–1.8) | 1.3 (1.1–1.5) | 1.2 (1.1–1.3) | 0.9 (0.8–1.3) |
| 4–5, critical/severe | 1.7 (1.2–2.3) | 1.1 (0.7–1.6) | 1.6 (1.4–1.7) | 1.3 (1.1–1.4) | 2.1 (1.6–2.6) | 1.8 (1.5–2.1) | 2.3 (1.8–2.8) | 1.8 (1.6–2.2) | 1.5 (1.4–1.6) | 1.6 (1.3–1.9) |
| Max AIS score | ||||||||||
| 1–2, minor/moderate | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 3, serious | 1.2 (0.9–1.5) | 1.1 (0.8–1.6) | 1.6 (1.4–1.8) | 1.5 (1.4–1.7) | 1.5 (1.3–1.8) | 1.3 (1.1–1.4) | 1.3 (1.1–1.5) | 1.2 (1.0–1.2) | 1.5 (1.4–1.6) | 1.2 (1.0–1.5) |
| 4, critical/severe | 1.0 (0.6–1.7) | 0.7 (0.4–1.3) | 1.8 (1.5–2.2) | 1.4 (1.2–1.7) | 1.5 (1.0–2.2) | 1.1 (0.9–1.4) | 1.1 (0.8–1.5) | 1.0 (0.9–1.4) | 1.5 (1.3–1.7) | 1.2 (0.9–1.7) |
| Plan type | ||||||||||
| Comprehensive | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Capitated | 0.6 (0.4–1.0) | 0.7 (0.4–1.3) | 0.8 (0.7–0.9) | 0.9 (0.8–1.0) | 0.9 (0.7–1.1) | 0.9 (0.8–1.1) | 0.9 (0.7–1.1) | 0.9 (0.9–1.2) | 0.9 (0.8–1.0) | 1.0 (0.9–1.1) |
| Race/ethnicity | ||||||||||
| NHW | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| NHB | 0.9 (0.7–1.2) | 1.1 (0.8–1.4) | 1.0 (0.8–1.1) | 0.8 (0.7–0.9) | 1.0 (0.8–1.2) | 0.8 (0.7–0.9) | 1.1 (0.9–1.3) | 1.0 (0.8–1.2) | 1.0 (0.9–1.0) | 0.9 (0.8–1.0) |
| Hispanic | 1.3 (1.0–1.7) | 1.4 (1.1–2.1) | 1.0 (0.8–1.2) | 0.8 (0.6–0.9) | 0.9 (0.6–1.3) | 0.6 (0.5–0.9) | 0.9 (0.7–1.2) | 0.8 (0.7–1.0) | 1.0 (0.9–1.1) | 0.9 (0.7–1.1) |
| Other | 1.2 (0.9–1.6) | 1.1 (0.7–1.6) | 1.2 (1.0–1.5) | 1.0 (0.8–1.2) | 1.4 (1.0–1.0) | 1.1 (0.8–1.3) | 1.3 (1.0–2.0) | 1.0 (0.8–1.2) | 1.1 (0.9–1.2) | 1.0 (0.7–1.1) |
| LOS | 1.0 (1.0–1.0) | 1.0 (0.9–1.0) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) |
LOS, length of stay; max, maximum; Ref, reference category.
The results of the sensitivity analysis of demographic and clinical characteristics among the subgroup of patients who were continuously enrolled during the study period were similar to those for the overall group, except for age (Supplemental Table 3). Patients who were continuously enrolled were more likely to be <4 years (44% vs 29% in the noncontinuously enrolled group). The results of the subgroup analysis were nearly identical to those using the entire cohort (Supplemental Table 4).
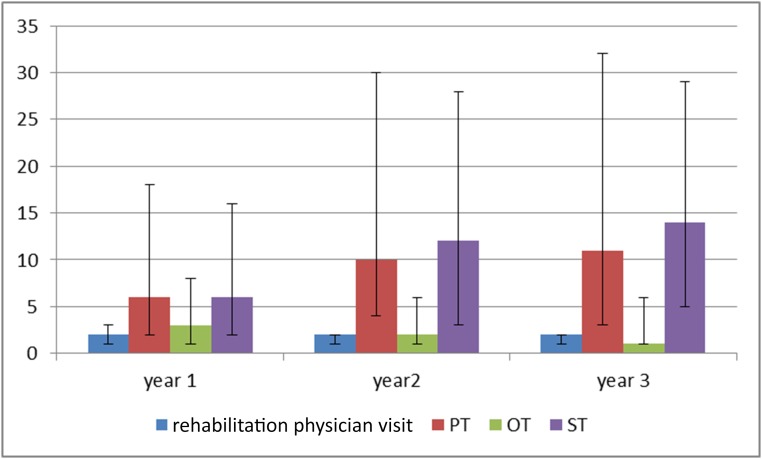
Among patients who received at least 1 outpatient rehabilitation service during the 36 month follow-up period, the median number of services during the first year was 2 visits with a rehabilitation physician, 6 PT visits, 3 OT visits, and 6 ST visits (Fig 2). Among children who received PT and ST for at least 2 years, more visits occurred during the second year after injury than the first year.
FIGURE 2.
Median number and IQR25–75 of outpatient rehabilitation visits after TBI.
The secondary analysis of the association between receipt of services and race or ethnicity found that Hispanic patients were significantly younger than non-Hispanic patients. The mean age and 95% confidence interval (CI) for Hispanics was 8.8 years (8.3–9.3), versus 10.2 (9.9–10.4) for NHBs, 10.9 (10.7–11.1) for NHWs, and 9.9 (9.5–10.3) for Others. A higher proportion of Hispanic children (44%) sustained severe head injuries than children who were NHB (33%), NHW (37%), or Other (33%). We found no differences in outpatient rehabilitation utilization between NHW, NHB, and Hispanic children. However, children in the Other category were more likely to receive PT, OT, and ST services than NHW children (Table 2). Among patients who received services, we found no racial or ethnic differences in the number of services received except for ST. At all follow-up times, Hispanics received significantly fewer ST visits than did patients in the remaining categories. During the first 12 months after injury, the mean number of speech therapies was 12.6 for NHWs, 13.4 for NHBs, 9.5 for Hispanics, and 9.5 for Others; the 2 subsequent follow-up periods showed similar results (Supplemental Fig 3).
Discussion
In this cohort of Medicaid-insured children hospitalized for a TBI, only 29% received any type of outpatient rehabilitation therapy during the first year after injury, even though 62% sustained a moderate to severe TBI. This finding adds to the current literature by demonstrating that children with TBI receive outpatient rehabilitation care at low rates. It is consistent with previously documented low referral rates to comprehensive inpatient rehabilitation,6 as well as low rates of inpatient evaluation for rehabilitation therapy during acute hospitalization for children withTBI.7
A second finding is that, after adjustment for known risk factors, such as age and injury severity, the most important predictor of receipt of outpatient rehabilitation was receipt of inpatient rehabilitation or consultation with a rehabilitation physician during acute inpatient care. This finding highlights the importance of initiating multidisciplinary rehabilitation assessment and management during acute care. For most children hospitalized for a TBI, rehabilitation can be addressed in the outpatient setting. Nevertheless, our results underscore the critical importance of receiving rehabilitation therapy or consultation as an inpatient to maximize the likelihood of receiving outpatient rehabilitation.
Although children who sustain TBI might be eligible to receive school-based rehabilitation services, these are designed to complement outpatient rehabilitation and should ideally be medically supervised. Previous studies demonstrate that even when such services are provided, parents still have difficulties navigating the complicated system of rehabilitation therapies available through clinical and school settings.23,24
A third important finding is the lower rate of receipt of outpatient rehabilitation among patients covered under Medicaid capitated plans. Although the ACA expanded services for children, it is still unclear how other aspects, such as bundled care and capitation, may affect the delivery of rehabilitation. Capitated plans may limit the ability to receive services by narrowing the choice of provider networks. Our data cover the first 2 years after the implementation of the ACA, which are not sufficient to analyze time trends. Future studies are warranted to understand the impact of capitation in the delivery of rehabilitation, especially for outpatient settings.
A last finding is the lower rate of outpatient ST among Hispanic children compared with non-Hispanics. We hypothesize that language might play a role in this disparity, as many Hispanics in the United States have limited English proficiency (LEP), whereas rehabilitation providers might not have procedures in place to ensure that families receive health care in their preferred language. This result is consistent with a previous finding that LEP parents were likely to have difficulties obtaining therapies in their primary language because of the scarcity of services provided for LEP children.25
We note several study limitations. Our data are limited to administrative claims and therefore restricted to the information provided by the database. We used ICD-9 codes for determining severity of injury; although the use of ICD-9 codes converted to AIS scores is validated, this method is limited in assessing the compounding effect of multiple injuries in a patient. Now that International Classification of Diseases, 10th Revision codes have been implemented, severity of injury should be better categorized because the codes are more specific and provide information on different stages of treatment.
Another limitation is that our ability to determine services received by patients is restricted to billed services. Unbilled services and services provided through the school system or community organizations were not available to us and therefore not included in the analyses. We also cannot assess if services were recommended but the family elected not to proceed with them. Nonetheless, our findings are similar to those previously described in clinical samples.6,7 We did not have information on the geographical locations of the patients included in this study, which hampered our ability to determine any regional variations. In addition, this is not a nationally representative sample because 14 states contributed, and these varied over the years, limiting the generalizability of the results. We had no data on language proficiency of patients or their families, limiting our ability to interpret our findings on receipt of ST by Hispanic children. Thus, our hypothesis that language barriers might make it less likely for Hispanic patients to receive ST should be taken with caution. Additionally, we had no data on provision of cognitive and behavioral therapies. The codes provided by our database did not provide that level of detail. Lastly, this is a retrospective, observational study and thus cannot establish cause and effect, merely statistical associations. Even though we controlled for known confounders, residual confounding might still be present.
Based on our findings, we encourage clinicians to initiate rehabilitation during acute inpatient treatment of TBI in children. Children hospitalized with moderate to severe TBI will benefit from an initial inpatient assessment of rehabilitation needs to identify areas where outpatient care will improve function. Ideally, an acute, multidisciplinary team approach, with a rehabilitation physician as part of the team, will prioritize this assessment and facilitate children’s transition to outpatient rehabilitation. Inpatient assessment can also help to identify and address financial, logistic, and language barriers to outpatient care. Although this is true for all children with TBI, it is even more important for low-income children, whose parents might fail to recognize their children’s need for care and thereby elevate the risk of poor outcomes.
Glossary
- ACA
Affordable Care Act
- AIS
Abbreviated Injury Scale
- CI
confidence interval
- ICD-9
International Classification of Diseases, Ninth Revision
- IQR
interquartile range
- LEP
limited English proficiency
- LOS
length of stay
- NHB
non-Hispanic black
- NHW
non-Hispanic white
- OT
occupational therapy
- PT
physical therapy
- RR
relative risk
- ST
speech therapy
- TBI
traumatic brain injury
Footnotes
Dr Jimenez conceptualized and designed the study and drafted the initial manuscript; Ms Symons assembled the database, carried out the analyses, and reviewed and revised the manuscript; Dr Wang carried out the analyses and reviewed and revised the manuscript; Drs Ebel, Vavilala, Buchwald, Temkin, and Jaffe critically reviewed the manuscript; Dr Rivara conceptualized and designed the study and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This work was supported by the National Institute of Child Health and Human Development (grant 1K23HD078453-01 to Dr Jimenez) and National Center for Injury Prevention and Control, Centers for Disease Control and Prevention grant R49 CE 001021. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Centers for Disease Control and Prevention Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. Atlanta, GA: National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention; 2014 [Google Scholar]
- 2.Cicerone KD, Dahlberg C, Kalmar K, et al. Evidence-based cognitive rehabilitation: recommendations for clinical practice. Arch Phys Med Rehabil. 2000;81(12):1596–1615 [DOI] [PubMed] [Google Scholar]
- 3.Cicerone KD, Dahlberg C, Malec JF, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 1998 through 2002. Arch Phys Med Rehabil. 2005;86(8):1681–1692 [DOI] [PubMed] [Google Scholar]
- 4.Cicerone KD, Langenbahn DM, Braden C, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 2003 through 2008. Arch Phys Med Rehabil. 2011;92(4):519–530 [DOI] [PubMed] [Google Scholar]
- 5.Kramer ME, Suskauer SJ, Christensen JR, et al. Examining acute rehabilitation outcomes for children with total functional dependence after traumatic brain injury: a pilot study. J Head Trauma Rehabil. 2013;28(5):361–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Variation in pediatric traumatic brain injury outcomes in the United States. Arch Phys Med Rehabil. 2014;95(6):1148–1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bennett TD, Niedzwecki CM, Korgenski EK, Bratton SL. Initiation of physical, occupational, and speech therapy in children with traumatic brain injury. Arch Phys Med Rehabil. 2013;94(7):1268–1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hakmeh W, Barker J, Szpunar SM, Fox JM, Irvin CB. Effect of race and insurance on outcome of pediatric trauma. Acad Emerg Med. 2010;17(8):809–812 [DOI] [PubMed] [Google Scholar]
- 9.Brown RL. Epidemiology of injury and the impact of health disparities. Curr Opin Pediatr. 2010;22(3):321–325 [DOI] [PubMed] [Google Scholar]
- 10.Haider AH, Weygandt PL, Bentley JM, et al. Disparities in trauma care and outcomes in the United States: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2013;74(5):1195–1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adams PF, Kirzinger WK, Martinez ME. Summary health statistics for the U.S. population: National Health Interview Survey, 2012. Hyattsville, MD: U.S. Department of Health and Human Services; 2013. Vital and Health Statistics, Series 10, Number 259 [PubMed]
- 12.Jimenez N, Ebel BE, Wang J, et al. Disparities in disability after traumatic brain injury among Hispanic children and adolescents. Pediatrics. 2013;131(6). Available at: www.pediatrics.org/cgi/content/full/131/6/e1850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rivara JB, Jaffe KM, Fay GC, et al. Family functioning and injury severity as predictors of child functioning one year following traumatic brain injury. Arch Phys Med Rehabil. 1993;74(10):1047–1055 [DOI] [PubMed] [Google Scholar]
- 14.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology. 2002;16(1):15–27 [DOI] [PubMed] [Google Scholar]
- 15.Yeates KO, Taylor HG, Walz NC, Stancin T, Wade SL. The family environment as a moderator of psychosocial outcomes following traumatic brain injury in young children. Neuropsychology. 2010;24(3):345–356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCarthy ML, MacKenzie EJ, Durbin DR, et al. ; Children’s Health After Trauma Study Group . Health-related quality of life during the first year after traumatic brain injury. Arch Pediatr Adolesc Med. 2006;160(3):252–260 [DOI] [PubMed] [Google Scholar]
- 17.Medicaid and Children’s Health Insurance Program (CHIP) information page. Available at: www.medicaid.gov/medicaid-chip-program-information/by-population/children/children.html. Accessed May 1, 2015
- 18.Sommers BD. From Medicaid to uninsured: drop-out among children in public insurance programs. Health Serv Res. 2005;40(1):59–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fairbrother G, Madhavan G, Goudie A, et al. Reporting on continuity of coverage for children in Medicaid and CHIP: what states can learn from monitoring continuity and duration of coverage. Acad Pediatr. 2011;11(4):318–325 [DOI] [PubMed] [Google Scholar]
- 20.Decker SL. Acceptance of new Medicaid patients by primary care physicians and experiences with physician availability among children on Medicaid or the Children’s Health Insurance Program. Health Serv Res. 2015;50(5):1508–1527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark DE, Turner M. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. Statistical Software Components. December 2009. Available at: https://ideas.repec.org/c/boc/bocode/s457028.html [Google Scholar]
- 22.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706 [DOI] [PubMed] [Google Scholar]
- 23.Roscigno CI, Fleig DK, Knafl KA. Parent management of the school reintegration needs of children and youth following moderate or severe traumatic brain injury. Disabil Rehabil. 2015;37(6):523–533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ennis SK, Rivara FP, Mangione-Smith R, Konodi MA, Mackenzie EJ, Jaffe KM. Variations in the quality of inpatient rehabilitation care to facilitate school re-entry and cognitive and communication function for children with TBI. Brain Inj. 2013;27(2):179–188 [DOI] [PubMed] [Google Scholar]
- 25.Moore M, Jimenez N, Rowhani-Rahbar A, et al. Availability of outpatient rehabilitation services for children after traumatic brain injury: differences by language and insurance status. Am J Phys Med Rehabil. 2016;95(3):204–213 [DOI] [PMC free article] [PubMed] [Google Scholar]