Abstract
We report the case of a 73-year-old who presented with multiple, small, in-transit melanoma nodules located in her right lower extremity below her knee. Positron emission tomography detected two additional non-palpable subcutaneous lesions posterior and medial to the area of previous wide local excision. A novel approach of radioactive seed localization was employed to guide the surgeon to successful surgical resection of all metastatic disease. To our knowledge, the application of radioactive seed localization to melanoma has not been previously reported.
Abbreviations: FDG, Fluorodeoxyglucose; PET, positron emission tomography; MRI, magnetic resonance imaging; RSL, radioactive seed localization; CT, computed tomography
Case Report
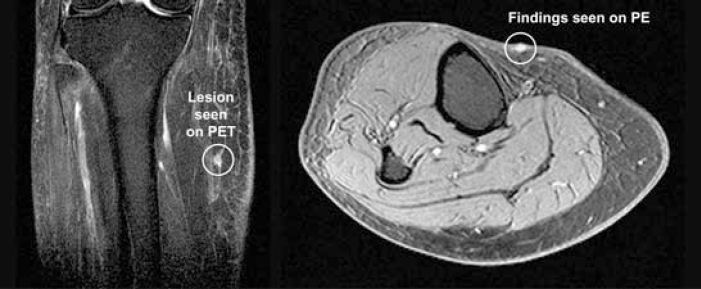
A 73-year-old woman had undergone a wide local excision with a 1.5 cm margin for a 3.9 mm thick, non-ulcerated malignant melanoma located on the right lower extremity over the mid tibia. There was a nodular aggregate of melanoma cells in the superficial subcutaneous adipose tissue, questionable for a satellite lesion. Subsequently, she underwent a sentinel lymph node biopsy with two of four nodes being positive for metastatic disease. A completion right inguinal lymphadenectomy found all 13 additional nodes free of disease. Metastatic work-up revealed no distant disease. She underwent adjuvant interferon-α2b therapy. After four months of adjuvant therapy, she developed multiple small nodules around her original wide local excision surgical site. Biopsy revealed recurrent melanoma of the right lower extremity inferior to the knee surrounding the site of the previous wide local excision (Figure 1).
Figure 1.
Right lower extremity with visible lesions inferior to the knee. [Powerpoint Slide]
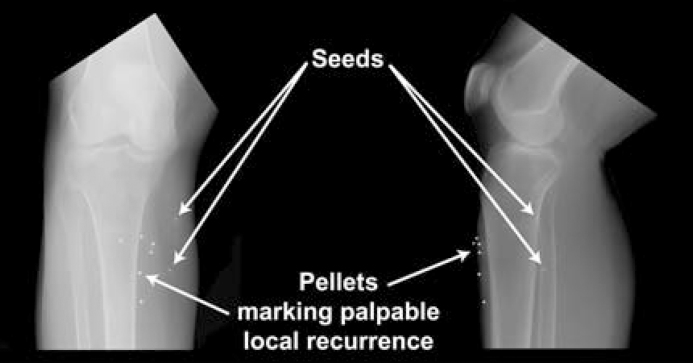
She was then referred to our institution for evaluation and treatment. Metastatic work-up was performed. Positron Emission Tomography (PET) using 16.1 mCi of fluorine-18 Fluorodeoxyglucose (FDG) revealed three focal areas of increased uptake in the skin of the pre-tibial region consistent with the skin lesions found on the physical exam. In addition, two focal areas of increased uptake were noted in the subcutaneous tissues posterior and medial to the previous areas of wide local excision. A Magnetic Resonance Image (MRI) of the right lower extremity demonstrated two deep lesions in the subcutaneous tissues measuring 4 × 6 mm and 2 × 5 mm separated by a distance of 3.4 cm (Figure 2). Due to the inability to palpate these two lesions on physical exam, it was decided to place radioactive seeds for intra-operative localization.
Figure 2.
Gadolinium-enhanced fat-saturation T1-weighted MR images of the right lower extremity which depicts one of the in-transit metastases seen in the MRI on the left and one of the local/superficial recurrences discovered on Physical Exam (PE) seen in the MRI on the right. [Powerpoint Slide]
Technique
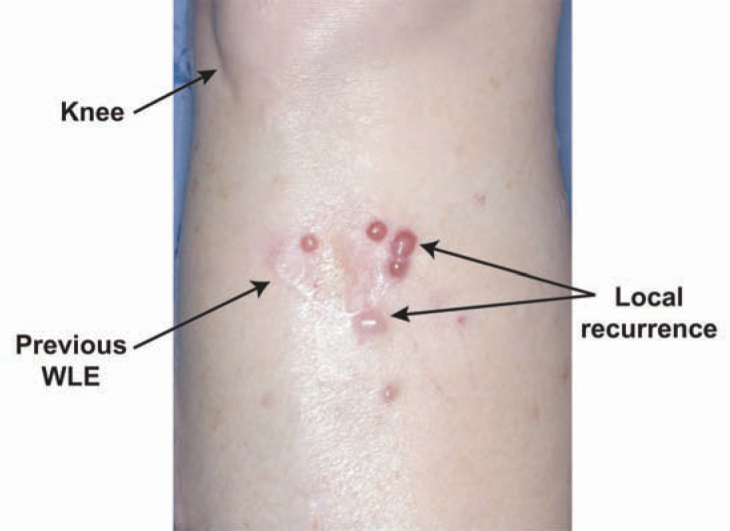
Radioactive seed localization (RSL) is accomplished with a 4.5 × 0.8-mm titanium seed with 100-200 mCi of 125I (Cardinal Health, Woodland Hills, CA). The seed is placed into an 18-gauge spinal needle with the tip occluded with bone wax and then guided to the lesion(s) under ultrasound or stereotactic guidance, in this case using ultrasound for each lesion. The seed is then deployed through the bone wax with a stylet (Figure 3). Six BB's were placed on the superficial recurrences of this patient and an AP and lateral film performed (Figure 4). These radiographs in turn were used by the surgeon to give a gross estimate of where the lesions are in relation to local landmarks (visible recurrences).
Figure 3.
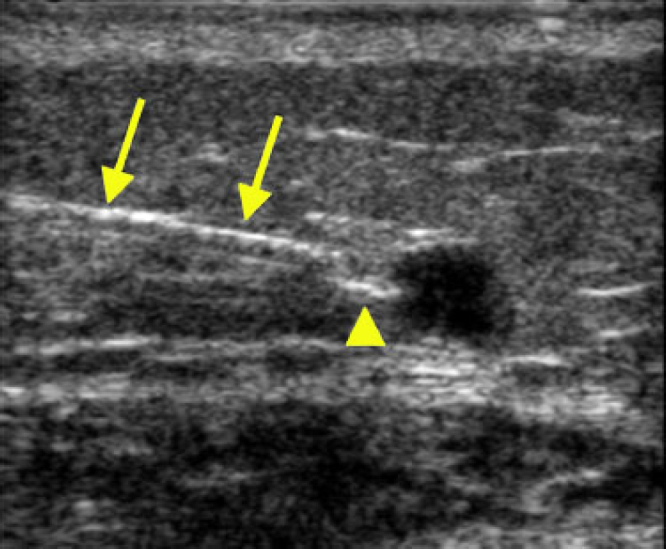
Sonogram of the right leg (15-MHz probe) demonstrates placement of a seed into one of the subcutaneous melanoma lesions. Arrows denote the 18 gauge spinal needle; arrowhead points to the seed prior to deployment into the lesion. [Powerpoint Slide]
Figure 4.
AP and Lateral films of right lower extremity which displays the gross location of the radioactive seeds in relation to the palpable recurrences [Powerpoint Slide]
These radiographs in turn were used by the surgeon to give a gross estimate of where the lesions are in relation to local landmarks (visible recurrences). The following day the patient underwent a wide local excision of the local recurrence obtaining a 1 cm margin with an immediate free flap reconstruction. Next, the two in-transit metastases were approached. In-transit metastases are thought to arise from lymphatic seeding of the subcutaneous tissue between the primary lesion and the regional lymph nodes, and are distinguished from satellitosis by having a distance greater than 2 cm from the primary lesion.[4] A gamma probe (Neo2000, Neoprobe Corporation, Dublin, OH) was used to localize the two areas of highest radioactivity. The gamma probe is a hand-held device that is set to detect scintigraphic hot spots (i.e. radioactive sentinel lymph nodes or radioactive seeds). Due to the close distance between the two metastases, one incision was utilized to resect the lesions using the gamma probe to provide ongoing feedback. Pathologic examination revealed successful excision of two in-transit metastases with a clear margin of adipose tissue.
Discussion
In 2005, an estimated 59,580 new cases of melanoma were diagnosed and approximately 7770 deaths occurred.[1] Since the 1970's, melanoma of the skin has steadily increased in incidence, and is now the sixth and seventh leading cancer diagnosis in men and women, respectively.[1, 2, 3] In-transit metastases usually present as small palpable nodules located between the primary melanoma site and the lymph node basin that receives drainage from the melanoma site. In one study of over 1500 stage I and II patients, 12.5% of patients developed in-transit metastasis.[5] In addition, there was an increased risk of in transit metastases with more positive lymph nodes: a 10.8% rate with one positive regional node versus a 31.4% rate with three or more positive regional nodes.[5]
In transit metastases can be associated with significant morbidity including bleeding, drainage from necrotic lesions, and pain. The American Joint Committee on Cancer stages in-transit metastasis as stage IIIB or IIIC, depending on regional node status with an associated five year mortality of 26.7-52.8%.[6] If possible, surgical excision is the treatment of choice for a small number of subcutaneous in-transit metastases and can be curative.[7] High rate of local recurrence after resection occurs due to the inability to remove all metastatic disease. In the era of improved imaging, smaller and deep subcutaneous lesions are now diagnosed. Surgical removal of these lesions is difficult due to their physically occult nature. Localization procedures, including wire localization or intra-operative ultrasound, have inherent limitations. Herein we report the novel technique of RSL of these lesions.
Radioactive seed localization has been reported by us and others for non-palpable breast lesions with improved margin status and patient satisfaction.[8, 9] The use of RSL for non-palpable breast lesions has resulted in easier placement by the radiologist and easier retrieval by the surgeon. The application of RSL to melanoma has not been previously reported.
With the advent of PET, MRI, Computed Tomography (CT), and high resolution ultrasound, smaller metastatic and in-transit lesions are being discovered. In fact, the resolution of FDG-PET is 5-6 mm, with a 90% sensitivity in tumors greater than 78 mm[3] and the smallest tumor detected in one study was less than 30mm[3, 10]. Often times these lesions are nonpalpable. Since surgical excision is the appropriate therapy for a small number of in-transit metastases, localization has become increasingly important for the treatment of metastatic melanoma.
RSL has advantages over other methods of intraoperative localization such as wire localization and intraoperative ultrasound. With wire localization, generally patients need to undergo surgery on the same day as radiographic wire placement, while radioactive seeds can be placed the day before surgery or longer. This provides improved patient convenience and operative and radiologic scheduling. Intraoperative ultrasound may require the presence of a radiologist within the operating room suite to help localize the lesion if the surgeon is not trained in ultrasonic evaluation. This is particularly true for small lesions where visualization is difficult.
In this case of non-palpable in-transit metastatic melanoma, RSL was both effective and technically intuitive. RSL has great potential for the localization of a variety of non-palpable lesions. Of note, the radioactive seed is not FDA approved for this procedure; therefore, one needs to investigate his/her hospital processes prior to use, including nuclear regulatory requirements.
In summary, RSL proved an effective means of localization of in-transit metastatic melanoma in this patient and should be considered for utilization for this purpose and future studies of wider application.
Footnotes
Disclaimer: The radioactive seed is a Food and Drug Administration (FDA) approved devise used in an off label application
Competing Interests: The authors declare that no competing interests exist.
Published: June 20, 2006
References
- 1.Jemal A, Murray T, Ward E, Samuels A, Tiwari R, Ghafoor A, Feuer E. Cancer Statistics, 2005. CA Cancer J Clin. 2005;55:10–30. doi: 10.3322/canjclin.55.1.10. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Devesa SS, Hartge P, Tucker MA. Recent trends in cutaneous melanoma incidence among whites in the United States. Journal of the National Cancer Institute. 2001;93(9):678–683. doi: 10.1093/jnci/93.9.678. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Jemal A, Clegg LX, Ward E, Ries LA, Wu X, Jaminson PM. Annual report to the nation on the status of cancer, 1975-2001, with special feature regarding survival. Cancer. 2004;101(1):3–27. doi: 10.1002/cncr.20288. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.AJCC Cancer Staging Manual. 6th Edition. Springer; New York: 2002. pp. 209–216. [Google Scholar]
- 5.Cascinelli N, Bufalino R, Marolda R, Belli F, Nava M, Galluzzo D. Regional non-nodal metastases of cutaneous melanoma. Eur J Surg Oncol. 1986;12:175. [PubMed] [PubMed] [Google Scholar]
- 6.Balch CM, Buzaid AC, Soong S, Atkins MB, Cascinelli N, Coit DG. Final version of the American joint committee on cancer staging system for cutaneous melanoma. J of Clin Onc. 2001;19(16):3635–3648. doi: 10.1200/JCO.2001.19.16.3635. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Cutaneous Melanoma. 4th Edition. Quality Medical Publishing; St. Louis: 2003. pp. 440–448. [Google Scholar]
- 8.Gray RJ, Salud C, Nguyen K, Dauway E, Friedland J, Berman C. Randomized prospective evaluation of a novel technique for biopsy or lumpectomy of nonpalpable breast lesions: radioactive seed versus wire localization. Annals of Surg Onc. 2001;8(9):711–715. doi: 10.1007/s10434-001-0711-3. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Gray RJ, Pockaj BA, Karstaedt PJ, Roarke MC. Radioactive seed localization of nonpalpable breast lesions is better than wire localization. Am J Surg. 2004 Oct;188(4):377–380. doi: 10.1016/j.amjsurg.2004.06.023. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Wagner JD, Schauwecker DS, Davidson D, Wench S, Jung S, Hutchins G. FDG-PET sensitivity for melanoma lymph node metastases is dependent on tumor volume. J of Surg Onc. 2001;77:237–242. doi: 10.1002/jso.1102. [PubMed] [DOI] [PubMed] [Google Scholar]