Abstract
We report a case of an adolescent female who had an initial outside clinical and imaging presentation that was considered highly suspicious for metastatic osteosarcoma. Extensive evaluation led to the diagnosis of chronic recurrent multifocal osteomyelitis. If this etiology had been considered earlier in the patient's clinical course, her diagnostic evaluation may have been less involved and treatment could have commenced sooner. When this entity is a diagnostic possibility along with neoplasm, strong consideration should be given to proceeding directly to open surgical biopsy due to the difficulty in diagnosing this lesion from small percutaneously-obtained biopsy samples.
Abbreviations: SAPHO, synovitis, acne, pustulosis, hyperostosis; CRMO, chronic recurrent multifocal osteomyelitis; CT, computed tomography; MRI, magnetic resonance imaging; CC, cranial-caudal; AP, anterior-posterior; ML, medial-lateral; ESR, erythrocyte sedimentation rate
Introduction
A sclerosing form of osteomyelitis was first described by Garré in 1893 [1]. The osteomyelitis he described caused distention and thickening of bone without sequestration or fistulization [1, 2]. The terminology relating to nonbacterial chronic osteomyelitis since that time has been confusing. Over 50 different terms have been used to describe what has been presumed to be the same disease entity [3, 4, 5]. The most accepted term currently being used is SAPHO syndrome. SAPHO stands for synovitis, acne, pustulosis, hyperostosis, and osteitis. Although dermatologic manifestations are included along with bone manifestations, patients do not need to exhibit all of the syndrome components. Chronic recurrent multifocal osteomyeltis (CRMO) is a subtype of the SAPHO syndrome that is most commonly seen in the metaphyseal lower extremity long bones of children and adolescents [4, 5]. Multifocality does not need to be present for a patient to have this diagnosis [4]. Prominent osteoproliferative change causing cortical thickening and medullary canal narrowing is the most striking finding seen in CRMO. In some cases, it may be impossible to distinguish chronic recurrent multifocal osteomyelitis from a neoplastic process without tissue biopsy [6]. The etiology of this entity is unknown. It has been theorized that it is either a seronegative spondyloarthropathy or is due to infection with a low virulence organism [3, 4, 5]. The mainstay of treatment is pain control with nonsteroidal anti-inflammatory medications. CRMO resolves spontaneously but can have a prolonged course with recurrent exacerbations of pain.
Case Report
A fifteen-year-old female was referred from an outside institution for definitive diagnosis and treatment of presumed metastatic osteosarcoma. She reported left lower extremity pain for over one year and described the pain as a dull ache with sharp exacerbations. Her symptoms were most severe at night. She had no history of trauma and had no systemic complaints of fever, chills, rash or abdominal pain. Her past medical and family history was unremarkable.
Physical examination revealed a pleasant, cooperative, thin female. Her gait was normal. There was no discrepancy with leg length. Examination of her left hip revealed a large fusiform, firm fullness affecting her proximal femur. She had no lymphadenopathy. Laboratory analysis revealed an elevated blood C-reactive protein.
Outside imaging was not available for review at the time of her initial evaluation at our institution. The patient proceeded directly to computed tomography (CT)-guided biopsy of her proximal femur (Figure 1). Multiple 15g core biopsy samples were placed into formalin for pathologic evaluation. The biopsy revealed fragments of abnormal remodeled bone surrounded by bland appearing fibrous stroma. Rare enlarged atypical cells were present but the appearance of these cells was nonspecific.
Figure 1.

CT-fluoroscopic image showing the biopsy needle (arrow) traversing thick periosteal and endosteal new bone in the subtrochanteric region of the left hip. While there is prominent osteoproliferative change, the borders of the new bone are smooth. The smooth contour and multiple lytic areas suggest the possibility of chronic osteomyelitis. [Powerpoint Slide]
Imaging was subsequently performed for presumed tumor staging. Radiographs demonstrated a large sclerotic lesion in the proximal (Figure 2). An unenhanced CT confirmed the irregular femoral lesion (Figure 3) and identified an additional, similar lesion in the sacrum (Figure 4). Both lesions had a smooth contour of the periosteal new bone and multiple small lytic regions. On magnetic resonance imaging (MRI) (Figure 5), the femoral mass measured 12.6 cm in the cranial-caudal dimension, × 8.1 cm in the anterior-posterior dimension, × 6.3 cm in the medial-lateral dimension. The femoral mass was seen to abut and possibly invade the vastus intermedius muscle and the deep margin of the superficial femoral and deep femoral vessels. Both the femoral and sacral bone lesions had moderate edema in the marrow edema and surrounding soft tissues. There was a moderate left hip joint effusion.
Figure 2.

An AP radiograph of the proximal left femur demonstrates a large sclerotic lesion extending from the intertrochanteric region into the proximal diaphysis. [Powerpoint Slide]
Figure 3.

A coronal reformatted CT shows the same prominent, smooth new bone (arrows) involving the proximal femur, as was seen on the radiograph. [Powerpoint Slide]
Figure 4.
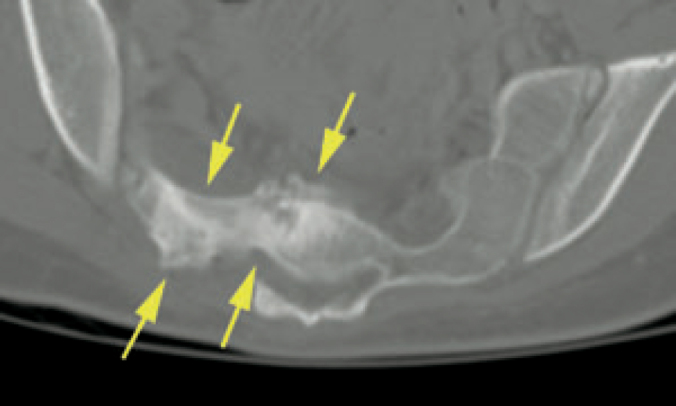
An axial CT image through the mid sacrum demonstrates an additional irregular region of sclerosis and periosteal new bone extending from midline to the right (arrows). [Powerpoint Slide]
Figure 5.
Coronal T1-weighted (A), coronal T2-weighted fat-suppressed (B), and axial T2-weighted fat-suppressed (C). MR images of the proximal left femur demonstrate prominent periosteal new bone and moderate edema. Extension of the mass into the surrounding soft tissues seen on T2-wieghted images was equivocal for invasion versus mass effect displacing the normal structures. [Powerpoint Slide]
After imaging, the possibility of osteomyelitis was raised. The patient then underwent a surgical Jamshidi needle biopsy under general anesthesia in the operating room. This biopsy produced similar tissue as the CT-guided biopsy. Additional samples were placed in saline for culture. Cultures of the tissue were negative for bacteria and fungi.
Since the patient had been referred for presumed osteosarcoma and there was no definitive diagnosis from either needle biopsy, it was felt that a larger tissue sample would be needed to exclude tumor. The patient was brought back to the operating room one month later where she underwent an open biopsy where large portions of bone were removed using an oscillating saw. Cultures of this tissue were also negative. The pathologic examination revealed fibroblastic sclerosing proliferation, consistent with sclerosing osteomyelitis. There were no malignant cells.
Discussion
Chronic recurrent multifocal osteomyelitis is considered a subtype of SAPHO syndrome. CRMO most often affects children or young adults. It is characterized by sclerotic osseous lesions without a detectable causative organism or tumor [7]. The long bone metaphyses are most commonly involved. Involvement of the clavicle and spine can also be seen [7]. The disease has an insidious onset and a prolonged course. Patients typically have recurrent episodes of pain [3]. The laboratory findings are nonspecific but suggest an inflammatory process [7]. Abnormal lab tests may include an elevated erythrocyte sedimentation rate (ESR), elevated alkaline phosphatase and an elevated c-reactive protein. Only rarely will the patient have an abnormal white blood cell count or differential count.
Pathogenesis
The etiology of chronic recurrent multifocal osteomyelitis is unknown. This may represent a seronegative spondyloarthropathy. Infection with an organism of low virulence has also been theorized [3]. Bacteria have rarely and inconsistently been isolated from biopsy samples [3]. Cultured organisms include Propionibacterium acnes, Streptococcus epidermidis, Bacillus species and alpha-Streptococcus [2, 8]. It is unclear if these bacteria represented the true infecting agents or contaminants.
Imaging
Chronic recurrent multifocal osteomyelitis can be difficult to differentiate from neoplastic processes, such as osteosarcoma, osteoblastoma, osteoid osteoma and Ewing sarcoma, based on imaging alone [9]. CRMO is often seen as a single or multiple sclerotic lesions with varying amounts of periosteal and endosteal new bone in the metaphysis of a long bone in a child or young adult [8]. Radiographically, there is expansile sclerosis and hyperostosis. The feature that somewhat differentiates CRMO from neoplasm is the smooth character of the periosteal new bone. Periosteal reaction in neoplastic processes tends to be more spiculated and ill-defined. This feature, however, is not diagnostic. Scattered lytic foci may also be present within the regions of new bone formation.
Radionuclide bone scan will show increased radiotracer uptake in both CRMO and neoplasm, thus it is not helpful in differentiating the two entities, but it can be helpful to identify additional regions of involvement. The appearance on MRI varies with the activity of the disease. Active lesions have prominent contrast enhancement and edema within and surrounding the bone. As the process becomes inactive, contrast enhancement and edema progressively decrease [10]. Soft tissue abscesses are absent in CRMO and SAPHO. Although growth disturbances are rare, serial radiographs are helpful to monitor bone maturation. Serial radiographs are essential to assess for any suspicious change in the lesion in case it had been initially misdiagnosed. Malignant transformation has not been reported.
Pathology
The key function of the histologic examination is to exclude malignancy. This requires a variable amount of tissue depending on institutional protocol and recommendations from the interpreting pathologist. The amount of tissue normally obtained from a needle biopsy can be inadequate to completely exclude a malignant lesion, due to the possibility of sampling error. The histopathological changes of chronic recurrent multifocal osteomyeltis are nonspecific and consist of subacute or chronic bone inflammation and reactive new bone [7]. Microscopically, the new bone formation may be seen along with marrow fibrosis, neovascularization and a mixture of lymphocytes, plasma cells and macrophages [3].
Treatment
The recommended treatment is steroidal or nonsteroidal anti-inflammatory medications. Antimicrobial therapy has no effect on the course of the disease [5, 8]. The goal of treatment is alleviating symptoms until the disease process spontaneously resolves [8]. The course of the disease tends to be prolonged and unpredictable. Patients have frequent episodes of painful swelling with intermittent periods of remission.
Conclusion
Chronic recurrent multifocal osteomyelitis can be difficult to differentiate from a neoplastic process. Single or multiple regions of abundant but smooth new bone formation, combined with a non-neoplastic histologic examination, suggests this diagnosis. The lack of a causative agent on culture should not dissuade the clinician from this diagnosis. Although the etiology of this entity is unknown, bone biopsy samples should always be placed in both saline and formalin to allow for culture when indicated. Since CRMO tends to be a diagnosis of exclusion, a generous tissue sample is often needed to completely eliminate the possibility of malignancy. One should give strong consideration to proceeding directly to open surgical biopsy if the radiologic differential diagnosis of a lesion includes both CRMO and malignancy.
Footnotes
Competing Interests: The authors declare that no competing interests exist.
Published: June 13, 2006
References
- 1.Garré C. Ueber besondre Formen und Folgezustande d. akuten infekt. Osteomyelitis Beitr z klin Chir. 1893;10:257. [Google Scholar]
- 2.Collert S, Isacson J. Chronic sclerosing osteomyelitis (Garre) Clin Orthop Relat Res. 1982 Apr;(164):136–140. [PubMed] [PubMed] [Google Scholar]
- 3.Stewart A, Carneiro R, Pollock L, Shaw D. Case report 834: Chronic sclerosing osteomyelitis of the mandible with long bone periostitis. Skeletal Radiol. 1994 Apr;23(3):225–227. doi: 10.1007/BF00197468. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Earwaker JW, Cotten A. SAPHO: syndrome or concept? Imaging findings. Skeletal Radiol. 2003 Jun;32(6):311–327. doi: 10.1007/s00256-003-0629-x. [PubMed] Epub 2003 Apr 29. [DOI] [PubMed] [Google Scholar]
- 5.Boutin RD, Resnick D. The SAPHO syndrome: an evolving concept for unifying several idiopathic disorders of bone and skin. AJR Am J Roentgenol. 1998 Mar;170(3):585–591. doi: 10.2214/ajr.170.3.9490935. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Segev E, Hayek S, Lokiec F, Ezra E, Issakov J, Wientroub S. Primary chronic sclerosing (Garre's) osteomyelitis in children. J Pediatr Orthop B. 2001 Oct;10(4):360–364. [PubMed] [PubMed] [Google Scholar]
- 7.Jurik AG, Moller SH, Mosekilde L. Chronic sclerosing osteomyelitis of the iliac bone. Etiological possibilities. Skeletal Radiol. 1988;17(2):114–118. doi: 10.1007/BF00365138. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Suei Y, Tanimoto K, Taguchi A. Possible identity of diffuse sclerosing osteomyelitis and chronic recurrent multifocal osteomyelitis. One entity or two. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995 Oct;80(4):401–408. doi: 10.1016/s1079-2104(05)80332-4. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Viejo-Fuertes D, Rossillon R, Mousny M. Primary chronic sclerosing osteomyelitis–a case-report. Joint Bone Spine. 2005 Jan;72(1):73–75. doi: 10.1016/j.jbspin.2004.02.007. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Anderson SE, Heini P, Sauvain MJ. Imaging of chronic recurrent multifocal osteomyelitis of childhood first presenting with isolated primary spinal involvement. Skeletal Radiol. 2003 Jun;32(6):328–336. doi: 10.1007/s00256-002-0602-0. [PubMed] [DOI] [PubMed] [Google Scholar]



