Abstract
Background:
Eribulin mesylate (eribulin) is a first-in-class halichondrin B-based microtubule dynamics inhibitor. To compare the anti-angiogenic activity of eribulin to that of bevacizumab, we compared tumour vessel remodelling and reoxygenation between the two agents.
Methods:
Patients with advanced breast cancer with stage III/IV were eligible for the study. Patients were assigned to receive either eribulin or single-agent bevacizumab. Tissue concentrations of oxyhaemoglobin (O2Hb) and deoxyhaemoglobin (HHb), and oxygen saturation (SO2) of breast tumours before and day 7 after the first infusion were repeatedly measured using diffuse optical spectroscopic imaging (DOSI). A pair of blood samples was collected for multiplex biomarker studies.
Results:
Baseline DOSI measurement of all 29 patients (eribulin, n=14 and bevacizumab, n=15) revealed significantly higher tumour concentrations of O2Hb and HHb than that in the normal breast tissue. After eribulin treatment, DOSI revealed a significant decrease in HHb concentration and increased SO2 during the observation period. This trend was not observed for bevacizumab. Instead, bevacizumab significantly decreased the concentration of O2Hb. The multiplex biomarker study revealed that both eribulin and bevacizumab decreased plasma concentrations of VEGF and bFGF, but only eribulin treatment suppressed the plasma concentration of TGF-β1.
Conclusions:
Eribulin, but not bevacizumab, treatment increased tumour SO2. Suppression of TGF-β1 by eribulin could have a favourable anti-angiogenic effect. Our results suggest that differences in vascular remodelling between these two agents may account for their different effects on tumour reoxygenation.
Keywords: eribulin, bevacizumab, angiogenesis, oxygenation, optical imaging, epithelial–mesenchymal transition
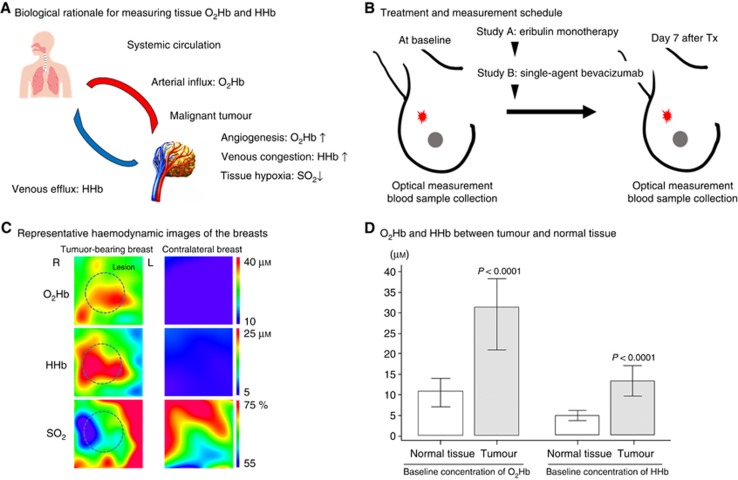
The highly vascularised nature of breast cancer makes it a strong candidate for anti-angiogenic therapy (Folkman, 1971). Bevacizumab, a humanised anti-VEGF monoclonal antibody, is known to play a pivotal role in inhibiting angiogenesis and to improve perfusion in a variety of cancers (Keating, 2014). A pivotal randomised phase III trial of metastatic breast cancer (MBC; ECOG2100) revealed that bevacizumab in combination with paclitaxel increased progression-free survival (PFS) but did not prolong overall survival (OS) compared with paclitaxel alone (Miller et al, 2007). Thus, the addition of bevacizumab to chemotherapy failed to have the drastic impact on survival that was anticipated. Eribulin mesylate (eribulin) was recently approved as a first-in-class halichondrin B-based microtubule dynamics inhibitor for MBC patients and has very unique features according to results from a pooled analysis of phase III clinical trials (EMBRACE and Study301; Twelves et al, 2014). In contrast to bevacizumab, eribulin monotherapy was observed to prolong OS in MBC patients who had previously received anthracycline- or taxane-based chemotherapy over that of conventional chemotherapy. However, the PFS did not differ from that of controls in either arm of the study. Recent research has revealed that eribulin has a distinct biological profile with respect to its mechanism of anti-angiogenesis action (Dybdal-Hargreaves et al, 2015). Using dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) to study a rat xenograph model of human breast cancer cells, Funahashi et al reported that tumour perfusion measured by average volume transfer constant value (Ktrans) increased in the tumour core within day 6 of eribulin infusion (Funahashi et al, 2014). In contrast, the results of DCE-MRI studies of bevacizumab were highly ambiguous (Mehta et al, 2011; Van der Veldt et al, 2012). A DCE-MRI study of bevacizumab in 70 patients with locally advanced breast cancer reported a strong decrease in multiple parameters, including tumour perfusion, concluding that bevacizumab administration was not associated with a histological response in the setting of neoadjuvant chemotherapy (Etxano et al, 2015). Hence, we hypothesise that the effects of eribulin on tumour vascularity may have a favourable impact on therapeutic outcomes and patient survival. We have recently established the use of near-infrared diffuse optical spectroscopic imaging (DOSI; TRS20; Hamamatsu Photonics K.K., Japan), a non-invasive functional imaging technique without ionising radiation exposure that quantifies in vivo tissue concentrations of oxyhaemoglobin (O2Hb), deoxyhaemoglobin (HHb), and oxygen saturation (SO2) in the breast (Ueda et al, 2013). Many investigators report that monitoring of tumour concentrations of O2Hb and HHb offers a novel opportunity for studying drug mechanisms in breast cancer and haemodynamic responses (Tromberg et al, 2005; Cerussi et al, 2011; Roblyer et al, 2011). The microvascular concentration of O2Hb is dominant to arterial blood inflow, whereas accumulation of HHb inside a tumour occurs in response to impaired venous outflow that results in tissue hypoxia (Figure 1A). Oxygen saturation is considered a good indicator of tumour tissue oxygenation compared with that of surrounding normal breast.
Figure 1.
(A) Monitoring tumour O2Hb and HHb illustrates arterial influx and venous efflux, respectively, inside the tumour. Tumour SO2 indicates the status of tissue oxygenation. (B) Breast tissues were analysed using optical imaging, and a pair of blood samples was collected before treatment and day 7 after the start of infusion. (C) Breast tumours were measured using an ultrasonography-assisted optical imaging system (TRS20, Hamamatsu Photonics K.K., Hamamatsu, Japan), and the contralateral normal breast was analysed as control. (D) Baseline concentrations of tumour O2Hb and HHb were significantly higher than those of the normal breast tissue.
We proposed that monitoring of these haemodynamic biomarkers could be used to improve our understanding of the biology of vascular remodelling and oxygenation response to these drugs. In this study, patients with advanced breast cancer were assigned to receive either eribulin monotherapy or single-agent bevacizumab followed by paclitaxel. Tumour concentrations of O2Hb, HHb, and SO2 at baseline and day 7 after the first drug infusion were measured. In addition, a pair of blood samples was collected during the observation window, and the changes in these plasma biomarkers were compared.
Methods:
Treatment and study design
Patients with histologically confirmed locally advanced stage III/IV breast cancer were enrolled in this study from June 2013 to July 2015. Locally advanced breast cancer was defined as a tumour >5 cm in size or a tumour with fixation to the chest wall or skin. In this study, 15 patients were assigned to study A, receiving eribulin monotherapy (1.4 mg m−2, i.v.) weekly, with rest every third week. Fifteen patients were assigned to study B, receiving a single dose of bevacizumab (10 mg kg−1, i.v.) as an induction therapy (day 1) followed by weekly paclitaxel (80 mg m−2, i.v.) beginning on day 7. Combination therapy was continued in 14-day cycles, with paclitaxel administered on days 1, 8, and 15, and bevacizumab on day 1. Breast tissues were optically analysed using DOSI before and day 7 after the induction of eribulin monotherapy or single-agent bevacizumab (and before combination chemotherapy), and a pair of blood samples was collected at that time (Figure 1B). Tumour responses were examined with serial scans (baseline and after 2–4 courses of treatment) of DCE-MRI and 2-deoxy-2-18F-fluoro-D-glucose (FDG) positron emission tomography (PET) scans during treatment in routine practice. This study was approved by the SMUIMC Institutional Review Board (12–084, 13–132, 14–055) and informed consent was obtained from all individual participants included in the study. The study is registered on UMIN Clinical trial registration (000015837 and 000015839).
Functional optical imaging and haemodynamic biomarkers
We developed a TRS breast imaging system that uses time-correlated single-photon counting for measuring temporal response profiles of tissue against optical pulse inputs and enables quantitative analysis of light absorption and scattering in tissues according to the photon diffusion theory. Details of the TRS breast imaging system have been previously published (Ueda et al, 2013; Nakamiya et al, 2014). This approach was used to quantify absolute concentrations of O2Hb and HHb in tissues. The per cent SO2 was calculated as [O2Hb]/total [Hb] (O2Hb+HHb) × 100. We used an ultrasound-assisted optical probe to detect the largest tumour lesions and made a 10-mm square grid map in which the breast tumour was centred. The grid map of a tumour-bearing breast comprised 7 × 7 points with a 10-mm intervals between each point in the x–y dimension. Custom imaging software (DataBreastViewer, version 109; SincereTechnology Corp., Kanagawa, Japan) was used to perform 2D image processing and analysis. Representative optical images are shown in Figure 1C. Following ultrasound examination, the lesion region of interest (ROI), a circular area with a 2-cm radius, was traced manually over the area of high tHb concentration on the US map of the tumour. The size and position of ROI were fixed for data analysis of both baseline and 7 days after treatment visits. The mean concentrations of O2Hb and HHb and mean per cent SO2 were calculated. We monitored changes in the mean levels of these haemodynamic biomarkers during an observational window.
Circulating biomarkers
Peripheral blood samples were obtained from patients who agreed to participate in the blood biomarker study. Plasma samples were separated by centrifugation and then aliquoted and stored at–80 °C until ELISA of free (non-bevacizumab bound) VEGF, bFGF, FLT-3L, EGF, G-CSF, TNFα, IL1b, IL4, IL6, IL8, IL10, and IL12p40 with a CLIA-certified multiplex protein array from Luminex Multiplex Assays Human Cytokine Magnetic 30-Plex and TGF-β1 using ELISA kits from R&D Systems. All samples were assayed in duplicate.
Statistical analysis
We considered that at least 10 patients in each study group were required to compare variables between the two groups; 15 patients were registered to each group, making it a total of 30 patients during the 2-year pilot study period. Changes in biomarkers are reported as ratios and were assessed using the one-sample, two-sided, exact Wilcoxon test. Samples for which biomarker measurements were missing were excluded from the analysis. P<0.05 was considered statistically significant. The data were analysed using Medcalc (Mariakerke, Belgium).
Results:
Haemodynamic response after treatment
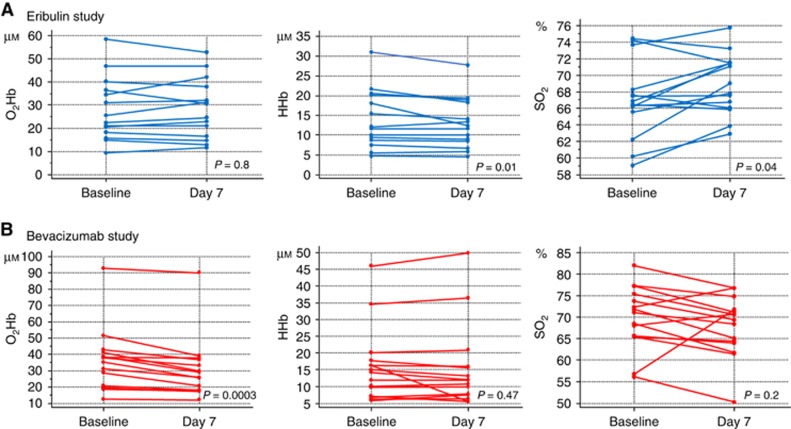
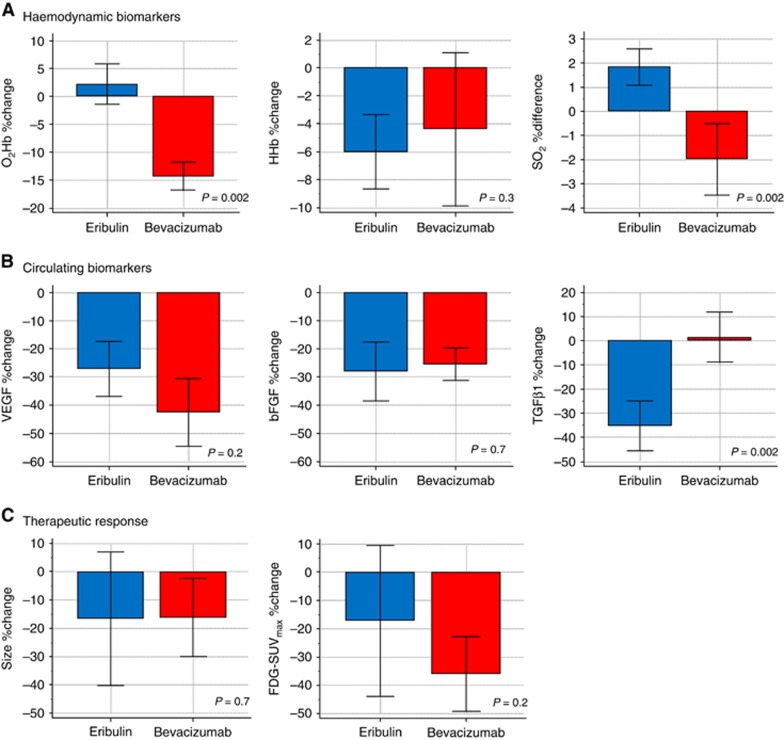
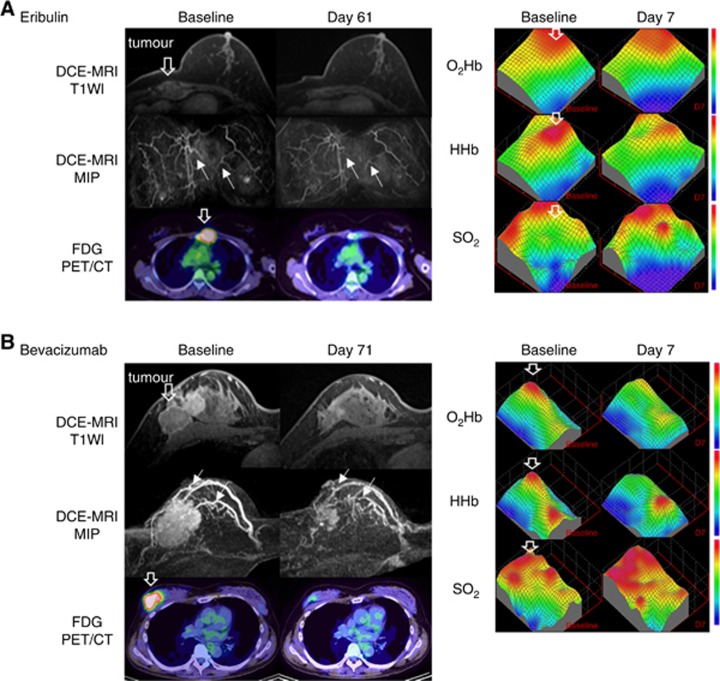
Data from 14 patients who received eribulin and 15 patients who received bevacizumab were evaluable in the optical study. Patient characteristics and details of treatment are shown in Table 1. Optical imaging demonstrated that the average tumour HbO2 and HHb concentrations before treatment initiation were significantly higher than those of the contralateral normal breast tissue, as shown in Figure 1D (P<0.0001 each). During eribulin treatment, tumour SO2 levels collectively increased on day 7 after the start of treatment (P=0.04), accompanied by a significant decrease in the tumour concentration of HHb (P=0.01) (Figure 2A). In the majority of patients receiving single-agent bevacizumab, the tumour concentration of O2Hb decreased (P=0.0003), but mean levels of tumour SO2 did not change at day 7 compared with baseline (Figure 2B) (P=0.2). The per cent decrease in O2Hb concentration and per cent SO2 in bevacizumab-treated patients were both significantly greater than those of eribulin-treated patients (both P=0.002) (Figure 3A). Representative cases are shown in Figure 4.
Table 1. Patient characteristics.
| Characteristic | Eribulin (n=14) | Bevacizumab (n=15) |
|---|---|---|
|
Mean age | ||
| y/o (s.d.) | 50.1 (9.4) | 52.4 (10.4) |
|
Menstrual status | ||
| Pre | 6 | 7 |
| Post | 8 | 8 |
|
Mean size | ||
| mm (s.d.) | 48.4 (14.5) | 48.3 (24.7) |
|
Histology | ||
| IDC | 14 | 14 |
| ILC | 0 | 1 |
|
ER | ||
| Positive | 10 | 11 |
| Negative | 4 | 4 |
|
PgR | ||
| Positive | 5 | 9 |
| Negative | 9 | 6 |
|
HER2 | ||
| Positive | 1 | 0 |
| Negative | 13 | 15 |
|
Distant metastasis | ||
| Positive | 9 | 6 |
| Negative | 5 | 9 |
|
Prior therapy | ||
| Anthracycline | 13 | 6 |
| Taxane | 13 | 8 |
| Trastuzumab | 1 | 0 |
| Endocrine therapy | 2 | 3 |
Abbreviations: ER=oestrogen receptor; IDC=invasive ductal carcinoma; ILC=invasive lobular carcinoma; PgR=progesterone receptor.
Figure 2.
Comparison of optical measurements of tumour O2Hb and HHb concentrations, and SO2 between baseline and day 7 after the start of eribulin (A) and bevacizumab (B).
Figure 3.
Comparison of per cent change in tumour concentrations of O2Hb and HHb, and differences in tumour SO2 between eribulin and bevacizumab (A). Comparison of per cent change in plasma concentrations of VEGF, bFGF, and TGF-β1 between eribulin and bevacizumab (B). Tumour size reduction and changes in glucose metabolism after 2–4 courses of chemotherapy were compared between eribulin and bevacizumab (C).
Figure 4.
Case presentation of serial images using DCE-MRI, FDG-PET/CT, and DOSI in a responding tumour treated with eribulin (A) and bevacizumab (B) before and after the second cycle of treatment.(A) A 40-year-old woman had parasternal lymph node metastasis detected 23 months after definitive surgery. (B) A 51-year-old woman had locally advanced breast cancer at diagnosis (T3N1M0). After the start of chemotherapy, both tumours showed significant shrinkage in size and decreased FDG uptake as measured by DCE-MRI and FDG-PET/CT scans 2–4 courses after the start of chemotherapy, respectively. The eribulin-treated tumour showed a decrease in HHb concentration and an increase in SO2. The bevacizumab-treated tumour showed decreased O2Hb and HHb concentrations coincident with an increase in SO2. The downward open arrow indicates the lesion location. The white arrow indicates enhancement of tumour blood vessels. CT=computed tomography; DCE-MRI=dynamic contrast-enhanced magnetic resonance imaging; DOSI=diffuse optical spectroscopic imaging; FDG=2-deoxy-2-18F-fluoro-D-glucose; HHb=deoxyhaemoglobin; O2Hb=oxyhaemoglobin; PET=positron emission tomography; SO2=oxygen saturation.
Changes in circulating biomarkers after treatment
Blood samples from 9 patients treated with eribulin and 10 patients treated with bevacizumab were analysed for circulating biomarkers and compared (Figure 3B). Significant decreases in plasma concentrations of VEGF and bFGF compared with baseline were observed in patients who received either eribulin or bevacizumab, with no difference between treatments. A significant decrease in plasma TGF-β1 concentration was seen only in patients treated with eribulin, and this decrease was significantly greater than that observed in patients treated with bevacizumab alone (P=0.002).
Therapeutic response to chemotherapy
Tumour response measured using MRI and FDG-PET/CT was evaluated after 2–4 courses of chemotherapy (Figure 3C). Tumour size reduction and change in FDG-standardised uptake value (SUV)max did not differ between eribulin-treated and bevacizumab-treated tumours (P=0.7 and 0.2, respectively).
Discussion:
We hypothesised that optical imaging with DOSI could be used to monitor vascular remodelling and reoxygenation in response to agents, such as eribulin and bevacizumab, by measuring haemodynamic parameters in breast tumours. In this study, we observed that bevacizumab significantly decreased tumour O2Hb concentrations after the start of infusion. Because arterial vessels are rich in O2Hb, such a decrease may indicate vessel pruning and extensive inhibition of neo-angiogenesis by neutralization of circulating VEGF. In the course of vascular remodelling, endothelial cells (ECs) are induced from bone marrow and are properly reconstructed into the microvasculature and reoxygenation could consequently occur (Jain, 2005). In fact, individuals showed a variety of tumour changes in SO2 after the start of bevacizumab. Although the overall tumour SO2 change did not differ significantly during the observation window, we previously reported that responding patients who had remarkable tumour shrinkage also had higher SO2 after treatment, whereas non-responding patients had lower SO2 after treatment (Ueda et al, 2014). These results suggest that when vascular remodelling works properly, bevacizumab should induce oxygenation. However, if the existing vasculature is destroyed without subsequent reorganisation, bevacizumab could lead to further hypoxia, contraindicating continuation of treatment.
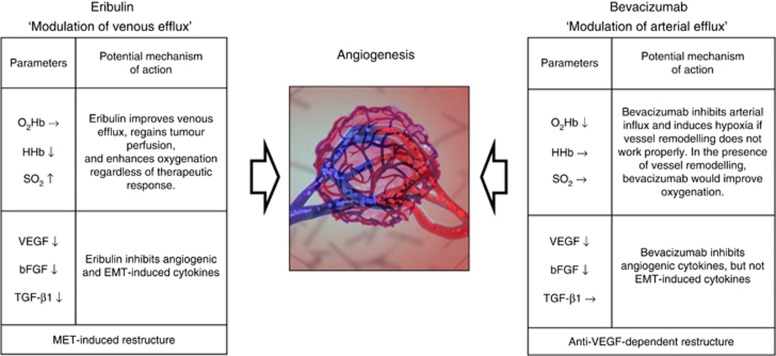
In contrast to bevacizumab, eribulin treatment significantly decreased the tumour HHb concentration and consequently improved the tumour SO2. The haemodynamic response occurred irrespective of clinical response. A decrease in tumour HHb concentration may reflect processes counteracting elevated interstitial fluid pressure caused by high vessel permeability, low lymphatic drainage, and poor perfusion. Increased tumour SO2 could indicate increased perfusion and reoxygenation. The tumour O2Hb concentration did not decrease after the start of eribulin administration. How could eribulin induce tumour reoxygenation without neutralising circulating VEGF as seen with bevacizumab? One possible answer may lie in the results of biomarker studies of circulating cytokines, which revealed that treatment with either eribulin or bevacizumab significantly decreased plasma concentrations of VEGF and bFGF immediately after the start of drug infusion. Because VEGF and bFGF are both potent angiogenic cytokines, the inhibition of these two major factors indicates that eribulin and bevacizumab have anti-angiogenic properties (Stathopoulos et al, 2010; Meng et al, 2015). However, a decrease in plasma TGF-β1 concentrations was observed in patients treated with eribulin but not bevacizumab. These findings clearly indicate that the mechanism of action of these two agents differs (Figure 5).
Figure 5.
Potential mechanisms of action of eribulin and bevacizumab on vasculature.EMT=epithelial–mesenchymal transition; HHb=deoxyhaemoglobin; MET=mesenchymal-epithelial transition; O2Hb=oxyhaemoglobin; SO2=oxygen saturation.
TGF-β1 plays multiple roles in activating stromal cells in the tumour microenvironment, including ECs, fibroblasts, and immune cells necessary for cancer progression and metastasis (Wendt et al, 2012; Principe et al, 2014). Multiple gene expression analyses have identified gene signatures associated with TGF-β1 signalling that are linked to the acquisition of epithelial–mesenchymal transition (EMT) and stem-cell-like phenotypes exhibited by breast cancer cells (Taylor et al, 2011). Yoshida et al reported that treatment of triple-negative breast cancer cells with eribulin monotherapy significantly upregulated mRNA expression levels of epithelial markers and simultaneously decreased the levels of several mesenchymal markers, leading to inhibition of neo-angiogenesis and the reversal of EMT in a TGF-β1-induced EMT model (Yoshida et al, 2014). Because eribulin stabilises the microvasculature by binding to high-affinity sites on EC microtubules, use of this drug to treat tumours may provide further benefits by affecting stromal cells in the tumour microenvironment (Smith et al, 2010; Dezso et al, 2014).
Conclusion:
Optical imaging technology revealed that eribulin induced tumour reoxygenation after the start of infusion, but bevacizumab showed otherwise. The mechanism of haemodynamic action differs between these two agents. Treatment with eribulin but not bevacizumab leads to remodelling of the microvasculature through suppression of activated stromal cells.
Acknowledgments
We thank Noriko Wakui for her help with the optical measurements of patients and Yukio Ueda for his help in maintenance of the TRS device. This research was supported by Eisai Co., Ltd., JSPS KAKEN grants 25830105 and 26282144, and a 2016 Hidaka research grant.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Shigeto Ueda and Toshiaki Saeki had a research grant from Eisai Co., Ltd. The remaining authors declare no conflict of interest.
References
- Cerussi AE, Tanamai VW, Hsiang D, Butler J, Mehta RS, Tromberg BJ (2011) Diffuse optical spectroscopic imaging correlates with final pathological response in breast cancer neoadjuvant chemotherapy. Philos Trans A Math Phys Eng Sci 369: 4512–4530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dezso Z, Oestreicher J, Weaver A, Santiago S, Agoulnik S, Chow J, Oda Y, Funahashi Y (2014) Gene expression profiling reveals epithelial mesenchymal transition (EMT) genes can selectively differentiate eribulin sensitive breast cancer cells. PLoS One 9: e106131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dybdal-Hargreaves NF, Risinger AL, Mooberry SL (2015) Eribulin mesylate: mechanism of action of a unique microtubule-targeting agent. Clin Cancer Res 21: 2445–2452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etxano J, Insausti LP, Elizalde A, Lopez Vega JM, Plazaola A, Martinez P (2015) Analysis of the changes induced by bevacizumab using a high temporal resolution DCE-MRI as prognostic factors for response to further neoadjuvant chemotherapy. Acta Radiol 56: 1300–1307. [DOI] [PubMed] [Google Scholar]
- Folkman J (1971) Tumor angiogenesis: therapeutic implications. N Engl J Med 285: 1182–1186. [DOI] [PubMed] [Google Scholar]
- Funahashi Y, Okamoto K, Adachi Y, Semba T, Uesugi M, Ozawa Y, Tohyama O, Uehara T, Kimura T, Watanabe H, Asano M, Kawano S, Tizon X, McCracken PJ, Matsui J, Aoshima K, Nomoto K, Oda Y (2014) Eribulin mesylate reduces tumor microenvironment abnormality by vascular remodeling in preclinical human breast cancer models. Cancer Sci 105: 1334–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain RK (2005) Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science 307: 58–62. [DOI] [PubMed] [Google Scholar]
- Keating GM (2014) Bevacizumab: a review of its use in advanced cancer. Drugs 74: 1891–1925. [DOI] [PubMed] [Google Scholar]
- Mehta S, Hughes NP, Buffa FM, Li SP, Adams RF, Adwani A, Taylor NJ, Levitt NC, Padhani AR, Makris A, Harris AL (2011) Assessing early therapeutic response to bevacizumab in primary breast cancer using magnetic resonance imaging and gene expression profiles. J Natl Cancer Inst Monogr 2011: 71–74. [DOI] [PubMed] [Google Scholar]
- Meng X, Vander Ark A, Lee P, Hostetter G, Bhowmick NA, Matrisian LM, Williams BO, Miranti CK, Li X (2015) Myeloid-specific TGF-beta signaling in bone promotes basic-FGF and breast cancer bone metastasis. Oncogene e-pub ahead of print 17 August 2015 doi:10.1038/onc.2015.297. [DOI] [PubMed]
- Miller K, Wang M, Gralow J, Dickler M, Cobleigh M, Perez EA, Shenkier T, Cella D, Davidson NE (2007) Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med 357: 2666–2676. [DOI] [PubMed] [Google Scholar]
- Nakamiya N, Ueda S, Shigekawa T, Takeuchi H, Sano H, Hirokawa E, Shimada H, Suzuki H, Oda M, Osaki A, Saeki T (2014) Clinicopathological and prognostic impact of imaging of breast cancer angiogenesis and hypoxia using diffuse optical spectroscopy. Cancer Sci 105: 833–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Principe DR, Doll JA, Bauer J, Jung B, Munshi HG, Bartholin L, Pasche B, Lee C, Grippo PJ (2014) TGF-beta: duality of function between tumor prevention and carcinogenesis. J Natl Cancer Inst 106: djt369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roblyer D, Ueda S, Cerussi A, Tanamai W, Durkin A, Mehta R, Hsiang D, Butler JA, Mclaren C, Chen WP, Tromberg B (2011) Optical imaging of breast cancer oxyhemoglobin flare correlates with neoadjuvant chemotherapy response one day after starting treatment. Proc Natl Acad Sci USA 108: 14626–14631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JA, Wilson L, Azarenko O, Zhu X, Lewis BM, Littlefield BA, Jordan MA (2010) Eribulin binds at microtubule ends to a single site on tubulin to suppress dynamic instability. Biochemistry 49: 1331–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stathopoulos J, Armakolas A, Stathopoulos GP, Gomatos IP (2010) Plasma VEGF levels in breast cancer patients with and without metastases. Oncol Lett 1: 739–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor MA, Lee YH, Schiemann WP (2011) Role of TGF-beta and the tumor microenvironment during mammary tumorigenesis. Gene Expr 15: 117–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tromberg BJ, Cerussi A, Shah N, Compton M, Durkin A, Hsiang D, Butler J, Mehta R (2005) Imaging in breast cancer: diffuse optics in breast cancer: detecting tumors in pre-menopausal women and monitoring neoadjuvant chemotherapy. Breast Cancer Res 7: 279–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twelves C, Cortes J, Vahdat L, Olivo M, He Y, Kaufman PA, Awada A (2014) Efficacy of eribulin in women with metastatic breast cancer: a pooled analysis of two phase 3 studies. Breast Cancer Res Treat 148: 553–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueda S, Kuji I, Shigekawa T, Takeuchi H, Sano H, Hirokawa E, Shimada H, Suzuki H, Oda M, Osaki A, Saeki T (2014) Optical imaging for monitoring tumor oxygenation response after initiation of single-agent bevacizumab followed by cytotoxic chemotherapy in breast cancer patients. PLoS One 9: e98715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueda S, Nakamiya N, Matsuura K, Shigekawa T, Sano H, Hirokawa E, Shimada H, Suzuki H, Oda M, Yamashita Y, Kishino O, Kuji I, Osaki A, Saeki T (2013) Optical imaging of tumor vascularity associated with proliferation and glucose metabolism in early breast cancer: clinical application of total hemoglobin measurements in the breast. BMC Cancer 13: 514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Veldt AA, Lubberink M, Bahce I, Walraven M, de Boer MP, Greuter HN, Hendrikse NH, Eriksson J, Windhorst AD, Postmus PE, Verheul HM, Serne EH, Lammertsma AA, Smit EF (2012) Rapid decrease in delivery of chemotherapy to tumors after anti-VEGF therapy: implications for scheduling of anti-angiogenic drugs. Cancer Cell 21: 82–91. [DOI] [PubMed] [Google Scholar]
- Wendt MK, Tian M, Schiemann WP (2012) Deconstructing the mechanisms and consequences of TGF-beta-induced EMT during cancer progression. Cell Tissue Res 347: 85–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshida T, Ozawa Y, Kimura T, Sato Y, Kuznetsov G, Xu S, Uesugi M, Agoulnik S, Taylor N, Funahashi Y, Matsui J (2014) Eribulin mesilate suppresses experimental metastasis of breast cancer cells by reversing phenotype from epithelial-mesenchymal transition (EMT) to mesenchymal-epithelial transition (MET) states. Br J Cancer 110: 1497–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]