Abstract
Posterior interosseous nerve entrapment is a potential cause of upper extremity muscle weakness and pain. The diagnosis may be difficult to make clinically, and electrodiagnostic tests may not identify the exact site of nerve compression. We report a case of posterior interosseous nerve entrapment in which electrodiagnostic studies suggested radial neuropathy at the level of the spiral groove, but the sonographic evaluation pinpointed the arcade of Frohse as the level of compression. The patient’s symptoms improved dramatically following surgical release of the nerve. Sonography may be a valuable, non-invasive diagnostic tool in evaluating patients with posterior interosseous nerve entrapment.
Abbreviations: MRI, magnetic resonance imaging; US, ultrasound; PIN, posterior interosseous nerve; ECRB, extensor carpi radialis brevis
Case Report
A 39-year-old woman presented with an inability to move her right wrist and hand, with diffuse numbness and coldness from the right mid forearm into the hand. There was no pain in the right hand, arm or neck. She underwent magnetic resonance imaging (MRI) examinations of the cervical and lumbar spine because of a previous back injury. The cervical spine demonstrated mild degenerative disc disease at the C5-6 level, and the lumbar spine demonstrated no significant stenosis. MRI of the brain showed no evidence of intracranial hemorrhage, parenchymal mass lesion or territorial infarct. No other diagnostic studies were obtained. At this time, clinical findings suggested the diagnosis of a right brachial plexus neuropathy. She was referred to physical therapy and obtained a neutral wrist brace.
In the following months, the patient experienced a decreased use of her right upper extremity including decreased active range of motion of the elbow and digits. A subsequent MRI of the right brachial plexus showed no abnormalities.
She was referred for a neurological consultation five months after her initial presentation. At that time she additionally complained of severe right arm pain. Electrodiagnostic studies showed right radial neuropathy at the level of the spiral groove. Although there was clinical suspicion of right brachial plexus neuropathy, this diagnosis was not demonstrated on the electromyographic or nerve conduction studies. Ultrasound (US) of the right arm was performed with attention to the radial nerve. Findings showed that the radial nerve and proximal posterior interosseous nerve (PIN) were normal, but just proximal to the supinator, the PIN swelled to 2 mm compared with 1 mm on the asymptomatic left side (Fig. 1 A-D).
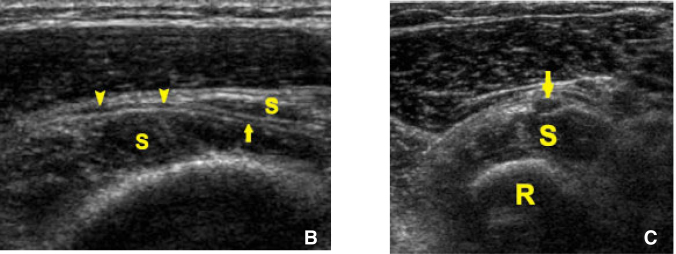
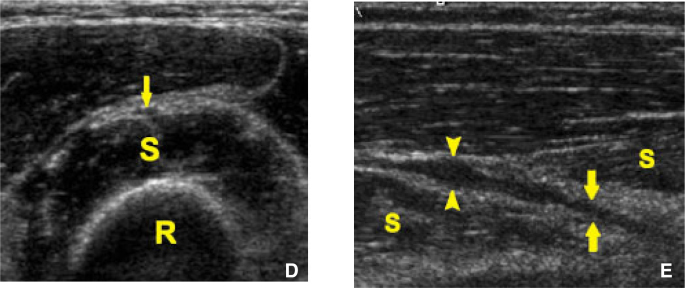
Figure 1.
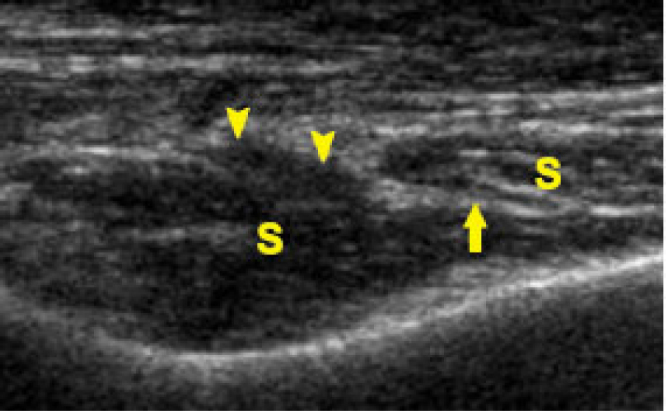
39-year-old woman with right radial neuropathy on electrodiagnostic testing.
A. Longitudinal sonogram of the right posterior interosseous nerve demonstrates fusiform swelling (arrowheads) of the nerve immediately before it pierces the supinator muscle (S). Within the muscle the nerve is almost imperceptible (arrow).
B. Longitudinal sonogram of the left posterior interosseous nerve performed for comparison demonstrates normal caliber of the nerve both proximal to (arrowheads) and within (arrow) the supinator muscle (S).
C. Short axis sonogram of the right posterior interosseous nerve (arrow) just proximal to the supinator muscle (S) demonstrates swelling, with short axis dimension 2mm. R = radius.
D. Short axis sonogram of the left posterior interosseous nerve (arrow) just proximal to the supinator muscle (S) performed for comparison demonstrates normal caliber of the nerve, with short axis dimension 1mm. R = radius. [Powerpoint Slide]
The nerve tapered rapidly after it pierced the supinator muscle. Findings were consistent with radial nerve entrapment at the arcade of Frohse.
Although both the electromyographic and US results were taken into consideration by the surgeon, surgical exploration showed that the lesion was purely at the radial tunnel, indicating that the prior diagnosis of entrapment at the spiral groove was incorrect. After a right lateral epicondylar release with radial nerve neurolysis at the radial tunnel, the patient noted marked improvement, with greatly decreased pain, as well as increased strength and muscle function. Upon physical examination post surgery three months later she was able to forward flex to 170°, internally rotate to 60° and externally rotate 80° compared to forward flexion of 135°, internal rotation of 20° and external rotation of 50° prior to the operation. Follow up electrodiagnostic studies demonstrated only minimal polyphasic units in a right radial distribution. Although follow up US demonstrated persistent swelling of the PIN proximal to the supinator muscle, compared to the preoperative US the nerve was of higher caliber within the supinator itself, consistent with successful radial tunnel release (Fig. 1E).
Figure 1E.
39-year-old woman with right radial neuropathy on electrodiagnostic testing. Longitudinal sonogram of the right posterior interosseous nerve 3 months after surgery demonstrates persistent swelling of the posterior interosseous nerve (arrowheads) proximal to the supinator muscle (S), but the nerve within the supinator (arrows) is of higher caliber than preoperatively, consistent with successful radial tunnel release. [Powerpoint Slide]
Discussion
The PIN is a branch of the radial nerve that consists mainly of motor fibers, in addition to stretch receptors and some sensory fibers [1]. The PIN typically branches off the radial nerve at the radiocapitellar joint, passes under the extensor carpi radialis brevis muscle, above the radiohumeral joint, through the arcade of Frohse (a fibrous band at the level of the proximal supinator muscle), and finally into the supinator muscle [2]. Upon exiting the supinator muscle, the PIN continues to branch and innervates the extensor muscles of the dorsal compartment of the forearm and hand [2].
PIN entrapment syndrome is neuropathy from compression of the nerve. With repetitive overuse, muscle fibers may become fibrous and compress the PIN. The arcade of Frohse is the most common area of compression, but others include the lateral intermuscular septum, the extensor carpi radialis brevis (ECRB) margin and the distal ligamentous margin of the supinator [2]. Symptoms of PIN entrapment include motor weakness in extensors of the wrists or fingers, and either partial or complete paralysis [1]. Clinically, PIN entrapment can mimic lateral epicondylitis and brachial plexopathy, and therefore diagnosis may be difficult [3, 4, 5].
PIN entrapment syndrome can be attributed to numerous causes of compression at any point along the nerve and its branches. The etiology may include systemic diseases, such as diabetes, rheumatoid arthritis, polyarteritis, neuralgic amyotrophy, chronic hypoperfusion, and post-systemic illness angioneuropathy [3]. Other acute causes may result from trauma, viral illness, or certain toxins, such as heavy metals [1]. Mass lesions, such as lipomas and ganglions, can also cause compression [1, 6]. The most common cause, however, can be ascribed to mechanical repetition of flexion-extension and/or pronation-supination [7]. This action is common to athletes, especially tennis players, and others in handicraft work [7].
Symptoms seen with PIN entrapment syndrome vary depending on the location of compression and the type of fibers affected. Compression of the PIN will mostly cause paresis, but may also cause pain due to stretch receptors [1]. Typically, patients present with a painless palsy, where the wrist is extended with radial deviation. The patient will not be able to extend the digits [1].
Another presentation of PIN entrapment is similar to lateral epicondylitis, with tenderness at the radial head and pain at the lateral epicondyle [3, 4, 5]. Maximal tenderness in PIN entrapment is elicited distal to the radial head by palpation through the mobile extensor muscle mass, as opposed to tenderness at the common extensor tendon origin from the lateral epicondyle in true lateral epicondylitis [3, 4, 5]. However, the relative proximity of the radial head and common extensor tendon origin results in possible misdiagnosis [3, 4, 5].
Initial therapy for PIN entrapment syndrome is rest, activity modification, and splinting [6]. However, most cases do progress to surgery for decompression of the nerve to relieve symptoms [6].
The similarity of clinical presentation of PIN syndrome to other upper extremity conditions including lateral epicondylitis, brachial plexopathy and anterior interosseous nerve syndrome makes diagnosis difficult from physical examination alone [1]. There is a definite need for a non-invasive and accurate modality to aid in early diagnosis of PIN entrapment syndrome. Currently, the initial diagnostic test for PIN entrapment syndrome is a nerve conduction study, which demonstrates slowing of conduction and low amplitude through the PIN [6]. However, nerve conduction studies may not always be abnormal in this condition so diagnostic imaging may have a role [6].
Chien, et al. have reported a case of PIN syndrome caused by an contiguous mass, diagnosed with US and MR imaging [6]. Our case report suggests that US may also be a valuable, non-invasive diagnostic tool in evaluating patients with PIN entrapment related to compression at the arcade of Frohse. The major diagnostic criterion is swelling of the nerve proximal to the arcade of Frohse, as has been demonstrated in a previous case series of supinator syndrome [8]. Prospective US studies are needed to establish diagnostic criteria for PIN syndrome based on nerve dimensions.
Footnotes
Published: January 10, 2007
References
- 1.Lubahn JD, Cermak MB. Uncommon nerve compression syndromes of the upper extremity. J Amer Acad Orthop Surg. 1998 Nov-Dec;6(6):378–386. doi: 10.5435/00124635-199811000-00006. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Thomas SJ, Yakin DE, Parry BR, Lubahn JD. The anatomical relationship between the posterior interosseous nerve and the supinator muscle. J Hand Surg [Am] 2000 Sep;25(5):936–941. doi: 10.1053/jhsu.2000.16360. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Umehara F, Yoshino S, Arimura Y, Fukuoka T, Arimura K, Osame M. Posterior interosseous nerve syndrome with hourglass-like fascicular constriction of the nerve. J Neurol Sci. 2003 Nov 15;215:111–113. doi: 10.1016/s0022-510x(03)00164-3. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Ebraheim NA, Jin F, Pulisetti D, Yeasting RA. Quantitative anatomical study of the posterior interosseous nerve. Am J Orthop. 2000 Sep;29(9):702–704. [PubMed] [PubMed] [Google Scholar]
- 5.Fuss FK, Wurzl GH. Radial nerve entrapment at the elbow: surgical anatomy. J Hand Surg [Am] 1991 Jul;16(4):742–747. doi: 10.1016/0363-5023(91)90205-p. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Chien AJ, Jamadar DA, Jacobson JA, Hayes CW, Louis DS. Sonography and MR imaging of posterior interosseous nerve syndrome with surgical correlation. AJR Am J Roentgenol. 2003 Jul;181(1):219–221. doi: 10.2214/ajr.181.1.1810219. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Omura T, Nagano A, Murata H, Takahashi M, Ogihara H, Omura K. Simultaneous anterior and posterior interosseous nerve paralysis with several hourglass-like fasicular constrictions in both nerves. J Hand Surg [Am] 2001 Nov;26(6):1088–1092. doi: 10.1053/jhsu.2001.27766. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Bodner G, Harpf C, Meirer R, Gardetto A, Kovacs P, Gruber H. Ultrasonographic appearance of supinator syndrome. J Ultrasound Med. 2002 Nov;21(11):1289–1293. doi: 10.7863/jum.2002.21.11.1289. [PubMed] [DOI] [PubMed] [Google Scholar]