Introduction
A young adult male pedestrian was struck by a car and sustained a closed complete rupture of both heads of the biceps brachii muscle belly, among other injuries. Rupture of the biceps brachii muscle belly is a rare injury, and complete muscle belly rupture of both long and short heads from direct blunt force trauma has not been reported outside of military parachutists. We describe the findings on magnetic resonance imaging (MRI) of this injury.
Abbreviations: MRI, magnetic resonance imaging; FSE, fast spin echo; STIR, short tau inversion recovery
Case Report
A 22-year-old right-hand dominant male was brought to the emergency room after being hit by an automobile while walking along the side of a road. He was amnesic to the event, unable to recall the mechanism of impact, actions after being struck by the car, or further details, but remembered walking along the side of a road carrying a small piece of luggage in his right hand prior to the accident. During his clinical course, he complained of right upper extremity pain and weakness. Physical examination revealed intact skin over the upper arm, but there was a palpable gap in the anterior soft tissues overlying his right humerus, and weakness in flexion of the elbow.
Based on the suspicion of biceps muscle injury from the findings on the clinical examination, a magnetic resonance imaging (MRI) scan of his right upper extremity was obtained, concentrating on the distal arm region. The MRI demonstrated a complete tear of both heads of the biceps brachii muscle through the mid-portion of the muscle belly (Fig. 1A). There was a 4 cm cleft in the mid-substance of the biceps brachii muscle belly. (Fig 1B) This cleft was filled with high signal material on T2-weighted images, consistent with hematoma and edema. The margins of the cleft were sharply defined and perpendicular to the long axis of the muscle, representing complete tears of the muscle belly through both the long and short heads, with proximal and distal retraction of the stumps. (Fig 1C) There was extensive surrounding high T2 signal in, consistent with edema and hemorrhage. (Fig 1A) The distal biceps brachii tendon was intact at its insertion at the radial tuberosity, and the lacertus fibrosis was also intact. Increased signal was diffusely present in the brachialis muscle belly and in the triceps muscle belly, consistent with muscle contusion, but without gross tear. The patient elected not to undergo surgery and was treated with cast immobilization in a hyperflexed and supinated position for six weeks, followed by physical therapy to restore elbow range of motion and upper arm strength. There were no complications of therapy, and the functional and cosmetic results were considered to be satisfactory.
Figure 1A.
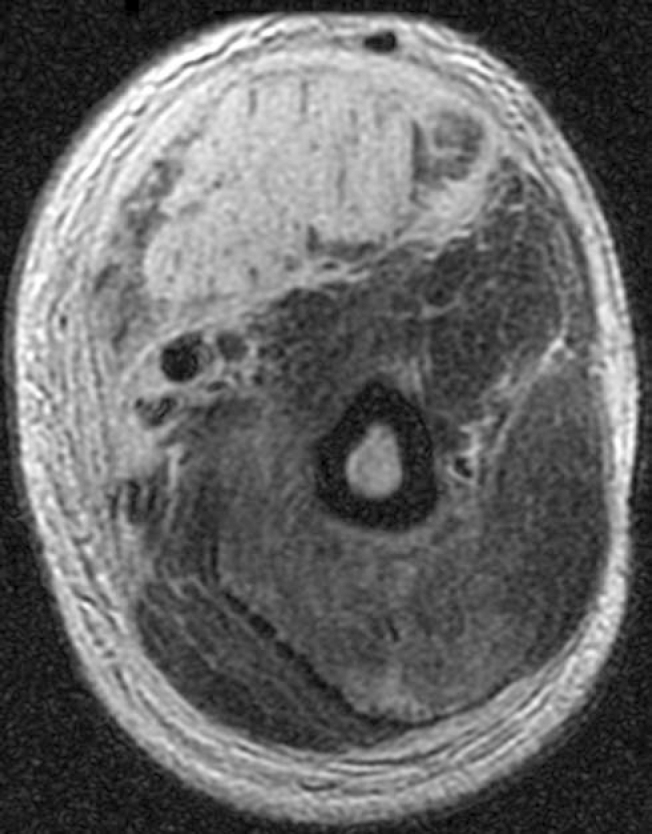
Young adult man with closed biceps muscle injury. Axial T2 FSE with fat suppression MR image through the distal arm shows high signal and discontinuity of muscle fibers in both heads of the biceps brachii muscle. There is extensive edema in the surrounding soft tissues. [Powerpoint Slide]
Figure 1B.
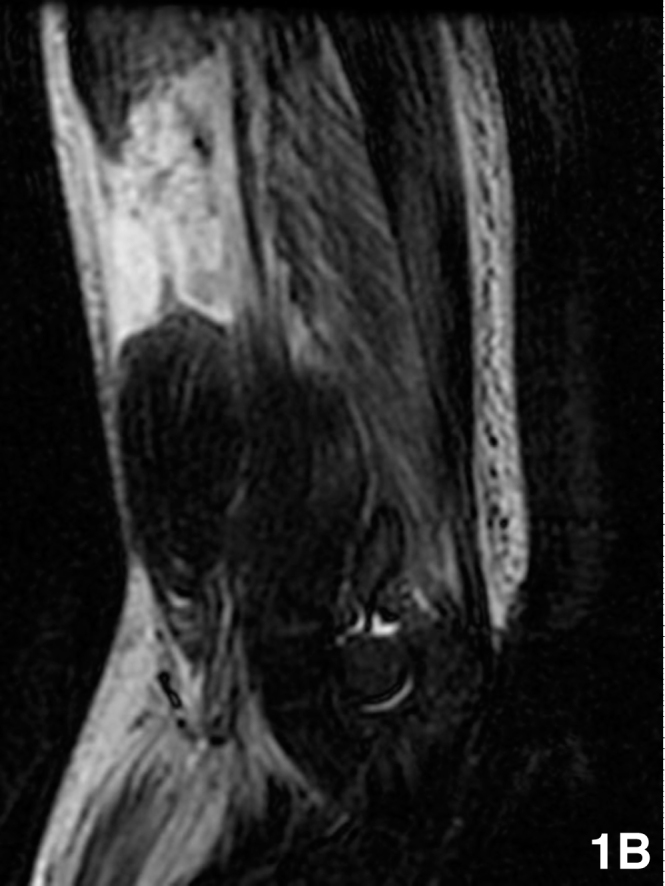
Young adult man with closed biceps muscle injury. Sagittal STIR MR image centered at the distal arm demonstrates high signal cleft in the mid-substance of the biceps brachii muscle. The distal biceps brachii tendon is intact. Increased signal is also present in the brachialis and triceps muscle bellies. [Powerpoint Slide]
Figure 1C.
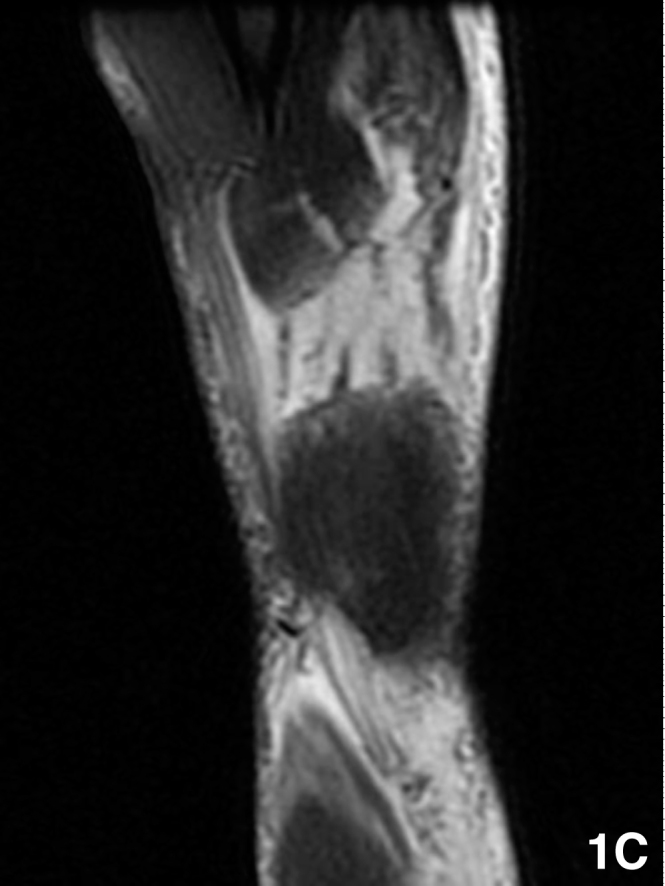
Young adult man with closed biceps muscle injury. Coronal T2 FSE fat suppression MR image centered at the distal arm shows high signal cleft in the mid-substance of the biceps brachii muscle. The sharply defined transverse ruptured ends of the long and short heads of the biceps brachii can be seen proximal to the cleft. [Powerpoint Slide]
Discussion
Rupture of the biceps brachii muscle belly is an exceedingly rare injury. The largest series biceps muscle belly tears have come from Womack Army Medical Center in Fort Bragg, NC. Heckman and Levine (1) reported 20 patients in 1978, and Kragh and Basamania (2) reported 12 patients in 2002. Balkisoon et al. (3) reported the MR features of these injuries in 1998. Fort Bragg is the training base for U.S. Army paratroopers. As described by these authors (1, 2, 3), it is believed that misrouting of the static line underneath the arm during jumping results in simultaneous rupture of both the long and short heads of the biceps muscle belly. The static line is a strong nylon strap that extends from the jumper's parachute pack to the interior of the delivering aircraft, and automatically begins the deployment of the parachute as the jumper falls away, allowing jumps from relatively low height (4). If the static line is wrapped around the upper arm during the jump, after the slack has been taken up, the static line will exert sudden direct blunt force on the substance of the biceps muscle belly, squeezing it in two against the humeral shaft (3). The injury rate requiring emergency care among U.S. military parachutists at Fort Bragg, NC, has been estimated at 8 per 1,000 jumps (5), and there are approximately 25,000 jumps per year (2). Thus, even among this high-risk population, biceps muscle belly ruptures are still relatively uncommon. Civilian parachutists generally use static lines only when learning to skydive or when base jumping; experienced skydivers generally prefer to free-fall. Biceps muscle belly injuries have not been reported in civilian parachutists or others not using a static line. In the sole report of a British military parachutist who sustained closed traumatic rupture of the biceps brachii muscle belly, American equipment and procedures were being used (6).
Outside of military parachutists, biceps muscle belly tears are only reported as individual cases. DiChristina and Lustig (7), and Carmichael et al. (8) both reported isolated tears of the short head biceps muscle belly in water skiers. The mechanism of injury in these two cases was sudden jerking of the flexed elbow into extension by tension on the tow-rope as the boat accelerated away. Moorman et al. (9) reported a water skiing injury with similar mechanism in which both long and short heads were torn through the belly, and the distal portion was catapulted like a sling-shot into the subcutaneous tissues of the forearm, where it was devascularized and became necrotic. Shah and Pruzansky (10) reported an isolated rupture of the short head of the biceps muscle belly in a motor vehicle accident. This injury occurred when the arm of an automobile passenger who had his arm abducted and externally rotated out of the window was struck by the open door of a parked car as he passed by.
In the case we report here, the mechanisms of injury was uncertain because of the patient's amnesia. We hypothesize that the patient may have been struck directly in the right arm by the side mirror of a passing automobile as he walked facing traffic, resulting in blunt force transection of the biceps. The height of the passenger side mirror of a typical automobile would match the upper arm height of a walking adult man of average height. The presence of other direct injuries to the soft tissues of the right arm and the lack of direct impact injuries of the pelvis or lower extremities support this hypothesis.
Biceps muscle belly tears appear to be injuries of young adult males. The age range in Kragh and Basmania's series of paratroopers was 18 to 26 years (2), and the ages in the other reported cases ranged from 15 to 21 years (7, 8, 9, 10). The patient described in this report was 22 years of age. In all of these cases, the subjects were male. Although it is more common for the biceps mechanism to be injured at its distal tendon or its distal insertion on the radial tuberosity than at the muscle belly, these more common distal biceps injuries are still relatively rare (11). The incidence of distal biceps injury among members of a healthcare system population was estimated at 1.2 ruptures per 100,000 patients per year, with almost all of these occurring in males who where 35 years or older (12). In older patients, the tendon is presumably weakened by tendinopathy, so that injuries involve the abnormal tendon rather than the belly. These injuries appear to be the result of indirect loading rather than direct trauma. The mechanisms of distal biceps tendinopathy are thought to be multifactorial (13).
Injury of the proximal portion of the biceps mechanism, the long head of the biceps tendon, is common, and is generally considered to be a component of a diffuse degenerative process related to shoulder impingement (14). Tendinopathy and ruptures of the long head of the biceps tendon represent a very different condition than muscle belly or distal tendon injuries, and is beyond the scope of this writing.
The clinical features of biceps muscle belly rupture mimic those of the more common distal tendon rupture. Symptoms include pain and tenderness, and physical examination findings include a palpable gap along the course of the biceps brachii muscle belly, a palpable mass, ecchymosis, and weakness. There are two heads to the biceps brachii muscle, a long head and a short head. The long head originates from the supraglenoid tuberosity of the scapula, and inserts on the radial tubercle and the fascia of the bicipital aponeurosis. The short head originates on the coracoid process of the scapula and shares the same insertions as the long head. This muscle crosses two joints, the glenohumeral and elbow articulations. The biceps brachii muscle's main roles are elbow flexion (in conjunction with the brachialis and brachioradialis muscles), and forearm supination.
Imaging may not be necessary in cases where complete rupture of the muscle belly or its tendon are strongly suspected and the relevant history, symptomatology, and physical findings are present. However, cross-sectional imaging, particularly MRI or sonography, may help in further elucidating relevant anatomy in ambiguous cases and to evaluate for partial tears. MRI or sonography would also help to distinguish biceps tendon disruption from the radial tuberosity from muscle belly tear. MRI interpretation in biceps abnormalities includes assessment of the distal biceps tendon, course and caliber of the biceps muscle belly, and evaluation of neurovascular structures in the surrounding soft tissues. For biceps brachii tears, abnormal signal can be seen in the muscle belly depending on age of injury with or without hematoma along with discontinuity of the muscle.
Treatment of biceps muscle belly tears includes several possible courses of action. Options include conservative immobilization with sling, to more invasive hematoma evacuation, and ultimately to surgical muscle reattachment. The two studies of the treatment of paratroopers supports the notion of early primary surgical repair (1, 2). Kragh and Basamania (2) found that patients with surgical repairs had better outcomes with regard to patient satisfaction, appearance, and strength. They suggested that if surgery were delayed, softening of the epimysium and muscle fibers might compromise the strength of the repair (2). Other considerations when deciding on treatment include the length of time since the inciting injury, presence or absence of concomitant neurovascular injury, overall condition of the muscle, and the age and activity level of the individual before the injury.
Footnotes
Published: December 28, 2006
References
- 1.Heckman JD, Levine MI. Traumatic closed transaction of the biceps brachii in the military parachutist. J Bone Joint Surg Am. 1978 Apr;60(3):369–372. [PubMed] [PubMed] [Google Scholar]
- 2.Kragh JF, Jr, Basamania CJ. Surgical repair of acute traumatic closed transection of the biceps brachii. J Bone Joint Surg Am. 2002 Jun;84-A(6):992–998. doi: 10.2106/00004623-200206000-00014. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Balkissoon AR, Snyder CF, Basmanian C. MR imaging of traumatic closed injuries of the biceps brachii muscle in military parachutists. AJR Am J Roentgenol. 1998 May;170(5):1400–1401. doi: 10.2214/ajr.170.5.9574630. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Anonymous Static line. http://en.wikipedia.org/wiki/Static_line (Last accessed Oct 30, 2006)
- 5.Craig SC, Morgan J. Parachuting injury surveillance, Fort Bragg, North Carolina, May 1993 to December 1994. Mil Med. 1997 Mar;162(3):162–164. [PubMed] [PubMed] [Google Scholar]
- 6.Bricknell MC. Traumatic rupture of bicepts brachii—a hazard of military parachuting. J R Army Med Corps. 1991 Oct;137(3):144. doi: 10.1136/jramc-137-03-10. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.DiChristina DG, Lustig KA. Rupture through the short head of the biceps muscle belly. Clin Orthop and Rel Res. 1992 Apr;277:139–141. [PubMed] [PubMed] [Google Scholar]
- 8.Carmichael KD, Foster L, Kearney JP. Biceps muscle rupture in a water skier. Orthopedics. 2005 Jan;28(1):35–37. doi: 10.3928/0147-7447-20050101-11. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Moorman CT, Silver SG, Potter HG, Warren RF. Proximal rupture of the biceps brachii with slingshot displacement into the forearm. A case report. J Bone Joint Surg Am. 1996 Nov;78(11):1749–1752. doi: 10.2106/00004623-199611000-00018. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Shah AK, Pruzansky ME. Ruptured biceps brachii short head muscle belly: a case report. J Shoulder Elbow Surg. 2004 Sept-Oct;13(5):562–565. doi: 10.1016/j.jse.2004.02.005. [PubMed] [DOI] [PubMed] [Google Scholar]
- 11.Bernstein AD, Breslow MJ, Jazrawi LM. Distal biceps tendon ruptures: a historical perspective and current concepts. Am J Orthop. 2001 Mar;30(3):193–200. [PubMed] [PubMed] [Google Scholar]
- 12.Safran MR, Graham SM. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002 Nov;(404):275–283. [PubMed] [PubMed] [Google Scholar]
- 13.Seiler J, Parker L, Chamberland P, Sherbourne GM, Carpenter WA. The distal biceps tendon. Two potential mechanisms involved in its rupture: arterial supply and mechanical impingement. J Shoulder Elbow Surg. 1995 May-Jun;4(3):149–156. doi: 10.1016/s1058-2746(05)80044-8. [PubMed] [DOI] [PubMed] [Google Scholar]
- 14.Warren RF. Lesions of the long head of the biceps tendon. Instr Course Lect. 1985;34:204–209. [PubMed] [PubMed] [Google Scholar]


