Abstract
Calciphylaxis is a rare but feared condition thought to related to derangements in calcium and phosphorus metabolism. The syndrome has a predilection for obese women receiving dialysis for chronic renal failure (1, 2). Patients develop painful violaceous lesions in the subcutis, which can lead to ulceration and wound-related sepsis. In severe cases, amputation is required for the gangrenous involved extremity (3).
We present two cases of calciphylaxis with similar clinical presentations and physical findings.
Abbreviations: PTH, parathormone
Case Report
Case 1
A 44-year-old white female with a history of end-stage renal disease on hemodialysis for approximately 24 months, then switched to continuous ambulatory peritoneal dialysis for several months prior to hospital admission for volume depletion. Past medical history also includes obesity, hypertension, anemia, and type II diabetes. Approximately five days prior to admission the patient experienced severe lower extremity pain from long-standing skin lesions (Figure 1).
Figure 1.
Photographs of the lower extremities demonstrate multiple ulcerated lesions with surrounding violaceous changes in the skin. [Powerpoint Slide]
Laboratory tests demonstrated a calcium level of 9.1 mg/dl (normal range 8.5 – 10.0) and phosphorus levels ranging from 3.3 – 4.9 mg/dl (normal range 2.7 – 4.5). Alkaline phosphatase was elevated at 171 (normal range 27 – 100). Serum parathormone (PTH) was normal, measuring 63 IU/L (normal range 15 – 75). The imaging findings (Figure 2) demonstrate confluent areas of minimally increased activity extending up the flanks to the level of the lower thorax. This finding is nonspecific, and could be related soft tissue anasarca. More intense activity is appreciated in the medial thighs, thought to correlate with the patient's skin lesions seen in the following photograph. The radionuclide distribution is slightly less focal as seen in Case 2, however, suggests calciphylaxis accounting for the clinical and physical findings.
Figure 2.
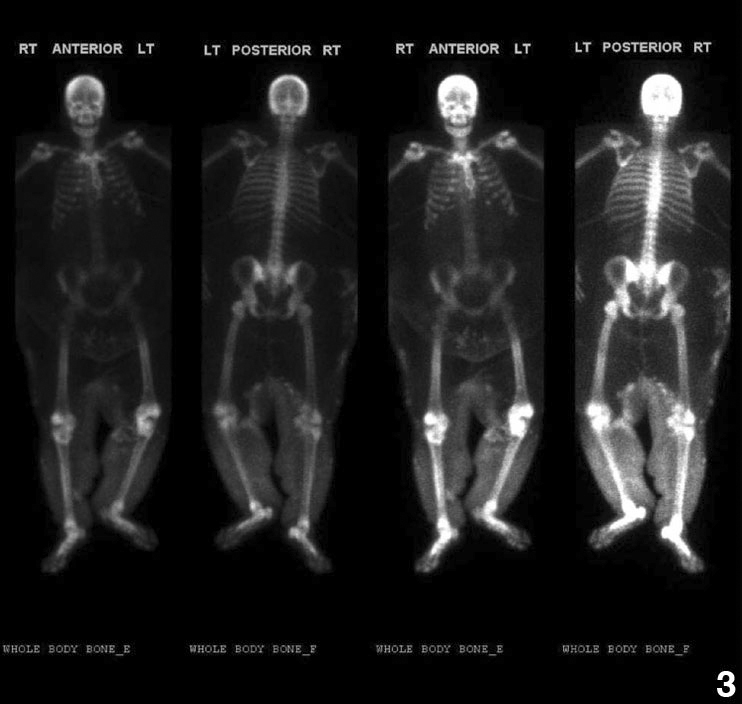
Tc-99m bone scan reveals confluent areas of moderately increased activity predominately around the medial and lateral aspects of the thighs. This radionuclide distribution corresponded to the locations of the patient's cutaneous lesions. Minimal activity is also appreciated extending up the flanks to the level of the lower thorax. Of note on the bone scan is the patient's large body habitus. There are very faint renal outlines without bladder activity related to the underlying renal failure. [Powerpoint Slide]
Case 2
A 54-year-old white female with a history of chronic renal failure requiring hemodialysis for approximately 12 months. Past medical history includes morbid obesity, type II diabetes, left lower extremity deep vein thrombosis, chronic lymphedema, and congestive heart failure. An open wound between abdominal folds in the right lower quadrant was being followed by surgery for approximately two months. Serum calcium was within normal range, measuring 8.3 mg/dl. Serum phosphorus was elevated, measuring 4.5 – 5.3 mg/dl. Serum PTH was normal, measuring 45 IU/L. The imaging findings (Figure 3) demonstrate more focal activity in the lower extremities when compared to Case 1, more typical and specific for calciphylaxis.
Figure 3.
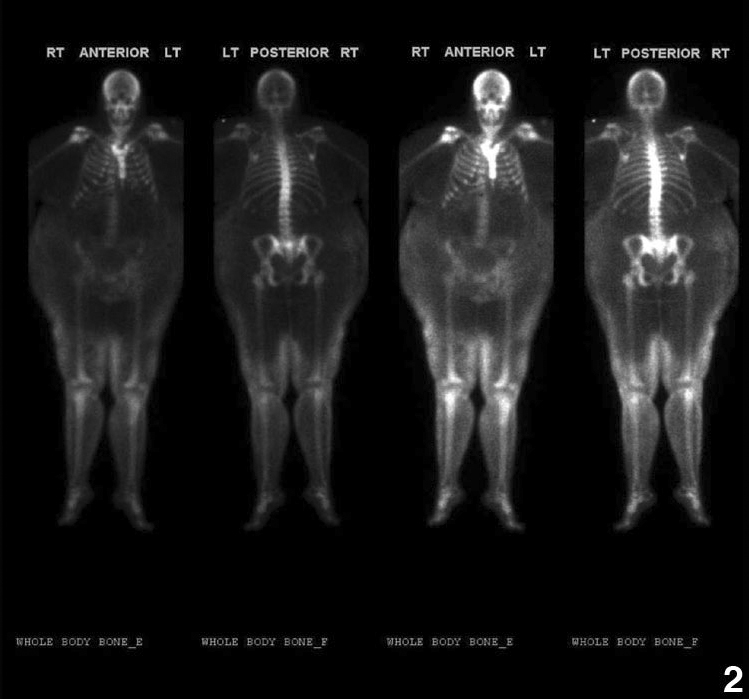
Tc-99m bone scan reveals confluent areas of moderately increased activity predominately around the medial and lateral aspects of the thighs. This radionuclide distribution corresponded to the locations of the patient's cutaneous lesions. Minimal activity is also appreciated extending up the flanks to the level of the lower thorax. Of note on the bone scan is the patient's large body habitus. There are very faint renal outlines without bladder activity related to the underlying renal failure. [Powerpoint Slide]
Discussion
Selye (4) is credited for the early descriptions of calciphylaxis based on experimentation with rat models. Vitamin D or parathormone was administered to achieve hypercalcemia, and then the skin of the rat was injured using varying applications of mechanical force or chemicals. Seyle observed calcification and necrosis in some of the compromised tissue.
Current literature suggests notable differences between the lesions Seyle described and the human counterpart of the syndrome (1). In humans, the syndrome is thought to emanate from elevated serum calcium-x-phosphorus product and elevated parathormone. Calcium salts are deposited in the media of small arteries and arterioles, leading to thrombosis. This process is referred to as the primary lesion of the human syndrome. These and other perfusion related changes lead to skin infarct and necrosis, deemed the secondary lesion of the human syndrome. The histologic changes associated with the primary and secondary lesions of the human syndrome were not initially described by Selye, and are currently felt to extend beyond the umbrella of classically described calciphylaxis. Current literature suggests a new moniker for the human syndrome to more accurately represent the histopathologic entity. Suggestions include subcutaneous calcific arteriolopathy and calcificuremic arteriolopathy.
Treatment for calciphylaxis depends on the severity of the clinical presentation. Local wound care and reduction of calcium intake remain the least invasive modes of therapy. More severe cases have been treated with subtotal parathyroidectomy (3). Recently, reports of treatment with IV sodium thiophosphate have demonstrated significant improvement of the clinical syndrome (5). Anecdotally, Case 1 above was treated with IV sodium thiophosphate and showed marked improvement in pain and appearance of the skin lesions approximately two weeks into treatment.
Imaging
The lesions of calciphylaxis tend to predicate the lower abdominal wall and upper thighs. The calcific deposits in the soft tissues can be seen on Tc 99-m bone scan as mild to moderate increased activity distributed diffusely or focally in the areas of soft tissue involvement. The diagnosis of calciphylaxis is usually clinically apparent. Technetium bone scan can provide supportive information to the clinician and can also be used to monitor therapy (5, 6).
Conclusion
Although radiology and nuclear medicine usually does not play a primary role in calciphylaxis diagnosis, imaging characteristics can compliment the clinical findings. In the appropriate setting, calciphylaxis can be included as one of the handful of conditions that can demonstrate soft tissue uptake on radionuclide bone scan. Radionuclide bone scan may have a role to monitor therapy as suggested by Cicone et al. (5), especially with the promising early data describing success with IV medications like sodium thiophosphate.
Footnotes
Competing interests: The authors have declared that no competing interests exist.
Published: 2007
References
- 1.Janigan American Journal of Kidney Diseases. April, 2000;35(4):588–597. doi: 10.1016/s0272-6386(00)70003-5. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Janigan DT, Prokopetz RD, Chawla S, Durning RG. Massive necrosis of fat and skin as complication of obesity. Can Med Assoc J. 1989;1450:665–668. [PubMed] [PMC free article] [PubMed] [Google Scholar]
- 3.Duh QY, Lim RC, Clark OH. Calciphylaxis in secondary hyperparathyroidism. Diagnosis and parathyroidectomy. Arch Surg. 1991 Oct;126(10):1213–1218. doi: 10.1001/archsurg.1991.01410340055008. [PubMed] discussion 1218-9. [DOI] [PubMed] [Google Scholar]
- 4.Selye H. Calcyphylaxis. University of Chicago Press; Chicago: 1962. [Google Scholar]
- 5.Cicone J. Successful treatment of calciphylaxis with intravenous sodium thiophosphate. American Journal of Kidney Diseases. June, 2004;43(6):1104–1108. doi: 10.1053/j.ajkd.2004.03.018. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Fine A, Zacharias J. Calciphylaxis is usually non-ulcerating: Risk factors, outcomes, and therapy. Kidney Int. 2002;61:2210–2217. doi: 10.1046/j.1523-1755.2002.00375.x. [PubMed] [DOI] [PubMed] [Google Scholar]



