Abstract
Objective
This study addresses whether adverse childhood experiences (ACEs) demonstrate disproportional prevalence across demographic- and health-affecting characteristics, offer significant explanation of adult health outcomes, and show patterned association with illness susceptibility early within and across adulthood when viewed in combination with income and psychosocial resources.
Methods
Data were derived from a population-based state health survey using stratified random sampling of household adults (n=7,470): ages 18–99 (M=55), 59.9% females, and race/ethnicity, income and education levels representative of the region. We assessed ACEs by aggregating 8 adversity forms, 5 health behaviors and 3 psychosocial resources; and health outcomes (number of chronic conditions, subjective wellness).
Results
Disproportionality was evident in ACEs levels by demographics, adult SES, health behaviors, and psychosocial resources in expected directions. Stepped multiple regressions of health outcomes demonstrated significant betas and R2 change for each predictor block, revealing cumulative as well as unique explanatory utility. Early onset chronic illness was evident on the basis of ACEs levels. These illnesses were amplified for low income respondents. Prevalence was highest across adulthood for those also reporting low psychosocial assets.
Conclusions
Findings offer novel insights as to the “long reach” of childhood adversity on health, conditioned by circumstances under which these effects may occur. Health resilience offered by health behaviors and psychosocial resources should shape thinking about preventive and remedial interventions by social work and allied professionals across a range of settings.
Keywords: ACE, adverse childhood experiences, health, weathering, stress, disparities
Introduction
We have long recognized that the strain of living under stressful and inhospitable circumstances has significant health consequences. Inequalities in health have been linked with not only with minority statuses and socioeconomic characteristics that form a health-wealth gradient, but also with increasing awareness of multiple risk exposures including jeopardizing stress loads at the family level.1,2 Running in tandem is the recognition that stressful experiences in childhood, such as maltreatment, loss, poverty, and family disorder, hold significant implications for later life development and health. Elevated exposure to adverse childhood experiences (ACEs), for example, has demonstrated a dose-response relationship—that is, steady decrements in health associated with increases in the number of ACEs—to a host of health problems.3,4
Growing efforts to articulate bridges across these lines of inquiry are illuminating the value of assessing the cumulative and distinctive contribution of early life adversities in addition to social determinant factors that reflect structured social patterning underlying inequalities5,6 The current paper focuses on this juncture, approaching the question of sustained impact of early life adversities on physical health into mature and later adulthood within a broader health factors context. We theorize that elevated ACEs in early life reflect multi-form stress exposure that is likely to be associated with incremental erosion of health as evidenced by earlier and greater susceptibility to illness, poor health through multiple clinical disorders, and a lessened sense of well-being and vitality. Recognizing that early life adversity can affect health through social as well as biological cascades, we argue the value of mutually assessing socioeconomic and early adversity contributions to distinguish both their unique and overlapping effects. As part of a health promotion framework, we also seek to evaluate the contribution of mutable health promotive factors such as optimism and social support toward buffering the effects of early adversity and social disadvantage.
Deepening understanding of etiologies regarding inequalities in stress and adverse environmental exposures and subsequent health outcomes requires integration of insights spanning disciplinary sciences as well as intervening professions.7 Social workers are essential partners in this vein. Social work is inherently an integrative discipline that conceptually locates problems within histories and contexts, embeds its work force in settings within which people live and seek supports, and uses collaborative team models when managing client care. Within this special issue, we argue the value of integrative approaches that consider intersections between individual- and family-level adverse childhood experiences and the social pathways within which cumulative impact on health evolves.8 We will address ways in which social work has special opportunities to interrupt these pathways, acknowledging also the relevance to allied professionals working with populations across the life course.
Theorized Pathways
Converging research across biological, health, and social sciences is revealing mechanisms through which adversities trigger neurobiological disruptions that can become embedded as biological traces within interconnected chains of response and development. Stress embodiment models illustrate pathways through which early life adversities affect later health via burdens placed on biological systems in response to chronic stressors.9,10 Evidence is building that these stress-evoking conditions in the early years of life, induce significant biological changes that modify maturation and disrupt the balance of stress response systems, leading to wear and tear and allostatic overload11,12 and become part of the groundwork for decrements to later well-being.
Early adversity predicts susceptibility to illness, such as the common cold, through processes that are complex, including inequalities in healthy living conditions, increased risk of social difficulties, and neurophysiological dyregulation and damage.13,14 ACEs are theorized to reflect chronic and toxic stressors, indicating social conditions characterized by multiple forms of stress/risk that can negatively affect the developing brain and physiological systems.15,16 ACEs exposure serves to trigger affective reactivity (depression, anxiety, and anger) as well as neurophysiological sensitivity—stimulating dysfunctional coping strategies that may foster risk behaviors and impairments in educational and work force success.
Early life adversities such as maltreatment and significant family dysfunction tend to undermine important psychosocial resources, resulting in lower levels of perceived social support and poorer perceptions of the self.17,18 Within a life course framework, these deficits hold negative implications as mediating influences on positive subsequent development and physical, psychological, and social health outcomes in adulthood.19 Psychosocial resources are also considerations as buffers of health consequences of maltreatment and related early life adversity. Examples of such resources include positive psychological dispositions (e.g., satisfaction) and stress appraisals related to optimism and personal control, and positive coping strategies (e.g., developing and nurturing social supports) and health promotive behaviors.20 When considering adult physical health, potentially buffering factors may include health behaviors and psychosocial resources, such as social support. Factors such as quality sleep and physical activity have long been known to positively affect perceived stress levels and physiological functioning, yielding better physical health outcomes. For example, exercise is currently advocated for children who live in contexts of toxic adversity as a means of minimizing lifetime effects on health21 and sleep education interventions emphasized to offset stress impacts and negative health risk activities.22 Social support and positive outlook are also reliably associated with better physical health and may serve as important buffers of adversity on later health outcomes. In addition to psychological effects, positive appraisals and support yield improved coping and increased likelihood of healthy behaviors, thereby reducing the impact of stress on the body.23,24
In this paper we examine evidence for early life adversities having multiple pathways of contribution to adult physical health, building on theories regarding neurophysiological, socioeconomic, health behavior, and psychosocial mechanisms. We first assess for disproportionality reflected through differential prevalence of ACEs across demographic, SES, health behavior, and psychosocial resource characteristics. We test the hypothesized value of ACEs for both chronic illness and subjective wellness distinguishing their contribution both cumulative with and distinctive from these other health contributors. Finally, we examine the relative presence or absence of buffering resources within a life course framework—testing for interactive relationships between ACEs and income relative to illness susceptibility and the health protective potential of psychosocial resources at three stages of adulthood.
Methods
Sample
Data were obtained from the 2009 Behavioral Risk Factor Surveillance System (BRFSS) for Washington State—a cross-sectional, random-digit-dialed telephone survey conducted by health departments in all 50 states and U.S. protectorates in collaboration with the Centers for Disease Control.* Participants are English and Spanish-speaking adults aged 18 years or older, who are non-institutionalized and live in a household with a working landline telephone. Washington State uses a disproportionate stratified random sampling method with one adult per household randomly selected to participate in the survey.25
The study sample (N = 7,470) consisted of 59.9% females and the following racial/ethnic composition: 87.1% Caucasian, 4.8% Latino/a, 2.6% Asian, 1.5% African American, 1.1% Native American, 0.4% Hawaiian/Pacific Islander, and 2.5% mixed or other race/ethnicity. Average sample age was 55.5 years (SD = 16.1), with approximately 28% age 65 or older and 25% age 44 or younger. Approximately one-third (33.4%) of the sample’s household income was $35,000 or less, and a third (31.4%) was $75,000 or more. Almost 6% of the sample never received a high school diploma, 21.3% had a high school education only, 32.6% attended some college, and 40.5% had a college degree and/or advanced training.
Measures
Demographics consisted of age, gender (0 = male, 1 = female), race/ethnicity (seven categories reported above; Caucasian served as the referent group in the regression analyses), and sexual orientation (0 = heterosexual, 1 = gay/lesbian, 2 = bisexual; heterosexual served as the statistical referent group).
Socioeconomic factors included highest education level completed (4-level categorical scale: not high school graduate, high school graduate, some college, college graduate) and annual household income (8-level categorical scale: $0 to less than $10,000; $10,000 to less than $15,000; $15,000 to less than $20,000; $20,000 to less than $25,000; $25,000 to less than $35,000; $35,000 to less than $50,000; $50,000 to less than $75,000; and $75,000 or more). Health insurance was coded none = 0, private or public insurance = 1. Medical cost barrier was assessed on the basis of needing to see a doctor but not being able to because of cost. This variable was reverse coded (such that 0 = did report this cost barrier; 1 = never reported this barrier) so that all SES factors would be in the same, positive direction to facilitate interpretation.
Total Adverse Childhood Experiences (ACE) score is calculated as the sum of dichotomized “yes” responses across 8 categories of adverse experiences before the age of 18: childhood household mental illness, household substance abuse (alcoholic or drug abuse), incarcerated family member, parental divorce, witnessing domestic violence (slap, hit, kick, punch, beat), physical abuse (parent/adult hit, beat, kick, physically hurt), sexual abuse (sexual touching or forced sex by adult/person 5 or more years older than self), and emotional abuse (parent/adult insult, swear at, put down) (CDC, 2010). In the current sample the range is 0–8, M = 1.58, SD=1.82.
Health behaviors included tobacco use (0 = never smoked; 1 = former or current smoker), CDC calculated variable for heavy alcohol use (heavy alcohol use is defined as men who reported more than 2 drinks per day and women who reported more than 1 drink per day) (0 = no heavy alcohol use; 1 = yes heavy alcohol use), CDC calculated variable for Body Mass Index (0 = neither overweight or obese, BMI less than or equal to 24.9; 1 = overweight, BMI between 25 and 29.9; 2 = obese, BMI over 30), sleep problems (continuous measure assessing how many days in the last month that respondent did not get enough sleep, range 0–30, M = 7.5, SD = 9.7), and CDC calculated variable for physical activity ranging from 0 minutes of activity per day/per week to 50 minutes or more per day of physical activity for 3 or more days per week in the past month (0 = meets recommendations for moderate and/or vigorous physical activity, 1 = does not meet recommendations for physical activity).
A summed psychosocial resource index was created on the basis of three items: socioemotional support assessing how often participants perceive themselves as receiving the emotional and social support they need, assessed on a 5-point Likert scale, how satisfied respondents are with their lives assessed with a four-point Likert scale, and optimism based on a reverse scored assessment of how often participants felt hopeless during the past 30 days assessed on a 5 point scale. Cronbach’s alpha coefficient for this scale is .64 (range = 0–11; M = 9.24; SD = 1.79).
Physical health outcomes included a chronic illness index, calculated as the sum of dichotomized “yes” responses across 9 categories of chronic health diagnoses (M = 1.65, SD = 1.50): high blood pressure, high cholesterol, cancer, diabetes, arthritis, asthma, angina, heart attack, and stroke—the latter three of which were combined for a cardiovascular index for Table 3. Self-assessed wellness is a Likert-type item representing the respondents’ assessment of their overall health (poor = 1 to excellent = 5; M = 3.52, SD = 1.08).
Table 3.
Prevalence of Early Onset of Poor Self-Assessed Health and Chronic Illness (Younger Adults, age 18 to 44) as a Function of ACEs, Income Level and Their Combination
| Self-Reported Health as Poor | Chronically Ill with 3 or more Diseases | Ill with a Particular Type of
Chronic Disease |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Cancer | Arthritis | Asthma | High Choles-terol | Cardio- vascular Disease | Diabetes | High Blood Pressure | |||
| # of ACEs | *** | * | ** | *** | ** | * | * | ||
| 0 | 4.6% | 3.8% | 1.2% | 6.3% | 10.3% | 24.1% | 1.0% | 2.2% | 10.8% |
| 1 | 8.9% | 6.5% | 1.8% | 6.1% | 14.7% | 23.4% | 0.2% | 2.5% | 9.4% |
| 2 | 9.7% | 6.7% | 3.3% | 12.3% | 17.6% | 20.9% | 2.1% | 2.9% | 12.4% |
| 3 or more | 15.2% | 8.8% | 5.0% | 14.6% | 19.9% | 22.4% | 2.1% | 3.0% | 17.2% |
|
| |||||||||
| Income Level a | *** | *** | * | * | * | ||||
| Highest | 3.3% | 3.9% | 4.4% | 9.3% | 16.2% | 21.9% | 1.0% | 1.9% | 11.0% |
| Moderate–High | 7.7% | 4.1% | 1.1% | 11.0% | 15.0% | 23.6% | 1.0% | 2.2% | 15.2% |
| Moderate-Low | 8.7% | 7.7% | 2.6% | 14.2% | 10.4% | 25.4% | 0.9% | 2.8% | 10.1% |
| Lowest | 20.8% | 13.4% | 3.1% | 10.1% | 17.9% | 23.6% | 2.8% | 5.3% | 17.0% |
|
| |||||||||
| Combination of ACEs & Income b | *** | *** | * | *** | * | * | ** | ** | *** |
| Lower ACEs & Moderate/High Income | 3.5% | 4.1% | 2.1% | 8.2% | 12.6% | 24.7% | 0.9% | 1.4% | 9.7% |
| Higher ACEs & Moderate/High Income | 8.9% | 5.7% | 5.6% | 14.9% | 17.8% | 19.6% | 0.8% | 2.5% | 15.2% |
| Lower ACEs & Lowest Income | 15.1% | 8.8% | 1.9% | 5.4% | 13.5% | 17.5% | 1.8% | 5.4% | 12.8% |
| Higher ACEs & Lowest Income | 30.2% | 17.4% | 5.2% | 15.9% | 23.0% | 33.8% | 4.5% | 4.8% | 24.1% |
|
| |||||||||
| Total Sample | 9.8% | 6.5% | 2.9% | 9.9% | 15.5% | 22.9% | 1.4% | 2.7% | 12.8% |
Household Income Level: Highest = $75,000 or more; Moderate High = $50,000 – 74,999; Moderate Low = $35,000–49.999; Lowest Income= Less than $35,000.
Lower ACEs = 0–2 ; Higher ACEs = 3 or more; Statistical Significance:
p≤05;
p≤.01;
p≤.001
Results
Sample ACE Characteristics
Within the overall sample, 37.68% reported no adverse childhood experiences, 23.18% reported 1 ACE, 13.88% reported 2 ACEs, 9.75% reported 3 ACEs, 6.67% reported 4 ACEs, 4.22% reported 5 ACEs, and 4.60% reported 6 or more. Table 1 presents the prevalence of adverse childhood experiences across each of the study covariates, testing whether mean differences achieved significance. Disproportionality was evident in ACEs levels relative to gender sexual minority, and several racial minority statuses (White, Latino/a, and Asian levels were lower than other respondents of color), as well as lower SES indicators, less favorable health behaviors, and lower psychosocial resources. The exception of slightly higher average ACEs associated with greater physical activity may be a function of younger respondents who reported higher ACEs being physically active. Higher ACEs associated with younger respondents may be a function of societal increases in some aspects of adversity assessed (e.g., divorce, parental incarceration, detected parental mental illness) and with attrition of older high-ACE exposed elders through death or health/residential restrictions that precluded participation. In corpus, results demonstrate patterned bivariate associations of ACEs with adult characteristics in theorized directions.
Table 1.
Adverse Childhood Experience Subgroup Score for Each Covariate
| Covariates | Subgroups | Avg. ACEs (sd.) | F test |
|---|---|---|---|
| Age | 18–34 | 2.03 (1.27) | F(3, 6724)=122.20** |
| 35–44 | 1.98 (1.72) | ||
| 45–64 | 1.69 (2.03) | ||
| 65 or older | 0.95 (1.81) | ||
| Gender | Female | 1.84 (2.17) | F(1, 6726)=10.84** |
| Male | 1.61 (1.63) | ||
| Race | Native American | 3.14 (2.26) | F(6, 6668)=7.73** |
| Mixed race | 2.86 (2.15) | ||
| Hawaiian/Pacific Islander | 2.02 (1.77) | ||
| Black | 1.79 (1.75) | ||
| White | 1.71 (1.92) | ||
| Latino | 1.52 (1.52) | ||
| Asian | 1.03 (1.20) | ||
| Sexual Orientation | Bisexual | 3.68 (1.88) | F(2, 6554)=17.24** |
| Homosexual | 2.78 (2.25) | ||
| Heterosexual | 1.69 (1.88) | ||
| Income | Less than $20,000 | 2.34 (2.42) | F(4, 6005)=7.29** |
| $20,000 – $34,999 | 1.93 (2.19) | ||
| $35,000 – $49,999 | 1.63 (1.83) | ||
| $50,000 – $74,999 | 1.61 (1.79) | ||
| $75,000 or more | 1.69 (1.71) | ||
| Education | Less than HS/HS grad | 1.85 (1.93) | F(1, 6721)=4.22* |
| Some college/College grad | 1.68 (1.90) | ||
| Health Insurance | No coverage | 2.13 (1.78) | F(1, 6711)=11.68*** |
| Some coverage | 1.67 (1.91) | ||
| Medical Cost Barrier | Access not limited | 1.60 (1.84) | F(1, 6714)=68.70** |
| Cost-limited access | 2.62 (2.05) | ||
| Smoking | Former/current smoker | 2.16 (2.22) | F(1, 6694)=106.22** |
| Never smoker | 1.43 (1.64) | ||
| Heavy Alcohol | Heavy alcohol use | 2.15 (2.10) | F(1, 6609)=8.87** |
| No heavy alcohol use | 1.70 (1.90) | ||
| BMI | Obese | 2.04 (2.08) | F(2, 6436)=12.45** |
| Overweight | 1.70 (1.93) | ||
| Not overweight | 1.57 (1.74) | ||
| Physical Activity | Meets activity rec’s | 1.81 (1.89) | F(1, 6510)=5.05** |
| Does not meet rec’s | 1.65 (1.93) | ||
| Sleep | Unsatisfactory Sleep | 2.36 (2.00) | F(1, 6653)=107.60** |
| Satisfactory Sleep | 1.49 (1.80) | ||
| Psychosocial resources | Lowest | 2.66 (2.25) | F(1, 6612)=92.79** |
| Highest | 1.58 (1.80) |
p≤.05,
p≤.01,
p≤.001
Regression Analyses
Hierarchical regressions were undertaken with the following order of variable block entry: 1) demographics, 2) ACEs, 3) socioeconomic factors, 4) health behaviors, and 5) psychosocial resource index. This procedure tests cumulative effects as well as the unique explanatory utility of each variable set and the independent relationship of each predictor to the outcome variable controlling for the effects of other covariates in the model. The dependent variable chronic illness index was examined with weighted linear regression techniques using the Stata survey commands. Analysis of self-assessed wellness was undertaken via both linear and ordered logistic regression, with highly comparable results. We report results using ordered logistic regression as a more conservative approach. The inclusion of two related yet distinct features of adult physical health allows assessment of the stability of findings and their interpretation.
At each step, all regression models achieved significance, R2 change was significant and significant effects of ACEs were sustained (see Table 2). The central study premise was supported: early childhood adverse experiences provide unique, significant explanatory value in clinical and subjective indicators of adult physical health, controlling for demographic characteristics and proximal health contributors involving SES and health behaviors. Each additional ACE was associated with reduced odds of positive self-assessed wellness. For example, for each ACE respondents experienced, they had 28% lesser odds of self-assessed wellness (based on .72 odds ratio in comparison to even odds of 1.00 for those without ACEs). When taking into account all the associations with health by the complete set of study variables, each ACE continued to uniquely reduce the odds of positive self-assessed wellness by 10% (based on .90 odds ratio).
Table 2.
Regressions Testing Cumulative and Unique Covariate Contributions to Chronic Illness and Self-Assessed Wellness.
| Chronic Illness Index (βs) Linear Regression | Self-Assessed Wellness (ORs) Ordered Logistic Regression | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Step 1 | Step 2 | Step 3 | Step 4 | Step 5 | Step 1 | Step 2 | Step 3 | Step 4 | Step 5 | |
| F | 170.24 | 175.25 | 141.93 | 123.73 | 117.73 | |||||
| R2Δ | .01*** | .02*** | .05*** | .001* | ||||||
| R2 | .29 | .30 | .33 | .37 | .38 | |||||
|
| ||||||||||
| Age | .53*** | .56*** | .54*** | .52*** | .52*** | .77*** | .72*** | .70*** | .72*** | .71*** |
| Gender | −.00 | −.01 | −.02 | .00 | .00 | 1.04 | 1.07* | 1.10** | 1.04 | 1.03 |
| African Amer. | .03 | .03 | .02 | .02 | .02 | .92** | .93* | .94* | .96 | .95 |
| Asian | −.05*** | −.03** | −.03** | −.01 | −.01 | 1.03 | 1.01 | .99 | .94 | .96 |
| HPI | −.00 | .00 | −.01 | −.02 | −.02 | .93** | .92** | .94*** | .96 | .96 |
| Native | .05* | .04 | .02 | .02 | .02 | .92* | .94 | .99 | .98 | .96 |
| Hispanic | −.02 | −.02 | −.04** | −.05*** | −.05*** | .87** | .86*** | .96 | .97 | .99 |
| Other | .04** | .03* | .02 | .02 | .02 | .89** | .92* | .95 | .96 | .95 |
| Gay/Lesbian | −.00 | −.01 | −.01 | −.01 | −.01 | .97 | .99 | .96 | .98 | .99 |
| Bisexual | .04 | .03 | .01 | .01 | .01 | .90* | .93 | .96 | .97 | .97 |
| ACEs | .12*** | .10*** | .06*** | .06*** | .72*** | .78*** | .85*** | .90* | ||
| Income | −.11*** | −.09*** | −.09*** | 1.45*** | 1.42*** | 1.33*** | ||||
| Education | −.07*** | −.06*** | −.06*** | 1.44*** | 1.40*** | 1.38*** | ||||
| Insurance | .09*** | .08*** | .08*** | .96 | .98 | .98 | ||||
| Med cost | −.04* | −.03 | −.03 | 1.17*** | 1.15*** | 1.11** | ||||
| Smoking | .04** | .04** | .85*** | .86*** | ||||||
| Heavy alcohol | .00 | .00 | .96 | .96 | ||||||
| BMI | .19*** | .19*** | .59*** | .59*** | ||||||
| Poor Physical Activity | .04*** | .04** | .75*** | .77*** | ||||||
| Poor Sleep | .08*** | .07*** | .75*** | .81*** | ||||||
| Psych/Soc Res. | −.03* | 1.52*** | ||||||||
β = standardized betas; OR = odds ratios;
p≤.05,
p≤.01,
p≤.001
Although gender, sexual minority, and racial minority status overall did not demonstrate significant unique contribution, SES factors, particularly income and education, did sustain significant association with both health outcomes in the predicted directions. The odds of positive self-assessed wellness were 1.33 and 1.38 higher for each increment of higher education and higher income, respectively. Medical cost as a barrier to accessing care was unfavorably associated with self-assessed wellness although having health insurance was not. Of the five health behaviors, all but heavy alcohol consumption demonstrated significant relationships in the expected direction controlling for all other predictors; body mass index was the strongest single health behavior contributor to both outcomes.
Psychosocial resources provided significant direct effects to both models—modestly associated with fewer chronic illnesses and robustly associated with better self-assessed health (OR = 1.51, p < .001). Results indicate psychosocial resources may offer a buffering role of ACEs in relation to health, indicated by the reduction of ACE coefficients after stepping in psychosocial resources. SES and health behaviors also appeared to attenuate the negative association of ACEs to higher self-assessed health, with the ACEs coefficient for both chronic illnesses and self-assessed wellness decreasing after that variable block entry.
Interactive Effects: ACEs Combined with Lesser Resources
Two sets of analyses examined the interactive effects of risk factors and ACEs relative to age-graded health outcomes. To capture earlier life onset for respondents age 45 years or younger (average age of 35), Table 3 presents chi-square tests of associations between the health outcome variables in dichotomized form, including the specific illnesses that constitute the chronic illness index, with ACEs, income, and their high/low combinations (low/low, low/high, high/low, high/high). For example, the first block shows the percentages who report poor health conditions who had experienced 0, 1, 2, or 3+ ACEs. A significant graded relationship was evident between number of ACEs relative to subjective (self-assessed) and objective health both in terms of types of chronic diseases as well as being diagnosed with three or more chronic conditions. The “double jeopardy” effects of childhood adversity and adult poverty are reflected in the substantially greater likelihood of those with both high ACEs and low income to report poor self-assessed health and diagnosis of 3 or more chronic diseases relatively early in life. Disproportionality of several chronic conditions (e.g., cancer, arthritis, asthma) as a function of higher ACEs was evident irrespective of current income.
We then integrated psychosocial resources as a potential moderator to the effects of high ACEs and low income on health. Within logistic regression, controlling for age, ACEs, income, and the interaction of ACEs with income, psychosocial resources exhibited significant association with the likelihood of having 3 or more chronic illnesses. Those with higher resources had a significantly lower average prevalence of multiple illnesses in adulthood (OR=.66, p<.001). Figure 1 illustrates these relationships over three adulthood period, wherein mean values for the prevalence of 3 or more chronic illnesses associated with each combination of high/low ACEs, income, and psychosocial resources are plotted. The proportion of respondents with multiple chronic illnesses increases with advanced age, yet with a sustained pattern of greater elevation among those with low income, and more markedly, those with low income and higher ACEs. This trend of lesser odds of multiple chronic illnesses for those with high psychosocial resources was more consistent for low income relative to high income respondents. For example, low income age 18–44 respondents with higher psychosocial resources are more than half as likely as those with lesser psychosocial resources to be diagnosed with 3 or more illnesses (OR = 0.28, p = 0.012) whereas differences in the odds of being as highly ill among higher income younger respondents do not achieve significance (OR = 0.91, p = 0.819).
Figure 1.
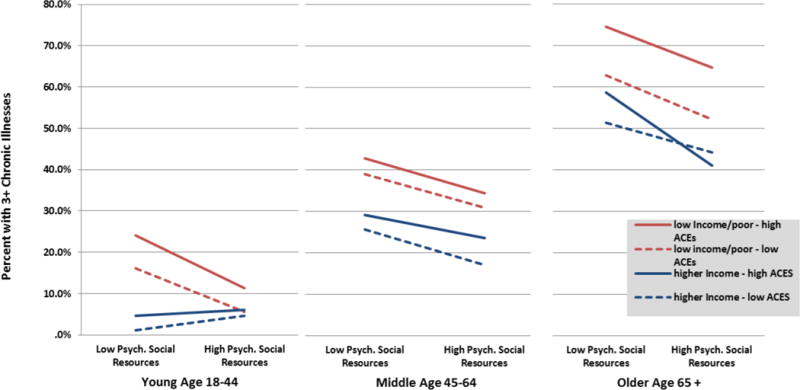
Prevalence of chronic illnesses associated with levels of ACEs, poverty, and psychosocial resources.
Discussion
This study adds to the evolving understanding of long-term detrimental effects of early childhood adverse experiences on health by examining direct and moderating effects of ACEs in conjunction with demographics, socioeconomic disadvantage, health risk behaviors, and psychosocial resources. Through this investigation, we draw upon the stress response model within life course theorizing, considering the interplay between multiple pathways through which early life adversity may manifest health effects. Findings support the value of embedding assessment of adverse childhood experiences within this kind of integrative framework to more fully elucidate disproportionality in early adversity exposures, the role of ACEs within a cumulative disadvantage analysis, and the confluence of strain and diminished resources in chains of disadvantage and health outcomes.
ACEs Disproportionality
A life-course perspective urges attention to ways that variation in strains and resources may be socially patterned, often beginning early in life and accumulating to produce relative advantage or disadvantage in health and related outcomes.26,27 Our findings are consistent with the premise that ACEs function as part of this patterning, arising during developmentally sensitive periods in the life course with the risk of catalyzing chains or linked pathways of disadvantage. Unequal distributions of adverse childhood exposures were significantly associated, for example, with multiple indicators of lower adult socioeconomic status, with higher health risk behaviors, and with lesser psychosocial resources—all of which individually and cumulatively serve to undermine health. Disparities in ACEs are also evident among sexual minorities, women, and several racial/ethnic minority groups. This social patterning mirrors stress proliferation processes wherein primary stressors lead to conditions or events that add to and scaffold the continuing impact of earlier life adversities,28 fostering socioeconomic, behavioral, and psychosocial pathways alongside biological mechanisms of stress reactivity.6,29
ACEs Embedded Within Multiple Pathways to Health
The multivariate regression analyses extend the social patterning findings through a more cumulative disadvantage assessment. As hypothesized, ACEs maintained significant independent direct effects on both chronic illness and self-assessed wellness after accounting for the effects of demographics, adult SES, health behaviors, and psychosocial resources. The attenuation of the beta coefficient of ACEs for chronic conditions and the odds ratio for self-assessed wellness within each regression step suggests partial mediation wherein the variables in that step (e.g., adult SES) serve as partial carriers of ACEs effects to the health outcome.30
These results collectively paint a picture of exacerbating trends. Illness pathways are complex, with ACEs undermining youth health and success in academic achievement, setting the stage for less favorable education and income achievement in adulthood.31 Greater adverse childhood exposure is associated with lower socioeconomic resources in adulthood.32,33 Individuals who rarely seek medical treatment are less likely to receive preventative care or screening, limiting early detection of illness, increasing the odds of becoming more seriously ill and staying sicker longer. Although earlier life socioeconomic conditions are not available for this sample, early and later life poverty are correlated, and poverty is itself a chronic stressor.34 In addition, ACEs have been found to exert effects on health independent of childhood poverty35 and, as seen here, independent of multiple aspects of adult socioeconomic disadvantage.
These processes tend to be mutually reinforcing as well as cumulative. Hobfoll’s36,37 conservation of resources theory highlights erosion of the interlocking array of individuals’ resources (socioeconomic, environmental, social, personal characteristics) as one mechanism through which early or recent life stress negatively impacts later mental and physical health. That is, stressors such as significant family dysfunction and trauma place people on the “resource edge” in many domains by leading to resource loss or preventing resource investment or gain. This can take forms such as reducing educational or employment achievement, constraining access to healthy social ties and lifestyles, limiting physical and leisure activities, and undermining successful experiences that fuel optimism. When high levels of life stress combine with relative depletion of resilience resources, a comparatively greater impact on health outcomes is likely. Thus, although social service interventions that target childhood poverty or adverse experiences should work in concert with one another, efforts to relieve poverty alone will not be sufficient to eliminate health inequalities associated with ACEs either in childhood or in adulthood.
Moderating ACE Effects, Illness Susceptibility, and Service Implications
Although these surveillance data lack diagnostic specificity (e.g., types of cancer, specific age of onset), the patterns in Table 3 parallel prior stress embodiment findings of early life adversity linked via mechanisms such as inflammation to a range diseases such asthma, arthritis, some cancers, cardiovascular disease, high cholesterol, and diabetes.15,38 Focusing on younger adults (under 45, average age of 35) allows insights into illness susceptibility and earlier stages of compromised biological systems that are likely to develop into more numerous and advanced health conditions. Life course stress models specify toxic early life adversity as overactivation of physiological stress responses that lead, in turn, to dysregulations incrementally cascading through multiple neurological and physiological systems, creating health-undermining biological wear and tear.3,39 Table 3 demonstrates hypothesized differential prevalence with more than double the proportion of younger adults with higher ACEs histories having multiple diagnosed conditions and more than three times these adults feeling themselves to be unhealthy compared to those with no ACEs.
These patterns among younger adults point to illness susceptibility at ages before chronic illness is typically a prominent concern either for the individuals themselves or for their health care providers. Yet, these trends indicate that earlier years are indeed important adult life stages for ACEs buffering interventions, particularly given that the predictive effects of ACEs on poor health, if left unremediated, continue to increase in middle to later adulthood.40 The disproportionality of greater ACEs exposure and ill health was most striking for those who also reported low incomes, wherein a quarter of those younger adults already had three or more chronic conditions and nearly a third assessed themselves as unwell.
These trends underscore the importance of safety net services across multiple fields of practice for social workers and other providers. This includes proactive outreach, screening, and education with younger, particularly lower income, adults for whom current stress may exacerbate ACE-related health risks, yet be sufficiently early such that significant illness remediation and prevention can be achieved.41 ACEs have been linked to greater emergency room use,42 which, combined with economic barriers to general health services, suggests inadequate receipt of preventive and early medical interventions. Implementation of the Affordable Care Act offers new opportunities for patient outreach, system navigation, preventive services, and care coordination. Social workers and allied professionals that bring a life course and person-in-environment understanding of relationships between health and factors such as developmental history, education, employment, and involvement in other systems will be crucial to shaping medical and social services attentive to the nuanced roles of ACEs in health.43
ACEs and Psychosocial Resources as Service Targets
The fact that adults with higher ACEs reported substantially lower psychosocial resources documents a kind of multiple jeopardy of elevated risks and lesser resilience assets. Illustrated through low income and lower psychosocial resources in the aftermath of higher childhood adversity, this convergence of life course factors is part of the trajectory of health erosion that leads to weathering and accelerated aging.46, 47 Yet, psychosocial resources indexed here capture dimensions of support, satisfaction, and optimism that are broadly associated with psychological health and resilience, enhancing subjective health perceptions, even in spite of declining vigor or major health issues.44,45 Emotional supports and positive expectancies serve to attenuate individuals’ perceptions of stressful conditions.
That said, the relatively conservative regression test of psychosocial resources as health-promotive factors in the current study, controlling for other factors with which these commonly co-vary, is very heartening. Each increment of psychosocial resources was associated with more than a 50% greater likelihood of high levels of perceived wellness. Although current psychosocial resources were comparatively less strongly associated with number of chronic illnesses that have taken years to develop, the direct sample effect was significant. Moreover, benefits of higher psychosocial resources are evident in younger adulthood where these supports are more proximal to slowly developing health conditions, indicating their value toward prevention.
Review of interventions fostering positive social supports, emotion regulation, and cognitive self-perceptions shows promise for changes in physiology and neuroplasticity involved in modulating stress and augmenting health in the aftermath of early adversity.48 These characteristics, in turn, can help to sustain engagement in healthier habits and effective self-management activities that are critical to slowing progression of chronic conditions. Childhood adversity thus appears to be an influential life course factor to assess in services to support the management and promotion of health across the life course, particularly in vulnerable populations.
Social workers embedded within a range of family, youth, health, community, and welfare services have important roles to play in preventive and resilience-promotive interventions. Such interventions range in target areas and may include family environment and parenting skills with vulnerable and “risky” families, stress management, social support improvement, and cognitive behavioral and coping interventions to strengthen factors such as emotion regulation, mindfulness and relaxation skills, positive reappraisal, hopefulness, and coping effectiveness.49–51 Evidence that individuals sensitized to stress by adverse early environments may be most likely to be helped by such interventions argues for ACEs screening and targeted interventions,52 including repair of regulatory systems and building physiological plasticity.53
Health Risk Behaviors: Implications for Intervention
Rather than being randomly distributed, health habits tend to cluster, with some individuals exhibiting multiple risk behaviors,54 evident here among respondents with higher ACEs exposure. Heightened reactivity in response to stress and neurophysiological dysregulations such as metabolic processes may lead individuals to engage in coping and arousal-reduction behaviors that carry longer-term health-compromising outcomes.55 Behaviors such as smoking, drinking, and diets high in sugar and fats provide short-term ameliorative effects on anxiety and distress.41,56 These health behaviors tend to promote inflammation, already elevated from early life adversity, and thus may act synergistically to trigger greater inflammation than either individually.57
These behaviors become interwoven with physiological processes involved in frequently activated stress responses that can create tenacious relationships in stress-accelerated biological aging.58 Obesity, for example, involves complex processes related to stress, eating responses, limited activity patterns, dysregulations in stress-sensitive metabolic systems, and temporary coping benefits of high calorie foods.59 Impaired sleep may gradually alter brain and neuroendocrine systems, compounding dysregulations among ACEs-affected individuals and elevating risk of a range of health disorders,60 a variety of health-adverse behaviors, and difficulties in work and school settings.61,62
However, all health behaviors, with the exception of heavy alcohol consumption, demonstrated positive independent associations to both health outcomes. Although heavy alcohol use is associated with higher ACEs in both the current and other studies,63,64 findings in general populations are inconclusive regarding its explanatory value when controlling for other health factors65, as evident here. These findings encourage attention to health behaviors aimed toward interrupting partial conduits of ACEs effects on later health and as malleable targets at early points in the lifespan. In addition to advantages from cessation, positive health behaviors such as activity, sleep, and healthy eating hold potential as both biological and psychological buffers of stress effects. Exercise, for example, conveys psychological and physical benefits reducing elevated inflammation associated with early life stress.66
Social work change strategies that integrate psychosocial resources and health behaviors are, for those with greater early life adversity, likely to work in tandem with behavioral and biological systems, more sustainably replacing maladaptive coping strategies with ones that better support health and wellness. Emergent theorizing such as “shift-and-persist” strategies illustrate this kind of integration.67 Based on psychobiological mechanisms, this approach balances shifting (adjusting to one’s stressors through cognitive and affective skills such as positive reappraisals and emotion regulation) as well as persisting (maintaining focused optimism and efforts directed to the future). Shift-and-persist strategies have been found to mitigate sympathetic-nervous-system and hypothalamic-pituitary-adrenocortical responding to the disproportionately high stress exposures experienced by low SES individuals, to forestall pathogenic sequelae of stress, and to be associated with better physical health children and adults.67,68 Findings that these benefits did not accrue to high SES individuals suggests, consistent with our findings, that low SES conveys importantly distinct stressors and resource limitations that intersect with ACEs but may require different types of interventions.
Limitations
Our findings are based on cross-sectional data including retrospective survey of ACEs. Considerable testing of retrospective measures of ACEs has indicated adequate variance, stability of linear trends between retrospectively assessed adversity and subsequent outcomes, and weak to no evidence of current mood state effects on reporting.69,70 Findings of underreporting of actual occurrence of ACEs may serve to attenuate linear associations, such that effects may be stronger than are evident. Although causal interpretation must be tempered, our outcomes are consistent with studies that have used longitudinal designs as well as biological data associated with early life stress.
Washington state’s racial/ethnic minority population is proportionally smaller (approximately 28%71) but more culturally diverse than some other states. Although this racial composition limits analysis with specific communities of color such as black/white comparisons, more diffuse diversity is a growing reality for many U.S. cities and states. Although social disadvantage such as truncated education and lower income constitute one set of pathways through which racial minority groups are at risk of poorer health, weathering effects of discrimination is another critical contributor that available data do not allow direct assessment of. The inclusion of socioeconomic assets, care access, and health behaviors as well as ACEs data, however, helps to disentangle effects on current health within a population based sample, with greater generalizability relative to nonprobability samples.
Conclusion and Future Directions
Primary prevention and early detection of adverse childhood experiences are priorities for immediate child and family well-being,72 but also hold urgency for the lives, productivity, and health of next generations. Findings here regarding socioeconomic assets, health behaviors, and psychosocial resources each point to mutable factors that play a part in offsetting early childhood adversity and preventing or decreasing risks to later health. Moreover, detection of direct, mediated, and moderated effects of adverse childhood experience effects argues for integrated research and service response approaches that capture multiple pathways through which adversity accumulates across the life course.
The current findings indicate promise for potentially lifelong health promotion among those with ACEs histories, supporting the need for low-barrier, integrated health care attentive to stress embodiment and stress proliferation trajectories that are often compounded by social disadvantage.28 Prevention of early life toxic stress continues to be the most important implication of ACEs studies, an area familiar to social workers and other providers who have long advocated for the protection of children and support for vulnerable families. Findings from this and other studies that investigate the links between ACEs and health outcomes for adults urge intervention in young adulthood through later life as a second priority.
In addition to targeting specific illnesses, health care attentive to life-course stress embodiment opens doors to targeting intermediate carriers of adversity impacts, augmenting health, wellness, and quality of life. Care provision that blends or coordinates physical and mental health services, such as interventions targeting healthy behaviors (including exercise, smoking cessation, and nutrition) as well as social support, community connections, and health care access is consistent with collaborative care models targeting comorbidities such as diabetes, cardiovascular disease, and depression.73 Curbing inequalities in exposure to and health effects of early life adversity will require contributions from many specialties. However, social workers’ ecological, life course perspective, attention to social inequalities, and placement in wide-ranging service domains equip them to be practical and innovative team contributors.
Acknowledgments
This research was supported in part by a grant from the National Institute on Mental Health grant 5 T32 MH20010 “Mental Health Prevention Research Training Program.”
Footnotes
Centers for Disease Control and Prevention [Internet]. BRFSS: Turning information into health. 2011 [cited 2011 June 11]. Available from: http://www.cdc.gov/BRFSS/index.htm
Contributor Information
Paula S. Nurius, University of Washington.
Sara Green, University of Washington.
Patricia Logan-Greene, University at Buffalo.
Dario Longhi, Participatory Research Consulting.
Chiho Song, University of Washington.
References
- 1.Evans GW, Kim P. Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status-health gradient. Ann N Y Acad Seci. 2010 Feb;1186:174–189. doi: 10.1111/j.1749-6632.2009.05336.x. [DOI] [PubMed] [Google Scholar]
- 2.Repetti RL, Robles TF, Reynolds B. Allostatic processes in the family. Dev Psychopathol. 2011 Aug;23(3):921–938. doi: 10.1017/S095457941100040X. [DOI] [PubMed] [Google Scholar]
- 3.Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. EUR ARCH PSY CLIN N. 2006 Apr;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998 May;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 5.Nurius PS, Logan-Greene P, Green S. Adverse childhood experiences (ACE) within a social disadvantage framework: distinguishing unique, cumulative, and moderated contributions to adult mental health. J Prev Interv Community. 2012;40(4):278–290. doi: 10.1080/10852352.2012.707443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Umberson D, Williams K, Thomas PA, Liu H, Thomeer MB. Race, gender, and chains of disadvantage: childhood adversity, social relationships, and health. J Health Soc Behav. 2014;55(1):20–38. doi: 10.1177/0022146514521426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gehlert S, Murray A, Sohmer D, McClintock M, Conzen S, Olopade O. The importance of transdisciplinary collaborations for understanding and resolving health disparities. Soc Work Public Health. 2010 May;25(3):408–422. doi: 10.1080/19371910903241124. [DOI] [PubMed] [Google Scholar]
- 8.Davidson G, Devaney J, Spratt T. The Impact of Adversity in Childhood on Outcomes in Adulthood Research Lessons and Limitations. J Soc Work. 2010 Oct;10(4):369–390. [Google Scholar]
- 9.Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev [Review] 2010 Sep;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 10.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med [Review] 1998 Jan 15;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 11.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012 Apr 12;106(1):29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 12.National Scientific Council on the Developing Child. Excessive Stress Disrupts the Architecture of the Developing Brain: Working Paper 3 [Internet] 2005/2014 [cited 2014, March 12]; Updated Edition. Available from: http://developingchild.harvard.edu/
- 13.Cohen S, Doyle WJ, Turner RB, Alper CM, Skoner DP. Childhood socioeconomic status and host resistance to infectious illness in adulthood. Psychosom Med. 2004 Jul-Aug;66(4):553–558. doi: 10.1097/01.psy.0000126200.05189.d3. [DOI] [PubMed] [Google Scholar]
- 14.Cohen S, Janicki-Deverts D, Chen E, Matthews KA. Childhood socioeconomic status and adult health. Ann N Y Acad Sci. 2010 Feb;1186:37–55. doi: 10.1111/j.1749-6632.2009.05334.x. [DOI] [PubMed] [Google Scholar]
- 15.Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011 Nov;137(6):959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP. Developmental neurobiology of childhood stress and trauma. Psychiatr Clin North Am. 2002 Jun;25(2):397–426. vii–viii. doi: 10.1016/s0193-953x(01)00003-x. [DOI] [PubMed] [Google Scholar]
- 17.Turner HA, Butler MJ. Direct and indirect effects of childhood adversity on depressive symptoms in young adults. Journal of Youth and Adolescence. 2003 Apr;32(2):89–103. [Google Scholar]
- 18.Vranceanu AM, Hobfoll SE, Johnson RJ. Child multi-type maltreatment and associated depression and PTSD symptoms: The role of social support and stress. Child Abuse & Neglect. 2007 Jan;31(1):71–84. doi: 10.1016/j.chiabu.2006.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matthews KA, Gallo LC, Taylor SE. Are psychosocial factors mediators of socioeconomic status and health connections? A progress report and blueprint for the future. Ann N Y Acad Sci [Review] 2010 Feb;1186:146–173. doi: 10.1111/j.1749-6632.2009.05332.x. [DOI] [PubMed] [Google Scholar]
- 20.Hill TD, Kaplan LM, French MT, Johnson RJ. Victimization in early life and mental health in adulthood: an examination of the mediating and moderating influences of psychosocial resources. J Health Soc Behav. 2010 Mar;51(1):48–63. doi: 10.1177/0022146509361194. [DOI] [PubMed] [Google Scholar]
- 21.Garner AS, Shonkoff JP. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012 Jan;129(1):e224–231. doi: 10.1542/peds.2011-2662. [DOI] [PubMed] [Google Scholar]
- 22.Blunden SL, Chapman J, Rigney GA. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep Med Rev [Review] 2012 Aug;16(4):355–370. doi: 10.1016/j.smrv.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 23.Taylor SE, Kemeny ME, Reed GM, Bower JE, Gruenewald TL. Psychological resources, positive illusions, and health. Am Psychol. 2000 Jan;55(1):99–109. doi: 10.1037//0003-066x.55.1.99. [DOI] [PubMed] [Google Scholar]
- 24.Uchino BN. Understanding the Links Between Social Support and Physical Health: A Life-Span Perspective With Emphasis on the Separability of Perceived and Received Support. Perspectives on Psychological Science. 2009 May;4(3):236–255. doi: 10.1111/j.1745-6924.2009.01122.x. [DOI] [PubMed] [Google Scholar]
- 25.WA Department of Health [Internet] Center for Health Statistics: What is BRFSS? 2010 [cited 2011 June 11]. Available from: http://www.doh.wa.gov/ehsphl/chs/chs-data/brfss/brfss_keypoints.htm.
- 26.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol [Editorial] 2002 Apr;31(2):285–293. [PubMed] [Google Scholar]
- 27.Ferraro KF, Shippee TP. Aging and cumulative inequality: how does inequality get under the skin? Gerontologist. 2009 Jun;49(3):333–343. doi: 10.1093/geront/gnp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pearlin LI, Schieman S, Fazio EM, Meersman SC. Stress, health, and the life course: some conceptual perspectives. J Health Soc Behav. 2005 Jun;46(2):205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- 29.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. 2009 Jun 3;301(21):2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 30.Mirowsky J. Analying associations between mental health and social circumstances. In: Aneshensel CS, Phelan JC, Bierman A, editors. Handbook of the sociology of mental helath. 2. NY: Springer; 2013. [Google Scholar]
- 31.Macmillan R, Hagan J. Violence in the transition to adulthood: Adolescent victimization, education, and socioeconomic attainment in later life. Journal of Research on Adolescence. 2004;14(2):127–158. [Google Scholar]
- 32.Sansone RA, Leung JS, Wiederman MW. Five forms of childhood trauma: Relationships with employment in adulthood. Child Abuse Negl. 2012 Sep;36(9):676–679. doi: 10.1016/j.chiabu.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 33.Zielinski DS. Child maltreatment and adult socioeconomic well-being. Child Abuse Negl. 2009 Oct;33(10):666–678. doi: 10.1016/j.chiabu.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 34.Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. J Health Soc Behav. 2006 Mar;47(1):17–31. doi: 10.1177/002214650604700102. [DOI] [PubMed] [Google Scholar]
- 35.Danese A, Moffitt TE, Harrington H, Milne BJ, Polanczyk G, Pariante CM, et al. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med. 2009 Dec;163(12):1135–1143. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hobfoll SE. The influence of culture, community, and the nested-self in the stress process: Advancing Conservation of Resources theory. Applied Psychology. 2001 Jul;50(3):337–421. [Google Scholar]
- 37.Hobfoll SE, Schumm JA. Conservation of resources theory: Application to public health promotion. 2009 [Google Scholar]
- 38.Kiecolt-Glaser JK, Gouin JP, Weng NP, Malarkey WB, Beversdorf DQ, Glaser R. Childhood adversity heightens the impact of later-life caregiving stress on telomere length and inflammation. Psychosom Med. 2011 Jan;73(1):16–22. doi: 10.1097/PSY.0b013e31820573b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006 May;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Logan-Greene P, Green S, Nurius PS, Longhi D. Distinctive contributions of adverse childhood experiences and resilience resources: A cohort analysis of adult physical and mental health. Social Work in Health Care. doi: 10.1080/00981389.2014.944251. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Larkin H, Felitti VJ, Anda RF. Social work and adverse childhood experiences research: implications for practice and health policy. Soc Work Public Health. 2014 Jan 2;29(1):1–16. doi: 10.1080/19371918.2011.619433. [DOI] [PubMed] [Google Scholar]
- 42.Chartier MJ, Walker JR, Naimark B. Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse Negl. 2010 Jun;34(6):454–464. doi: 10.1016/j.chiabu.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 43.Andrews CM, Darnell JS, McBride TD, Gehlert S. Social work and implementation of the Affordable Care Act. Health Soc Work [Editorial] 2013 May;38(2):67–71. doi: 10.1093/hsw/hlt002. [DOI] [PubMed] [Google Scholar]
- 44.Mulkana SS, Hailey BJ. The role of optimism in health-enhancing behavior. Am J Health Behav. 2001 Jul-Aug;25(4):388–395. doi: 10.5993/ajhb.25.4.4. [DOI] [PubMed] [Google Scholar]
- 45.Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S. Dispositional optimism and health behaviour in community-dwelling older people: associations with healthy ageing. Br J Health Psychol. 2006 Feb;11(Pt 1):71–84. doi: 10.1348/135910705X42850. [DOI] [PubMed] [Google Scholar]
- 46.Tyrka AR, Price LH, Kao HT, Porton B, Marsella SA, Carpenter LL. Childhood maltreatment and telomere shortening: preliminary support for an effect of early stress on cellular aging. Biol Psychiatry. 2010 Mar 15;67(6):531–534. doi: 10.1016/j.biopsych.2009.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.O’Rand AM, Hamil-Luker J. Processes of cumulative adversity: childhood disadvantage and increased risk of heart attack across the life course. J Gerontol B Psychol Sci Soc Sci. 2005 Oct;60(Spec No 2):117–124. doi: 10.1093/geronb/60.special_issue_2.s117. [DOI] [PubMed] [Google Scholar]
- 48.Davidson RJ, McEwen BS. Social influences on neuroplasticity: stress and interventions to promote well-being. Nature neuroscience. 2012 May;15(5):689–695. doi: 10.1038/nn.3093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Repetti RL, Taylor SE, Seeman TE. Risky families: family social environments and the mental and physical health of offspring. Psychol Bull. 2002 Mar;128(2):330–366. [PubMed] [Google Scholar]
- 50.Shonkoff JP. Leveraging the biology of adversity to address the roots of disparities in health and development. Proc Natl Acad Sci U S A [Addresses] 2012 Oct 16;109(Suppl 2):17302–17307. doi: 10.1073/pnas.1121259109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Taylor SE, Way BM, Seeman TE. Early adversity and adult health outcomes. Dev Psychopathol. 2011 Aug;23(3):939–954. doi: 10.1017/S0954579411000411. [DOI] [PubMed] [Google Scholar]
- 52.Way BM, Taylor SE. Social influences on health: is serotonin a critical mediator? Psychosom Med. 2010 Feb;72(2):107–112. doi: 10.1097/PSY.0b013e3181ce6a7d. [DOI] [PubMed] [Google Scholar]
- 53.Slopen N, McLaughlin KA, Shonkoff JP. Interventions to improve cortisol regulation in children: a systematic review. Pediatrics. 2014 Feb;133(2):312–326. doi: 10.1542/peds.2013-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pruchno R, Wilson-Genderson M. Adherence to clusters of health behaviors and successful aging. J Aging Health [Research Support, Non-U.S. Gov’t] 2012 Dec;24(8):1279–1297. doi: 10.1177/0898264312457412. [DOI] [PubMed] [Google Scholar]
- 55.Umberson D, Liu H, Reczek C. Stress and health behaviors. In: Turner HA, Schieman S, editors. Advances in life course research: Stress processes across the life course. NY: Elsevier; 2008. [Google Scholar]
- 56.Ford JD, Wasser T, Connor DF. Identifying and determining the symptom severity associated with polyvictimization among psychiatrically impaired children in the outpatient setting. Child Maltreat. 2011 Aug;16(3):216–226. doi: 10.1177/1077559511406109. [DOI] [PubMed] [Google Scholar]
- 57.Kiecolt-Glaser JK. Stress, food, and inflammation: psychoneuroimmunology and nutrition at the cutting edge. Psychosom Med. 2010 May;72(4):365–369. doi: 10.1097/PSY.0b013e3181dbf489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Geronimus AT, Hicken MT, Pearson JA, Seashols SJ, Brown KL, Cruz TD. Do US Black Women Experience Stress-Related Accelerated Biological Aging?: A Novel Theory and First Population-Based Test of Black-White Differences in Telomere Length. Hum Nat. 2010 Mar 10;21(1):19–38. doi: 10.1007/s12110-010-9078-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dallman MF, Pecoraro N, Akana SF, La Fleur SE, Gomez F, Houshyar H, et al. Chronic stress and obesity: a new view of “comfort food”. Proc Natl Acad Sci U S A. 2003 Sep 30;100(20):11696–11701. doi: 10.1073/pnas.1934666100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meerlo P, Sgoifo A, Suchecki D. Restricted and disrupted sleep: effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Med Rev. 2008 Jun;12(3):197–210. doi: 10.1016/j.smrv.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 61.Bader K, Schafer V, Schenkel M, Nissen L, Schwander J. Adverse childhood experiences associated with sleep in primary insomnia. J Sleep Res. 2007 Sep;16(3):285–296. doi: 10.1111/j.1365-2869.2007.00608.x. [DOI] [PubMed] [Google Scholar]
- 62.Chapman DP, Wheaton AG, Anda RF, Croft JB, Edwards VJ, Liu Y, et al. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. 2011 Sep;12(8):773–779. doi: 10.1016/j.sleep.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 63.Dong M, Dube SR, Felitti VJ, Giles WH, Anda RF. Adverse childhood experiences and self-reported liver disease: new insights into the causal pathway. Arch Intern Med. 2003 Sep 8;163(16):1949–1956. doi: 10.1001/archinte.163.16.1949. [DOI] [PubMed] [Google Scholar]
- 64.Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addict Behav. 2002 Sep-Oct;27(5):713–725. doi: 10.1016/s0306-4603(01)00204-0. [DOI] [PubMed] [Google Scholar]
- 65.Springer KW. Childhood physical abuse and midlife physical health: testing a multi-pathway life course model. Soc Sci Med. 2009 Jul;69(1):138–146. doi: 10.1016/j.socscimed.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hassmen P, Koivula N, Uutela A. Physical exercise and psychological well-being: a population study in Finland. Prev Med. 2000 Jan;30(1):17–25. doi: 10.1006/pmed.1999.0597. [DOI] [PubMed] [Google Scholar]
- 67.Chen E, Miller GE. “Shift-and-Persist” Strategies: Why Being Low in Socioeconomic Status isn’t Always Bad for Health. Perspectives on Psychological Science. 2012 Mar 1;7(2):135–158. doi: 10.1177/1745691612436694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen E, Miller GE, Lachman ME, Gruenewald TL, Seeman TE. Protective factors for adults from low-childhood socioeconomic circumstances: the benefits of shift-and-persist for allostatic load. Psychosom Med. 2012 Feb-Mar;74(2):178–186. doi: 10.1097/PSY.0b013e31824206fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hardt J, Vellaisamy P, Schoon I. Sequelae of prospective versus retrospective reports of adverse childhood experiences. Psychol Rep. 2010 Oct;107(2):425–440. doi: 10.2466/02.04.09.10.16.21.PR0.107.5.425-440. [DOI] [PubMed] [Google Scholar]
- 70.Yancura LA, Aldwin CM. Stability and change in retrospective reports of childhood experiences over a 5-year period: findings from the Davis Longitudinal Study. Psychol Aging. 2009 Sep;24(3):715–721. doi: 10.1037/a0016203. [DOI] [PubMed] [Google Scholar]
- 71.U.S. Census Bureau [Internet] State and County QuickFacts. 2013 [cited 2013 June 27]. Available from: http://quickfacts.census.gov/qfd/states/53000.html.
- 72.Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012 Jan;129(1):e232–246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 73.Katon WJ, Von Korff M, Lin EH, Simon G, Ludman E, Russo J, et al. The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry. 2004 Oct;61(10):1042–1049. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]


